Introduction
Most small burns are treated at home or by local providers as outpatients. This topic focuses on the initial resuscitation and management of severe burns. (Also see Burns, Evaluation and Management and Burns, Thermal).[1][2][3] The patient's age determines burn severity classification, the percentage of total body surface area burned (%TBSA), depth of burn, type of burn, and whether specific body parts are involved. Patients are classified as having severe burns if they have any of the following;
- >10% TBSA in children (<10 years old) or elderly (>50 years old)
- >20% TBSA in adults
- > 5% full thickness
- high-voltage electrical burns
- significant burns to the face, eyes, ears, joints, or genitalia
Other factors that should be considered and increase the patient’s morbidity and mortality include associated inhalation injury, associated traumatic injury, and the patient’s baseline medical conditions like heart disease or lung disease. Several factors may predispose the specific group of patients to more complicated injuries.[4][5] Severe burns cause not only significant injury at the local burn site but also a systemic response throughout the body. Inflammatory and vasoactive mediators such as histamines, prostaglandins, and cytokines are released, causing a systemic capillary leak, intravascular fluid loss, and large fluid shifts. These responses occur mostly over the first 24 hours, peaking around 6 to 8 hours after injury. This response, along with decreased cardiac output and increased vascular resistance, can lead to marked hypovolemia and hypoperfusion, called “burn shock.” This can be managed with aggressive fluid resuscitation and close monitoring for adequate, but not excessive, IV fluids.[6][7]It is important to remember that burns alone do not cause significant hypotension initially, and “burn shock” develops over the first few hours. If the patient is profoundly hypotensive initially, other causes of hypotension should be sought.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Burns to the face, eyes, ears, joints, hands, or genitalia are genitalia are generally considered more significant and require transfer to a burn center.
Indications
Adults and children with burns greater than 20% TBSA should undergo fluid resuscitation using estimates of body size and surface area burned. Common formulas used to initiate resuscitation estimate a crystalloid need for 2–4 ml/kg body weight/% TBSA during the first 24 hours.[8][9][10]
Contraindications
Excessive fluids are contraindicated in the hemodynamically stable burn patient, which likely contributes to edema.
Preparation
If a trauma with extensive burns is suspected, the team should prepare for burn resuscitation, which includes fluids, sterile sheets, and having pain medications quickly available.
Technique or Treatment
Resuscitation for Major Burns
Burns are dramatic injuries that can draw healthcare providers’ attention away from more immediate life or limb-threatening problems. The initial assessment and management of severely burned patients should be similar to the approach of a major trauma patient. However, for the burn patient, the very first step is to immediately stop the burning process and remove burning or hot items from skin contact. Providers should obtain an initial A.M.P.L.E. history (allergies, medications, past medical history, last oral intake, events of injury). The primary survey assesses the A.B.C.s for life threats. In the burn patient, attention should focus on the airway, looking for oral burns that might cause swelling and obstruction, breathing problems from smoke inhalation or lung injury, and bleeding or circulation problems by looking for life-threatening bleeding and checking blood pressure, heart rate, and pulses. The next step would be resuscitation and immediate intervention for life threats. A secondary survey with a complete physical exam follows this.
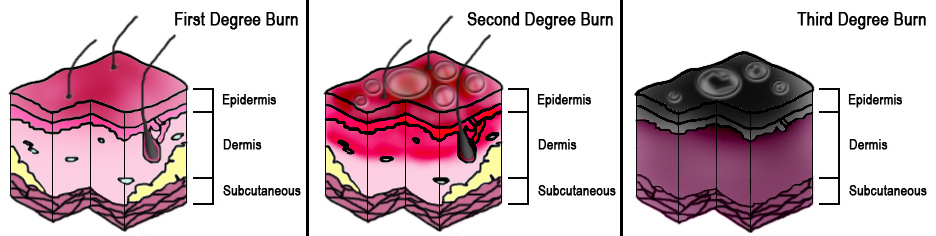
Evaluating and treating the burns are part of the secondary survey. The fundamental physical exam findings to record in burns are the extent of the burns, expressed as a percentage of total body surface area burned (% TBSA), and the depth of the burns, expressed as superficial (or first-degree), partial-thickness (or second-degree) or full-thickness (or third-degree).[11][12] See Image. Burn Degrees. Patients with burns of more than 20% - 25% of their body surface should be managed with aggressive IV fluid resuscitation to prevent “burn shock." Various formulas exist, like Brooke, Galveston, Rule of Ten, etc, but the Parkland Formula is the most common. This formula estimates the amount of fluid given in the first 24 hours, starting from the time of the burn.[13][14][15]
The Formula
Four mL lactated ringers solution × %TBSA burned × patient's weight in kilograms = total amount of fluid given in the first 24 hours. One-half of this fluid should be given in the first 8 hours. For example, a 75 kg patient with 55% total body surface area burn would need 4 mL LR × 75kg × 55% TBSA = 16,500 mL in the first 24 hours, with 8,250 mL in the first 8 hours or approximately 1 liter/hr for the first 8 hours. The Parkland Formula can be used for pediatric patients, plus normal maintenance fluids can be added.[16][17][18][19]
Whichever formula is used, the critical point to remember is the fluid amount calculated is just a guideline. The patient’s vital signs, mental status, capillary refill, and urine output must be monitored and fluid rates adjusted accordingly. Urine output of 0.5 mL/kg or about 30 – 50 mL/hr in adults and 0.5-1.0 mL/kg/hr in children under 30kg is a good target for adequate fluid resuscitation. Recent literature has raised concerns about complications from over-resuscitation, described as "fluid creep." Again, adequate fluid resuscitation is the goal.
Other management for severe burns includes nasal gastric tube placement, as most patients develop ileus. Foley catheters should be placed to monitor urine output. Cardiac and pulse oximetry monitoring is indicated. Pain control is best managed with IV medication.[20]Finally, burns are considered tetanus-prone wounds; tetanus prophylaxis is implied if not given in the past 5 years.[21]In any severe flame burn, you should always consider possible associated inhalation injury, carbon monoxide, or cyanide poisoning (see Inhalation Injury chapter).[22][23][24] Severe burn wound management should be directed to your local burn center. The burns should be gently cleansed and covered with clean dressings. Extensive debridement and application of topical antimicrobial creams or ointment are not needed if the patient is urgently transferred to a burn center because they need to do their burn assessment once the patient arrives.[25]
In certain situations, an emergent escharotomy may be necessary before transfer. An escharotomy is a surgical procedure performed to relieve the constricting effect of full-thickness burns. Because full-thickness burns are firm, leathery, and nonpliable, they can limit the typical swelling. This can create a compartment syndrome effect if the burns surround an extremity or an abdominal compartment syndrome effect if the burns surround the abdomen. If the burn involves extensive chest areas, then adequate ventilation may be impossible. In such cases, escharotomy should relieve the constriction effects and allow for adequate circulation or ventilation. An escharotomy is done by incision through the firm burn eschar, deep enough into the fat layer to enable the eschar to split open. This can be done at the bedside without an anesthetic because the burn has destroyed the nerve fibers, and the skin has lost sensation. Incisions are made on the medial and lateral sides of extremities and digits, along with the axillary lines and parallel to the clavicles on the upper chest and along the lateral abdominal walls on the abdomen.[26][27]
Complications
Deep or Extensive Burns Complications
- Breathing problems
- Bone and joint problems
- Dangerously low body temperature
- Infection and sepsis
- Low blood volume
- Scarring
- Tetanus[28][29]
Infection is the most common complication. In order of frequency, potential complications include pneumonia, cellulitis, urinary tract infections, and respiratory failure. Pneumonia commonly occurs in those with inhalation injuries.[30][31] Superficial partial-thickness burns are characterized by forming blisters within 24 hours between the epidermis and dermis. These wounds are painful, red, and weeping and become blanch with applying pressure. Initial burn assessments might be underestimated. Burns that initially seem to involve epidermal depth may be later categorized as partial-thickness wounds. These burns generally heal in 1 to 3 weeks; scarring is unusual, although discoloration may occur. These burns generally heal without any functional impairment or hypertrophic scarring. Deep partial-thickness wounds extend into the deeper dermis and have a different course than superficial partial-thickness burns. Deep burns involve hair follicles and glandular tissue. They almost always blister, are macerated, wet, or waxy dry, and demonstrate variable mottled colorization. Deep burns do not blanch when applied pressure. If the infection is prevented and spontaneous healing without grafting occurs, it heals in 2 to 9 weeks. Deep partial-thickness wounds always result in hypertrophic scarring. A deep partial-thickness burn that does not heal in 2 weeks would be considered a full-thickness burn in terms of functional and cosmetic outcomes.[32][33]
Other Complications
- Anemia secondary to full-thickness burns of greater than 10% TBSA is common.
- Electrical burns may result in compartment syndrome or rhabdomyolysis.
- Blood clotting in the veins of the legs occurs in 6-25% of patients with extensive burns.
- The hypermetabolic state that may persist for years after a major burn may decrease bone density and muscle mass.
- Keloids may form after a burn.
- Following a burn, psychological trauma and post-traumatic stress disorder may develop.
- Scarring may result in a disturbance in body image.
- In the developing world, significant burns may result in social isolation, poverty, and child abandonment.[34][35][36]
Clinical Significance
Burns are often preventable. Treatment depends on severity. Superficial burns may be managed with cleaning and pain medication, while major burns require prolonged treatment. Partial-thickness burns require cleaning with soap and water, followed by dressings. Full-thickness burns usually require surgical treatments, such as skin grafting. Extensive burns often require large amounts of intravenous fluid due to capillary fluid leakage and tissue swelling. The most common complications of burns involve infection. Burns are considered tetanus-prone wounds, and tetanus toxoids should be given every 5 years if not up to date. Burns often become infected; tetanus toxoid should be given if not current. Burns account for over 30 million injuries per year in the United States. This resulted in about 3 million hospitalizations and 240,000 deaths per year. In the United States, approximately 96% of those admitted to a burn center survive their injuries, but prompt treatment is required. All clinicians need to be familiar with the evaluation and appropriate referral of the burned patient.[37]
Enhancing Healthcare Team Outcomes
Managing burns requires an interprofessional team that includes an intensivist, burn specialist, pain specialist, infectious disease expert, emergency department physicians, wound care nurses, dietitians, and physical therapists. In general, second —and third-degree burns require more care than first-degree burns.
The most common complications of burns involve infection. Burns are considered tetanus-prone wounds, and tetanus toxoids should be given every 5 years if not up to date. Burns affect the entire body's physiology and often require management from specialists, including dietitians. Even after recovery, many require extensive physical therapy to regain muscle mass and function. Because burns profoundly affect aesthetics, all patients should be seen by a mental health nurse at regular intervals. The outcomes after burn injury depend on age, the extent of the injury, the type of burn, and the involvement of other organs. All clinicians need to be familiar with the evaluation and appropriate referral of the burned patient.[38][39][40]
Media
References
Arbuthnot MK, Garcia AV. Early resuscitation and management of severe pediatric burns. Seminars in pediatric surgery. 2019 Feb:28(1):73-78. doi: 10.1053/j.sempedsurg.2019.01.013. Epub 2019 Jan 18 [PubMed PMID: 30824139]
Berry J, Stone K, Reid J, Bell A, Burns R. Pediatric Emergency Medicine Simulation Curriculum: Electrical Injury. MedEdPORTAL : the journal of teaching and learning resources. 2018 Apr 27:14():10710. doi: 10.15766/mep_2374-8265.10710. Epub 2018 Apr 27 [PubMed PMID: 30800910]
Mehta M, Tudor GJ. Parkland Formula. StatPearls. 2024 Jan:(): [PubMed PMID: 30725875]
Chuang S, Chang KS, Woods DD, Chen HC, Reynolds ME, Chien DK. Beyond surge: Coping with mass burn casualty in the closest hospital to the Formosa Fun Coast Dust Explosion. Burns : journal of the International Society for Burn Injuries. 2019 Jun:45(4):964-973. doi: 10.1016/j.burns.2018.12.003. Epub 2018 Dec 28 [PubMed PMID: 30598266]
Padalko A, Cristall N, Gawaziuk JP, Logsetty S. Social Complexity and Risk for Pediatric Burn Injury: A Systematic Review. Journal of burn care & research : official publication of the American Burn Association. 2019 Jun 21:40(4):478-499. doi: 10.1093/jbcr/irz059. Epub [PubMed PMID: 30918946]
Level 1 (high-level) evidenceGentges J, Schieche C, Nusbaum J, Gupta N. Points & Pearls: Electrical injuries in the emergency department: an evidence-based review. Emergency medicine practice. 2018 Nov 1:20(Suppl 11):1-2 [PubMed PMID: 30383348]
Lam NN, Huong HTX, Tuan CA. Knowledge on emergency management for burn and mass burn injuries amongst physicians working in emergency and trauma departments. Annals of burns and fire disasters. 2018 Jun 30:31(2):138-143 [PubMed PMID: 30374267]
Pham C, Collier Z, Gillenwater J. Changing the Way We Think About Burn Size Estimation. Journal of burn care & research : official publication of the American Burn Association. 2019 Jan 1:40(1):1-11. doi: 10.1093/jbcr/iry050. Epub [PubMed PMID: 30247559]
Sun D, Zhao P, Ni JY, Sun JJ, Ren YW, Wang F, Zhu LH. [Effects of airway management team in the treatment of severely mass burn patients combined with inhalation injury]. Zhonghua shao shang za zhi = Zhonghua shaoshang zazhi = Chinese journal of burns. 2018 Jun 20:34(6):354-359. doi: 10.3760/cma.j.issn.1009-2587.2018.06.008. Epub [PubMed PMID: 29961292]
Mehrotra S, Misir A. Special Traumatized Populations: Burns Injuries. Current pediatric reviews. 2018:14(1):64-69. doi: 10.2174/1573396314666180608095033. Epub [PubMed PMID: 29879889]
Zuo KJ, Medina A, Tredget EE. Important Developments in Burn Care. Plastic and reconstructive surgery. 2017 Jan:139(1):120e-138e. doi: 10.1097/PRS.0000000000002908. Epub [PubMed PMID: 28027250]
Litt JS. Evaluation and Management of the Burn Patient: A Case Study and Review. Missouri medicine. 2018 Sep-Oct:115(5):443-446 [PubMed PMID: 30385993]
Level 3 (low-level) evidenceHollén L, Coy K, Day A, Young A. Resuscitation using less fluid has no negative impact on hydration status in children with moderate sized scalds: a prospective single-centre UK study. Burns : journal of the International Society for Burn Injuries. 2017 Nov:43(7):1499-1505. doi: 10.1016/j.burns.2017.04.011. Epub 2017 Jun 7 [PubMed PMID: 28601484]
Vivó C, Galeiras R, del Caz MD. Initial evaluation and management of the critical burn patient. Medicina intensiva. 2016 Jan-Feb:40(1):49-59. doi: 10.1016/j.medin.2015.11.010. Epub 2015 Dec 24 [PubMed PMID: 26724246]
Jennes S, Hanchart B, Keersebilck E, Rose T, Soete O, François PM, Engel H, Van Trimpont F, Davin C, Trippaerts M, Vanderheyden B, Etienne L, Lacroix C, Teodorescu S, Mashaekhi S, Persoons P, Baekelandt D, Hachimi Idrissil S, Watelet JB. Management of burn wounds of the head and neck region. B-ENT. 2016:Suppl 26(1):107-126 [PubMed PMID: 29461737]
Guilabert P, Usúa G, Martín N, Abarca L, Barret JP, Colomina MJ. Fluid resuscitation management in patients with burns: update. British journal of anaesthesia. 2016 Sep:117(3):284-96. doi: 10.1093/bja/aew266. Epub [PubMed PMID: 27543523]
Daniels M, Fuchs PC, Lefering R, Grigutsch D, Seyhan H, Limper U, The German Burn Registry, Schiefer JL. Is the Parkland formula still the best method for determining the fluid resuscitation volume in adults for the first 24 hours after injury? - A retrospective analysis of burn patients in Germany. Burns : journal of the International Society for Burn Injuries. 2021 Jun:47(4):914-921. doi: 10.1016/j.burns.2020.10.001. Epub 2020 Oct 17 [PubMed PMID: 33143988]
Level 2 (mid-level) evidenceZodda D. Calculated decisions: Parkland formula for burns. Pediatric emergency medicine practice. 2018 Apr 1:15(Suppl 4):1-2 [PubMed PMID: 29617546]
Zodda D. Calculated decisions: Parkland formula for burns. Emergency medicine practice. 2018 Jan 25:20(Suppl 2):S1-S2 [PubMed PMID: 29369604]
Walsh K, Stiles K, Dheansa B. Concerns relating to the European resuscitation guidelines for the first aid management of burns. Burns : journal of the International Society for Burn Injuries. 2016 Feb:42(1):240-241. doi: 10.1016/j.burns.2015.11.005. Epub 2015 Dec 13 [PubMed PMID: 26695125]
Ito T, Kukino R, Takahara M, Tanioka M, Nakamura Y, Asano Y, Abe M, Ishii T, Isei T, Inoue Y, Imafuku S, Irisawa R, Ohtsuka M, Ohtsuka M, Ogawa F, Kadono T, Kawakami T, Kawaguchi M, Kono T, Kodera M, Sakai K, Nakanishi T, Hashimoto A, Hasegawa M, Hayashi M, Fujimoto M, Fujiwara H, Maekawa T, Matsuo K, Madokoro N, Yamasaki O, Yoshino Y, Le Pavoux A, Tachibana T, Ihn H, Wound/Burn Guidelines Committee. The wound/burn guidelines - 5: Guidelines for the management of lower leg ulcers/varicose veins. The Journal of dermatology. 2016 Aug:43(8):853-68. doi: 10.1111/1346-8138.13286. Epub 2016 Mar 12 [PubMed PMID: 26973097]
Foncerrada G, Culnan DM, Capek KD, González-Trejo S, Cambiaso-Daniel J, Woodson LC, Herndon DN, Finnerty CC, Lee JO. Inhalation Injury in the Burned Patient. Annals of plastic surgery. 2018 Mar:80(3 Suppl 2):S98-S105. doi: 10.1097/SAP.0000000000001377. Epub [PubMed PMID: 29461292]
Dries DJ, Endorf FW. Inhalation injury: epidemiology, pathology, treatment strategies. Scandinavian journal of trauma, resuscitation and emergency medicine. 2013 Apr 19:21():31. doi: 10.1186/1757-7241-21-31. Epub 2013 Apr 19 [PubMed PMID: 23597126]
Culnan DM, Craft-Coffman B, Bitz GH, Capek KD, Tu Y, Lineaweaver WC, Kuhlmann-Capek MJ. Carbon Monoxide and Cyanide Poisoning in the Burned Pregnant Patient: An Indication for Hyperbaric Oxygen Therapy. Annals of plastic surgery. 2018 Mar:80(3 Suppl 2):S106-S112. doi: 10.1097/SAP.0000000000001351. Epub [PubMed PMID: 29461288]
Carmichael H, Dyamenahalli K, Duffy PS, Lambert Wagner A, Wiktor AJ. Triage and Transfer to a Regional Burn Center-Impact of a Mobile Phone App. Journal of burn care & research : official publication of the American Burn Association. 2020 Sep 23:41(5):971-975. doi: 10.1093/jbcr/iraa098. Epub [PubMed PMID: 32588890]
Zhang L, Labib A, Hughes PG. Escharotomy. StatPearls. 2024 Jan:(): [PubMed PMID: 29489153]
de Barros MEPM, Coltro PS, Hetem CMC, Vilalva KH, Farina JA Jr. Revisiting Escharotomy in Patients With Burns in Extremities. Journal of burn care & research : official publication of the American Burn Association. 2017 Jul/Aug:38(4):e691-e698. doi: 10.1097/BCR.0000000000000476. Epub [PubMed PMID: 27984410]
Irie BGS, Asse KV, Kadiane NJ, Kofi N, Nda-Koffi C, Ogondon B, Kouadio S, Kouame KE, Brouh Y. Tetanus after application of traditional topical treatment to a severe burn. Medecine et sante tropicales. 2018 Nov 1:28(4):446-447. doi: 10.1684/mst.2018.0803. Epub [PubMed PMID: 30095076]
Ladhani HA, Yowler CJ, Claridge JA. Burn Wound Colonization, Infection, and Sepsis. Surgical infections. 2021 Feb:22(1):44-48. doi: 10.1089/sur.2020.346. Epub 2020 Oct 20 [PubMed PMID: 33085576]
Nielson CB, Duethman NC, Howard JM, Moncure M, Wood JG. Burns: Pathophysiology of Systemic Complications and Current Management. Journal of burn care & research : official publication of the American Burn Association. 2017 Jan/Feb:38(1):e469-e481. doi: 10.1097/BCR.0000000000000355. Epub [PubMed PMID: 27183443]
Başaran A,Gürbüz K,Özlü Ö,Demir M,Eroğlu O,Daş K, Electrical burns and complications: Data of a tertiary burn center intensive care unit. Ulusal travma ve acil cerrahi dergisi = Turkish journal of trauma & emergency surgery : TJTES. 2020 Mar [PubMed PMID: 32185768]
Young AW, Dewey WS, King BT. Rehabilitation of Burn Injuries: An Update. Physical medicine and rehabilitation clinics of North America. 2019 Feb:30(1):111-132. doi: 10.1016/j.pmr.2018.08.004. Epub 2018 Oct 31 [PubMed PMID: 30470416]
Thananopavarn P, Hill JJ 3rd. Rehabilitation of the Complex Burn Patient with Multiple Injuries or Comorbidities. Clinics in plastic surgery. 2017 Oct:44(4):695-701. doi: 10.1016/j.cps.2017.05.002. Epub 2017 Jul 21 [PubMed PMID: 28888295]
Cable CA, Razavi SA, Roback JD, Murphy DJ. RBC Transfusion Strategies in the ICU: A Concise Review. Critical care medicine. 2019 Nov:47(11):1637-1644. doi: 10.1097/CCM.0000000000003985. Epub [PubMed PMID: 31449062]
Dubick MA,Barr JL,Keen CL,Atkins JL, Ceruloplasmin and Hypoferremia: Studies in Burn and Non-Burn Trauma Patients. Antioxidants (Basel, Switzerland). 2015 Mar 6 [PubMed PMID: 26785343]
Wang Y, Beekman J, Hew J, Jackson S, Issler-Fisher AC, Parungao R, Lajevardi SS, Li Z, Maitz PKM. Burn injury: Challenges and advances in burn wound healing, infection, pain and scarring. Advanced drug delivery reviews. 2018 Jan 1:123():3-17. doi: 10.1016/j.addr.2017.09.018. Epub 2017 Sep 20 [PubMed PMID: 28941987]
Level 3 (low-level) evidenceArmstrong M, Wheeler KK, Shi J, Thakkar RK, Fabia RB, Groner JI, Noffsinger D, Giles SA, Xiang H. Epidemiology and trend of US pediatric burn hospitalizations, 2003-2016. Burns : journal of the International Society for Burn Injuries. 2021 May:47(3):551-559. doi: 10.1016/j.burns.2020.05.021. Epub 2020 May 30 [PubMed PMID: 33781634]
Gupta N, Nusbaum J. Points & Pearls: Emergency department management of patients with thermal burns. Emergency medicine practice. 2018 Feb 1:20(2):e1-e2 [PubMed PMID: 29388754]
Kuo LW, Yen CI, Fu CY, Pan CH, Hsu CP, Hsiao YC, Hsieh CH, Hsu YP. The role of preliminary hospitals in the management of a mass burn casualty disaster. Burns : journal of the International Society for Burn Injuries. 2018 Jun:44(4):800-806. doi: 10.1016/j.burns.2017.11.014. Epub 2017 Dec 16 [PubMed PMID: 29258727]
Caldwell NW, Serio-Melvin ML, Chung KK, Salinas J, Shiels ME, Cancio LC, Stockinger ZT, Mann-Salinas EA. Follow-Up Evaluation of the U.S. Army Institute of Surgical Research Burn Flow Sheet for En Route Care Documentation of Burned Combat Casualties. Military medicine. 2017 Nov:182(11):e2021-e2026. doi: 10.7205/MILMED-D-17-00121. Epub [PubMed PMID: 29087874]