Introduction
Community-acquired pneumonia is a leading cause of hospitalization and mortality and incurs significant healthcare costs. As disease presentation varies from a mild illness that can be managed as an outpatient to a severe illness requiring treatment in the intensive care unit, diagnosing early and determining the appropriate level of care is important for improving outcomes.[1][2][3][4][5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Many pathogens cause community-acquired pneumonia, including bacteria, viruses, and fungi.[6] Common bacterial pathogens can be classified as:
- Gram-positive agents such as Streptococcus pneumoniae, Staphylococcus aureus, group A streptococci, and other streptococci
- Gram-negative agents such as Haemophilus influenzae, Moraxella catarrhalis, and Enterobacteriaceae
- Atypical agents such as Legionella, Mycoplasma, Chlamydia pneumoniae, and Chlamydia psittaci [7]
Among viruses, rhinovirus, influenza, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and other respiratory viruses (parainfluenza, respiratory syncytial virus, human metapneumovirus, etc) have become increasingly detected as pathogens based on molecular detection methods. Worldwide, S pneumoniae and H influenzae are still the leading causes of acute bacterial pneumonia (see Image. Mycobacterium Avium-Intracellulare Pneumonia). The most recent population-based active surveillance in the United States identified that human rhinovirus, influenza virus, and S pneumoniae were the most common pathogens.[8]
Epidemiology
The estimated worldwide incidence of community-acquired pneumonia varies between 1.5 to 14 cases per 1000 person-years and is affected by geography, season, and population characteristics.[5] In the US the annual incidence is 24.8 cases per 10,000 adults, with higher rates as age increases. Pneumonia is the eighth leading cause of death and first among infectious causes of death. The mortality rate is as high as 23% for patients admitted to the intensive care unit for severe pneumonia.
All patients with comorbid illness are considered at risk for pneumonia, but specific risk factors exist for particular pathogens. Drug-resistant pneumococci are more likely in:
- Those older than 65
- Children in daycare centers
- Those who have taken beta-lactam antibiotics in the previous 90 days
- Individuals with alcohol use disorder, chronic medical conditions, and immune suppression
Pseudomonas pneumonia is more likely in those with:
- Bronchiectasis
- Malnutrition
- Corticosteroid therapy
- Antibiotic intake for greater than 7 days in the preceding month
Other etiological clues from geographic regions include the following:
- Coccidioidomycosis in the Southwestern US
- Blastomycosis or histoplasmosis in the states of the Ohio River valley bird exposures for Chlamydia psittaci
- Contact with flea-infested or infected rodents or rabbits during outside activities such as lawn mowing in the Northeast US (Martha's Vineyard, Cape Cod, etc) for tularemia pneumonia
Pathophysiology
Pathogens initially colonize the pharynx, followed by micro-aspiration, which is the mechanism of entry into the lower respiratory tract. Once there, the pathogen induces the host's pulmonary defense. If there is a defect in the host's defense or it is overcome by high inoculum or virulence of the pathogen, then pneumonia will result. Pathogens may also spread through the hematogenous route and macro-aspiration.
History and Physical
Common symptoms of pneumonia include fever, chills, cough productive of purulent sputum, dyspnea, pleuritic chest pain, and weight loss. Patients with alcohol use disorder and those who are immune-compromised may have an absence of fever and less evident or systemic symptoms such as weakness, lethargy, altered mental status, dyspepsia, or other upper gastrointestinal symptoms. The presence of some symptoms may provide etiological clues. For example, diarrhea, headache, and confusion (related to hyponatremia) can indicate Legionella infection; otitis media, Stevens-Johnson syndrome, or anemia with jaundice (hemolytic anemia) may indicate Mycoplasma infection. Pneumonia can provoke acute decompensation of an underlying chronic illness, such as congestive heart failure, and can confound the initial presentation of pneumonia and result in delays in diagnosis and treatment.
Evaluation
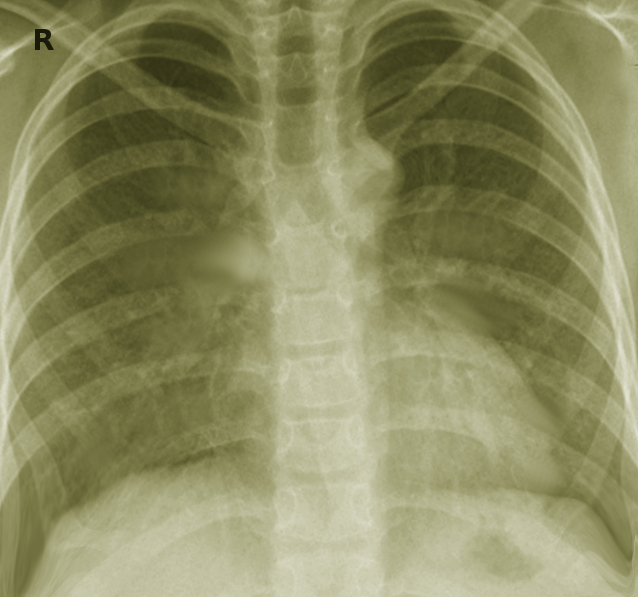
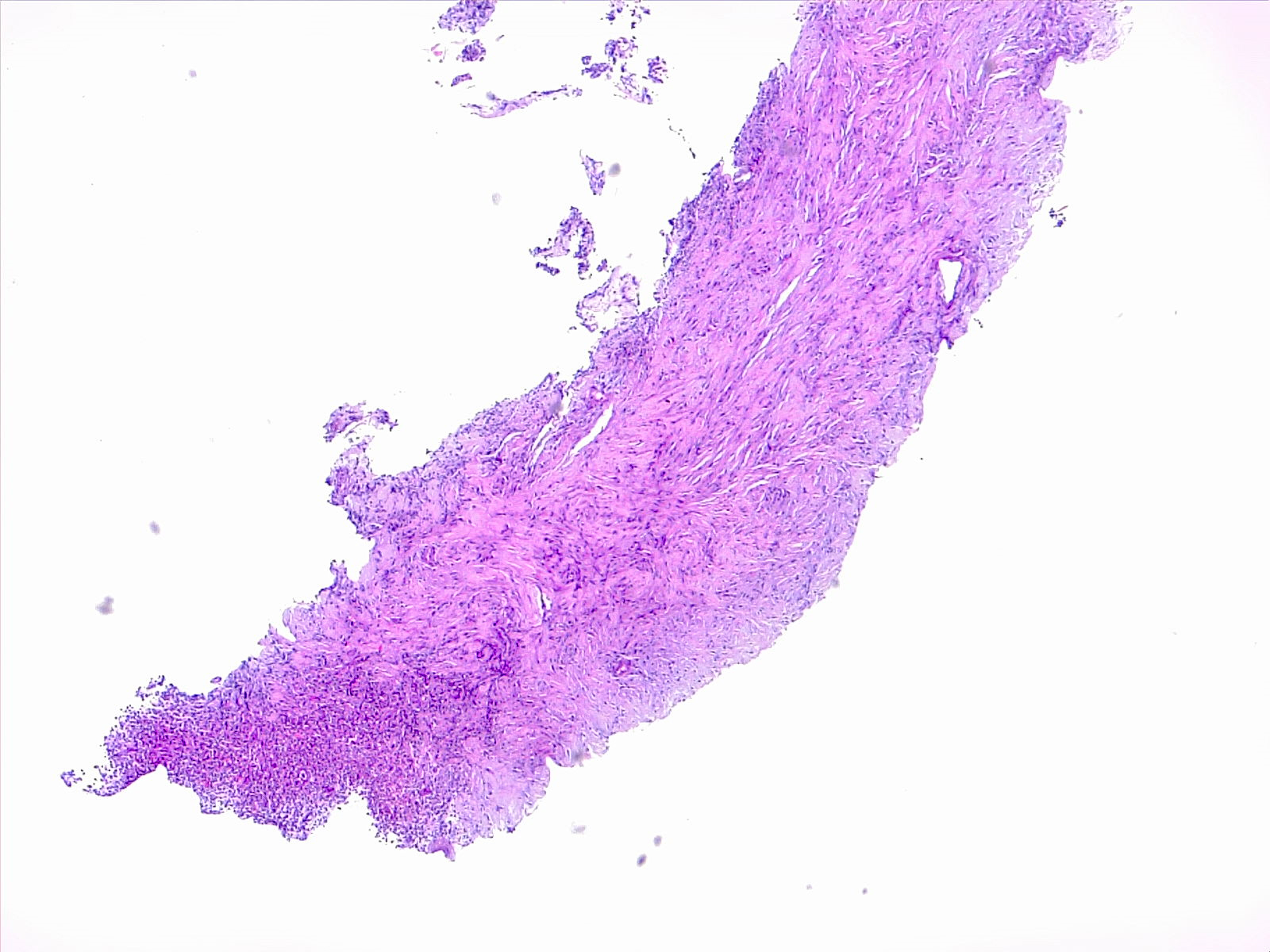
Initial workup for pneumonia will include imaging and blood work (see Images. Lung Abscess, Computed Tomography Scan and Bilateral Pneumonia, Computed Tomography Scan and Lung Pneumonia with Fibrosis). A chest x-ray will be needed to identify an infiltrate or effusion, which, if present, will improve diagnostic accuracy (see Image. Healthy Lung and Q Fever Pneumatic Lung, Chest X-ray). Bloodwork should include a complete blood count with differentials; serum electrolytes with renal and liver function tests help confirm evidence of inflammation and assess severity. Influenza testing is recommended during the winter season. Testing for respiratory viruses on nasopharyngeal swabs by molecular methods can be considered if available.
Tools such as CURB 65 (confusion, urea greater than or equal to 20 mg/dL, respiratory rate greater than or equal to 30/min, blood pressure systolic less than 90 mm Hg or diastolic less than 60 mm Hg), and Pneumonia Severity Index for severity assessment may assist in determining the treatment setting, such as outpatient versus inpatient. Still, accuracy is limited when used alone or without practical clinical judgment.
In hospitalized patients, blood and sputum cultures should be collected, preferably before the institution of antimicrobial therapy, but without delay in treatment. If cultures are negative, urine collection and testing for legionella and pneumococcal antigens must be considered as they aid in diagnosis. In the presence of confounding comorbidities, such as congestive heart failure, serum procalcitonin levels can be used as a biomarker to initiate and guide antimicrobial therapy. Serology for tularemia, endemic mycoses, or C psittaci can be evaluated in the presence of epidemiologic clues.[9][10][11]
Treatment / Management
Monotherapy with a macrolide (erythromycin, azithromycin, or clarithromycin), amoxicillin, or doxycycline is recommended in the outpatient setting. In the presence of comorbid illness (chronic heart disease excluding hypertension); chronic lung disease (chronic obstructive pulmonary disease and asthma); chronic liver disease; chronic alcohol use disorder; diabetes mellitus; smoking; splenectomy; human immunodeficiency virus (or other immunosuppression); a respiratory fluoroquinolone (high-dose levofloxacin, moxifloxacin, gemifloxacin); a combination of oral beta-lactam (high dose amoxicillin or amoxicillin-clavulanate, cefuroxime, cefpodoxime); and macrolide is recommended.[11][12][13][14](B2)
Inpatient management is recommended for patients with a CURB 65 score greater than or equal to 2. A respiratory fluoroquinolone monotherapy or combination therapy with beta-lactam (cefotaxime, ceftriaxone, ampicillin-sulbactam, or ertapenem) and macrolide are recommended options for non-intensive care settings.
Admission to the intensive care unit must be considered in patients with 3 or more signs of early deterioration. These include respiratory rate greater than 30, PaO2/FiO2 less than or equal to 250, multilobar infiltrates, encephalopathy, thrombocytopenia, hypothermia, leucopenia, and hypotension. Combination therapy with a beta-lactam and either a macrolide or a respiratory fluoroquinolone is recommended. In patients with suspected aspiration, ampicillin-sulbactam or ertapenem can be used. Monotherapy is not recommended.
If risk factors for Pseudomonas are present, then antipseudomonal beta-lactam (piperacillin-tazobactam, cefepime, ceftazidime, meropenem, imipenem) along with either an antipseudomonal fluoroquinolone (ciprofloxacin or levofloxacin) or a combination of aminoglycoside and azithromycin are recommended. Vancomycin or linezolid should be added if community-acquired methicillin-resistant S aureus is a consideration.
The recommended duration of therapy is 5 to 7 days in patients with a favorable clinical response, such as the absence of fever for more than 48 to 72 hours, not requiring supplemental oxygen, and resolution of tachycardia, tachypnea, or hypotension. Prolongation of therapy is indicated in patients with a delayed response, specific bacterial pathogens such as Pseudomonas (14-21 days) or S aureus (7-21 days), or Legionella pneumonia (14 days), and for complications such as empyema, lung abscess, or necrotizing pneumonia. Chest tube placement will be needed to drain an empyema, and in cases with multiple loculations, a surgical decortication may be needed. A 14-day therapy with macrolide or doxycycline will treat tularemia pneumonia or psittacosis, and itraconazole is the drug of choice for pneumonia caused by coccidioidomycosis or histoplasmosis.
A 5-day therapy with oseltamivir is recommended for all patients who test positive for the influenza virus and present within 48 hours of symptom onset; there is no benefit to oseltamivir if started beyond 48 hours after symptom onset. Still, any hospitalized patients with influenza must be treated with this agent regardless of the presentation time from the beginning of the illness.
Intravenous glucocorticoids can be considered adjunctive therapy in critically ill patients with severe community-acquired pneumonia without risk factors for adverse outcomes from using steroids (eg, influenza infection). They are associated with reductions in short-term mortality and duration of intensive care days.[15][16][17][18](A1)
Differential Diagnosis
Differential diagnoses for community-acquired pneumonia include:
- Acute bronchitis
- Acute exacerbation of chronic bronchitis
- Aspiration pneumonitis
- Congestive heart failure and pulmonary edema
- Pulmonary fibrosis
- Myocardial infarction
- Systemic lupus erythematosus pneumonitis
- Pulmonary drug hypersensitivity reactions (nitrofurantoin, daptomycin)
- Drug-induced pulmonary disease (bleomycin)
- Sarcoidosis
- Cryptogenic organizing pneumonia
- Pulmonary embolus
- Pulmonary infarction
- Bronchogenic carcinomas
- Granulomatosis with polyangiitis (Wegener granulomatosis)
- Lymphoma
- Tracheobronchitis
- Radiation pneumonitis
Pearls and Other Issues
Vaccine recommendations evolve in parallel with changing epidemiology vaccine developments and formulation advancements. All adults 65 years and older and those younger than 65 and considered at risk for pneumonia must receive a pneumococcal vaccination (PCV). The 2 vaccines used until 2021 were the pneumococcal polysaccharide vaccine (PPSV) 23 and PCV13. In summer 2021, the US FDA approved 2 additional preparations, PCV20 and PCV15, for adult vaccinations. Since then, the Advisory Committee on Immunization Practices (ACIP) recommendations favored using these latter formulations for adult vaccinations. Current ACIP recommendations for previously unvaccinated, non-immune-compromised individuals who are at least aged 65 years, as well as those between 19 to 64 years with risk factors for pneumonia, receive either PCV20 alone or PCV15 coupled with PPSV23 one year later.
For adults who already had vaccinations with prior formulations (PCV13 or PPSV23), subsequent options are different. Those who received only PCV13 can be followed by PPSV23 vaccination a year later. If the prior vaccine was only with PPSV23, then after a year, either PCV20 alone or PCV15 followed a year later with another PPSV23 can be given. The 1-year interval between pneumococcal doses can be shortened to 8 weeks for immunocompromised individuals.
Influenza vaccination is recommended for all adult patients at risk for influenza-related complications. Inactivated flu shots (trivalent or quadrivalent, egg-based or recombinant) are usually recommended for adults. Live attenuated intranasal vaccine can be given to healthy, nonpregnant adults under 49. This is contraindicated in pregnancy, the immune-suppressed and health care workers caring for them, and in those with comorbidities.
COVID-19 vaccination is recommended for all non-immune-compromised adults with either a single dose of a 2023-24 mRNA vaccine regardless of previous vaccination and that it be given at least 2 months after the most recent prior dose of COVID-19 vaccine. Novavax (protein-based) vaccine is given in 2 doses separated by 3 to 8 weeks for unvaccinated individuals. In contrast, a single dose after 2 months of the last dose is sufficient for those previously vaccinated with any other formulation of the COVID-19 vaccine. For individuals with moderate to severe immune compromise, 3 or 4 vaccine doses are recommended, with at least one using an mRNA formulation. A vaccine against respiratory syncytial virus is recommended for adults over 60 who may be at risk for severe disease.
Enhancing Healthcare Team Outcomes
Patients with community-acquired pneumonia may present to the clinician or the emergency department. The medical staff should be aware of the signs and symptoms associated with pneumonia. Working together, the healthcare team will improve outcomes. Members can include primary care, emergency department personnel, specialists, nurses, and pharmacists. Most patients respond to outpatient antibiotic therapy for 5 to 7 days. Patients who are short of breath, febrile, and in respiratory distress need to be admitted. An infectious disease or pulmonology consult is recommended if the diagnosis is unclear. Some patients may present with a parapneumonic effusion, which may require drainage. Typically, nurses monitor the patients and report current status and updates to the rest of the team. Pharmacists evaluate medication choices, check for allergies and drug interactions, and educate patients about possible side effects and the importance of compliance.
The providers should encourage all patients to get the annual influenza vaccine. In addition, all adults 65 and older and those considered at risk for pneumonia must receive the pneumococcal vaccination. The outcomes in most patients with community-acquired pneumonia are favorable.[19]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
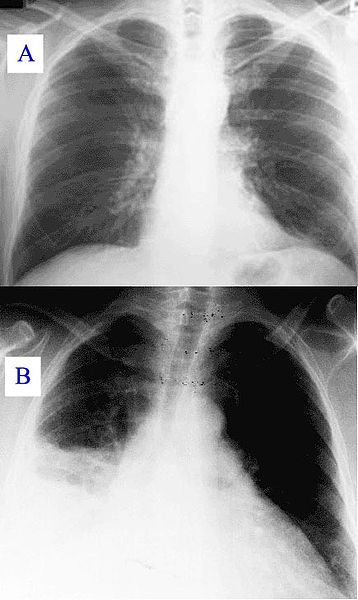
Healthy Lung and Q Fever Pneumatic Lung, Chest X-ray. X-ray A represents a normal healthy lung; X-ray B represents a lung with Q fever pneumonia.
Hehkuviini, Public Domain, via Wikimedia Commons.
(Click Image to Enlarge)
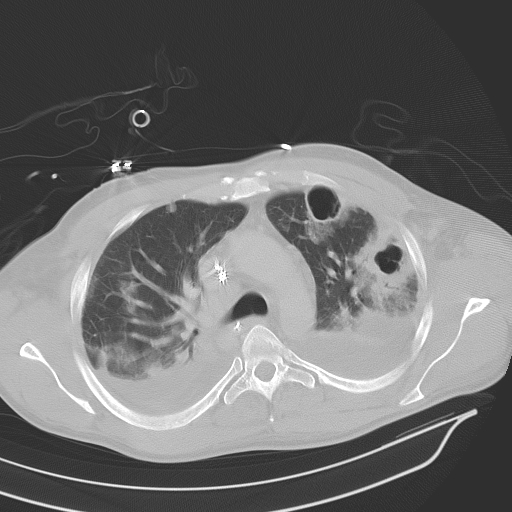
Bilateral Pneumonia, Computed Tomography Scan. Bilateral pneumonia with abscesses, effusions, and cavers in an adult male.
Christaras A, Public Domain, via Wikimedia Commons (CC by 2.5).
(Click Image to Enlarge)
References
Lu H, Zeng N, Chen Q, Wu Y, Cai S, Li G, Li F, Kong J. Clinical prognostic significance of serum high mobility group box-1 protein in patients with community-acquired pneumonia. The Journal of international medical research. 2019 Mar:47(3):1232-1240. doi: 10.1177/0300060518819381. Epub 2019 Feb 7 [PubMed PMID: 30732500]
Hassen M, Toma A, Tesfay M, Degafu E, Bekele S, Ayalew F, Gedefaw A, Tadesse BT. Radiologic Diagnosis and Hospitalization among Children with Severe Community Acquired Pneumonia: A Prospective Cohort Study. BioMed research international. 2019:2019():6202405. doi: 10.1155/2019/6202405. Epub 2019 Jan 9 [PubMed PMID: 30729128]
Alshahwan SI, Alsowailmi G, Alsahli A, Alotaibi A, Alshaikh M, Almajed M, Omair A, Almodaimegh H. The prevalence of complications of pneumonia among adults admitted to a tertiary care center in Riyadh from 2010-2017. Annals of Saudi medicine. 2019 Jan-Feb:39(1):29-36. doi: 10.5144/0256-4947.2019.29. Epub [PubMed PMID: 30712048]
Guo Q, Song WD, Li HY, Zhou YP, Li M, Chen XK, Liu H, Peng HL, Yu HQ, Chen X, Liu N, Lü ZD, Liang LH, Zhao QZ, Jiang M. Scored minor criteria for severe community-acquired pneumonia predicted better. Respiratory research. 2019 Jan 31:20(1):22. doi: 10.1186/s12931-019-0991-4. Epub 2019 Jan 31 [PubMed PMID: 30704469]
Tsoumani E, Carter JA, Salomonsson S, Stephens JM, Bencina G. Clinical, economic, and humanistic burden of community acquired pneumonia in Europe: a systematic literature review. Expert review of vaccines. 2023 Jan-Dec:22(1):876-884. doi: 10.1080/14760584.2023.2261785. Epub 2023 Oct 13 [PubMed PMID: 37823894]
Level 1 (high-level) evidenceGadsby NJ, Musher DM. The Microbial Etiology of Community-Acquired Pneumonia in Adults: from Classical Bacteriology to Host Transcriptional Signatures. Clinical microbiology reviews. 2022 Dec 21:35(4):e0001522. doi: 10.1128/cmr.00015-22. Epub 2022 Sep 27 [PubMed PMID: 36165783]
File TM Jr, Ramirez JA. Community-Acquired Pneumonia. Reply. The New England journal of medicine. 2023 Oct 26:389(17):1633-1634. doi: 10.1056/NEJMc2310748. Epub [PubMed PMID: 37888934]
Jain S, Self WH, Wunderink RG, Fakhran S, Balk R, Bramley AM, Reed C, Grijalva CG, Anderson EJ, Courtney DM, Chappell JD, Qi C, Hart EM, Carroll F, Trabue C, Donnelly HK, Williams DJ, Zhu Y, Arnold SR, Ampofo K, Waterer GW, Levine M, Lindstrom S, Winchell JM, Katz JM, Erdman D, Schneider E, Hicks LA, McCullers JA, Pavia AT, Edwards KM, Finelli L, CDC EPIC Study Team. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults. The New England journal of medicine. 2015 Jul 30:373(5):415-27. doi: 10.1056/NEJMoa1500245. Epub 2015 Jul 14 [PubMed PMID: 26172429]
Level 2 (mid-level) evidenceTorres A, Chalmers JD, Dela Cruz CS, Dominedò C, Kollef M, Martin-Loeches I, Niederman M, Wunderink RG. Challenges in severe community-acquired pneumonia: a point-of-view review. Intensive care medicine. 2019 Feb:45(2):159-171. doi: 10.1007/s00134-019-05519-y. Epub 2019 Jan 31 [PubMed PMID: 30706119]
Pickens CI, Wunderink RG. Principles and Practice of Antibiotic Stewardship in the ICU. Chest. 2019 Jul:156(1):163-171. doi: 10.1016/j.chest.2019.01.013. Epub 2019 Jan 25 [PubMed PMID: 30689983]
Nuttall JJC. Current antimicrobial management of community-acquired pneumonia in HIV-infected children. Expert opinion on pharmacotherapy. 2019 Apr:20(5):595-608. doi: 10.1080/14656566.2018.1561864. Epub 2019 Jan 21 [PubMed PMID: 30664362]
Level 3 (low-level) evidenceFroes F, Pereira JG, Póvoa P. Outpatient management of community-acquired pneumonia. Current opinion in pulmonary medicine. 2019 May:25(3):249-256. doi: 10.1097/MCP.0000000000000558. Epub [PubMed PMID: 30585861]
Level 3 (low-level) evidenceMi X, Li W, Zhang L, Li J, Zeng L, Huang L, Chen L, Song H, Huang Z, Lin M. The drug use to treat community-acquired pneumonia in children: A cross-sectional study in China. Medicine. 2018 Nov:97(46):e13224. doi: 10.1097/MD.0000000000013224. Epub [PubMed PMID: 30431600]
Level 2 (mid-level) evidenceHagel S, Moeser A, Pletz MW. [Management of community acquired pneumonia]. MMW Fortschritte der Medizin. 2018 Nov:160(19):52-61. doi: 10.1007/s15006-018-0027-x. Epub [PubMed PMID: 30406515]
Meduri GU, Shih MC, Bridges L, Martin TJ, El-Solh A, Seam N, Davis-Karim A, Umberger R, Anzueto A, Sriram P, Lan C, Restrepo MI, Guardiola JJ, Buck T, Johnson DP, Suffredini A, Bell WA, Lin J, Zhao L, Uyeda L, Nielsen L, Huang GD, ESCAPe Study Group. Low-dose methylprednisolone treatment in critically ill patients with severe community-acquired pneumonia. Intensive care medicine. 2022 Aug:48(8):1009-1023. doi: 10.1007/s00134-022-06684-3. Epub 2022 May 13 [PubMed PMID: 35723686]
Dequin PF, Meziani F, Quenot JP, Kamel T, Ricard JD, Badie J, Reignier J, Heming N, Plantefève G, Souweine B, Voiriot G, Colin G, Frat JP, Mira JP, Barbarot N, François B, Louis G, Gibot S, Guitton C, Giacardi C, Hraiech S, Vimeux S, L'Her E, Faure H, Herbrecht JE, Bouisse C, Joret A, Terzi N, Gacouin A, Quentin C, Jourdain M, Leclerc M, Coffre C, Bourgoin H, Lengellé C, Caille-Fénérol C, Giraudeau B, Le Gouge A, CRICS-TriGGERSep Network. Hydrocortisone in Severe Community-Acquired Pneumonia. The New England journal of medicine. 2023 May 25:388(21):1931-1941. doi: 10.1056/NEJMoa2215145. Epub 2023 Mar 21 [PubMed PMID: 36942789]
Bergmann F, Pracher L, Sawodny R, Blaschke A, Gelbenegger G, Radtke C, Zeitlinger M, Jorda A. Efficacy and Safety of Corticosteroid Therapy for Community-Acquired Pneumonia: A Meta-Analysis and Meta-Regression of Randomized, Controlled Trials. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2023 Dec 15:77(12):1704-1713. doi: 10.1093/cid/ciad496. Epub [PubMed PMID: 37876267]
Level 1 (high-level) evidencePeng B, Li J, Chen M, Yang X, Hao M, Wu F, Yang Z, Liu D. Clinical value of glucocorticoids for severe community-acquired pneumonia: A systematic review and meta-analysis based on randomized controlled trials. Medicine. 2023 Nov 17:102(46):e36047. doi: 10.1097/MD.0000000000036047. Epub [PubMed PMID: 37986401]
Level 1 (high-level) evidenceEspinoza R, Silva JRLE, Bergmann A, de Oliveira Melo U, Calil FE, Santos RC, Salluh JIF. Factors associated with mortality in severe community-acquired pneumonia: A multicenter cohort study. Journal of critical care. 2019 Apr:50():82-86. doi: 10.1016/j.jcrc.2018.11.024. Epub 2018 Nov 22 [PubMed PMID: 30502687]