Anatomy, Shoulder and Upper Limb, Forearm Ulna
Anatomy, Shoulder and Upper Limb, Forearm Ulna
Introduction
The ulna is one of the two forearm long bones that, in conjunction with the radius, make up the antebrachium. The bone spans from the elbow to the wrist on the medial side of the forearm when in anatomical position. In comparison to the radius, the ulna is described to be larger and longer. It serves as the origin and/or insertion site for more than a dozen muscles and is involved in motions assisted by the elbow and the wrist joints. Common pathologies are also associated with the bone as several fractures are pathognomonic depending on the location within the ulna, as well as the resulting position of the fractured segments.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
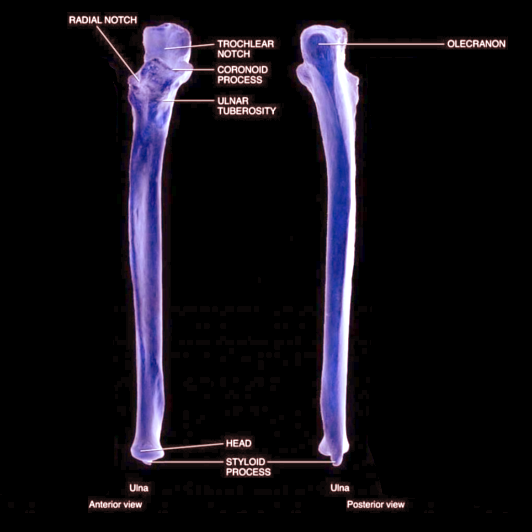
Beginning with the sites around the elbow, the ulna has a bony process called the olecranon process. It is a thick, curved distinction at the proximal and posterior end and is bent forward. This trait allows the bone to fit into the olecranon fossa of the humerus. The articular surface of the proximal ulna is a notch in the olecranon along the volar surface; this forms the "hinged" ulnohumeral component of the elbow joint. Together, the olecranon and olecranon fossa are involved in the extension/flexion of the forearm while simultaneously preventing hyperextension.[2]
The coronoid process is a protrusion from the proximal and anterior side of the ulna. It slightly arches upward and fits into the coronoid fossa of the humerus. At this point, the surfaces of the coronoid process allow for the insertion of the brachialis. The most medial portion of the coronoid process is referred to as the sublime tubercle and serves as the attachment side to the anterior bundle of the medial ulnar collateral ligament. Lateral to the coronoid process, a narrow depression serves as an articulating surface for the head of the radius, called the radial notch. This proximal radioulnar articulation plays a role in the supination and pronation of the forearm allowing the radial head to rotate relative to the proximal ulna. The semilunar notch is another depression, formed as a bridge between the coronoid process and the olecranon process. Here, the depression articulates with the humeral trochlea.[3]
The body of the ulna has a series of borders and surfaces as it travels down distally. The volar border starts at the coronoid process and ends anterior to the styloid process. This border serves to be an origin site for the flexor digitorum profundus and the pronator quadratus. The dorsal border starts posterior to the olecranon process and runs down to the styloid process as well. Here, it works as attachment sites for the flexor carpi ulnaris, extensor carpi ulnaris, and the flexor digitorum profundus. The interosseous crest starts at the radial notch and then ends at the ulnar head, giving attachment to the interosseous membrane, a compact fibrous area of connective tissue filling the space between the ulna and the radius.[4][5][6]
The volar or anterior surface of the ulna covers more area proximally than distally and allows for the origin of the flexor digitorum profundus and the pronator quadratus. Between the upper and the middle third of the ulna, an opening termed the nutrient canal, is present. Here, a system of blood vessels enters to span the shaft of the bone by extending into the medullary cavity. The dorsal surface consists of the posterior and the lateral sides of the bone and houses the insertion sites for the anconeus muscle and the supinator. However, more distally, it also is involved in attachments of the extensor carpi ulnaris, supinator, abductor pollicis longus, extensor pollicis longus, and the extensor indicis propius. The medial surface of the ulna only serves as an additional origin site to the flexor digitorum profundus.[7][8][9][10]
At the distal end, the ulna consists of two protrusions – the ulnar head and the styloid process. The head of the ulna points downward and serves as an articulating surface for the radius in a groove called the ulnar notch. Together the ulnar notch in the distal radius and curved surface of the lateral or radial margin of the distal ulna allows for supination/pronation of the distal forearm and wrist, similar in function but the inverse role of the bones of the proximal radioulnar joint. The styloid process descends lower than the ulnar head and connects to the bones of the wrist through the ulnar collateral ligament, as well as serving as an attachment site for the triangular fibrocartilage and radioulnar ligaments stabilizing the distal radioulnar joint.[11]
Embryology
The ulna develops from the induction of the lateral plate mesoderm. From this, it differentiates into the somatic mesoderm, which, in turn, gives rise to all of the bones, ligaments, connective tissue, and blood vessels of the extremities. Endochondral ossification allows for the induction of bone from previously laid hyaline cartilage. The ulna itself is ossified in three sections. First, it commences at the body of the ulna. Around week eight of gestation, the chondrocytes in the middle of the ulna lay down collagen and fibronectin to appropriately calcify the bone template. At the time of birth, the ends of the bone are still cartilaginous and not ossified. Around age four, an ossification center arises in the middle of the ulnar head and then encompasses into the styloid process. At age ten, a subsequent center appears in the olecranon, which is then met by the growth of the epiphysis at approximately age sixteen. The ossification centers about the elbow occur in a predictable order and understanding/knowledge of these stages of development is essential for identifying traumatic injuries about the elbow [12][13]
Blood Supply and Lymphatics
The main blood supply of the ulna originates from the ulnar artery or the ulnar recurrent artery. The ulnar artery then branches into a common interosseous artery that then further subdivides into the posterior and anterior interosseous vessels. These vessels are vital for the nutrients of the ulnar diaphysis. The ulnar metaphysis is supplied by the end branches of the anterior interosseous artery, while the head of the ulna receives its supply from small divisions off of the ulnar artery proper.[14][15]
The lymphatics of the ulna drain either to the supratrochlear lymph node or directly travel to the adjacent cluster of axillary lymph nodes.[16]
Nerves
Three main nerves run in the forearm in the proximity of the ulna: the median, ulnar, and radial nerves. The median nerve runs anterolaterally and innervates the muscles responsible for flexion of the wrist and the fingers (digits 1 to 3 and radial aspect of the fourth). The ulnar nerve is positioned more anteromedially, running in between the flexor digitorum superficialis and flexor digitorum profundus. This nerve is also involved in flexion of the wrist and fingers (the ulnar aspect of 4th and all of the 5th) but also is responsible for spanning the fingers. A major branch of the median nerve is the anterior interosseous nerve. Impingement or entrapment of the anterior interosseous nerve results in the characteristic clinical finding of weakness related to the "pincer" movement. The radial nerve extends posteriorly to the ulna and the radius and is the sole nerve involved in the muscles responsible for extension of the forearm, wrist, and fingers. The posterior interosseous nerve is a branch of the radial nerve with both motor and sensory functions. Posterior interosseous nerve impingement or entrapment occurs in the region of the radial tunnel resulting in weakness related to the extension of the digits.[17][18]
Muscles
The ulna serves as the attachment site for numerous muscles with a myriad of actions. The following are organized in terms of the direction and where on the ulna is the attachment of the muscle’s fibers.
The following muscles insert into the ulna:
Triceps brachii – posterior section of the superior surface of the olecranonAnconeus – olecranonBrachialis – the volar surface of the coronoid process
The following muscles originate from the ulna[19][20]:
- Pronator teres – the medial surface of the coronoid process
- Flexor carpi ulnaris – olecranon process
- Flexor digitorum superficialis – coronoid process
- Flexor digitorum profundus – anteromedial surface
- Pronator quadratus – distal anterior shaft
- Extensor carpi ulnaris – posterior border
- Supinator – proximal ulna
- Abductor pollicis longus – posterior surface
- Extensor pollicis longus – dorsal shaft
- Extensor indicis – posterior distal shaft
Physiologic Variants
Radioulnar synostosis is a rare congenital fusion of the proximal radius and ulna, resulting in limited supination and pronation of the forearm. Although rare, when present, it is bilateral in 60 to 80% of cases. This malformation commonly gets identified early in life, most often children age 2 through 5 years. A classification scheme has been developed by Cleary and Omer with four distinct types of malformation described with various forms of osseous hypoplasia and synostosis. Management options vary from conservative to surgical, depending on the type of malformation and the age of presentation.[21]
Surgical Considerations
Ulnar impaction syndrome (UIS) has become a very common cause of medial wrist pain in individuals with occupational injuries. Discovered by Henry Milch in 1941, UIS is identified in patients with acute trauma, chronic degeneration, or overuse injury in the ulnar side of the wrist and can present with changes in the bone, such as subchondral sclerosis and bone edema, and alterations in the cartilage and ligaments of the wrist. With its prevalence trending upwards, the need for quicker and more stable solutions to relieve the symptoms is crucial. Ulnar shortening osteotomy (USO) has been a surgical technique used by orthopedists after the nonoperative options of NSAIDs and immobilization have been ineffective. This procedure achieves relief in the patient by decreasing the length of the ulna, which will eventually decrease the load on the triangular fibrocartilage complex, a cushion buttressing the carpal bones. In recent literature, USO has shown to be able to reduce pain as well as improve disability. However, there have been reports of a limited range of motion of the joint following the procedure.[22]
Clinical Significance
Most of the pathologies encompassing the ulna stem from various fractures and fracture-dislocations. The radius and ulna form a ring structure of the forearm connected by ligaments and the interosseous membrane. Injury/fracture of one bone should increase clinical concern for injury of the other or an associated dislocation. These fractures can be differentiated based on the specific location involved as well as the configurations of the residual fragments. Often, a fracture in the ulna is concomitant with a radial fracture. Diagnosing a fracture of the ulna involves taking a proper history and physical first and foremost. With high clinical suspicion, the patient should have plain films taken of the area of the interest along with the associated joints above and below. The appropriate radiographic views must be also be included to develop a suitable treatment plan. The following are common fractures involving the ulna[23][24][25][26]:
- Nightstick fracture – a break in the middle shaft of the ulna excluding any other sites of fracture
- Monteggia fracture – a break in the proximal third of the ulna with a radial head dislocation
- Galeazzi Fracture - a break in the distal third of the radius with associated distal radioulnar joint dislocation
- Essex-Lopresti - a fracture of the radial head with dislocation of the distal radioulnar joint
- Hume fracture – a break in the olecranon along with a radial head anterior dislocation
- Distal ulna fracture – most commonly associated with a distal radial fracture
Media
(Click Image to Enlarge)
References
Shin WJ, Kim JP, Yang HM, Lee EY, Go JH, Heo K. Topographical Anatomy of the Distal Ulna Attachment of the Radioulnar Ligament. The Journal of hand surgery. 2017 Jul:42(7):517-524. doi: 10.1016/j.jhsa.2017.03.031. Epub 2017 Apr 25 [PubMed PMID: 28450099]
Card RK, Lowe JB. Anatomy, Shoulder and Upper Limb, Elbow Joint. StatPearls. 2023 Jan:(): [PubMed PMID: 30422543]
Beşer CG, Demiryürek D, Özsoy H, Erçakmak B, Hayran M, Kızılay O, Özsoy A. Redefining the proximal ulna anatomy. Surgical and radiologic anatomy : SRA. 2014 Dec:36(10):1023-31. doi: 10.1007/s00276-014-1340-4. Epub 2014 Jul 17 [PubMed PMID: 25031124]
Bhandari M, Schemitsch EH. Fractures of the shaft of the ulna. Journal of orthopaedic trauma. 2004 Aug:18(7):473-5 [PubMed PMID: 15289698]
Bandovic I, Holme MR, Black AC, Futterman B. Anatomy, Bone Markings. StatPearls. 2023 Jan:(): [PubMed PMID: 30020631]
Soubeyrand M, Assabah B, Bégin M, Laemmel E, Dos Santos A, Crézé M. Pronation and supination of the hand: Anatomy and biomechanics. Hand surgery & rehabilitation. 2017 Feb:36(1):2-11. doi: 10.1016/j.hansur.2016.09.012. Epub 2016 Oct 27 [PubMed PMID: 28137437]
Lung BE, Burns B. Anatomy, Shoulder and Upper Limb, Hand Flexor Digitorum Profundus Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 30252302]
Sawyer E, Sajjad H, Tadi P. Anatomy, Shoulder and Upper Limb, Forearm Extensor Carpi Ulnaris Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 30969582]
Berezovsky DR, Bordoni B. Anatomy, Shoulder and Upper Limb, Forearm Arteries. StatPearls. 2023 Jan:(): [PubMed PMID: 31424739]
Chaudhry F, Aminullah H, Sinkler MA, Arain A. Anatomy, Shoulder and Upper Limb, Forearm Compartments. StatPearls. 2023 Jan:(): [PubMed PMID: 30969606]
Haugstvedt JR, Langer MF, Berger RA. Distal radioulnar joint: functional anatomy, including pathomechanics. The Journal of hand surgery, European volume. 2017 May:42(4):338-345. doi: 10.1177/1753193417693170. Epub 2017 Feb 1 [PubMed PMID: 28399788]
Vuillermin C, Butler L, Ezaki M, Oishi S. Ulna Growth Patterns After Soft Tissue Release With Bilobed Flap in Radial Longitudinal Deficiency. Journal of pediatric orthopedics. 2018 Apr:38(4):244-248. doi: 10.1097/BPO.0000000000000807. Epub [PubMed PMID: 27280899]
Wiśniewski M, Baumgart M, Grzonkowska M, Szpinda M, Pawlak-Osińska K. Quantitative anatomy of the ulna's shaft primary ossification center in the human fetus. Surgical and radiologic anatomy : SRA. 2019 Apr:41(4):431-439. doi: 10.1007/s00276-018-2121-2. Epub 2018 Oct 31 [PubMed PMID: 30382328]
Koslowsky TC, Berger V, Hopf JC, Müller LP. Presentation of the vascular supply of the proximal ulna using a sequential plastination technique. Surgical and radiologic anatomy : SRA. 2015 Sep:37(7):749-55. doi: 10.1007/s00276-015-1476-x. Epub 2015 Apr 18 [PubMed PMID: 25894529]
Sheetz KK, Bishop AT, Berger RA. The arterial blood supply of the distal radius and ulna and its potential use in vascularized pedicled bone grafts. The Journal of hand surgery. 1995 Nov:20(6):902-14 [PubMed PMID: 8583061]
Gatsalov MD. [The intraorgan lymphatic bed of the periosteum in the upper extremity]. Arkhiv anatomii, gistologii i embriologii. 1967 Apr:52(4):70-7 [PubMed PMID: 6033730]
Strohl AB, Zelouf DS. Ulnar Tunnel Syndrome, Radial Tunnel Syndrome, Anterior Interosseous Nerve Syndrome, and Pronator Syndrome. The Journal of the American Academy of Orthopaedic Surgeons. 2017 Jan:25(1):e1-e10. doi: 10.5435/JAAOS-D-16-00010. Epub [PubMed PMID: 27902538]
Franco MJ, Nguyen DC, Phillips BZ, Mackinnon SE. Intraneural Median Nerve Anatomy and Implications for Treating Mixed Median Nerve Injury in the Hand. Hand (New York, N.Y.). 2016 Dec:11(4):416-420. doi: 10.1177/1558944716643290. Epub 2016 Apr 5 [PubMed PMID: 28149207]
Mitchell B, Whited L. Anatomy, Shoulder and Upper Limb, Forearm Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 30725660]
Javed O, Maldonado KA, Ashmyan R. Anatomy, Shoulder and Upper Limb, Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 29494017]
Siemianowicz A, Wawrzynek W, Besler K. Congenital radioulnar synostosis - case report. Polish journal of radiology. 2010 Oct:75(4):51-4 [PubMed PMID: 22802806]
Level 3 (low-level) evidenceFulton C, Grewal R, Faber KJ, Roth J, Gan BS. Outcome analysis of ulnar shortening osteotomy for ulnar impaction syndrome. The Canadian journal of plastic surgery = Journal canadien de chirurgie plastique. 2012 Spring:20(1):e1-5 [PubMed PMID: 23598767]
Nogueira AF, Moratelli L, Martins MDS, Iupi RT, de Abreu MFM, Nakamoto JC. EVALUATION OF DISTAL FOREARM FRACTURES USING THE AO 2018 CLASSIFICATION. Acta ortopedica brasileira. 2019 Jul-Aug:27(4):220-222. doi: 10.1590/1413-785220192704218467. Epub [PubMed PMID: 31452624]
Ali M, Clark DI, Tambe A. Nightstick Fractures, Outcomes of Operative and Non-Operative Treatment. Acta medica (Hradec Kralove). 2019:62(1):19-23. doi: 10.14712/18059694.2019.41. Epub [PubMed PMID: 30931892]
Ring D. Monteggia fractures. The Orthopedic clinics of North America. 2013 Jan:44(1):59-66. doi: 10.1016/j.ocl.2012.08.007. Epub 2012 Oct 10 [PubMed PMID: 23174326]
Kim JK, Kim JO, Koh YD. Management of Distal Ulnar Fracture Combined with Distal Radius Fracture. The journal of hand surgery Asian-Pacific volume. 2016 Jun:21(2):155-60. doi: 10.1142/S2424835516400075. Epub [PubMed PMID: 27454628]