Introduction
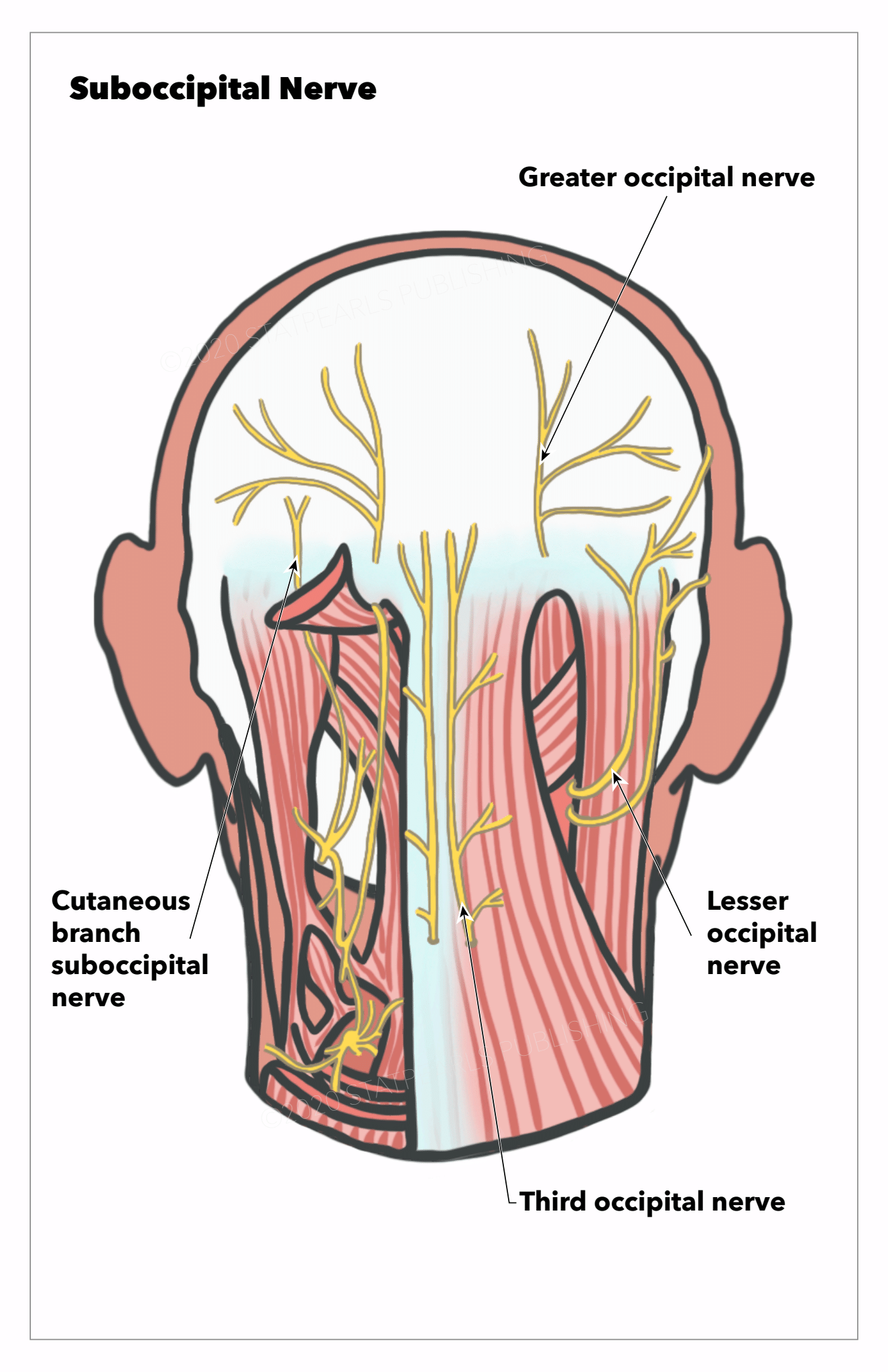
The suboccipital muscles are a group of 4 muscles located in the posterior region of the neck, inferior to the occipital bone. These 4 muscles are the rectus capitis posterior major, rectus capitis posterior minor, obliquus capitis superior, and obliquus capitis inferior (see Image. Deep Posterior Neck Muscles). The muscles serve as postural support of the head and neck and allow neck extension and rotation movements. The muscles are innervated by the suboccipital nerve, which is formed by the dorsal ramus of C1. Three of the 4 muscles form the suboccipital triangle. This common anatomic landmark localizes the vertebral artery and suboccipital nerve (see Image. Nerves of the Posterior Head and Neck Region). This landmark is particularly important to surgeons operating in the posterior cervical region to avoid life-threatening bleeding.
The vertebral artery takes a torturous course behind the suboccipital muscles while giving off branches that supply the suboccipital muscles. Clinically, the suboccipital muscles are important because of their close relationship to the vertebral artery and surgical access to the posterior cranial fossa. Various cranial pathologies can be accessed by a suboccipital surgical approach that requires knowledge of the posterior cervical region. The 4 muscles have been implicated in the pathogenesis of cervicogenic headaches due to their connections with the dura mater.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The suboccipital muscles are a group of 4 muscles located inferior to the external occipital prominence of the skull. The 4 muscles are the rectus capitis posterior major, rectus capitis posterior minor, obliquus capitis inferior, and obliquus capitis superior.[1]
Rectus Capitis Posterior Major
- Origin: Spinous process of C2 vertebrae
- Insertion: Inferior nuchal line of the occipital bone
- Action: Extension of the neck, ipsilateral rotation of the head
Rectus Capitis Posterior Minor
- Origin: Posterior tubercle of C1 vertebrae
- Insertion: Inferior nuchal line of the occipital bone
- Action: Extension of the neck, ipsilateral rotation of the head
Obliquus Capitis Superior
- Origin: Transverse process of C1 vertebrae
- Insertion: Portion of the occipital bone between nuchal lines
- Action: Extension and lateral flexion
Obliquus Capitis Inferior
- Origin: Spinous process of C2 vertebrae
- Insertion: Transverse process of C1 vertebrae
- Action: Ipsilateral rotation of the head
The innervation of all the suboccipital muscles is the suboccipital nerve, which is the dorsal ramus of the C1 spinal nerve.
Suboccipital Triangle
- The suboccipital triangle is an anatomic landmark involving the suboccipital muscles and allows for the localization of the vertebral artery and the suboccipital nerve.
- Rectus capitis posterior major forms the superomedial border
- Obliquus capitis superior forms the superolateral border
- Obliquus capitis inferior forms the inferolateral border
- The posterior atlantooccipital membrane forms the floor of the triangle
- The roof of the triangle is formed by the semispinalis capitis muscle[2][3]
- The contents of the suboccipital triangle are the suboccipital nerve (dorsal ramus of C1), the third part of the vertebral artery (V3), and the suboccipital venous plexus.
Directly posterior (or superficial) to the suboccipital muscles is the semispinalis capitis. Further posterior to these muscles include the splenius, sternocleidomastoid, and trapezius. While the suboccipital muscles function as postural muscles, they also allow for head movement.[1][2]
Embryology
The suboccipital muscles, similar to all striated and smooth muscles, are derived from the mesoderm. With attachments to the skull base, there is a complex interaction between the mesoderm and the occipital sclerotomes that form the occipital bone. During embryologic development, derangements can lead to anatomic variations in the suboccipital muscles.[4][5][6][7]
Blood Supply and Lymphatics
The suboccipital muscles cover the vertebral artery as it enters the transverse process of C1. The vertebral artery is divided into 4 segments, separated based on anatomical positioning within the body. The origin of the vertebral artery is from the subclavian arteries, after which it ascends superiorly alongside the cervical spinal vertebrae until, at the level of C6, it traverses the foramina of the remaining vertebrae until C2, where it exits.[8] At this point, the portion of the vertebral artery behind the suboccipital muscles is labeled the third segment (V3). V3, or the suboccipital segment, travels from the transverse process of C2 through the transverse process of C1 and into the dura mater. During this course, the V3 segment gives off a muscular artery that supplies the suboccipital muscles. The suboccipital venous plexus is the main venous structure surrounding and draining the suboccipital muscles. These surrounding veins are located posterior to the suboccipital muscles and anastomose with a venous sinus surrounding the V3 segment of the vertebral artery.[9]
Nerves
The suboccipital muscles are innervated by the suboccipital nerve, which arises from the dorsal rami of C1. Before the formation of the rami, rootlets emerge from the spinal cord at the level of C1. Ventral and dorsal rootlets combine to form ventral and dorsal rami. The dorsal or posterior ramus exits through the posterior atlanto-occipital membrane before branching into different segments to innervate the suboccipital muscles and the semispinalis capitis.[9][10]
Physiologic Variants
Case reports have found variants of the suboccipital muscles. A third rectus capitis muscle was found in the suboccipital region in 1 patient.[6] In another instance, there was a unilateral absence of rectus capitis posterior minor muscle replaced with 2 rectus capitis posterior major muscles.[7] Both of these variants may provide further insight and explanations for the development of cervicogenic headaches.
Surgical Considerations
A posterior suboccipital approach may be used when considering surgery for various diseases involving the cerebellum, spinal cord, or atlantoaxial joint. Understanding the relationship between neurovascular structures within the suboccipital region is crucial before surgery to avoid life-threatening injury. The suboccipital muscles form a suboccipital triangle, which can be used as a consistent marker for the location of the vertebral artery and suboccipital nerve. The rectus outlines the suboccipital triangle capitis posterior major, obliquus capitis superior, and obliquus capitis superior. The third portion of the vertebral artery courses horizontally as it moves throughout the suboccipital triangle. Other landmarks that can be utilized during a posterior surgical approach include the spinous process of C2, the posterior arch of C1, and the transverse processes of C1/C2.[11] The suboccipital approach has been used for multiple neurologic and vascular pathologies.[12][13]
The midline suboccipital approach is a versatile neurosurgical technique. It is commonly used within pediatric neurosurgery as an approach to posterior fossa tumors. Still, it can also be employed to access Chiari malformations, vascular lesions, tumors of the foramen magnum, and those exiting the brainstem, such as hypoglossal nerve sheath tumors.[14][15] For the procedure, the patient is generally positioned in a prone position but may also be in a semi-sitting position.[14] The inion - a small rounded protuberance in the midline of the inferior part of the occipital bone) is used as a landmark for the superior part of the incision, which starts 2 or 3 cm above the inion and extends in the midline inferiorly to the spinous process of the C2 vertebra.[16] After the skin and subcutaneous tissue have been incised, the suboccipital muscles are in the operative field, either side of the midline, and are carefully disconnected from the inion. Thereafter, burr holes can be placed to expose, taking care at every point to avoid damage to the transverse sinus. The posterior arch of the C1 vertebra can also be removed, and an extension of the foramen magnum with bony dissection can be used to achieve further exposure as appropriate to the pathology being treated.[15]
Clinical Significance
The suboccipital muscles form an anatomic landmark of particular importance to surgeons operating within the posterior cervical spine or cranial fossa region. The suboccipital triangle forms a distinct area where surgeons can recognize the vertebral artery and its position within the posterior cervical region. The close relationship between the suboccipital muscles and the vertebral artery may be relevant in patients with significant atherosclerosis. Contraction of the suboccipital muscles may lead to minor artery compression, further reducing blood flow. The decreased blood flow can lead to symptoms of light-headedness and dizziness. Additionally, the suboccipital muscles can be strained by constant movement or injury. This may lead to headaches or neck pain that can be relieved through physical therapy and pain control.
Cervicogenic Headaches
Cervicogenic headaches initially present as unilateral neck pain and spread to the head. The pain becomes worse with movement or palpation of the neck. This type of headache can commonly be mistaken for migraines or tension headaches. The pain may radiate to other areas, including the shoulder and arm. The suboccipital muscles have been investigated as a potential cause of cervicogenic headaches. In 1 study, the suboccipital muscles were found to have increased tone and stiffness compared to healthy controls.[17] The suboccipital muscles have been noted to have connections with the dura mater, a connection labeled the “myodural bridge.” It has been hypothesized that tension produced by the suboccipital muscles may directly lead to tension within the dura, which can lead to characteristic cervicogenic headache pain.[18] Other studies have implicated the C1-C3 nerves as potential causes of cervicogenic headaches.[19] Treatment of these headaches involves physical therapy. If symptoms persist, other therapies include steroid injections for severe symptoms.
Post Dural Puncture Headache (PDPH)
Pregnant women at full term who are undergoing cesarean section anesthesia for the surgery, and this is most commonly achieved by a regional technique, by administering anesthetic drugs into intradural space, alone or in combination with ongoing drug administration in the epidural space.[20] Owing to the puncture of the dura and likely cerebrospinal fluid (CSF) leak occurring secondary to this, patients can present following this with postural headaches, sometimes accompanied by neck stiffness, and more rarely with photophobia, tinnitus, or vomiting.[21][22] Although the exact cause is not completely understood, CSF leak following puncture is the more likely mechanism. Increased rates have been reported among women with a higher body mass index. Furthermore, the technical expertise of the practitioner performing the procedure and the overall number of attempts required before accessing the CSF space successfully are related to PDPH incidence. Overall, the estimated incidence is 25% following spinal anesthesia.[23]
The management of post-dural puncture headaches has been a topic of debate, with current practice favoring the placement of an epidural blood patch as a treatment for the presumed pathological mechanism of CSF leak following the puncture [21]. However, a randomized control trial evaluated the effect of suboccipital muscle injection with steroids and local anesthetic as a therapeutic intervention for PDPH. They randomized patients with PDPH to receive either a sham intramuscular suboccipital injection of normal saline or an intramuscular suboccipital injection of a combination of dexamethasone and lidocaine.[24] The results demonstrated reduced headache scores and reduced ongoing reliance on oral analgesia within the treatment arm of the trial, supporting suboccipital intramuscular injection with the steroid-anesthetic combination as a treatment for PDPH.
Suboccipital Muscle Trauma
Owing to their function as supporters and enablers of head and neck movements, the suboccipital muscles are vulnerable to strain and spasms in trauma, for example, whiplash in car accidents or other rapid deceleration injuries.[25] Ongoing pain following such injuries can result from both suboccipital muscular spasms and damage to the suboccipital nerve. Specifically, it has been hypothesized that injury to the rectus capitis posterior minor muscle is implicated most significantly in this situation, as cadaveric dissections found dorsal spinal dura mater in the region of the atlantooccipital junction. Therefore, a tear or rupture of the muscle following trauma could be a conceivable mechanism for cervicogenic headaches that manifest more broadly as regional pain syndromes.[26] Following suboccipital muscle trauma such as strain or spasm, the treatment is generally conservative and supportive, in line with the treatment of muscular strains elsewhere in the body. Rest, guided physiotherapy exercises, massage, NSAIDs, and acupuncture are all common treatments.[27][28][29]
Media
(Click Image to Enlarge)
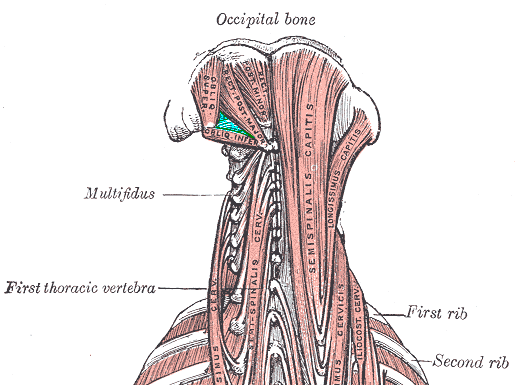
Deep Posterior Neck Muscles. This illustration shows the muscles bordering the suboccipital triangle: the rectus capitis posterior major (medial), obliquus capitis superior (superolateral), and obliquus capitis inferior (inferolateral). Other muscles in this image include the rectus capitis posterior minor, multifidus, semispinalis capitis and cervicis, longissimus capitis and cervicis, and iliocostalis cervicis. Labeled bony structures include the 1st thoracic vertebra and first and second ribs.
Medical Gallery of Mikael Häggström 2014, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
La Rocca G, Altieri R, Ricciardi L, Olivi A, Della Pepa GM. Anatomical study of occipital triangles: the 'inferior' suboccipital triangle, a useful vertebral artery landmark for safe postero-lateral skull base surgery. Acta neurochirurgica. 2017 Oct:159(10):1887-1891. doi: 10.1007/s00701-017-3300-3. Epub 2017 Aug 22 [PubMed PMID: 28828558]
Gutierrez S, Huynh T, Iwanaga J, Dumont AS, Bui CJ, Tubbs RS. A Review of the History, Anatomy, and Development of the C1 Spinal Nerve. World neurosurgery. 2020 Mar:135():352-356. doi: 10.1016/j.wneu.2019.12.024. Epub 2019 Dec 12 [PubMed PMID: 31838236]
Graefe SB, Jozsa F. Neuroanatomy, Suboccipital Nerve. StatPearls. 2024 Jan:(): [PubMed PMID: 32310593]
Maschner A, Krück S, Draga M, Pröls F, Scaal M. Developmental dynamics of occipital and cervical somites. Journal of anatomy. 2016 Nov:229(5):601-609. doi: 10.1111/joa.12516. Epub 2016 Jul 6 [PubMed PMID: 27380812]
Loukas M, Tubbs RS. An accessory muscle within the suboccipital triangle. Clinical anatomy (New York, N.Y.). 2007 Nov:20(8):962-3 [PubMed PMID: 17415745]
Level 3 (low-level) evidenceTagil SM, Ozçakar L, Bozkurt MC. Insight into understanding the anatomical and clinical aspects of supernumerary rectus capitis posterior muscles. Clinical anatomy (New York, N.Y.). 2005 Jul:18(5):373-5 [PubMed PMID: 15971221]
Level 3 (low-level) evidenceNayak SR, Swamy R, Krishnamurthy A, Dasgupta H. Bilateral anomaly of rectus capitis posterior muscles in the suboccipital triangle and its clinical implication. La Clinica terapeutica. 2011:162(4):355-6 [PubMed PMID: 21912824]
Level 3 (low-level) evidenceEskander MS, Drew JM, Aubin ME, Marvin J, Franklin PD, Eck JC, Patel N, Boyle K, Connolly PJ. Vertebral artery anatomy: a review of two hundred fifty magnetic resonance imaging scans. Spine. 2010 Nov 1:35(23):2035-40. doi: 10.1097/BRS.0b013e3181c9f3d4. Epub [PubMed PMID: 20938397]
Level 2 (mid-level) evidenceBerguer R. Suboccipital approach to the distal vertebral artery. Journal of vascular surgery. 1999 Aug:30(2):344-9 [PubMed PMID: 10436455]
Tubbs RS, Loukas M, Slappey JB, Shoja MM, Oakes WJ, Salter EG. Clinical anatomy of the C1 dorsal root, ganglion, and ramus: a review and anatomical study. Clinical anatomy (New York, N.Y.). 2007 Aug:20(6):624-7 [PubMed PMID: 17330847]
Jhawar SS, Nunez M, Pacca P, Voscoboinik DS, Truong H. Craniovertebral junction 360°: A combined microscopic and endoscopic anatomical study. Journal of craniovertebral junction & spine. 2016 Oct-Dec:7(4):204-216 [PubMed PMID: 27891029]
Mingdong W, Fernandez-Miranda JC, Mathias RN, Wang E, Gardner P, Wang H. Fully Endoscopic Minimally Invasive Transrectus Capitis Posterior Muscle Triangle Approach to the Posterolateral Condyle and Jugular Tubercle. Journal of neurological surgery. Part B, Skull base. 2017 Oct:78(5):359-370. doi: 10.1055/s-0037-1601369. Epub 2017 Apr 18 [PubMed PMID: 28875113]
Nonaka M, Yagi K, Abe H, Miki K, Morishita T, Iwaasa M, Inoue T. Endoscopic surgery via a combined frontal and suboccipital approach for cerebellar hemorrhage. Surgical neurology international. 2018:9():68. doi: 10.4103/sni.sni_346_17. Epub 2018 Apr 5 [PubMed PMID: 29721347]
Bocchetti A, Cioffi V, Gragnaniello C, de Falco R. Versatility of sub-occipital approach for foramen magnum meningiomas: a single centre experience. Journal of spine surgery (Hong Kong). 2017 Sep:3(3):411-418. doi: 10.21037/jss.2017.09.03. Epub [PubMed PMID: 29057351]
Tatagiba M, Koerbel A, Roser F. The midline suboccipital subtonsillar approach to the hypoglossal canal: surgical anatomy and clinical application. Acta neurochirurgica. 2006 Sep:148(9):965-9 [PubMed PMID: 16817032]
Level 3 (low-level) evidenceNaderi S, Usal C, Tural AN, Korman E, Mertol T, Arda MN. Morphologic and radiologic anatomy of the occipital bone. Journal of spinal disorders. 2001 Dec:14(6):500-3 [PubMed PMID: 11723399]
Park SK, Yang DJ, Kim JH, Heo JW, Uhm YH, Yoon JH. Analysis of mechanical properties of cervical muscles in patients with cervicogenic headache. Journal of physical therapy science. 2017 Feb:29(2):332-335. doi: 10.1589/jpts.29.332. Epub 2017 Feb 24 [PubMed PMID: 28265168]
Sillevis R, Hogg R. Anatomy and clinical relevance of sub occipital soft tissue connections with the dura mater in the upper cervical spine. PeerJ. 2020:8():e9716. doi: 10.7717/peerj.9716. Epub 2020 Aug 10 [PubMed PMID: 32864219]
Bogduk N. The anatomical basis for cervicogenic headache. Journal of manipulative and physiological therapeutics. 1992 Jan:15(1):67-70 [PubMed PMID: 1740655]
Sadashivaiah J, Wilson R, McLure H, Lyons G. Double-space combined spinal-epidural technique for elective caesarean section: a review of 10 years' experience in a UK teaching maternity unit. International journal of obstetric anesthesia. 2010 Apr:19(2):183-7. doi: 10.1016/j.ijoa.2009.06.005. Epub 2009 Nov 28 [PubMed PMID: 19945843]
Malhotra S. All patients with a postdural puncture headache should receive an epidural blood patch. International journal of obstetric anesthesia. 2014 May:23(2):168-70. doi: 10.1016/j.ijoa.2014.01.001. Epub 2014 Jan 18 [PubMed PMID: 24656528]
Thew M, Paech MJ. Management of postdural puncture headache in the obstetric patient. Current opinion in anaesthesiology. 2008 Jun:21(3):288-92. doi: 10.1097/ACO.0b013e3282f8e21a. Epub [PubMed PMID: 18458543]
Level 3 (low-level) evidenceGirma T, Mergia G, Tadesse M, Assen S. Incidence and associated factors of post dural puncture headache in cesarean section done under spinal anesthesia 2021 institutional based prospective single-armed cohort study. Annals of medicine and surgery (2012). 2022 Jun:78():103729. doi: 10.1016/j.amsu.2022.103729. Epub 2022 May 7 [PubMed PMID: 35600186]
Abdelraouf M, Salah M, Waheb M, Elshall A. Suboccipital Muscles Injection for Management of Post-Dural Puncture Headache After Cesarean Delivery: A Randomized-Controlled Trial. Open access Macedonian journal of medical sciences. 2019 Feb 28:7(4):549-552. doi: 10.3889/oamjms.2019.105. Epub 2019 Feb 19 [PubMed PMID: 30894910]
Level 1 (high-level) evidenceFakhran S, Qu C, Alhilali LM. Effect of the Suboccipital Musculature on Symptom Severity and Recovery after Mild Traumatic Brain Injury. AJNR. American journal of neuroradiology. 2016 Aug:37(8):1556-60. doi: 10.3174/ajnr.A4730. Epub 2016 Mar 24 [PubMed PMID: 27012296]
Hack GD, Koritzer RT, Robinson WL, Hallgren RC, Greenman PE. Anatomic relation between the rectus capitis posterior minor muscle and the dura mater. Spine. 1995 Dec 1:20(23):2484-6 [PubMed PMID: 8610241]
Taylor JR, Finch PM. Neck sprain. Australian family physician. 1993 Sep:22(9):1623-5, 1627, 1629 [PubMed PMID: 8240126]
Moraska AF, Schmiege SJ, Mann JD, Butryn N, Krutsch JP. Responsiveness of Myofascial Trigger Points to Single and Multiple Trigger Point Release Massages: A Randomized, Placebo Controlled Trial. American journal of physical medicine & rehabilitation. 2017 Sep:96(9):639-645. doi: 10.1097/PHM.0000000000000728. Epub [PubMed PMID: 28248690]
Level 1 (high-level) evidenceCohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clinic proceedings. 2015 Feb:90(2):284-99. doi: 10.1016/j.mayocp.2014.09.008. Epub [PubMed PMID: 25659245]