Dieulafoys Lesion Causing Gastrointestinal Bleeding
Dieulafoys Lesion Causing Gastrointestinal Bleeding
Introduction
Dieulafoy lesion is a developmental vascular malformation of the gastrointestinal tract (GIT) first described by a French Surgeon, Paul Georges Dieulafoy, in 1898 as “exulceratio simplex.” It is a rare cause of life-threatening gastrointestinal bleeding that constitutes about 1% to 2% of all the causes of gastrointestinal bleeding and 6.5% of all causes of upper gastrointestinal non-variceal bleeding.[1][2]
The Dieulafoy lesion is composed of a normal blood vessel with an abnormally wide diameter of 1 to 3 mm, protruding into the mucosa from the submucosa. The protrusion results in a small wall defect in GIT with fibrinoid necrosis at the base of the lesion; 70% of these lesions are found in the stomach, usually along the lesser curvature.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
A Dieulafoy lesion is an enlarged submucosal blood vessel that bleeds in the absence of any abnormality such as ulcers or erosions. The majority of the lesions arise in the stomach at the lesser curvature, within 6 cm of the gastroesophageal junction, as this region receives its arterial blood supply directly from the branches of the left gastric artery.[3]
Less commonly, extra-gastric lesions may also arise in the duodenum, colon, jejunum, esophagus, or surgical anastomosis site.[4] Bleeding from a Dieulafoy lesion is most commonly associated with comorbid conditions like cardiovascular disease, chronic kidney disease, hypertension, peptic ulcer disease, diabetes mellitus, and chronic use of certain drugs(nonsteroidal anti-inflammatory drugs(NSAIDs) and anticoagulants).[5]
Epidemiology
Dieulafoy lesion accounts for 6.5% of the causes of upper gastrointestinal hemorrhage.[2] In adults, they are found twice as frequently in men as in women (2 to 1).[6] In the pediatric population, they occur in an equal distribution among the male and female populations.[7] The lesions reportedly present in all age groups; however, they are most common in the elderly in their fifth decade of life with multiple comorbidities such as cardiovascular disease, hypertension, chronic kidney disease, and diabetes mellitus.[5]
Pathophysiology
There are several possible theories about the mechanism that results in the development of Dieulafoy lesions and their complications. The three main theories include the following:
- Pulsations of an abnormally large artery may disrupt the mucosal surface leading to exposure of the artery to the bowel contents resulting in mechanical and chemical erosion and bleeding[8]
- Wear and tear of the gastric mucosa may lead to arterial thrombus formation resulting in necrosis and bleeding.
- Age-related gastric mucosal atrophy
Several factors appear to trigger the rupture of the tortuous vessel, including nonsteroidal anti-inflammatory drugs (NSAIDs), tobacco, alcohol, and peptic ulcer disease (PUD); however, there is no proven association yet.
Histopathology
A biopsy is not recommended for the diagnosis of Dieulafoy lesions due to an increased risk of bleeding. Histological examination of the lesion in the past revealed a normal artery with the presence of occasional amyloid deposits.[9]
Macroscopically, the lesion resembles a pseudopolyp. Lesions that are actively bleeding have a wide arterial size of 1 to 2 mm, with arterial spurting and mucosal erosions measuring up to 5 mm. Microscopically, the artery has an elastic lamina and impinges on the muscularis mucosae. Dieulafoy lesion can be distinguished from gastric ulcers on histology by a lack of subintimal fibrosis and mucosal inflammation.[10]
History and Physical
Dieulafoy lesions are often asymptomatic unless the mucosa overlying the vessel erodes, resulting in bleeding. The signs and symptoms are related to blood loss, either due to intermittent or massive gastrointestinal hemorrhage. Melena is the most common presentation, followed by hematemesis, hematochezia, iron deficiency anemia (IDA), hemoptysis, or hemodynamic instability. In rare circumstances, Dieulafoy lesion of the gall bladder may present with upper abdominal pain in the absence of overt bleeding.[11]
Evaluation
Direct endoscopic visualization of the Dieulafoy lesion is the gold standard method for diagnosis. Most patients are diagnosed after a single endoscopy; however, poor visualization of the GIT due to food particles or blood may require multiple endoscopies. The endoscopic visual diagnostic criteria that are necessary for a diagnosis of Dieulafoy lesion is as following:
- Normal mucosa around the small defected mucosal lesions which has active pulsatile bleeding smaller than 3 mm
- The visualization of a protruding vessel from a slight defect or normal mucosa
- The observation of a fresh clot attached to a defect of normal mucosa[12]
If lesions are not detected by endoscopy, angiography and capsule endoscopy can be used to confirm the diagnosis. On an angiogram, there is an extravasation of contrast into the GIT from the eroded artery. The presence of tortuous vessels in the arterial phase with no early venous return also indicates Dieulafoy lesions. The bleeding source is visualizable using technetium-99m red blood cell scanning or computerized tomography (CT) angiography.[13]
Treatment / Management
The first-line treatment modality for Dieulafoy lesion is endoscopy.[14] In the past, surgical treatment with gastrostomy or gastrectomy was performed; however, it has been primarily replaced by endoscopy since 1986. The three commonly performed endoscopic treatment procedures include:
- Thermal, heat probe, or argon plasma coagulation
- Regional injection-epinephrine (EPI) or norepinephrine(NOR) injection and sclerotherapy
- Mechanical banding and hemoclips[6][15] (A1)
Mechanical hemostasis comprising of banding and hemoclips is the safest and most effective treatment.[16] A study by Alis et al. revealed that endoscopic band ligation (EBL) was associated with a lower risk of recurrent bleeding and shorter hospital stay compared with sclerotherapy.[15] Hemoclipping has proven effective in the treatment of Dieulafoy lesions with a success rate of 95%.[17] Combination therapy has better outcomes when compared with monotherapy for Dieulafoy lesions. During endoscopic treatment, the bleeding site is often tattooed with India ink for ease of future identification in a recurrent bleed event.[18] If endoscopic treatment fails, surgical treatment is performed, including wide wedge resection or partial /wedge gastrectomy.[19] (A1)
Differential Diagnosis
Dieulafoy lesion has a vast number of differential diagnoses based on the patients’ age, comorbidities, and overall health. Angiodysplasia is an important differential due to similar presenting symptoms. It can be differentiated on angiography, by the presence of arteriovenous shunting and vascular ectasia, and by histological examination of the lesion, which reveals the presence of abnormal submucosal vessels. Other similar conditions should be differentiated from Dieulafoy lesion based on presenting signs and symptoms, endoscopy, and angiography. These include diverticulosis, telangiectasias, vascular neoplasms, mucosal spider nevi, and connective tissue disorders.
Prognosis
The mortality and morbidity of Dieulafoy lesions have significantly reduced to 8.6% since the development of endoscopy.[8] Hemostasis is successfully achievable in 80 to 85% of the cases treated with endoscopy.
Complications
Due to the subtle nature of the disease, it is often missed as a diagnosis initially and may result in delayed treatment resulting in adverse complications. The most common complication is massive spontaneous gastrointestinal hemorrhage that may be fatal if left untreated. Intermittent blood loss may lead to iron deficiency anemia (IDA) and, in severe cases, hemodynamic instability. In some cases, it may lead to the worsening of pre-existing co-morbidities.
Deterrence and Patient Education
Patients need to minimize the risk factors for Dieulafoy lesion by avoiding the use of nonsteroidal anti-inflammatory drugs (NSAIDs) and alcohol. Regular follow up with a gastroenterologist is necessary to monitor the condition and prevent a recurrence.
Enhancing Healthcare Team Outcomes
Most cases of Dieulafoy lesions go undiagnosed due to lack of awareness, acute onset of signs and symptoms, intermittent bleeding pattern, and difficulty in visualization on endoscopy. On endoscopy, Dieulafoy lesion may be difficult to diagnose due to its small size or the presence of normal-appearing surrounding mucosa.[9]
Excessive blood in the GIT may also prevent visualization and further delay diagnosis. For these reasons, physicians and endoscopists should consider this condition as a differential diagnosis for intermittent or massive GIT bleeding. Radiologists should also be aware of the subtle nature of this condition that may be missed in a patient with gastrointestinal bleeding. Once diagnosed, endoscopy should be the preferred treatment since it has replaced invasive surgery due to better health care outcomes. During the evaluation of the lesion, it is essential to determine the focal point of the bleeding for the management of future episodes.
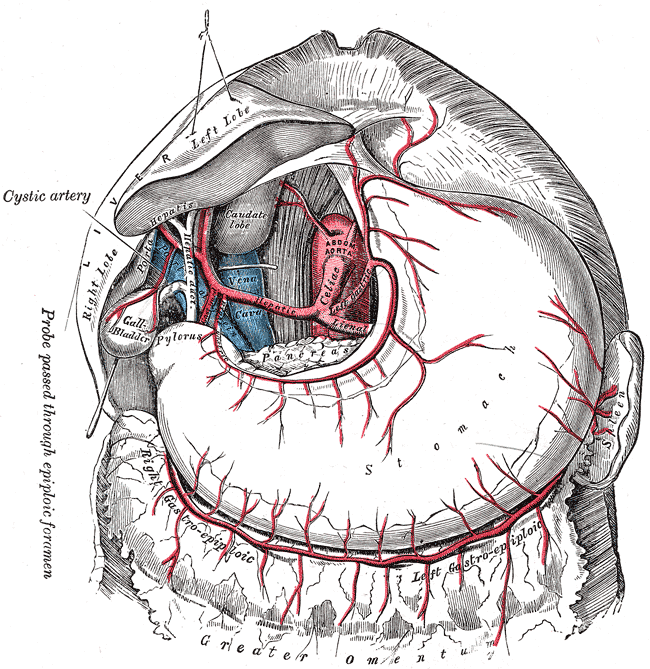
Media
(Click Image to Enlarge)
References
Marangoni G, Cresswell AB, Faraj W, Shaikh H, Bowles MJ. An uncommon cause of life-threatening gastrointestinal bleeding: 2 synchronous Dieulafoy lesions. Journal of pediatric surgery. 2009 Feb:44(2):441-3. doi: 10.1016/j.jpedsurg.2008.09.033. Epub [PubMed PMID: 19231553]
Level 3 (low-level) evidenceMansfield G, Sabharwal R, Bansi DS, Cohen P, El-Masry N, Jackson JE. Dieulafoy lesions: rare but often overdiagnosed? Observations based upon a case of small bowel haemorrhage and a critical review of the literature. Clinical radiology. 2012 Jan:67(1):78-80. doi: 10.1016/j.crad.2010.12.023. Epub 2011 Jun 11 [PubMed PMID: 21658692]
Level 3 (low-level) evidenceThen EO, Bijjam R, Ofosu A, Rawla P, Culliford A, Gaduputi V. Rectal Dieulafoy's Lesion: A Rare Etiology of Lower Gastrointestinal Hemorrhage. Case reports in gastroenterology. 2019 Jan-Apr:13(1):73-77. doi: 10.1159/000497139. Epub 2019 Feb 14 [PubMed PMID: 31043932]
Level 3 (low-level) evidenceClements J, Clements B, Loughrey M. Gastric Dieulafoy lesion: a rare cause of massive haematemesis in an elderly woman. BMJ case reports. 2018 Mar 15:2018():. pii: bcr-2017-223615. doi: 10.1136/bcr-2017-223615. Epub 2018 Mar 15 [PubMed PMID: 29545438]
Level 3 (low-level) evidenceSaleh R, Lucerna A, Espinosa J, Scali V. Dieulafoy lesion: the little known sleeping giant of gastrointestinal bleeds. The American journal of emergency medicine. 2016 Dec:34(12):2464.e3-2464.e5. doi: 10.1016/j.ajem.2016.06.024. Epub 2016 Jun 7 [PubMed PMID: 27342971]
Baxter M, Aly EH. Dieulafoy's lesion: current trends in diagnosis and management. Annals of the Royal College of Surgeons of England. 2010 Oct:92(7):548-54. doi: 10.1308/003588410X12699663905311. Epub [PubMed PMID: 20883603]
Senger JL, Kanthan R. The Evolution of Dieulafoy's Lesion Since 1897: Then and Now-A Journey through the Lens of a Pediatric Lesion with Literature Review. Gastroenterology research and practice. 2012:2012():432517. doi: 10.1155/2012/432517. Epub 2012 Feb 14 [PubMed PMID: 22474434]
Alshumrani G, Almuaikeel M. Angiographic findings and endovascular embolization in Dieulafoy disease: a case report and literature review. Diagnostic and interventional radiology (Ankara, Turkey). 2006 Sep:12(3):151-4 [PubMed PMID: 16972222]
Level 3 (low-level) evidenceChristoffersen RK, Nielsen TS, Vesterby A. Dieulafoy lesion of the esophagus causing massive upper gastrointestinal bleeding and death: a case report. The American journal of forensic medicine and pathology. 2012 Jun:33(2):186-7. doi: 10.1097/PAF.0b013e318221be16. Epub [PubMed PMID: 21659839]
Level 3 (low-level) evidenceShin HJ, Ju JS, Kim KD, Kim SW, Kang SH, Kang SH, Moon HS, Sung JK, Jeong HY. Risk Factors for Dieulafoy Lesions in the Upper Gastrointestinal Tract. Clinical endoscopy. 2015 May:48(3):228-33. doi: 10.5946/ce.2015.48.3.228. Epub 2015 May 29 [PubMed PMID: 26064823]
Wu JM, Zaitoun AM. A galling disease? Dieulafoy's lesion of the gallbladder. International journal of surgery case reports. 2018:44():62-65. doi: 10.1016/j.ijscr.2018.01.027. Epub 2018 Feb 10 [PubMed PMID: 29477106]
Level 3 (low-level) evidenceDogan U, Gomceli I, Koc U, Habibi M, Bulbuller N. Rectal dieulafoy lesions: a rare etiology of chronic lower gastrointestinal bleeding. Case reports in medicine. 2014:2014():180230. doi: 10.1155/2014/180230. Epub 2014 Oct 1 [PubMed PMID: 25349614]
Level 3 (low-level) evidenceNga ME, Buhari SA, Iau PT, Raju GC. Jejunal Dieulafoy lesion with massive lower intestinal bleeding. International journal of colorectal disease. 2007 Nov:22(11):1417-1418. doi: 10.1007/s00384-006-0227-1. Epub 2006 Nov 4 [PubMed PMID: 17086394]
Level 3 (low-level) evidenceLinhares MM, Filho BH, Schraibman V, Goitia-Durán MB, Grande JC, Sato NY, Lourenço LG, Lopes-Filho GD. Dieulafoy lesion: endoscopic and surgical management. Surgical laparoscopy, endoscopy & percutaneous techniques. 2006 Feb:16(1):1-3 [PubMed PMID: 16552369]
Alis H, Oner OZ, Kalayci MU, Dolay K, Kapan S, Soylu A, Aygun E. Is endoscopic band ligation superior to injection therapy for Dieulafoy lesion? Surgical endoscopy. 2009 Jul:23(7):1465-9. doi: 10.1007/s00464-008-0255-8. Epub 2009 Jan 6 [PubMed PMID: 19125307]
Level 1 (high-level) evidenceNojkov B, Cappell MS. Distinctive aspects of peptic ulcer disease, Dieulafoy's lesion, and Mallory-Weiss syndrome in patients with advanced alcoholic liver disease or cirrhosis. World journal of gastroenterology. 2016 Jan 7:22(1):446-66. doi: 10.3748/wjg.v22.i1.446. Epub [PubMed PMID: 26755890]
Ünal F, Çakır M, Baran M, Duygulu Ş, Aydoğdu S. Application of endoscopic hemoclips for nonvariceal upper gastrointestinal bleeding in children. The Turkish journal of gastroenterology : the official journal of Turkish Society of Gastroenterology. 2014 Apr:25(2):147-51. doi: 10.5152/tjg.2014.3419. Epub [PubMed PMID: 25003673]
Garg R. Bleeding from a gastric Dieulafoy lesion. Emergency medicine journal : EMJ. 2007 Jul:24(7):520 [PubMed PMID: 17582061]
Level 3 (low-level) evidenceHoffman A, Kunert A, Lahat A, Volkov A, Zmora O, Rosin D. Laparoscopic resection of gastric Dieulafoy lesion following preoperative tattooing. The Israel Medical Association journal : IMAJ. 2011 Mar:13(3):187-8 [PubMed PMID: 21608344]