Introduction
Prurigo pigmentosa, also known as Nagashima disease or "keto rash," is a rare inflammatory skin disease initially described by Nagashima et al in 1971.[1] Prurigo pigmentosa typically, but not exclusively, affects young females of East Asian ethnicity, presenting as a symmetrical eruption of urticarial papules on the neck, chest, and back.[2][3] The papular eruption typically coalesces into a reticulated pattern that repeatedly resolves and recurs, resulting in hyperpigmented skin of cosmetic concern.[4] Prurigo pigmentosa can be triggered by metabolic derangements, including those secondary to ketogenic diets, which have experienced a rise in popularity in recent years. This activity reviews the proposed etiology, pathogenesis, clinical evaluation, and therapeutic management of prurigo pigmentosa and highlights the role of the interprofessional team in improving outcomes for patients with this rare dermatosis.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of prurigo pigmentosa is unclear. It has been theorized that prurigo pigmentosa can be triggered by metabolic disorders, dietary modifications, hormonal changes, or infections.[5]
Prurigo pigmentosa has been linked to ketoacidosis, fasting, calorie restriction, and carbohydrate restriction, particularly in a ketogenic diet. Several reports have suggested a link between flares of prurigo pigmentosa and a serum ketone body measurement greater than 0.6 mmol/L, with the dermatosis resolving as urinary ketone levels correct. Additional studies are necessary to elucidate this connection further.[6]
Some cases of prurigo pigmentosa have occurred during pregnancy.[7][8] Prurigo pigmentosa has been reported following a COVID-19 vaccine.[9] Other studies suggest an association between prurigo pigmentosa and specific human leukocyte antigens.[10]
Epidemiology
Prurigo pigmentosa was first described in a Japanese woman. Since this initial description, prurigo pigmentosa has been reported in patients from Europe, the United States, and other countries.[1] While most commonly described in patients of East Asian ethnicity, there is no obvious reason for an ethnic preference; it has been proposed that this tendency is due to a lack of clinical awareness of this disease outside of East Asia.[11] However, mis- and underdiagnosis are frequent, and epidemiological studies reflect this. Prurigo pigmentosa is most commonly described in young women in late adolescence or early adulthood.[1][12]
Pathophysiology
The pathogenic and pathophysiologic mechanisms of prurigo pigmentosa remain unclear; research is ongoing.[8] It is hypothesized that when a susceptible person enters a ketotic state through fasting, ketoacidosis, or while on a ketogenic diet, prurigo pigmentosa develops via as yet unknown mechanisms. It has been demonstrated that a persistent ketotic state delays the healing of this dermatosis and that increasing carbohydrate consumption promotes its resolution.[13]
Additionally, it has been proposed that the chronic inflammation associated with prurigo pigmentosa may activate melanocytes to produce excess melanin, the dermal deposition of which results in persistent hyperpigmentation.[1] Postinflammatory melanin synthesis or impaired melanosome degradation may also contribute to persistent hyperpigmentation.[14]
Histopathology
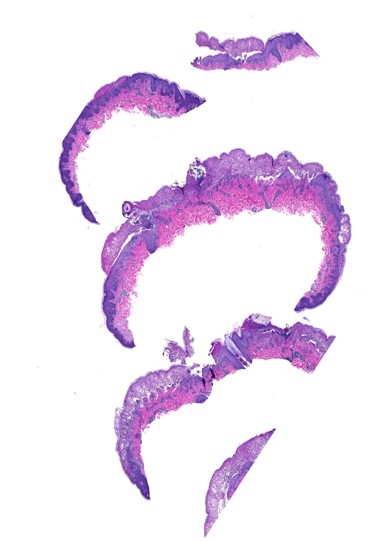
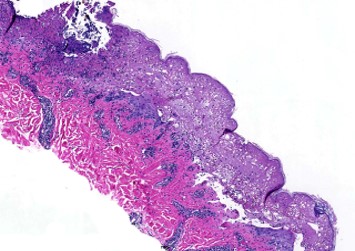
Prurigo pigmentosa is typically a clinical diagnosis. However, skin biopsies are essential to rule out other disease mimickers.[15] The histopathological features of prurigo pigmentosa will vary with the stage of the disease.[16]
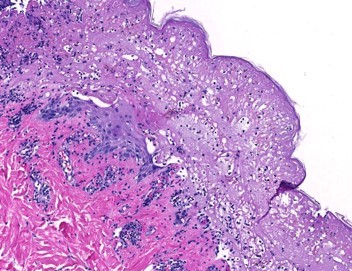
In the initial stages of the disease, the epidermis exhibits focal epidermal eosinophilic spongiosis, contributing to early papule formation (see Image. Prurigo Pigmentosa, 40X Magnification).[12] Intraepidermal vesicles may be seen, but these rarely become pustular. Edema may be present in the papillary dermis, and patchy lichenoid proliferation of inflammatory cell infiltrates may be observed. A mixed superficial perivascular inflammatory infiltrate comprising lymphocytes, neutrophils, and eosinophils may be noted in the upper dermis, extending to involve the dermal papillae. Vacuolar interface changes, necrotic keratinocytes, and focal epidermal necrosis are commonly noted.[17] A key histopathologic feature of prurigo pigmentosa is dermal-based dense inflammatory infiltrates of lymphocytes, histiocytes, and eosinophils; this finding may be linked to prior infectious processes, such as Helicobacter pylori.[18]
Histopathological changes commonly seen in the later stages of prurigo pigmentosa include lymphocytic infiltrates, the presence of melanophages, and pigmentary incontinence (see Image. Prurigo Pigmentosa, 100X Magnification).[12] Advanced stages of the disease exhibit a mildly hyperplastic epidermis with parakeratosis and basal hyperpigmentation (see Image. Prurigo Pigmentosa, 200X Magnification).[4]
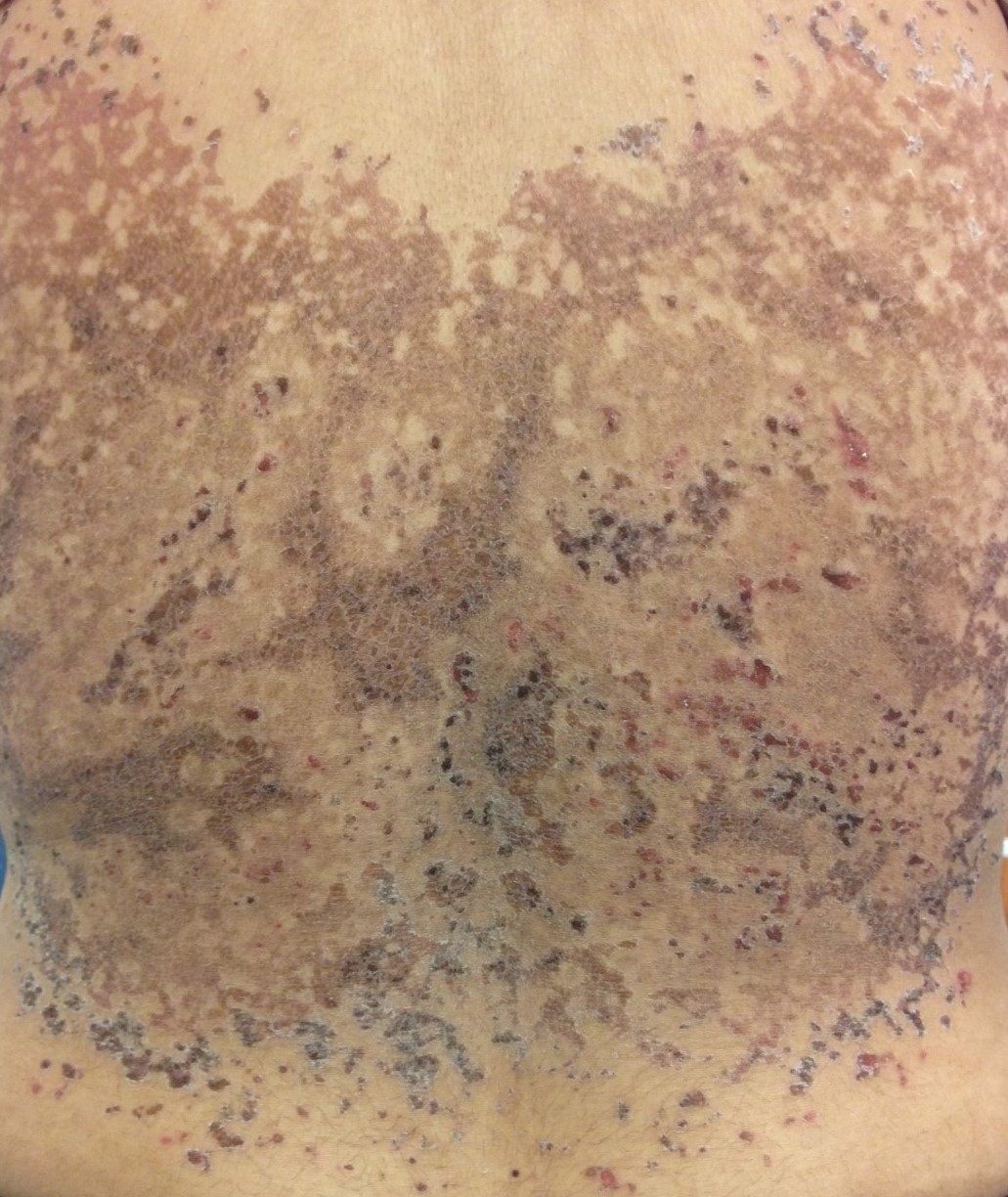
History and Physical
The clinical examination of patients with prurigo pigmentosa reveals pruritic erythematous papules, papulovesicles, and vesicles in a symmetric and reticular pattern, predominantly on the back, upper chest, and neck (see Image. Early Stage Prurigo Pigmentosa).[1][12] The erythematous papules spontaneously evolve into hyperpigmented reticulated patches or plaques (see Image. Prurigo Pigmentosa, Late Stage). The forehead, the arms, or the abdomen are rarely affected; mucous membrane involvement is unlikely (see Image. Prurigo Pigmentosa, Hyperpigmentation).[15] Recurrences favor previously affected anatomical sites. Presentations of unilateral, segmental, bullous, or exfoliative skin lesions have been reported, albeit rarely.[19][20][21][22]
Evaluation
Laboratory testing is sometimes warranted to determine the underlying risk of developing prurigo pigmentosa and exclude an underlying clinical condition.[6][23][24][23] Laboratory evaluations that aid in identifying patients with ketoacidosis include but are not limited to:
- Serum electrolytes
- Serum glucose
- Serum insulin
- Serum ketones, including beta-hydroxybutyrate
- Urinalysis
- HbA1c
Treatment / Management
Most cases of prurigo pigmentosa resolve spontaneously. Medical therapy is required to achieve resolution for some patients. Addressing predisposing medical conditions is essential to disease management.
The standard therapeutic approach to prurigo pigmentosa includes oral tetracycline or macrolide antibiotics.[25] An oral minocycline regimen of 100 mg orally twice daily for 2 to 4 weeks is the preferred initial therapy; tetracyclines inhibit inflammatory cytokines, including interleukins 1 and 6, and inhibit neutrophil chemotaxis.[12][26][27][28] Macrolides are a viable antimicrobial therapy. Dapsone, a sulfone, has also demonstrated therapeutic efficacy for prurigo pigmentosa; the mechanism of action is thought to be inhibition of neutrophil chemotaxis.[26][29][30](A1)
Adjunctive topical therapies for prurigo pigmentosa include corticosteroids or calcineurin inhibitors.[31] These topical agents aid in alleviating the symptomatic pruritus associated with prurigo pigmentosa.[32] The benefits of topical dapsone and topical minocycline remain questionable.
Colchicine inhibits neutrophil chemotaxis and has demonstrated therapeutic benefit for prurigo pigmentosa.[33] Dietary modification is warranted for patients following a ketogenic diet or in patients from countries with a high prevalence of ketosis-inducing diets.[34] In susceptible individuals, the resolution of skin lesions with dietary modification supports the diagnosis of prurigo pigmentosa and guides the treatment plan for high-risk patients.[13][35](B3)
There is no known definitive treatment for persistent hyperpigmentation secondary to prurigo pigmentosa. However, topical agents, laser therapy, chemical peels, microdermabrasion, intensed pulsed light treatments, and narrowband UV-B phototherapy have been employed with varying success.[36][37][36] One study noted improvement in hyperpigmentation with Q-switched double-frequency 532-nm Nd:YAG laser therapy.[38] Hydroquinone, retinoids, and corticosteroids are the most commonly utilized topical agents.[39][40] Adjunctive measures, including strict sun protection, may also help to alleviate the visible sequelae of prurigo pigmentosa; prolonged sun exposure may worsen existing pigmentation.[41] (B3)
Differential Diagnosis
The misdiagnosis of prurigo pigmentosa is believed to be common. The most common diagnostic pitfalls of prurigo pigmentosa include confluent and reticulated papillomatosis, atopic dermatitis, and contact dermatitis.[42][43][42][44] Dermatitis herpetiformis may easily be confused with prurigo pigmentosa; however, biopsy does not commonly demonstrate ballooning and spongiosis.[1] Cutaneous lupus erythematosus may mimic prurigo pigmentosa despite the absence of spongiosis, spongiotic vesicles, and neutrophilic infiltrates in the upper epidermis. However, other mimickers of prurigo pigmentosa include but are not limited to:
- lichen planus pigmentosus
- dermatitis herpetiformis
- bullous lichen planus
- acanthosis nigricans
- tinea versicolor
- terra firma-forme dermatosis
- febrile pityriasis lichenoides et varioliformis acuta (Mucha-Habermann disease)
- Darier disease
- Dowling-Degos disease
- Galli-Galli disease
- primary cutaneous amyloidosis
- erythema ab igne
Prognosis
Most cases of prurigo pigmentosa have a favorable prognosis with no dangerous sequelae. However, residual hyperpigmentation may persist for prolonged periods and be a cosmetic concern; early treatment reduces the risk of prolonged hyperpigmentation.[45][46]
Complications
Prurigo pigmentosa is an inflammatory skin condition with no known clinical complications.
Deterrence and Patient Education
Patient education for prurigo pigmentosa includes describing the common symptoms of prurigo pigmentosa, illustrating the recurrent nature of the disease, and explaining the contributing or triggering factors that may worsen symptoms.[12] Discussing potential triggers such as fasting and carbohydrate-restricted diets in addition to appropriate control of diabetes mellitus is essential to avoid the recurrence of the disease.[6][13] It should be stressed that the lesions are not contagious.
Enhancing Healthcare Team Outcomes
Prurigo pigmentosa is a rare dermatologic inflammatory disorder characterized by distinctive clinical and histopathological features. It is often associated with intense pruritus, which can cause skin irritation and excoriations, causing significant distress and discomfort for patients. Many cases of prurigo pigmentosa are related to metabolic derangements, and collaboration between primary care practitioners, dermatologists, diabetologists, and endocrinologists facilitates the management and resolution of the disorder. Comprehensive patient education employing nurses and pharmacists ensures a holistic approach to patient care.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Michor-Tscharre C, D'Alì L, Cota C, Fink-Puches R, Cerroni L. Clinical and Pathological Spectrum of Prurigo Pigmentosa in Central European Individuals. JAMA dermatology. 2023 Aug 1:159(8):864-869. doi: 10.1001/jamadermatol.2023.1917. Epub [PubMed PMID: 37436763]
Shen A, Cheng CE, Malik R, Mark E, Vecerek N, Maloney N, Leavens J, Nambudiri VE, Saavedra AP, Hogeling M, Worswick S. Prurigo pigmentosa: A multi-institutional retrospective study. Journal of the American Academy of Dermatology. 2023 Aug:89(2):376-378. doi: 10.1016/j.jaad.2023.03.034. Epub 2023 Mar 30 [PubMed PMID: 37001731]
Level 2 (mid-level) evidenceAlmaani N, Al-Tarawneh AH, Msallam H. Prurigo Pigmentosa: A Clinicopathological Report of Three Middle Eastern Patients. Case reports in dermatological medicine. 2018:2018():9406797. doi: 10.1155/2018/9406797. Epub 2018 Jul 9 [PubMed PMID: 30105102]
Level 3 (low-level) evidenceBöhler L, Dumann K, Kunz M. Symmetrical pruritic lesions on the trunk in a young woman - a rare case of non-associated Prurigo pigmentosa in Germany. Journal of the European Academy of Dermatology and Venereology : JEADV. 2022 Aug:36(8):e648-e650. doi: 10.1111/jdv.18113. Epub 2022 Apr 6 [PubMed PMID: 35349741]
Level 3 (low-level) evidenceDerrick KM, Mazori DR, Heilman ER, Glick SA. Prurigo pigmentosa and new-onset type 1 diabetes in a black female patient testing positive for SARS-CoV-2 IgG. The British journal of dermatology. 2021 Jan:184(1):e5. doi: 10.1111/bjd.19568. Epub 2020 Oct 25 [PubMed PMID: 33103238]
Nellore A, Maher E, Abate M. Prurigo Pigmentosa Induced by a Ketogenic Diet. Cureus. 2023 May:15(5):e39498. doi: 10.7759/cureus.39498. Epub 2023 May 25 [PubMed PMID: 37362479]
Maincent O, Husson B, Kieffer J, Durlach A, Cribier B, Viguier M. [Prurigo pigmentosa in a pregnant woman]. Annales de dermatologie et de venereologie. 2019 Mar:146(3):252-254. doi: 10.1016/j.annder.2019.01.007. Epub 2019 Mar 2 [PubMed PMID: 30833035]
Devred I, Sfecci A, Cardot-Leccia N, Lacour JP, Passeron T. [Prurigo pigmentosa during pregnancy]. Annales de dermatologie et de venereologie. 2019 Mar:146(3):215-218. doi: 10.1016/j.annder.2018.07.006. Epub 2018 Aug 11 [PubMed PMID: 30104019]
Skowron F, Carbonnelle-Puscian A. Prurigo pigmentosa following booster dose of COVID-19 vaccine. Journal of the European Academy of Dermatology and Venereology : JEADV. 2023 Mar:37(3):e289-e290. doi: 10.1111/jdv.18766. Epub 2022 Nov 26 [PubMed PMID: 36433722]
Danielsen M, Pallesen K, Riber-Hansen R, Bregnhøj A. A Rare Case of Prurigo Pigmentosa in a Danish Sibling Couple. Case reports in dermatology. 2023 Jan-Apr:15(1):26-30. doi: 10.1159/000528422. Epub 2023 Jan 27 [PubMed PMID: 36726802]
Level 3 (low-level) evidenceBoer A, Asgari M. Prurigo pigmentosa: an underdiagnosed disease? Indian journal of dermatology, venereology and leprology. 2006 Nov-Dec:72(6):405-9 [PubMed PMID: 17179613]
Mufti A, Mirali S, Abduelmula A, McDonald KA, Alabdulrazzaq S, Sachdeva M, Yeung J. Clinical manifestations and treatment outcomes in prurigo pigmentosa (Nagashima disease): A systematic review of the literature. JAAD international. 2021 Jun:3():79-87. doi: 10.1016/j.jdin.2021.03.003. Epub 2021 Apr 10 [PubMed PMID: 34409375]
Level 1 (high-level) evidenceDaneshpazhooh M, Nikyar Z, Kamyab Hesari K, Rostami E, Taraz Jamshidi S, Mohaghegh F. Remission of Prurigo Pigmentosa after Breaking Ketogenic Diet and Resuming Regular Diet. Advanced biomedical research. 2022:11():70. doi: 10.4103/abr.abr_138_21. Epub 2022 Aug 30 [PubMed PMID: 36325168]
Woolery-Lloyd H, Friedman A. Optimizing patient care with "natural" products: treatment of hyperpigmentation. Journal of drugs in dermatology : JDD. 2009 Jun:8(6 Suppl):s10-3 [PubMed PMID: 19562884]
Level 3 (low-level) evidenceOba MC, Arican CD. Clinical Features and Follow-Up of Prurigo Pigmentosa: A Case Series. Cureus. 2022 Apr:14(4):e24600. doi: 10.7759/cureus.24600. Epub 2022 Apr 29 [PubMed PMID: 35664395]
Level 2 (mid-level) evidenceOnaygil E, Songur A, Kutlubay Z, Demirkesen C. Early Stage Prurigo Pigmentosa : A Case Report. Turk patoloji dergisi. 2018:34(2):182-185. doi: 10.5146/tjpath.2015.01333. Epub [PubMed PMID: 28272658]
Level 3 (low-level) evidenceBöer A, Misago N, Wolter M, Kiryu H, Wang XD, Ackerman AB. Prurigo pigmentosa: a distinctive inflammatory disease of the skin. The American Journal of dermatopathology. 2003 Apr:25(2):117-29 [PubMed PMID: 12652193]
Missall TA, Pruden S, Nelson C, Fohn L, Vidal CI, Hurley MY. Identification of Helicobacter pylori in skin biopsy of prurigo pigmentosa. The American Journal of dermatopathology. 2012 Jun:34(4):446-8. doi: 10.1097/DAD.0b013e318231ae4a. Epub [PubMed PMID: 22197863]
Level 3 (low-level) evidenceKita K, Kurokawa I, Hayashi D, Hashimoto T. Prurigo pigmentosa clinically and immunologically mimicking autoimmune bullous disease: A case report. Frontiers in medicine. 2022:9():1047870. doi: 10.3389/fmed.2022.1047870. Epub 2022 Dec 2 [PubMed PMID: 36530916]
Level 3 (low-level) evidenceChoi H, Kim CJ, Na CH, Shin BS, Kim MS. A Case of Exfoliative Vesiculobullous Prurigo Pigmentosa Cured by Doxycycline and Topical Tacrolimus. Case reports in dermatology. 2021 Sep-Dec:13(3):474-480. doi: 10.1159/000512708. Epub 2021 Sep 23 [PubMed PMID: 34720921]
Level 3 (low-level) evidenceTorrelo A, Azorín D, Noguera L, Hernández-Martín A, Happle R, Requena L. Segmental prurigo pigmentosa. Pediatric dermatology. 2014 Jul-Aug:31(4):523-5. doi: 10.1111/pde.12349. Epub 2014 May 20 [PubMed PMID: 24846714]
Level 3 (low-level) evidenceTeraki Y, Hitomi K. Unilateral prurigo pigmentosa: A report of two cases. The Journal of dermatology. 2016 Jul:43(7):846-7. doi: 10.1111/1346-8138.13289. Epub 2016 Feb 12 [PubMed PMID: 26872306]
Level 3 (low-level) evidenceMehta H, Bishnoi A, Vinay K, Kaushik A, Kumaran MS, Kollabathula A, Chatterjee D, Saikia UN, Parsad D. Prurigo Pigmentosa: Dermoscopic Evaluation. Dermatology practical & conceptual. 2021 Oct:11(4):e2021115. doi: 10.5826/dpc.1104a115. Epub 2021 Oct 1 [PubMed PMID: 35024228]
Deng XY, Yi M, Li WG, Ye HY, Chen ZS, Zhang XD. The prevalence, hospitalization outcomes and risk factors of euthyroid sick syndrome in patients with diabetic ketosis/ketoacidosis. BMC endocrine disorders. 2023 Sep 12:23(1):195. doi: 10.1186/s12902-023-01451-x. Epub 2023 Sep 12 [PubMed PMID: 37700304]
Heymann WR. Confluent and reticulated papillomatosis, prurigo pigmentosa, and antibiotic preference. Journal of the American Academy of Dermatology. 2023 Aug:89(2):233-234. doi: 10.1016/j.jaad.2023.05.066. Epub 2023 Jun 2 [PubMed PMID: 37271454]
Yang J, Hu X, Niu M, Zheng X. Prurigo Pigmentosa Successfully Treated with Oral Minocycline: A Case Report. Clinical, cosmetic and investigational dermatology. 2023:16():1073-1077. doi: 10.2147/CCID.S404859. Epub 2023 Apr 24 [PubMed PMID: 37123623]
Level 3 (low-level) evidenceFöhr J, Gschnell M, Cunha T, Hertl M, Didona D. Complete remission of prurigo pigmentosa after oral doxycycline. Dermatologic therapy. 2022 Dec:35(12):e15908. doi: 10.1111/dth.15908. Epub 2022 Oct 23 [PubMed PMID: 36205101]
Level 3 (low-level) evidenceCélérier P, Litoux P, Dréno B. In vitro modulation of epidermal inflammatory cytokines (IL-1 alpha, IL-6, TNF alpha) by minocycline. Archives of dermatological research. 1996 Jun:288(7):411-4 [PubMed PMID: 8818192]
Majmundar VD, Baxi K. Acute Febrile Neutrophilic Dermatosis. StatPearls. 2023 Jan:(): [PubMed PMID: 32644568]
Wozel G, Blasum C. Dapsone in dermatology and beyond. Archives of dermatological research. 2014 Mar:306(2):103-24. doi: 10.1007/s00403-013-1409-7. Epub 2013 Dec 6 [PubMed PMID: 24310318]
Level 3 (low-level) evidenceWallengren J. Prurigo: diagnosis and management. American journal of clinical dermatology. 2004:5(2):85-95 [PubMed PMID: 15109273]
Chu L, Wang L, Wu Y, Yang H, Wang W, Lu Q, Deng H. Plasma Steroids and Endocannabinoids Used as Biomarkers to Assess the Pruritus Severity of Patients With Prurigo Nodularis. Actas dermo-sifiliograficas. 2022 Mar:113(3):T244-T253. doi: 10.1016/j.ad.2021.10.004. Epub 2021 Nov 1 [PubMed PMID: 35331446]
An I, Ucmak D, Ibiloglu I, Demir V, Akdeniz S. Colchicine may be of therapeutic benefit in prurigo pigmentosa. Pediatric dermatology. 2018 May:35(3):e202-e203. doi: 10.1111/pde.13480. Epub 2018 Apr 11 [PubMed PMID: 29644750]
Michaels JD, Hoss E, DiCaudo DJ, Price H. Prurigo pigmentosa after a strict ketogenic diet. Pediatric dermatology. 2015 Mar-Apr:32(2):248-51. doi: 10.1111/pde.12275. Epub 2013 Dec 30 [PubMed PMID: 24372546]
Level 3 (low-level) evidenceMitsuhashi Y, Suzuki N, Kawaguchi M, Kondo S. Prurigo pigmentosa on a patient with soft-drink ketosis. The Journal of dermatology. 2005 Sep:32(9):767-8 [PubMed PMID: 16361724]
Level 3 (low-level) evidenceJang MS, Suh KS, Kwon DI, Jung JH, Seong SH, Lee KH, Kang JH, Park JB. Successful treatment with narrowband ultraviolet B phototherapy in prurigo pigmentosa. Journal of the European Academy of Dermatology and Venereology : JEADV. 2021 Nov:35(11):e796-e798. doi: 10.1111/jdv.17477. Epub 2021 Jul 12 [PubMed PMID: 34166545]
Choi JR, Kim JK, Won CH, Lee MW, Oh ES, Chang S. Prurigo pigmentosa treated with Jessner's peel and irradiation with an 830-nm light-emitting diode. The Journal of dermatology. 2012 May:39(5):493-6. doi: 10.1111/j.1346-8138.2011.01368.x. Epub 2011 Nov 13 [PubMed PMID: 22077395]
Level 3 (low-level) evidenceRoss A, Dunn R, Bekhor P, Rodrigues M, Barton C. Prurigo pigmentosa - Response to treatment with Q-Switched neodymium: YAG at 532 nm. The Australasian journal of dermatology. 2019 May:60(2):147-149. doi: 10.1111/ajd.12943. Epub 2018 Oct 30 [PubMed PMID: 30378095]
Akoglu G, Boztepe G, Karaduman A. Prurigo pigmentosa successfully treated with low-dose isotretinoin. Dermatology (Basel, Switzerland). 2006:213(4):331-3 [PubMed PMID: 17135740]
Level 3 (low-level) evidenceRequena Caballero C, Nagore E, Sanmartín O, Botella-Estrada R, Serra C, Guillén C. Vesiculous prurigo pigmentosa in a 13-year-old girl: good response to isotretinoin. Journal of the European Academy of Dermatology and Venereology : JEADV. 2005 Jul:19(4):474-6 [PubMed PMID: 15987297]
Level 3 (low-level) evidenceShetty NP, Taylor SC, Lim HW. Personalized photoprotection: Commentary on "Adjusting best practices in the treatment of melasma with a focus on patients with skin of color". Journal of the American Academy of Dermatology. 2023 Sep:89(3):635-636. doi: 10.1016/j.jaad.2023.05.038. Epub 2023 May 24 [PubMed PMID: 37230365]
Level 3 (low-level) evidenceAltalhi ER, Azhari MS, Aljuhani SS, Baltow BA, Al Hawsawi K. Prurigo Pigmentosa: A Case Report With Unusual Presentation. Cureus. 2022 Dec:14(12):e32242. doi: 10.7759/cureus.32242. Epub 2022 Dec 6 [PubMed PMID: 36620814]
Level 3 (low-level) evidenceKim MH, Choi YW, Choi HY, Myung KB. Prurigo pigmentosa from contact allergy to chrome in detergent. Contact dermatitis. 2001 May:44(5):289-92 [PubMed PMID: 11298695]
Level 3 (low-level) evidenceGambichler T, Doerler M, Scheel CH, Bastek K, Chatzipantazi M. Prurigo pigmentosa (Nagashima disease) in bathing suit distribution mimicking contact dermatitis. Journal of the European Academy of Dermatology and Venereology : JEADV. 2023 Apr:37(4):e472-e473. doi: 10.1111/jdv.18607. Epub 2022 Oct 8 [PubMed PMID: 36165584]
Ishikawa T, Takemoto M, Yokote K. Itchy papules on the back and neck of a young woman. European journal of internal medicine. 2023 Feb:108():97-98. doi: 10.1016/j.ejim.2022.12.012. Epub 2022 Dec 23 [PubMed PMID: 36567231]
Tiao J, Shin G, Al Janahi S, Chung KY, Kim DY, Mun JH, Lee JB, Chung HJ. Skin diseases in Asian individuals that you do not want to miss: A selection of unique or relatively more common conditions in Asian populations. Clinics in dermatology. 2021 Sep-Oct:39(5):879-886. doi: 10.1016/j.clindermatol.2021.05.023. Epub 2021 May 18 [PubMed PMID: 34785016]