Introduction
A sesamoid bone is a small bone commonly found embedded within a muscle or tendon near joint surfaces, existing as focal areas of ossification and functioning as a pulley to alleviate stress on that particular muscle or tendon. Unlike standard bones, which connect via joints, sesamoid bones connect to muscles via tendons. The word "sesamoid" derives from the Arabic word 'sesamum' translating to sesame, given that many sesamoid bones are small. Sesamoid bones are most commonly located in the foot, hand, and wrist; the largest and most well-known is the patella.[1] There are many sesamoid bones in a person, with up to 42 reportedly found in an individual.[2]
These bones are often formed in response to added strain to muscles and tendons but can also be normal variants, most commonly present in the hand.[3][4] Sesamoid bones relieve tension within muscles and tendons, allowing for increased weight-bearing and tolerance by redistributing forces throughout a muscle or tendon, thereby protecting them from significant strain and injury. While most sesamoid bones are small, these bones play a critical role in our body in leverage, decreasing overall friction and allowing for our body's unique biomechanics and distinct range of motion.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The body contains many sesamoid bones, often offering an added strength advantage to the muscles and supporting tendon stability. For example, the patella increases joint leverage and contributes to our knee's extensor properties. This unique mechanism allows for the knee's range of motion and increased weight-bearing activities. Injuries to the patella greatly reduce its leverage and extensor capabilities; these injuries commonly result from trauma and increased tension.[5]
Based on their positioning and attachment, sesamoid bones can be divided into two broad categories, type A and B. Bony surfaces are surrounded by cartilage and incorporated within the cavity, forming the synovium. Together a sesamoid bone and its relation to other tendons form a joint.
Type A sesamoid bones are adjacent to a joint, becoming a part of the joint capsule. Common examples of this type include the hallucis and pollicis sesamoids along with the patella, allowing for increased leverage. Type B sesamoid bones overlie a bony prominence and are separated by an underlying bursa. An example of a Type B sesamoid bone is the sesamoid of the peroneus (fibularis) longus tendon.[6] Both types of sesamoid bones serve unique functions and biomechanical properties.
Another type of sesamoid bone is the fibrocartilaginous sesamoid. This type of sesamoid allows the maintenance of tendon structure and provides immense flexibility from the fibrous component and elasticity via the cartilage tissue.[7][8]
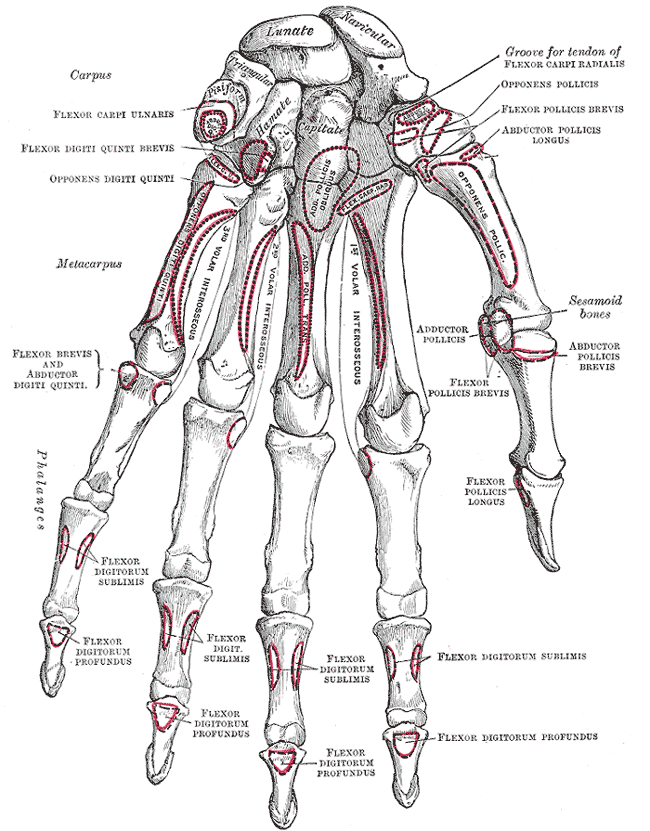
In the upper extremities, notable sesamoid bones are found in the hand and wrist. Most individuals usually have five sesamoid bones in each hand. Two sesamoid bones are located in the distal portions of the first metacarpal bones of the hand, more specifically within the tendons of the flexor pollicis brevis and adductor pollicis. A third sesamoid bone exists within the interphalangeal joint. In addition, the other two sesamoid bones are present in the distal portion of the second metacarpal bone and the distal portion of the fifth metacarpal joint.[4] In the wrist, the presence of the pisiform bone located within the tendon of the flexor carpi ulnaris has led to a debate about whether it exists as a sesamoid bone or possibly a vestigial bone.[9]
In the lower extremities, the patella is found in the knee and is the largest sesamoid bone. Other lower limb sesamoids that can be seen as normal variants in humans include the fabella (often near the lateral head of the gastrocnemius), cyamella (within the popliteus tendon), os peroneum (located within the peroneus longus tendon), and the hallux sesamoid pair (one on the medial and the lateral side of the first metatarsal bone of the foot).
Another sesamoid bone within the ear is the lenticular process of the incus, often known as the fourth ossicle of the middle ear.
Embryology
The formation of sesamoid bones is attributed to the body's natural growth and various stressors imposed on the body. Starting as cartilaginous nodules, most sesamoid bones undergo further endochondral ossification during the prepubertal years. Further calcification is evident during puberty, with sesamoid bones appearing much earlier in females. A lack of sesamoid bone formation often indicates a delay in puberty and can be useful in monitoring the progression of puberty. While most sesamoid bones seemingly develop in response to various stress factors, the patella is present in all humans. Its development plays a crucial role in the form and function of the lower extremities allowing for the study of sesamoid bone development.[10]
The patella is unique in its relatively larger size and stable presence in humans compared to other sesamoid bones. Development of the patella starts during the first trimester of gestation after the chondrification of the femur and tibia, with the early patella visible as a continuous band of fibrous tissue. As the patella develops inside the band of fibrous tissue, the embryological patella becomes chondrified and inserts into the quadriceps by the 9th week of gestation.[11]
As the embryo reaches 14 weeks of gestation, the patella is wholly cartilaginous and resembles the adult patella structure by 23 weeks of gestation. The patella continues its rapid growth rate until the end of the 2nd trimester, and then it grows at a similar rate as the rest of the growing fetus.[12] Like other sesamoid bones, ossification begins in the patella during childhood and continues into early adolescence. During the pubertal years, the patella becomes confluent with the quadriceps, stabilizing into the adult patella.[13]
Blood Supply and Lymphatics
The blood supply and lymphatics of any bone are vital to its nourishment and development. Given the variability in the development of most sesamoid bones, the blood supply and lymphatics primarily depend on the location of the specific bone and its development. These bones have limited blood supply and are susceptible to potential avascular necrosis, leading to complications.
However, the patella is an exception due to its significance, size, and consistent function in the human body. Its early development during gestation and critical role in supporting the lower extremity requires a rich blood supply. An extensive extraosseous and intraosseous network of blood vessels nourishes the patella.[14] A vascular anastomotic ring surrounds the patella with contributions from the genicular arteries (superior medial, lateral, descending, inferior medial, lateral, and anterior genicular) and the anterior tibial recurrent arteries forming the extraosseous network of blood supply. The intraosseous blood supply comprises two systems: the mid-patellar vessels, which enter the anterior surface, and the polar vessels, which enter the deep surface of the patella. Together the extraosseous and intraosseous vasculature ensure the rich blood supply of the patella.[15]
While the patella is unique among sesamoid bones, others, like the hallux sesamoids, can present with a varied blood supply. A study of 29 dissected human feet was analyzed, showing the medial plantar artery branching into the digital plantar arteries of the hallux before giving rise to the sesamoid arteries. The study concluded that the number of sesamoid arteries to the bone increased with increasing sesamoid bone size between different-sized feet.[16] This variation in anatomy proves critical in evaluating anomalies between different people and further understanding potential avascular necrosis in sesamoid bones.
Other vasculature of sesamoid bones includes the palmar metacarpal arteries that arise from the deep palmar arch supplying the first and second metacarpals. The pisiform receives its blood supply from the ulnar artery. The ossicular branch of the anterior tympanic artery supplies the lenticular process of the incus. In addition, the fabella receives its blood supply primarily from the articular external branches of the popliteal artery. Similarly, the cyamella receives its arterial supply from the medial inferior genicular branch of the popliteal artery. Most often, the os peroneum receives its blood supply from the peroneal artery and anterior tibial artery.
Nerves
A sesamoid bone's innervation depends on its anatomical location. For example, the patella has an extensive innervation, with different nerves accounting for the anterior, medial, and lateral aspects of the knee. Nerve roots L2 through L5 innervate the cutaneous portion of the anterior knee. Meanwhile, the nerve supply of the anteromedial aspect of the knee includes the genitofemoral, femoral, obturator, and saphenous nerves. The anterolateral aspect of the knee receives innervation from the lateral femoral and lateral sural cutaneous nerves.[17] Together these nerves provide an extensive innervation network to the patella for its unique biomechanical function.
Other sesamoid bones, like the hallux sesamoid, receive innervation from the plantar digital nerves. The proximity of nerves to sesamoid bones can create clinical complications. The pisiform is unique in that it also forms the Guyon canal, allowing the ulnar nerve to course through. Any fracture to the pisiform bone is associated with ulnar nerve compression and complications.[18] Similarly, a case of os peroneum fracture has been shown to cause sural nerve entrapment.[19]
The presence of the fabella bone near the gastrocnemius can lead to the common fibular nerve palsy, requiring a potential fabellectomy if symptoms persist despite conservative management.[20] Other sesamoid bones like the cyamella are rare, and their innervation has yet to be fully explored.
Muscles
Whereas bones are typically connected at joints, sesamoid bones are unique because they are not connected to other bones. Instead, they are found within muscles and are often connected through tendons. The patella's function and relation to the other muscles have been well studied and form the basis for discussing sesamoid bones with muscle groups.
The patella's unique position in the lower extremities allows it to act as a pivot point, allowing the quadriceps to bear increased loads with decreased friction.[21] Serving as a unique connection between the quadriceps tendon and the patellar ligament, the patella allows for flexion to the extension of the lower extremities. The quadriceps tendon can bear increased maximal forces many times the body weight of an average human. This flexed position requires more of the linking function. As the knee proceeds from flexion to extension, the patella shifts load-bearing to the patellofemoral and tendo-femoral connections.[22] Proceeding to full extension of the knee, the patella is the only extensor to contact the femur, creating a biomechanical advantage similar to a pulley.[23]
The vital connection between the quadriceps tendon and the patellar ligament via the patella allows for the knee's extensive and distinct range of motion by transferring forces. However, not all sesamoid bones serve this unique purpose. The fabella bone, a common sesamoid bone variant near the gastrocnemius and articulating with the lateral femoral epicondyle, often presents with complications like the fabella pain syndrome.[20]
Physiologic Variants
Sesamoid bones are common in humans, with some bones like the patella being present in everyone and vital to lower extremity function. The patella is an anomaly among sesamoid bones due to its consistent presence, size, and significance in humans. While the patella is present in all humans, it has been shown that it fails to develop entirely in paralyzed embryos due to a lack of mechanical stress, indicating the role that both genetics and concurrent biomechanical stress play in developing a sesamoid bone.
There are also lesser-known sesamoid bones that exist as variants and can develop spontaneously due to extrinsic and intrinsic factors. Mechanical forces, biomechanics, and skeletal geometry all contribute to the development of sesamoid bones. Intrinsic genetic factors also play a crucial role. One study noted the frequency of the appearance of the fabella sesamoid bone and the os peroneum sesamoid bone together in individuals. These sesamoid bones are smaller and variable in occurrence. Inconclusive evidence also remains on various factors affecting sesamoid bone variant development. Genetics and mechanical factors play equally important roles in developing mainstay sesamoid bones like the patella and variants such as the fabella and the os peroneum.
Even within the hand, there is variety in sesamoid bone development between individuals. Two sesamoid bones were seen at the thumb metacarpophalangeal (MCP) joints, but variations in the shape and fusion lines of the sesamoid bones were seen in 30% of the individuals studied. The thumb MCP joints consistently showed two sesamoid bones compared to the joints of the other fingers. Similarly, 60% of individuals had an index finger MCP sesamoid bone, and 59% had the 5th finger MCP sesamoid bone present.[24] Sesamoid bones vary in humans through their presence, number, size, and shape, with both external and internal contributing factors.
Surgical Considerations
When performing surgeries, it is important to be aware of anatomical variations of sesamoid bones. While surgeries involving the patella, such as total knee arthroplasty, are commonplace, medical imaging plays a critical role in the pre-operative evaluation, surgical technique, and postoperative follow-up.[25]
Special consideration should be taken to cut medial to the patella, reflecting the patella laterally to reach the patellofemoral joint. Similarly, surgeries involving the various ligaments of the knee also utilize imaging to visualize multiple structures within the knee. The patella remains the exception in the study of sesamoid bones due to its consistent presence and significance.
Sesamoid excision has been studied in athletes with a sesamoid bone injury and whether an athlete's ability was affected because of this. The study showed that about 80% of athletes who underwent a sesamoidectomy could return to sports in five months.[26]
Another commonly studied sesamoid surgery involves the hallux sesamoid. A successful union of a hallux sesamoid fracture is challenging, and a sesamoidectomy was explored for the potential to provide better outcomes. The study showed that sesamoidectomy provided better pain relief and allowed a return to normal activities within 12 weeks.[27] Often, avascular necrosis of the sesamoid can be managed medically, but ultimately a sesamoid excision results in complete relief of the pain and greater patient satisfaction.[28]
Whereas a sesamoid bone often posed no significant discomfort or pain, any fracture or injury to a sesamoid bone greatly benefited from excision instead of a union repair.
An unexpected sesamoid bone poses a unique challenge in surgeries involving that particular area if adequate imaging is not readily available in an emergent situation. Surgeons must be aware of potential anatomical variants and their interactions with the local anatomy if operating in an area with high suspicion of a sesamoid bone. Special consideration must be taken into account for an unexpected sesamoid bone if conventional surgical techniques and approaches do not allow it.
Clinical Significance
From its initial development during gestation to its day-to-day function within the body, sesamoid bones are clinically crucial in our everyday biomechanics and range of motion. Consistent, stable sesamoid bones like the patella allow the lower extremities to offload forces for our ambulation and support greater weight. Without the patella, instability of the knee joint, reduced range of motion, and difficulty straightening the leg would be common problems. This adaptation has allowed humans to develop over many millennia.
While the patella remains a consistent example throughout the body, some adaptations of sesamoid bones have been shown in keyboard musicians.[29] The study showed that musicians tended to have greater sesamoid bone volume within the hand; an unusually shaped sesamoid is more prevalent in female musicians. A musician's repetitive use of their hands and the subsequent increase in the sesamoid bone volume show that the body constantly adapts to the various stressors faced. Sesamoid bones play a crucial role in the body, allowing for everyday actions many take for granted. Studies continue to explore the many other sesamoid bones and their role in the human body.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)

Anatomy of the Plantar Surface of Right Foot Bones. Anatomy of calcaneus, abductor hallucis, quadratus plantar, abductor digiti quinti, talus, navicular, tibial posterior, cuboid, tubercle of navicular, tibialis posterior, cuneiform, flexor digitalis quinti, flexor brevis, abductor digiti quinti, flexor digitorum brevis, flexor digitorum longus, and sesamoid.
Gray's Anatomy
(Click Image to Enlarge)
(Click Image to Enlarge)
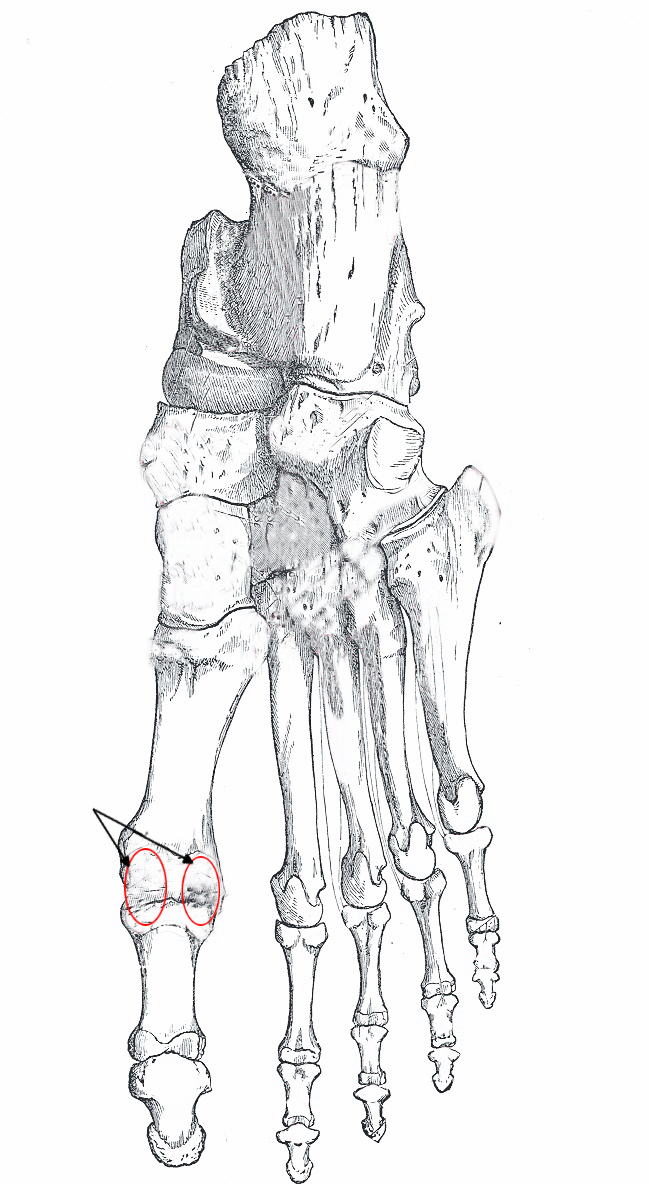
Right, Foot, Bones, Plantar Surface, Calcaneus, Abductor Hallucis, Quadratus Plantar, Abductor Digiti Quinti, Talus, Navicular, Tibial Posterior, Cuboid, Tubercle of navicular, Tibialis Posterior, Cuneiform, Flexor Digitalis Quinti, Flexor Brevis, Abductor Digiti Quinti, Flexor Digitorum Brevis, Flexor Digitorum Longus, Sesamoid,
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Fox AJ, Wanivenhaus F, Rodeo SA. The basic science of the patella: structure, composition, and function. The journal of knee surgery. 2012 May:25(2):127-41 [PubMed PMID: 22928430]
Sarin VK, Erickson GM, Giori NJ, Bergman AG, Carter DR. Coincident development of sesamoid bones and clues to their evolution. The Anatomical record. 1999 Oct 15:257(5):174-80 [PubMed PMID: 10597342]
Level 3 (low-level) evidenceSummers A. Accessory ossicles and sesamoid bones: recognition and treatment. Emergency nurse : the journal of the RCN Accident and Emergency Nursing Association. 2015 Mar:22(10):27-32. doi: 10.7748/en.22.10.27.e1404. Epub [PubMed PMID: 25746889]
Wood VE. The sesamoid bones of the hand and their pathology. Journal of hand surgery (Edinburgh, Scotland). 1984 Oct:9(3):261-4 [PubMed PMID: 6512360]
Level 3 (low-level) evidenceMelvin JS, Mehta S. Patellar fractures in adults. The Journal of the American Academy of Orthopaedic Surgeons. 2011 Apr:19(4):198-207 [PubMed PMID: 21464213]
Hallinan JTPD, Wang W, Pathria MN, Smitaman E, Huang BK. The peroneus longus muscle and tendon: a review of its anatomy and pathology. Skeletal radiology. 2019 Sep:48(9):1329-1344. doi: 10.1007/s00256-019-3168-9. Epub 2019 Feb 15 [PubMed PMID: 30770941]
Benjamin M, Ralphs JR. Fibrocartilage in tendons and ligaments--an adaptation to compressive load. Journal of anatomy. 1998 Nov:193 ( Pt 4)(Pt 4):481-94 [PubMed PMID: 10029181]
Delfaut EM, Demondion X, Bieganski A, Cotten H, Mestdagh H, Cotten A. The fibrocartilaginous sesamoid: a cause of size and signal variation in the normal distal posterior tibial tendon. European radiology. 2003 Dec:13(12):2642-9 [PubMed PMID: 14531012]
May O. [The pisiform bone: sesamoid or carpal bone?]. Annales de chirurgie de la main et du membre superieur : organe officiel des societes de chirurgie de la main = Annals of hand and upper limb surgery. 1996:15(4):265-71 [PubMed PMID: 9026058]
Level 3 (low-level) evidenceAbushhiwa MH, Alrtib AM, Elmeshreghi TN, Abdunnabi MA, Shmela ME, Bennour EM. Patellar luxation in Hejazi goats. Open veterinary journal. 2021 Apr-Jun:11(2):295-300. doi: 10.5455/OVJ.2021.v11.i2.14. Epub 2021 Jun 18 [PubMed PMID: 34307087]
Gardner E, O'Rahilly R. The early development of the knee joint in staged human embryos. Journal of anatomy. 1968 Jan:102(Pt 2):289-99 [PubMed PMID: 5643844]
Level 3 (low-level) evidenceWalmsley R. The development of the patella. Journal of anatomy. 1940 Apr:74(Pt 3):360-368.3 [PubMed PMID: 17104819]
Ogden JA. Radiology of postnatal skeletal development. X. Patella and tibial tuberosity. Skeletal radiology. 1984:11(4):246-57 [PubMed PMID: 6729496]
Shim SS, Leung G. Blood supply of the knee joint. A microangiographic study in children and adults. Clinical orthopaedics and related research. 1986 Jul:(208):119-25 [PubMed PMID: 3522019]
CROCK HV. The arterial supply and venous drainage of the bones of the human knee joint. The Anatomical record. 1962 Nov:144():199-217 [PubMed PMID: 14023913]
Pretterklieber ML, Wanivenhaus A. The arterial supply of the sesamoid bones of the hallux: the course and source of the nutrient arteries as an anatomical basis for surgical approaches to the great toe. Foot & ankle. 1992 Jan:13(1):27-31 [PubMed PMID: 1577338]
Horner G, Dellon AL. Innervation of the human knee joint and implications for surgery. Clinical orthopaedics and related research. 1994 Apr:(301):221-6 [PubMed PMID: 8156678]
Chang MK, Yap RTJ. Acute ulnar nerve compression associated with pisiform fracture - a case report and literature review. Case reports in plastic surgery & hand surgery. 2019:6(1):1-6. doi: 10.1080/23320885.2018.1522959. Epub 2019 Jan 28 [PubMed PMID: 32550255]
Level 3 (low-level) evidencePerlman MD. Os peroneum fracture with sural nerve entrapment neuritis. The Journal of foot surgery. 1990 Mar-Apr:29(2):119-21 [PubMed PMID: 2338470]
Level 3 (low-level) evidenceDalip D, Iwanaga J, Oskouian RJ, Tubbs RS. A Comprehensive Review of the Fabella Bone. Cureus. 2018 Jun 5:10(6):e2736. doi: 10.7759/cureus.2736. Epub 2018 Jun 5 [PubMed PMID: 30087812]
Kwak SD, Colman WW, Ateshian GA, Grelsamer RP, Henry JH, Mow VC. Anatomy of the human patellofemoral joint articular cartilage: surface curvature analysis. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 1997 May:15(3):468-72 [PubMed PMID: 9246097]
Goodfellow J, Hungerford DS, Zindel M. Patello-femoral joint mechanics and pathology. 1. Functional anatomy of the patello-femoral joint. The Journal of bone and joint surgery. British volume. 1976 Aug:58(3):287-90 [PubMed PMID: 956243]
Wendt PP, Johnson RP. A study of quadriceps excursion, torque, and the effect of patellectomy on cadaver knees. The Journal of bone and joint surgery. American volume. 1985 Jun:67(5):726-32 [PubMed PMID: 3997925]
Chen W, Cheng J, Sun R, Zhang Z, Zhu Y, Ipaktchi K, Zhang Y. Prevalence and variation of sesamoid bones in the hand: a multi-center radiographic study. International journal of clinical and experimental medicine. 2015:8(7):11721-6 [PubMed PMID: 26380010]
Scott AM. Total Knee Replacement and Imaging. Radiologic technology. 2015 Sep-Oct:87(1):65-86 [PubMed PMID: 26377268]
Dean RS, Coetzee JC, McGaver RS, Fritz JE, Nilsson LJ. Functional Outcome of Sesamoid Excision in Athletes. The American journal of sports medicine. 2020 Dec:48(14):3603-3609. doi: 10.1177/0363546520962518. Epub 2020 Oct 23 [PubMed PMID: 33095661]
Bichara DA, Henn RF 3rd, Theodore GH. Sesamoidectomy for hallux sesamoid fractures. Foot & ankle international. 2012 Sep:33(9):704-6 [PubMed PMID: 22995255]
Bartosiak K, McCormick JJ. Avascular Necrosis of the Sesamoids. Foot and ankle clinics. 2019 Mar:24(1):57-67. doi: 10.1016/j.fcl.2018.09.004. Epub [PubMed PMID: 30685013]
Dąbrowski KP, Stankiewicz-Jóźwicka H, Kowalczyk A, Wróblewski J, Ciszek B. Morphology of sesamoid bones in keyboard musicians. Folia morphologica. 2021:80(2):410-414. doi: 10.5603/FM.a2020.0066. Epub 2020 Jul 8 [PubMed PMID: 32639576]