Anatomy, Shoulder and Upper Limb, Hand Thenar Eminence
Anatomy, Shoulder and Upper Limb, Hand Thenar Eminence
Introduction
The word thenar originates from the Greek meaning “palm of the hand.” The hypothenar eminence is located on the ulnar portion of the volar hand at the base of the fifth digit (small finger). The thenar eminence is located on the radial portion of the volar hand at the base of the first digit (thumb).
The thenar eminence is composed of three muscles that control the movements of the thumb: abductor pollicis brevis (APB), flexor pollicis brevis (FPB), and the opponens pollicis. Medical conditions that can affect the thenar eminence include carpal tunnel syndrome, arthritis, and amyotrophic lateral sclerosis (ALS), among others.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The thenar eminence can be easily identified by palpating the base of the thumb on the palm (volar) side of the hand. The abductor pollicis brevis, flexor pollicis brevis, and the opponens pollicis are located here and control the movements of the thumb. These muscles work to provide adduction, abduction, flexion, pronation, and opposition for the thumb.
The abductor pollicis brevis abducts the thumb. This muscle is located superficial and lateral to the other two muscles. Its origin is mainly from the flexor retinaculum but also originates from the tubercles of the scaphoid and trapezium. It then travels both distal and lateral to insert on the base of the proximal phalanx of the thumb.
The flexor pollicis brevis is located superficial and medial to the opponens pollicis. It has two muscle heads, a superficial and a deep one. Both heads are separated by the flexor pollicis longus. Its origin is the trapezium and flexor retinaculum, and it inserts on the proximal phalanx of the thumb. It functions to flex the thumb.
The opponens pollicis is located deep to the other muscles, and it is also the largest. It originates from both the flexor retinaculum and the trapezium tubercle. It inserts on the anterolateral portion of the first metacarpal shaft and opposes the thumb. Opposition in this context is both adduction and pronation. This movement allows the tip of the thumb to contact the tips of the other digits on the same hand.[2][3]
Embryology
The muscles of the thenar eminence are derived from the mesodermal germ layer. The mesoderm further differentiates into the vasculature involved in this location. The ectodermal germ layer differentiates to form the skin and neural networks located here.[4]
Blood Supply and Lymphatics
The abductor pollicis brevis, flexor pollicis brevis, and opponens pollicis receive their blood supply from the superficial palmar branch of the radial artery. This artery branches from the radial artery immediately proximal to the flexor retinaculum. It then runs superficial to the flexor retinaculum as it travels distally to supply the thenar eminence. Later, it anastomoses with the superficial palmar arch, the terminal branch of the ulnar artery.[5]
Nerves
The thenar eminence is primarily innervated by the median nerve (T1) but does receive some contribution from the ulnar nerve (C8, T1): the two heads of the flexor pollicis brevis have different innervation. The deep head is innervated by the deep branch of the ulnar nerve (C8, T1), while the superficial head is innervated by the recurrent branch of the median nerve (T1). The abductor pollicis brevis and opponens pollicis are both innervated solely by the recurrent branch of the median nerve.[6]
The median nerve arises from the medial and lateral cords of the brachial plexus. It then travels distally down the arm between the two heads of the pronator teres. It passes within the carpal tunnel, deep to the flexor retinaculum, and branches further. One of these branches is the recurrent branch which innervates the thenar eminence.
Muscles
The thenar eminence is composed of three muscles that control the movements of the thumb, as described previously. The muscles are listed below:
- Abductor pollicis brevis
- Flexor pollicis brevis
- Opponens pollicis
Physiologic Variants
Some consider the adductor pollicis to be a member of the thenar eminence. This muscle consists of an oblique and transverse head. The oblique head originates from the capitate and the bases of metacarpals two and three.
The transverse head originates from the base of metacarpal three. The two heads combine and travel laterally to insert onto the base of the proximal phalanx of the thumb. It is supplied by the deep palmar arch and is innervated by the ulnar nerve. It functions to adduct the thumb and also assists in producing the movement of opposition.[7]
Surgical Considerations
Many surgical operations of the hand require a thorough understanding of thenar eminence anatomy. Carpal tunnel syndrome, thumb arthritis, and fractures are common conditions that may require surgery.
Carpal tunnel syndrome (CTS) is caused by compression of the median nerve at the transverse carpal ligament. The thenar eminence is innervated by a branch of this nerve, so severe forms of CTS can have significant ramifications on the thenar eminence and, ultimately, thumb function.[7] Patients can experience atrophy of the thenar eminence as well as pain and paresthesia. Surgery is considered if conservative management fails or acute onset of CTS, such as after distal radius fractures or lunate or perilunate dislocations.[8]
Carpal tunnel release can be performed to decompress the median nerve by incising the transverse carpal ligament to increase the space within the carpal tunnel. It can be performed in either an open or endoscopic manner. Open techniques use a slightly larger incision, but there are no differences in outcomes. The surgery only takes about 15 minutes, and most patients will have relief from either some or all of their symptoms.[8]
Surgical options for thumb arthritis include arthroscopic debridement, osteotomy of the first metacarpal, trapeziectomy, carpometacarpal (CMC) arthrodesis, CMC denervation, and CMC prosthetic arthroplasty. Each of these procedures is unique in its technique, but all of them involve navigating through or manipulating some anatomical portion of the thenar eminence.[9]
Fractures of the first metacarpal or trapezium affect the thenar eminence. All three muscles of the thenar eminence have part of their origin on the trapezium and travel superficially to the first metacarpal. Fractures here can disrupt the integrity of these muscles and may also damage nearby neurological structures causing sensory or motor deficits. Surgical interventions include open reduction, internal fixation, external fixation, and metacarpophalangeal arthroplasty or fusion.[10]
Clinical Significance
Carpal tunnel syndrome is considered a compressive neuropathy of the median nerve that causes pain, paresthesia, and muscle wasting in the thenar eminence. It is diagnosed clinically based on a patient’s signs and symptoms. Females are three times more likely than males to be affected by CTS. Conditions such as pregnancy and arthritis are considered risk factors as well. People who perform repetitive motions or vibrations of the wrist, such as excessive typing, are more likely to be affected by CTS.[8]
The median nerve has multiple branches. Therefore, the palmar cutaneous branch travels superficially to the carpal tunnel and is not affected by CTS. This branch is responsible for skin sensation over the thenar eminence. The recurrent branch travels through the carpal tunnel before returning proximally to innervate the muscles of the thenar eminence. Compression of the recurrent branch can lead to muscle atrophy of the thenar eminence.[7]
Multiple physical exam maneuvers can be performed to identify CTS, and these include Tinel’s test, Durkan’s test, and Phalen’s Test. Additional modalities are not required for diagnosis but can provide useful adjunctive information, especially in complex presentations. Nerve conduction velocity (NCV) and electromyography (EMG) are often used. NCV shows slowing conduction velocity, and EMG shows fibrillations and fasciculations of the muscles.[7][8]
First-line treatment for CTS is non-operative and typically involves the use of NSAIDs, activity modification, and nighttime neutral splinting. If first-line therapy fails, steroid injections may be utilized and have shown transient improvement in 80% of patients. Surgical intervention may be considered if non-operative management fails to treat CTS and often results in partial or complete relief of symptoms in 75% of patients.[7][8]
Atrophy of the hand muscles is a characteristic feature of ALS. It most often occurs in the thenar eminence while the hypothenar eminence is spared. This is known as the split hand sign, and it can be the initial presentation of ALS as it may appear before upper motor nerve signs. Kuwabara et al. used EMG on 77 patients with ALS and 171 patients without ALS, which confirmed thenar involvement and hypothenar sparing muscle wasting in early ALS.[11]
Ape hand deformity is caused by damage to the recurrent motor branch of the median nerve. This causes the muscles of the thenar eminence to be denervated and lose function, specifically the opponens pollicis. People with this deformity are not able to perform opposition with the thumb. Damage to this nerve typically occurs at either the elbow or the wrist. Median nerve palsy may also present with ape hand deformity and typically occurs following a deep penetrating injury or blunt force trauma to the arm, forearm, or wrist.
Supracondylar humerus fractures may also cause this deformity. The anterior interosseus nerve (AIN), a significant motor branch of the median nerve, lies anterior to the supracondylar humerus and is at risk of being stretched, impinged, or pierced during fracture. This type of fracture is most common in children due to falling on an outstretched arm.[7]
Media
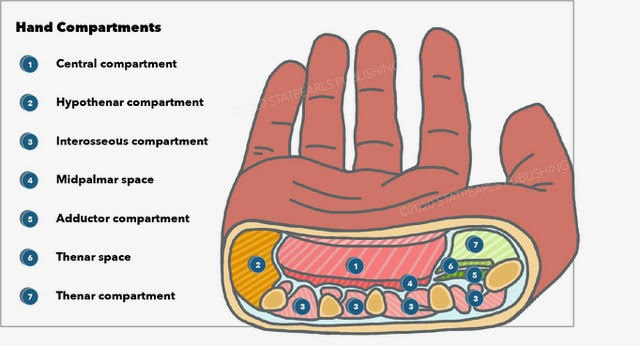
(Click Image to Enlarge)
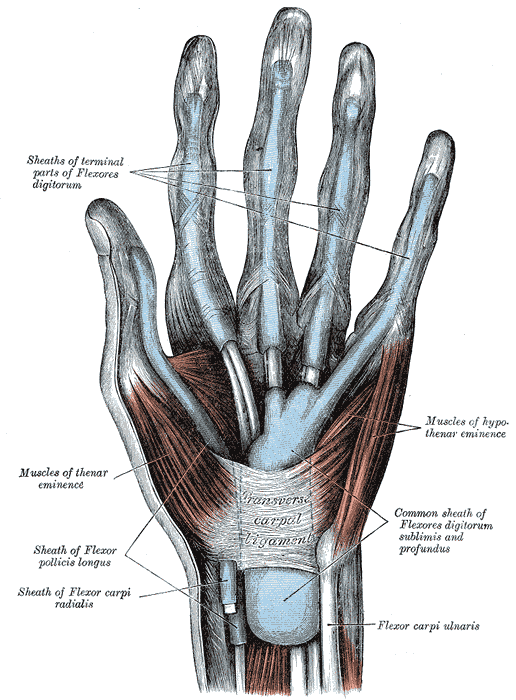
Muscles and Fascia of the Hand. Sheaths of terminal parts of flexores digitorum, muscles of thenar eminence, muscles of hypothenar eminence, sheath of Flexor pollicis longus, transverse carpal ligament, common sheath of flexors digitorum sublimis and profundus, and flexor carpi ulnaris.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Nguyen JD, Duong H. Anatomy, Shoulder and Upper Limb, Hand Hypothenar Eminence. StatPearls. 2023 Jan:(): [PubMed PMID: 31536229]
Vargas A, Chiapas-Gasca K, Hernández-Díaz C, Canoso JJ, Saavedra MÁ, Navarro-Zarza JE, Villaseñor-Ovies P, Kalish RA. Clinical anatomy of the hand. Reumatologia clinica. 2012 Dec-2013 Jan:8 Suppl 2():25-32. doi: 10.1016/j.reuma.2012.10.004. Epub 2012 Dec 6 [PubMed PMID: 23219083]
Moran CA. Anatomy of the hand. Physical therapy. 1989 Dec:69(12):1007-13 [PubMed PMID: 2685840]
Cole P, Kaufman Y, Hatef DA, Hollier LH Jr. Embryology of the hand and upper extremity. The Journal of craniofacial surgery. 2009 Jul:20(4):992-5. doi: 10.1097/SCS.0b013e3181abb18e. Epub [PubMed PMID: 19553860]
Zekavica A, Milisavljević M, Erić D, Ćurčić B, Popović S, Vitošević B, Dožić A, Štimec BV, Manojlović R. Vascular anatomy of the thenar eminence: its relevance to a pedicled or free thenar flap. Folia morphologica. 2017:76(2):232-238. doi: 10.5603/FM.a2016.0077. Epub 2016 Dec 27 [PubMed PMID: 28026846]
Duncan SF, Saracevic CE, Kakinoki R. Biomechanics of the hand. Hand clinics. 2013 Nov:29(4):483-92. doi: 10.1016/j.hcl.2013.08.003. Epub 2013 Oct 15 [PubMed PMID: 24209947]
Dydyk AM, Negrete G, Sarwan G, Cascella M. Median Nerve Injury. StatPearls. 2023 Jan:(): [PubMed PMID: 31971749]
Beran R. Paraesthesia and peripheral neuropathy. Australian family physician. 2015 Mar:44(3):92-5 [PubMed PMID: 25770571]
Earp B, Cefalu C, Blazar P. Thumb Metacarpophalangeal Joint Arthritis. The Journal of the American Academy of Orthopaedic Surgeons. 2019 Dec 1:27(23):e1029-e1039. doi: 10.5435/JAAOS-D-18-00683. Epub [PubMed PMID: 31356425]
Meals C, Meals R. Hand fractures: a review of current treatment strategies. The Journal of hand surgery. 2013 May:38(5):1021-31; quiz 1031. doi: 10.1016/j.jhsa.2013.02.017. Epub [PubMed PMID: 23618458]
Benny R, Shetty K. The split hand sign. Annals of Indian Academy of Neurology. 2012 Jul:15(3):175-6. doi: 10.4103/0972-2327.99700. Epub [PubMed PMID: 22919187]