Introduction
The ulna's coronoid process is the bony prominence on the most proximal portion of the ulna’s volar surface. In connection with the olecranon process, it forms the greater sigmoid notch which articulates with the distal humerus at the elbow joint. It serves as a buttress, preventing posterior displacement of the ulna. It is also the site of attachment for the anterior bundle of the ulnar collateral ligament which inserts on the medial portion of the coronoid, the sublime tubercle, approximately 1.8 centimeters from the tip of the coronoid.[1] The ulnar collateral ligament serves to limit valgus forces on the elbow joint. More proximally, the elbow joint capsule also attaches about 0.6 centimeters from the intra-articular coronoid tip.[1] Distally, near the base of the coronoid, the brachialis muscle takes a broad insertion; it acts to flex the elbow without effecting forearm rotation.[1]
Fractures of the coronoid are highly suggestive of elbow instability; and they often present in association with elbow dislocations and other fractures of the radius, ulna, or humerus.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Coronoid fractures are believed to occur due to a shearing force when elbow experiences excess stress. They are often the result of an associated elbow dislocation.[2] Two to fifteen percent of elbow dislocations result in fractures of the coronoid.[3] Significant varus forces on the elbow can lead to fractures of the anteromedial facet of the coronoid.
Epidemiology
Coronoid fractures are almost always traumatic; therefore, those participating in sporting events, high-velocity activity, and other riskier behaviors are at risk to sustain this injury. Motor vehicle accidents are the most common cause of proximal ulna fractures.[4]
Coronoid fractures account for approximately 10 to 15% of fractures about the elbow.[5][3]
History and Physical
Patients may describe a dislocation and potential self-reduction of the elbow.
If dislocated, the elbow deformity will be obvious. Note the position of comfort; this will be approximately 75 degrees of flexion if a large effusion is present.[6] This position maximizes space within the joint capsule. The normal “carrying angle,” or cubital valgus, is approximately 11 degrees for men and 13 degrees for women. There will likely be diffuse tenderness to palpation. Open fractures must be ruled out by thorough inspection of the skin about the elbow. If a reduction of the elbow joint is required, the range of motion should undergo assessment after the reduction; attention should focus on identifying which positions increase or decrease stability. Normal elbow flexion is approximately 140 degrees. Normal supination and pronation are about 80 degrees in each direction; evaluation should be with the elbow flexed to 90 degrees. The neurovascular status also requires evaluation, both before and after the attempted reduction of dislocations.
The ulnar or medial collateral ligaments of the elbow testing can be by performing standard valgus stress to the elbow. This should be performed with the elbow flexed to 30 degrees, allowing the olecranon to disengage the humerus. It may be difficult to stabilize the humerus and subtle laxity in the UCL can be missed. Therefore, the “moving valgus stress test” is an important test to learn. It has been noted to have a very high sensitivity.[6] This test is performed with the shoulder abducted to 90 degrees and fully externally rotated; the elbow is fully flexed. Gentle valgus stress is applied as the elbow is smoothly and quickly moved into an extended position. Pain between the ranges of 70 and 120 degrees of flexion constitutes a positive exam.
The “milking maneuver” is another good examination tool to assess the medial ligamentous structures which may be frequently injured in association with a coronoid process fracture. This involves placing the involved upper extremity in a position where the shoulder and elbow are both flexed to 90 degrees and the forearm is supinated. From this position, either the patient or the examiner may pull the thumb to apply a valgus force on the elbow. A positive test is apprehension, medial elbow pain, or instability at the elbow.[6]
Posterolateral rotatory instability (PLRI) may be assessed with both the “lateral pivot shift test” and the “posterolateral drawer test”. The pivot shift test is performed is initiated with the patient supine, the arm abducted over the head and fully externally rotated, and the forearm supinated. The clinician holds the wrist. A valgus and supinating force is applied along with gentle axial compression as the elbow is moved from full extension into flexion. A positive test involved pain and apprehension at approximately 40 degrees of flexion. If performed under anesthesia, a clunk may be appreciated with a dimple visualized proximal to the radial head. This represents subluxation of the radiocapitallar joint. Further flexion should lead to a reduction of the joint.[6]
The posterolateral rotatory drawer test is completed with the elbow at a position of 30 to 40 degrees of flexion. The examiner then applies a posteriorly directed force to the lateral portion of the proximal forearm; this resembles hyper-supination of the forearm. The goal is to translate the radius and ulna posteriorly by pivoting around the intact medial elbow ligaments. A test is deemed positive if apprehension or skin dimpling is noted.[6]
Perhaps a simpler physical exam maneuver can be performed by having the patient push up from the armrest of their chair with the forearm supinated and shoulders abducted. Pain, instability, and apprehension can again be considered a positive test for posterolateral rotatory instability. Repeating the maneuver with the forearm pronated by eliminating the apprehension.
Evaluation
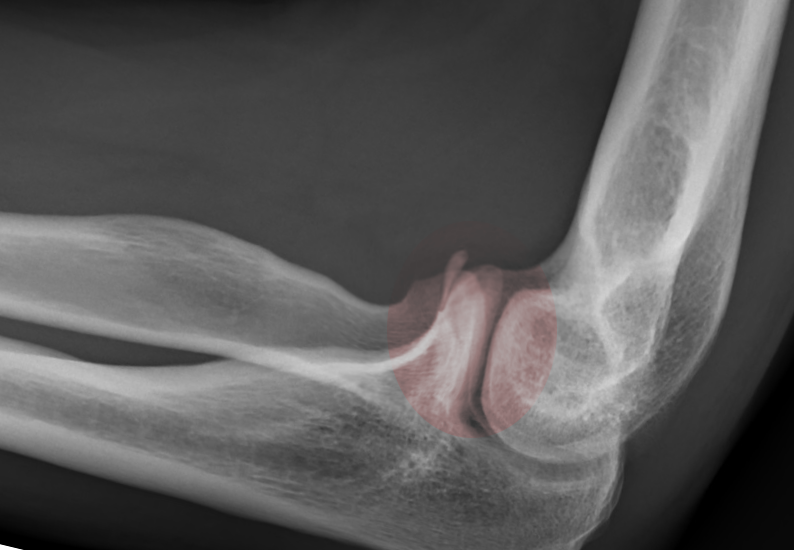
Imaging
Standard radiographs are the initial step in evaluating coronoid fractures after the physical exam. Anterior-posterior, lateral, and oblique views are standard images to obtain. The lateral view may often be the best image to appreciate the size and displacement of the coronoid fracture.
Computed tomography (CT) scans can often be helpful in better characterizing these fractures as interpreting plain film radiographs can be difficult due to overlapping cortical lines.
Classifications
Traditionally, the Regan and Morrey classification has been used to describe coronoid fractures based on the amount of the process that is involved. Type one fractures include only the tip of the coronoid. Type two fractures involve 50% or less of the coronoid height; whereas, type three fractures involve large fragments over 50% of the coronoid height.[7]
The O’Driscoll classification system provides a more comprehensive scheme, which importantly brings attention to fractures involving the anteromedial facet.[2][8] Within this classification system is type I fractures, which affect the tip of the coronoid. These are often associated with terrible triad injuries and posterolateral instability of the elbow. O’Driscoll type II fractures involve the anteromedial portion of the process which may or may not include the sublime tubercle. These types of injuries often have associations with posteromedial rotary instability, potentially disrupting the lateral collateral ligament of the elbow. Type III fractures disrupt the base of the coronoid process and many times are associated with other proximal ulna fractures such as the olecranon or the proximal portion of the ulnar shaft.[9]
Treatment / Management
The clinician should attempt a closed reduction of any associated elbow dislocation as early as possible. Open reduction may be necessary in the event of entrapped bony fragments or soft tissues within the joint.
Non-operative treatment of isolated coronoid process fractures should include brief immobilization and early range of motion to deter stiffness. Favorable results have occurred with conservative treatment in some patients. Indications include a perfectly concentric ulnohumeral joint, absence of a significantly associated radial head fractures, and a coronoid fracture involving less than 50% of the coronoid height.[10]
Stability of the elbow, not the size of the coronoid fragment, is the main consideration for surgical fixation. Small fragments, however, such as Regan and Morrey type I fractures are more likely to result in stable elbows and be amenable to conservative treatment. Indications for operative management include coronoid fractures associated with unstable elbows. Fixation strategies and surgical approaches vary depending on the characteristics of the fracture as well as associated injuries.[7] Posterior approaches have been suggested to be advantageous for severe coronoid fractures with other significant associated elbow injuries.[11] The direct anterior approach for anterior buttressing of large coronoid fragments is another option that provides good access but places neurovascular structures at risk.[12][13] Lastly, the classic “over-the-top Hotchkiss approach” to the medial elbow exposes the anteromedial facet for buttress plating; however, a flexor carpi ulnaris splitting approach has been suggested to provide additional anteromedial exposure.[14](B2)
In terms of internal fixation, once these fractures are visualized and reduced, there are again multiple considerations. Lasso suture fixation of the coronoid via a trans-osseous tunnel drilled posterior to anterior through the proximal ulna has been shown to restore stability of the coronoid.[15] This approach may be most useful with small coronoid fragments. Other internal fixation options include the use of internal fixation with a retrograde screw or small plate and screw fixation. Anteromedial facet fractures, O’Driscoll type II, are been shown to be well addressed with medial buttress plating and lateral collateral ligament repair.[16](B2)
Differential Diagnosis
Simple elbow dislocations, while less common, can occur without any associated fractures.
Terrible triad injuries of the elbow are notorious for recurrent instability and significant post-traumatic arthritis. The triad consists of a coronoid fracture, a radial head fracture, and an elbow dislocation (usually with lateral collateral ligament injury resulting in posterolateral rotatory instability). These injuries most often require surgical stabilization of the fractures as well as ligamentous repair. Non-operative treatment is an option if the elbow is stable after a concentric reduction, and both the coronoid and radial head fractures are independently amenable to non-operative treatment.
Prognosis
Prompt and appropriate treatment of coronoid fractures can lead to good outcomes. Failure to diagnose and appropriately treat these injuries can significantly limit the use of the elbow due to pain and instability.
Complications
Heterotopic ossifications due to surgical dissection are common about the elbow. Indomethacin and radiation therapy are options to address this.
Elbow stiffness is also a common issue after extended periods of immobilization.[3]
Recurrent instability and posttraumatic arthritis are also common complications of coronoid fractures. A congruent reduction of the elbow joint is paramount to minimize these issues. Many experts agree that the stability of the elbow can be restored with maintains of an anatomic reduction for at least 4 weeks, allowing collateral ligaments to heal appropriately.[17]
Postoperative and Rehabilitation Care
Physical therapy following coronoid fracture fixation is usually surgeon dependent and is variable. The elbow is typically immobilized initially in a position of 90 degrees of flexion. In cases of associated lateral instability, the forearm often gets placed in a pronated position to increase stability and protect ligamentous repair or reconstruction. Immobilization in supination is the recommended approach for cases with involved medial ligament injuries.[12] Shoulder abduction should be avoided as it may stress repaired lateral collateral ligaments.[15] Passive range of motion is initiated around weeks one or two and advanced to strengthing exercises around 8 to 12 weeks. Prolonged immobilization has been frequently shown to lead to significant stiffness and poor outcomes.[3] A hinged elbow brace may be utilized in the early stages of rehabilitation to provided additional protect and limit terminal extension. Unrestricted activity is often allowed within a 4 to 6-month range following surgical fixation.
Deterrence and Patient Education
Deterrence of coronoid fractures is difficult given their traumatic nature.
The patient should always have a thorough comprehension through education on the common complications of this injury. Instability and arthritis are possible with and without surgical intervention. As many coronoid process fractures require surgical treatment, the risk and benefit of such procedures should always be discussed at length to provide patient autonomy and the ability to make wise decisions. There should also be a discussion regarding expectations and limitations after surgery.
Enhancing Healthcare Team Outcomes
Coronoid fractures can be associated with other injuries of the arm and can be difficult to diagnose; for this reason, an interprofessional team is the best approach to managing this condition. Even though patients initially present to the emergency department, the orthopedic surgeon should be involved in the care.
The emergency department physician or nurse practitioner usually orders the initial X-rays but should not attempt treatment until receiving a radiologist's report and obtaining a consult from the surgeon. The pharmacy may be involved in the acute phase as pain control may be necessary, and the pharmacist should verify agent selection, dosing, and perform medication reconciliation and report back to the healthcare team any discrepancies. Following management by the orthopedic surgeon, the nurse practitioner and primary care provider may follow the patient. Functional motion, strength, and the ability to return to daily activities can experience significant improvement by physical and occupational therapy, who should keep the managing physician apprised of the progress with rehabilitation. Whether in the postoperative setting or as a component of conservative treatment, rehabilitation is an essential factor when seeking the best possible outcome following a coronoid process fracture. Before returning to any sporting activity, the orthopedic surgeon should render a final consultation. Nursing staff will have involvement at every step of the way, from initial visits through surgery, and follow-up visits. They should report any unusual findings to the managing clinician as they find them — This type of interprofessional collaboration optimizes patient outcomes. [Level 5]
Open interprofessional communication and trust between patients, therapists, and physicians can improve outcomes and satisfaction.[18] [Level 3]
Media
References
Cage DJ, Abrams RA, Callahan JJ, Botte MJ. Soft tissue attachments of the ulnar coronoid process. An anatomic study with radiographic correlation. Clinical orthopaedics and related research. 1995 Nov:(320):154-8 [PubMed PMID: 7586820]
O'Driscoll SW, Jupiter JB, King GJ, Hotchkiss RN, Morrey BF. The unstable elbow. Instructional course lectures. 2001:50():89-102 [PubMed PMID: 11372363]
Wells J, Ablove RH. Coronoid fractures of the elbow. Clinical medicine & research. 2008 May:6(1):40-4. doi: 10.3121/cmr.2008.753. Epub [PubMed PMID: 18591378]
Niéto H, Billaud A, Rochet S, Lavoinne N, Loubignac F, Pietu G, Baroan C, Espie A, Bonnevialle P, Fabre T. Proximal ulnar fractures in adults: a review of 163 cases. Injury. 2015 Jan:46 Suppl 1():S18-23. doi: 10.1016/S0020-1383(15)70006-9. Epub 2015 Jan 19 [PubMed PMID: 26528935]
Level 3 (low-level) evidenceSelesnick FH, Dolitsky B, Haskell SS. Fracture of the coronoid process requiring open reduction with internal fixation. A case report. The Journal of bone and joint surgery. American volume. 1984 Oct:66(8):1304-6 [PubMed PMID: 6490710]
Level 3 (low-level) evidenceSmith MV, Lamplot JD, Wright RW, Brophy RH. Comprehensive Review of the Elbow Physical Examination. The Journal of the American Academy of Orthopaedic Surgeons. 2018 Oct 1:26(19):678-687. doi: 10.5435/JAAOS-D-16-00622. Epub [PubMed PMID: 30095513]
Regan W, Morrey B. Fractures of the coronoid process of the ulna. The Journal of bone and joint surgery. American volume. 1989 Oct:71(9):1348-54 [PubMed PMID: 2793888]
Level 2 (mid-level) evidenceSanchez-Sotelo J, O'Driscoll SW, Morrey BF. Medial oblique compression fracture of the coronoid process of the ulna. Journal of shoulder and elbow surgery. 2005 Jan-Feb:14(1):60-4 [PubMed PMID: 15723014]
Level 3 (low-level) evidenceTashjian RZ, Katarincic JA. Complex elbow instability. The Journal of the American Academy of Orthopaedic Surgeons. 2006 May:14(5):278-86 [PubMed PMID: 16675621]
Foruria AM, Gutiérrez B, Cobos J, Haeni DL, Valencia M, Calvo E. Most coronoid fractures and fracture-dislocations with no radial head involvement can be treated nonsurgically with elbow immobilization. Journal of shoulder and elbow surgery. 2019 Jul:28(7):1395-1405. doi: 10.1016/j.jse.2019.01.005. Epub 2019 Apr 5 [PubMed PMID: 30956143]
Chen HW, Teng XF. A comparative study on the validity and reliability of anterior, medial, and posterior approaches for internal fixation in the repair of fractures of the coronoid process of the ulna. European journal of medical research. 2018 Sep 11:23(1):40. doi: 10.1186/s40001-018-0336-7. Epub 2018 Sep 11 [PubMed PMID: 30205841]
Level 2 (mid-level) evidenceFeng D, Zhang X, Jiang Y, Zhu Y, Wang H, Wu S, Zhang K, Wang Z, Zhang J. Plate fixation through an anterior approach for coronoid process fractures: A retrospective case series and a literature review. Medicine. 2018 Sep:97(36):e12041. doi: 10.1097/MD.0000000000012041. Epub [PubMed PMID: 30200084]
Level 2 (mid-level) evidenceShen JJ, Qiu QM, Gao YB, Tong SL, Huang JF. Direct anterior approach for mini plate fixation of Regan-Morrey type II comminuted ulnar coronoid process fracture. Journal of orthopaedic surgery (Hong Kong). 2019 Jan-Apr:27(1):2309499018825223. doi: 10.1177/2309499018825223. Epub [PubMed PMID: 30798735]
Level 2 (mid-level) evidenceHuh J, Krueger CA, Medvecky MJ, Hsu JR, Skeletal Trauma Research Consortium. Medial elbow exposure for coronoid fractures: FCU-split versus over-the-top. Journal of orthopaedic trauma. 2013 Dec:27(12):730-4. doi: 10.1097/BOT.0b013e31828ba91c. Epub [PubMed PMID: 23412510]
Garrigues GE, Wray WH 3rd, Lindenhovius AL, Ring DC, Ruch DS. Fixation of the coronoid process in elbow fracture-dislocations. The Journal of bone and joint surgery. American volume. 2011 Oct 19:93(20):1873-81. doi: 10.2106/JBJS.I.01673. Epub [PubMed PMID: 22012524]
Level 2 (mid-level) evidencePark SM, Lee JS, Jung JY, Kim JY, Song KS. How should anteromedial coronoid facet fracture be managed? A surgical strategy based on O'Driscoll classification and ligament injury. Journal of shoulder and elbow surgery. 2015 Jan:24(1):74-82. doi: 10.1016/j.jse.2014.07.010. Epub 2014 Oct 7 [PubMed PMID: 25304044]
Level 2 (mid-level) evidenceRing D. Editorial comment: Traumatic elbow instability and its sequelae. Clinical orthopaedics and related research. 2014 Jul:472(7):2035-6. doi: 10.1007/s11999-014-3599-5. Epub [PubMed PMID: 24711132]
Level 3 (low-level) evidenceHall AM, Ferreira PH, Maher CG, Latimer J, Ferreira ML. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Physical therapy. 2010 Aug:90(8):1099-110. doi: 10.2522/ptj.20090245. Epub 2010 Jun 24 [PubMed PMID: 20576715]
Level 1 (high-level) evidence