Introduction
The pancreas is an abdominal organ possessing both endocrine and exocrine functions. The pancreas produces various hormones that primarily pertain to regulating blood sugar levels. As an exocrine gland, it secretes pancreatic fluid that contains bicarbonate and digestive enzymes. Commonly, a few broad categories of diseases affect the pancreas that can be characterized on imaging: pancreatitis, pancreatic insufficiency, cystic lesions of the pancreas, and pancreatic tumors.[1]
Pancreatitis is a generalized inflammation of the pancreas due to the activation of digestive enzymes produced by the pancreas while still inside the organ. Acutely, this can result from gallstones, alcohol misuse, or hypertriglyceridemia.[2][3] Gallstones are the etiology of the majority of acute pancreatitis cases, 40% to 70%, while alcohol misuse accounts for 25% to 35%.[4][5] Pancreatitis typically presents as an acute onset of epigastric pain that may radiate through to the back. Nausea and vomiting frequently accompany abdominal pain. The revised Atlanta classification separates acute pancreatitis into two subtypes: interstitial edematous pancreatitis and necrotizing pancreatitis.[6] The severity further classifies acute pancreatitis into mild, moderately severe, or severe, based on the absence of organ failure, the presence of transient organ failure, or persistent organ failure, respectively.[7] The mortality rate from acute pancreatitis is approximately 5%, while those with necrotizing pancreatitis see a higher rate at 17%.[8] Chronic pancreatitis can occur in patients with alcohol use disorder, in which scarring of the gland prevents it from functioning properly.[9]
Pancreatic insufficiency results when the pancreas cannot produce enough digestive enzymes to break down food in the digestive tract.[10] This condition is typically a deficiency in the exocrine function of the gland that can be caused by a variety of disease processes, most commonly cystic fibrosis in children and chronic pancreatitis in adults.
Pancreatic exocrine cancer is one of the leading causes of cancer-related deaths in the United States.[11] It also ranks among the most lethal cancers, with a one-year survival rate of 20% and a 5-year survival rate of only 5%.[1] The lethality is mostly due to the insidious onset of the malignancy, with symptoms (eg, jaundice, weight loss, and vague subacute epigastric pain) not present until late in the course of the illness.[12] See Image. Pancreatic Cancer, Courvoisier Sign. Frequently, at the time of diagnosis, the lesion is inoperable due to extension into nearby structures. Over one-third of the tumors are Stage IV upon identification, and less than 20% of these cancers are candidates for surgical resection.[13][14] The most common malignancy is ductal adenocarcinoma involving the exocrine glands; most of these tumors are discovered in the head of the pancreas (see Image. Pancreatic Adenocarcinoma, Computed Tomography).[15]
Pancreatic neuroendocrine tumors (NETs) are malignancies that form in the endocrine tissue of the pancreas. Also known as islet cell tumors, these are rare tumors occurring in approximately 1 in every 100,000 people, and only 1% of all pancreatic tumors are NETs.[16] NETs can result in the overproduction and secretion of pancreatic hormones, including insulin, gastrin, glucagon, and vasoactive intestinal peptide (VIP), resulting in specific clinical syndromes on presentation. See Image. Gastrinoma on Distal Pancreas.
Cystic lesions of the pancreas are a relatively common incidental finding on body imaging, with prevalence in the general population ranging up to 14%.[17] Classification of these cysts is crucial as they can either be true cysts, pseudocysts (usually related to pancreatitis), or related to benign or malignant neoplasms. Radiological imaging has historically helped distinguish the etiology of the cystic lesions in 75% to 90% of presentations.[18] True epithelial cysts are rare in the general population and are classically only associated with cystic fibrosis, von Hippel-Lindau disease, and autosomal dominant polycystic kidney disease. Pseudocysts, related to pancreatitis or trauma, are the most common cystic lesions identified in the pancreas. Approximately 20% to 40% of patients with chronic pancreatitis develop pseudocysts, while only 2% to 3% of those with acute pancreatitis will develop them.[18] Cysts associated with malignancy may rarely occur with exocrine tumors, occasionally with endocrine tumors, or in isolation. Cystic neoplasms include intraductal papillary mucinous neoplasms, mucinous cystic neoplasms, and serous cystadenomas.
Anatomy
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy
The anatomy of the pancreas and nearby structures are particularly important for understanding gallstone pancreatitis and surgical contraindications to pancreatic cancer. The common bile duct enters the pancreas and merges with the main pancreatic duct just before the ampulla of Vater, where they both empty into the second part of the duodenum through the major duodenal papilla.[19] In gallstone pancreatitis, a gallstone that escapes the gallbladder moves down the common bile duct, entering the pancreas. The gallstone can become lodged at the ampulla of Vater, blocking both the common bile duct and the main pancreatic duct from emptying into the duodenum.[20] This blockage will cause bile and pancreatic juice back up, resulting in gallstone pancreatitis.
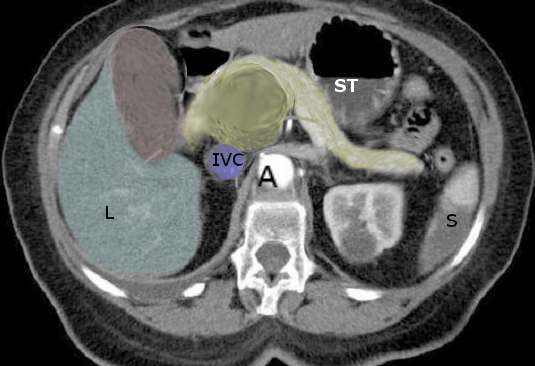
The anatomy of the pancreas and surrounding structures is critical for understanding the surgical indications and contraindications for pancreatic cancer. The head of the pancreas resides in the “C-loop” of the duodenum, with the uncinate process curling back and behind the superior mesenteric artery and vein.[21] The pancreatic neck crosses over the inferior vena cava and aorta near the celiac trunk, while the tail continues to traverse to the left side of the abdomen, along with the splenic artery, terminating at or near the splenic hilum. The stomach sits in front of the pancreas. These nearby structures, particularly the celiac axis and superior mesenteric vessels near the head of the pancreas, can become involved in a rapidly enlarging pancreatic malignancy, complicating the surgical approach or making it inoperable.[22]
Plain Films
The use of plain radiographs is extremely limited in evaluating the pancreas. Although not diagnostic, calcifications of the pancreas may be visible on abdominal radiographs in the setting of chronic pancreatitis.[23]
Computed Tomography, Magnetic Resonance Imaging, and Ultrasound
A few general principles common to imaging in various body parts are essential when deciding which of these three cross-sectional modalities to use and the relative strengths and weaknesses of each. In general, CT and MRI have large fields of view and are both very effective in identifying local abnormalities along with regional or more distant involvement.[24] Ultrasound has a limited field of view and can be subject to substantial limitations by body habitus and overlying gas.[25]
CT and MR are better than ultrasound for characterizing solid lesions due to the advantage of administering intravenous contrast material and differences in signal intensity seen on MRI. On the other hand, cystic lesions can be detected with all three modalities but are better characterized by ultrasound and even better by MRI.[26]
Computed Tomography
Computed tomography (CT) is the backbone of pancreatic imaging. Intravenous contrast is nearly always indicated with multiphase-enhanced imaging and is optimal for identifying and characterizing pancreatic masses or complications from pancreatitis. Multiphase pancreas protocols usually include an unenhanced sequence, a ‘pancreas phase’ or late-arterial phase, and portal venous phase sequences.[27]
In acute pancreatitis, intravenous contrast-enhanced CT will show focal or diffuse enlargement of the pancreatic parenchyma due to interstitial edema, with heterogeneous enhancement.[28] The pancreatic margins will be ill-defined due to inflammation, and peripancreatic fat stranding may also be present. An obstructing gallstone may or may not be visible if that is the cause of pancreatitis. Complications may be seen acutely or delayed, including necrosis, hemorrhage, vascular complications, pancreatic pseudocysts, and abscess formation. Areas that lack contrast enhancement are diagnostic of pancreatic necrosis.[29] Visualization of necrotic pancreatitis is best between 48 and 72 hours after onset; therefore, early scanning in acute pancreatitis might under-call patients with necrosis.[30] Initial imaging is recommended to be performed 5 to 7 days after hospital admission.[7] In cases of infected necrosis, gas bubbles may be apparent, which is pathognomonic for emphysematous pancreatitis. Hemorrhagic pancreatitis can present radiographically as a fluid of high attenuation on unenhanced CT, with the attenuation decreasing as the blood ages.[31] Vascular complications include portal vein thrombosis, which is identifiable as either no enhancement or a filling defect of the portal vein. An additional vascular complication is aneurysm formation of any of the peripancreatic arteries.
Regarding chronic pancreatitis, findings may include a dilated main pancreatic duct, atrophy of the pancreatic parenchyma, and pancreatic calcifications. While pancreatic atrophy occurs in approximately 54% of patients with chronic pancreatitis, this is not a specific finding and can also occur with normal aging.[32] Pancreatic pseudocysts typically present as a unilocular fluid collection without enhancing solid components.[18]
Nearly nine out of ten cystic fibrosis patients experience pancreatic exocrine gland insufficiency due to ductal obstruction and subsequent fibrosis and fatty replacement. This blockage can cause acute pancreatitis when residual pancreatic exocrine function remains. CT imaging can reveal fatty replacement of the pancreas, which appears as fat (low) attenuation areas (see Image. Fatty Replacement of Pancreas Seen on Computed Tomography). Eventually, the continuing fatty replacement can lead to complete pancreatic lipomatosis, typically before the patient reaches 20 years of age.[33] Calcifications and small pancreatic cysts may also be present. True epithelial cysts generally have no internal septa or enhancement post-intravenous contrast administration.
When evaluating pancreatic exocrine tumors, the ‘pancreas phase’ sequence best accentuates the attenuation difference between the malignancy and the healthy pancreatic tissue due to the tumor’s hypovascularity.[34] The masses will appear on CT as ill-defined. The lesion is usually hypodense throughout arterial phase sequences, although up to 10% of tumors, especially those less than 2 cm, will be isodense compared to the normal pancreatic parenchyma.[35][36] Associated signs, such as pancreatic duct cutoff and the double duct sign, may also be visible. The overall reported sensitivity of CT in detecting pancreatic cancer is 89 to 97%,[14] with a positive predictive value of 89% in predicting the surgical resectability of the tumor.[35]
Multiphase, contrast-enhanced CT is also the ideal imaging technique for evaluating pancreatic neuroendocrine tumors. NETs are highly vascular tumors that will enhance during the arterial or pancreatic phase. Washout should be noted during the portal venous phase sequencing.[31] Smaller tumors are well-circumscribed, homogeneous masses on CT; however, larger NETs can have a variety of appearances due to necrosis, cystic changes, or hemorrhage. Isolated cystic neoplasms are potentially visible via CT; however, characterization is usually more effective with magnetic resonance imaging.[37] Intraductal papillary mucinous neoplasms (IPMN) may show pancreatic ductal dilation or cystic lesions. The cystic lesions are typically hypoattenuating and heterogeneous. Mucinous cystic neoplasms will also present as hypoattenuating but will often display a thick enhancing wall on delayed imaging. Serous cystadenomas may have a central scar with ‘sunburst calcifications’ extending out from the central focus in up to 30% of cases.[18]
Magnetic Resonance
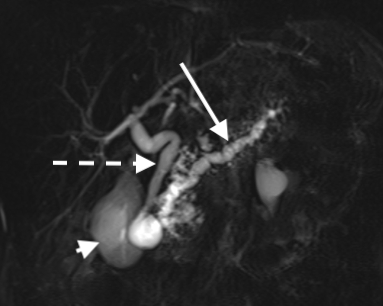
Although CT is the initial modality for diagnosing pancreatic abnormalities, MRI is beneficial for characterizing cystic lesions and characterizing and even identifying some solid tumors, particularly smaller ones. [38] Additionally, magnetic resonance cholangiopancreatography (MRCP) can better visualize the pancreatic and biliary ducts and demonstrate any communication or obstruction related to a lesion (see Image. Chronic Pancreatitis via MRCP). Typical pancreatic MR protocol includes T1- and T2-weighted images with multiphasic imaging after intravenous gadolinium administration.[38]
Pancreatitis evaluation in the acute setting is nearly always with CT; however, MRI is comparable to CT and can be useful in some complicated cases or patients who cannot receive iodinated contrast. Fat-suppressed T2-weighted sequences demonstrate more significant differentiation between pancreatic and peripancreatic tissues, making any peripancreatic inflammation much more conspicuous.[39] T2-weighted images can also help distinguish simple appearing pseudocysts from more internally complex walled-off necrosis.[40] MRCP can demonstrate pancreatic and bile ducts and gallstone detection with higher sensitivity than CT. Fat-suppressed, T1-weighted images will reveal focal or diffuse enlargement of the pancreatic parenchyma with ill-defined borders, similar to findings on CT. Due to inflammation and edema, the inflamed pancreatic parenchyma will be hypointense compared to the normal pancreas or the liver on T1 and hyperintense on T2. Necrosis will appear hypointense on T2-weighted images and hyperintense when liquified.[3] Hemorrhage can be visualized via fat-suppressed T1 and T2-weighted images, but gradient-recalled echo (GRE) sequences are also extremely sensitive to the magnetic properties of hemoglobin.[31] Gadolinium-enhanced T1-weighted images will be best for assessing necrosis and the extent of inflammation.
MRCP is increasingly used to diagnose chronic pancreatitis due to its ability to visualize pancreatic duct obstruction and dilation; however, the typical calcifications in chronic pancreatitis are not visualized as effectively as on CT. [41] Pancreatic atrophy can be seen as irregular margins of the pancreas and decreased T1-weighted signal with delayed enhancement post-gadolinium injection. Secretin-enhanced MRCP (sMRCP) provides better visualization of the main pancreatic duct and its branches. Pancreatic duct flow rates can also be evaluated with sMRCP.[32] Pseudocysts will present as hyperintense lesions on T2-weighted images, while pseudocysts containing blood will demonstrate an increased signal on T1-weighted sequences.[18]
MR can help differentiate pancreatic lipomatosis from fibrotic changes in cystic fibrosis patients. Fibrotic replacement of the pancreas will appear as hypointense areas on T1- and T2-weighted imaging, while fatty changes will reveal the opposite: hyperintensity on both T1- and T2-weighted sequences.[33]
Pancreatic adenocarcinomas appear hypointense on T1-weighted images vis-a-vis the normally bright appearance of the healthy pancreas. There is less utility of T2-weighted images as the signal is similar to the normal pancreas. Diffusion-weighted images can show restricted diffusion of adenocarcinomas, but restricted diffusion is not specific to carcinomas as it can also present in pancreatitis.[35] However, utilizing diffusion gradients with lower b-values, correlating with lower amplitudes, shorter durations, and shorter intervals between gradient pulses may accentuate subtle T2-weighted signal abnormalities. MRCP may reveal ductal obstruction in the area of a suspected small mass. The double duct sign of simultaneous dilation of the common bile and pancreatic ducts may also be visible.[42]
Pancreatic NETs appear on MRI as hypointense on T1- and hyperintense on T2-weighted images with hyperenhancement after gadolinium administration on arterial or pancreatic phase timing due to their hypervascular nature. Large islet cell tumors may have areas of cystic or necrotic nonenhancement.[43] MRI can further characterize cystic neoplasms.[44] IPMNs should show either main pancreatic ductal dilation (diffuse or segmental) or a multi-cystic lobulated mass. Mucinous cystic neoplasms appear congruent with simple cystic fluid collections that may have fluid-fluid levels on T2-weighted images. Postcontrast T1-weighted sequences may show enhancing mural nodules within the lesion. The main pancreatic duct is usually not involved. Serous cystadenoma will typically reveal numerous small cysts that are hyperintense on T2-weighted images. Thin septa may enhance, and if a central scar is present, it will enhance on delayed imaging.[18]
Lastly, in cases of biliary ductal dilation, MRCP can help differentiate an obstructing gallstone (no enhancement and dark on T2) or intraluminal mass (enhancing mass without dark T2-weighted signal).
Ultrasonography
Transabdominal ultrasound’s main role in acute pancreatitis is identifying gallstones and choledocholithiasis. Otherwise, ultrasound has limited use in significant measure due to difficult visualization of the pancreas, often due to overlying bowel gas.[45] The inflamed pancreas will appear hypoechoic and diffusely enlarged due to edema. Anechoic and hypoechoic fluid collections may be present in severe disease, representing peripancreatic fluid.
On the other hand, endoscopic ultrasound (EUS) may be useful in the setting of chronic pancreatitis evaluation.[46] Features of the pancreatic parenchyma include hyperechoic foci/strands due to fibrosis and cysts. Dilation of the main pancreatic duct over 3 mm may be visible, with areas of focal narrowing and hyperechoic margins representing periductal fibrosis. Side branches of the main duct may also be dilated with a diameter over 1 mm. EUS is highly sensitive for detecting changes in the normal pancreatic architecture; however, limitations are mainly due to operator variability and its more invasive nature.[32] Pseudocysts manifest as unilocular, anechoic lesions with thin walls.
Pancreatic lipomatosis, in the setting of cystic fibrosis, classically shows increased pancreatic echogenicity on ultrasonography. The characteristic lobular architecture of the pancreas may also appear diminished.[33]
Transabdominal ultrasound is not an uncommon initial imaging modality for a patient with jaundice, epigastric pain, or weight loss, as ultrasound is highly sensitive for detecting obstruction of the biliary tract and resultant dilation. If these symptoms are due to a pancreatic carcinoma, the mass usually appears as an ill-defined hypoechoic hypovascular structure with or without ductal dilation.[35]
Ultrasound’s place in the evaluation of pancreatic NETs is uncertain. However, these well-circumscribed, hypoechoic, and hypervascular lesions can sometimes be seen on ultrasound, even if their morphology is nonspecific. EUS can be helpful in the setting of both exocrine and endocrine tumors, as biopsy via FNA can be performed during the ultrasound.[47] Differentiating various cystic lesions via EUS alone may be challenging. However, when using EUS in conjunction with fine-needle aspiration (FNA), it is the most effective means of classifying cystic lesions of the pancreas, with specificity greater than 90%.[18] Morphologically, mucinous cystic neoplasms may be unique in demonstrating internal septa with differing thicknesses and containing hyperechoic internal debris. Microcystic serous cystadenomas have highly specific features for their etiology: multiple demarcated anechoic cystic lesions separated by thin septa resulting in a ‘honeycomb’ appearance that is not associated with the pancreatic ducts.[18] Alternatively, via ultrasonography, macro cystic serous cystadenomas may look very similar to IPMNs and mucinous cystic neoplasms.
Nuclear Medicine
In patients with NETs, nuclear medicine studies may be necessary for further staging and characterization of the lesion.[48] Historically, octreotide scans have been performed, in which octreotide (a somatostatin analog) is linked to the tracer indium-111 and injected before imaging. This modality evolved into indium-111 octreotide coupled with single-photon emission computed tomography (SPECT). More recently, somatostatin receptor (SSTR) positron emission tomography (PET) is being increasingly utilized due to improved sensitivity for detecting small lesions, decreased radiation dose, and its ability to quantify uptake. SSTR PET uses Ga-DOTATATE and Ga-DOTATOC tracers, which both have high affinities for subtype 2 SSTRs.[49] SSTR PET can also be coupled with MRI or CT for greater spatial resolution.
Clinical Significance
The differential of pancreatic disease processes is challenging, but it can demonstrate significant morbidity and mortality in the population. Understanding the various imaging modalities available and when each is appropriate is critically important. CT and MR provide an excellent spatial resolution of the pancreatic anatomy and are the modalities of choice when considering the pancreas. EUS-FNA is highly specific and valuable in diagnosing pancreatic cystic lesions.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Low G, Panu A, Millo N, Leen E. Multimodality imaging of neoplastic and nonneoplastic solid lesions of the pancreas. Radiographics : a review publication of the Radiological Society of North America, Inc. 2011 Jul-Aug:31(4):993-1015. doi: 10.1148/rg.314105731. Epub [PubMed PMID: 21768235]
Shanbhogue AK, Fasih N, Surabhi VR, Doherty GP, Shanbhogue DK, Sethi SK. A clinical and radiologic review of uncommon types and causes of pancreatitis. Radiographics : a review publication of the Radiological Society of North America, Inc. 2009 Jul-Aug:29(4):1003-26. doi: 10.1148/rg.294085748. Epub [PubMed PMID: 19605653]
Türkvatan A, Erden A, Türkoğlu MA, Seçil M, Yener Ö. Imaging of acute pancreatitis and its complications. Part 1: acute pancreatitis. Diagnostic and interventional imaging. 2015 Feb:96(2):151-60. doi: 10.1016/j.diii.2013.12.017. Epub 2014 Feb 8 [PubMed PMID: 24512896]
Forsmark CE, Baillie J, AGA Institute Clinical Practice and Economics Committee, AGA Institute Governing Board. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007 May:132(5):2022-44 [PubMed PMID: 17484894]
Yang AL, Vadhavkar S, Singh G, Omary MB. Epidemiology of alcohol-related liver and pancreatic disease in the United States. Archives of internal medicine. 2008 Mar 24:168(6):649-56. doi: 10.1001/archinte.168.6.649. Epub [PubMed PMID: 18362258]
Thoeni RF. The revised Atlanta classification of acute pancreatitis: its importance for the radiologist and its effect on treatment. Radiology. 2012 Mar:262(3):751-64. doi: 10.1148/radiol.11110947. Epub [PubMed PMID: 22357880]
Foster BR, Jensen KK, Bakis G, Shaaban AM, Coakley FV. Revised Atlanta Classification for Acute Pancreatitis: A Pictorial Essay. Radiographics : a review publication of the Radiological Society of North America, Inc. 2016 May-Jun:36(3):675-87. doi: 10.1148/rg.2016150097. Epub [PubMed PMID: 27163588]
Banks PA, Freeman ML, Practice Parameters Committee of the American College of Gastroenterology. Practice guidelines in acute pancreatitis. The American journal of gastroenterology. 2006 Oct:101(10):2379-400 [PubMed PMID: 17032204]
Level 1 (high-level) evidenceBarry K. Chronic Pancreatitis: Diagnosis and Treatment. American family physician. 2018 Mar 15:97(6):385-393 [PubMed PMID: 29671537]
Capurso G, Traini M, Piciucchi M, Signoretti M, Arcidiacono PG. Exocrine pancreatic insufficiency: prevalence, diagnosis, and management. Clinical and experimental gastroenterology. 2019:12():129-139. doi: 10.2147/CEG.S168266. Epub 2019 Mar 21 [PubMed PMID: 30962702]
Mattiuzzi C, Lippi G. Current Cancer Epidemiology. Journal of epidemiology and global health. 2019 Dec:9(4):217-222. doi: 10.2991/jegh.k.191008.001. Epub [PubMed PMID: 31854162]
Oberstein PE, Olive KP. Pancreatic cancer: why is it so hard to treat? Therapeutic advances in gastroenterology. 2013 Jul:6(4):321-37. doi: 10.1177/1756283X13478680. Epub [PubMed PMID: 23814611]
Level 3 (low-level) evidencePorta M, Fabregat X, Malats N, Guarner L, Carrato A, de Miguel A, Ruiz L, Jariod M, Costafreda S, Coll S, Alguacil J, Corominas JM, Solà R, Salas A, Real FX. Exocrine pancreatic cancer: symptoms at presentation and their relation to tumour site and stage. Clinical & translational oncology : official publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico. 2005 Jun:7(5):189-97 [PubMed PMID: 15960930]
Valls C, Andía E, Sanchez A, Fabregat J, Pozuelo O, Quintero JC, Serrano T, Garcia-Borobia F, Jorba R. Dual-phase helical CT of pancreatic adenocarcinoma: assessment of resectability before surgery. AJR. American journal of roentgenology. 2002 Apr:178(4):821-6 [PubMed PMID: 11906855]
McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS. Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment and outcomes. World journal of gastroenterology. 2018 Nov 21:24(43):4846-4861. doi: 10.3748/wjg.v24.i43.4846. Epub [PubMed PMID: 30487695]
Klimstra DS. Nonductal neoplasms of the pancreas. Modern pathology : an official journal of the United States and Canadian Academy of Pathology, Inc. 2007 Feb:20 Suppl 1():S94-112 [PubMed PMID: 17486055]
Mizuno S, Isayama H, Nakai Y, Yoshikawa T, Ishigaki K, Matsubara S, Yamamoto N, Ijichi H, Tateishi K, Tada M, Hayashi N, Koike K. Prevalence of Pancreatic Cystic Lesions Is Associated With Diabetes Mellitus and Obesity: An Analysis of 5296 Individuals Who Underwent a Preventive Medical Examination. Pancreas. 2017 Jul:46(6):801-805. doi: 10.1097/MPA.0000000000000833. Epub [PubMed PMID: 28609369]
Kucera JN, Kucera S, Perrin SD, Caracciolo JT, Schmulewitz N, Kedar RP. Cystic lesions of the pancreas: radiologic-endosonographic correlation. Radiographics : a review publication of the Radiological Society of North America, Inc. 2012 Nov-Dec:32(7):E283-301. doi: 10.1148/rg.327125019. Epub [PubMed PMID: 23150863]
Strazzabosco M, Fabris L. Functional anatomy of normal bile ducts. Anatomical record (Hoboken, N.J. : 2007). 2008 Jun:291(6):653-60. doi: 10.1002/ar.20664. Epub [PubMed PMID: 18484611]
Level 3 (low-level) evidenceTakano Y, Nagahama M, Maruoka N, Yamamura E, Ohike N, Norose T, Takahashi H. Clinical features of gallstone impaction at the ampulla of Vater and the effectiveness of endoscopic biliary drainage without papillotomy. Endoscopy international open. 2016 Jul:4(7):E806-11. doi: 10.1055/s-0042-109265. Epub [PubMed PMID: 27556102]
Talathi SS, Zimmerman R, Young M. Anatomy, Abdomen and Pelvis, Pancreas. StatPearls. 2024 Jan:(): [PubMed PMID: 30422507]
Masiak-Segit W, Rawicz-Pruszyński K, Skórzewska M, Polkowski WP. Surgical treatment of pancreatic cancer. Polski przeglad chirurgiczny. 2018 Apr 30:90(2):45-53. doi: 10.5604/01.3001.0011.7493. Epub [PubMed PMID: 29773761]
Kamat R, Gupta P, Rana S. Imaging in chronic pancreatitis: State of the art review. The Indian journal of radiology & imaging. 2019 Apr-Jun:29(2):201-210. doi: 10.4103/ijri.IJRI_484_18. Epub [PubMed PMID: 31367093]
van Beek EJ, Hoffman EA. Functional imaging: CT and MRI. Clinics in chest medicine. 2008 Mar:29(1):195-216, vii. doi: 10.1016/j.ccm.2007.12.003. Epub [PubMed PMID: 18267192]
Dimcevski G, Erchinger FG, Havre R, Gilja OH. Ultrasonography in diagnosing chronic pancreatitis: new aspects. World journal of gastroenterology. 2013 Nov 14:19(42):7247-57. doi: 10.3748/wjg.v19.i42.7247. Epub [PubMed PMID: 24259955]
Level 3 (low-level) evidencePinho DF, Rofsky NM, Pedrosa I. Incidental pancreatic cysts: role of magnetic resonance imaging. Topics in magnetic resonance imaging : TMRI. 2014 Apr:23(2):117-28. doi: 10.1097/RMR.0000000000000018. Epub [PubMed PMID: 24690615]
Boland GW, O'Malley ME, Saez M, Fernandez-del-Castillo C, Warshaw AL, Mueller PR. Pancreatic-phase versus portal vein-phase helical CT of the pancreas: optimal temporal window for evaluation of pancreatic adenocarcinoma. AJR. American journal of roentgenology. 1999 Mar:172(3):605-8 [PubMed PMID: 10063844]
Thoeni RF. Imaging of Acute Pancreatitis. Radiologic clinics of North America. 2015 Nov:53(6):1189-208. doi: 10.1016/j.rcl.2015.06.006. Epub 2015 Aug 5 [PubMed PMID: 26526433]
Shinagare AB, Ip IK, Raja AS, Sahni VA, Banks P, Khorasani R. Use of CT and MRI in emergency department patients with acute pancreatitis. Abdominal imaging. 2015 Feb:40(2):272-7. doi: 10.1007/s00261-014-0210-1. Epub [PubMed PMID: 25078061]
Level 2 (mid-level) evidenceShyu JY, Sainani NI, Sahni VA, Chick JF, Chauhan NR, Conwell DL, Clancy TE, Banks PA, Silverman SG. Necrotizing pancreatitis: diagnosis, imaging, and intervention. Radiographics : a review publication of the Radiological Society of North America, Inc. 2014 Sep-Oct:34(5):1218-39. doi: 10.1148/rg.345130012. Epub [PubMed PMID: 25208277]
Sahni VA, Mortelé KJ. The bloody pancreas: MDCT and MRI features of hypervascular and hemorrhagic pancreatic conditions. AJR. American journal of roentgenology. 2009 Apr:192(4):923-35. doi: 10.2214/AJR.08.1602. Epub [PubMed PMID: 19304696]
Anaizi A, Hart PA, Conwell DL. Diagnosing Chronic Pancreatitis. Digestive diseases and sciences. 2017 Jul:62(7):1713-1720. doi: 10.1007/s10620-017-4493-2. Epub 2017 Mar 17 [PubMed PMID: 28315036]
Lavelle LP, McEvoy SH, Ni Mhurchu E, Gibney RG, McMahon CJ, Heffernan EJ, Malone DE. Cystic Fibrosis below the Diaphragm: Abdominal Findings in Adult Patients. Radiographics : a review publication of the Radiological Society of North America, Inc. 2015 May-Jun:35(3):680-95. doi: 10.1148/rg.2015140110. Epub 2015 Apr 24 [PubMed PMID: 25910185]
Brennan DD, Zamboni GA, Raptopoulos VD, Kruskal JB. Comprehensive preoperative assessment of pancreatic adenocarcinoma with 64-section volumetric CT. Radiographics : a review publication of the Radiological Society of North America, Inc. 2007 Nov-Dec:27(6):1653-66 [PubMed PMID: 18025509]
Lee ES, Lee JM. Imaging diagnosis of pancreatic cancer: a state-of-the-art review. World journal of gastroenterology. 2014 Jun 28:20(24):7864-77. doi: 10.3748/wjg.v20.i24.7864. Epub [PubMed PMID: 24976723]
Yoon SH, Lee JM, Cho JY, Lee KB, Kim JE, Moon SK, Kim SJ, Baek JH, Kim SH, Kim SH, Lee JY, Han JK, Choi BI. Small (≤ 20 mm) pancreatic adenocarcinomas: analysis of enhancement patterns and secondary signs with multiphasic multidetector CT. Radiology. 2011 May:259(2):442-52. doi: 10.1148/radiol.11101133. Epub 2011 Mar 15 [PubMed PMID: 21406627]
Level 2 (mid-level) evidenceLana S, Vallara M, Bono NE, Russo G, Artioli G, Capretti G, Paladini I, Pesce A, Ruggirello M, Barbalace S, Mostardi M. MRI findings of intraductal papillary mucinous neoplasms (IPMNs). Acta bio-medica : Atenei Parmensis. 2016 Jul 28:87 Suppl 3():28-33 [PubMed PMID: 27467864]
Jang KM, Kim SH, Kim YK, Park MJ, Lee MH, Hwang J, Rhim H. Imaging features of small (≤ 3 cm) pancreatic solid tumors on gadoxetic-acid-enhanced MR imaging and diffusion-weighted imaging: an initial experience. Magnetic resonance imaging. 2012 Sep:30(7):916-25. doi: 10.1016/j.mri.2012.02.017. Epub 2012 Apr 9 [PubMed PMID: 22495239]
Level 3 (low-level) evidenceKim YK, Kim CS, Han YM. Role of fat-suppressed t1-weighted magnetic resonance imaging in predicting severity and prognosis of acute pancreatitis: an intraindividual comparison with multidetector computed tomography. Journal of computer assisted tomography. 2009 Sep-Oct:33(5):651-6. doi: 10.1097/RCT.0b013e3181979282. Epub [PubMed PMID: 19820487]
Level 2 (mid-level) evidenceManikkavasakar S, AlObaidy M, Busireddy KK, Ramalho M, Nilmini V, Alagiyawanna M, Semelka RC. Magnetic resonance imaging of pancreatitis: an update. World journal of gastroenterology. 2014 Oct 28:20(40):14760-77. doi: 10.3748/wjg.v20.i40.14760. Epub [PubMed PMID: 25356038]
Parakh A, Tirkes T. Advanced imaging techniques for chronic pancreatitis. Abdominal radiology (New York). 2020 May:45(5):1420-1438. doi: 10.1007/s00261-019-02191-0. Epub [PubMed PMID: 31428813]
Oterdoom LH, van Weyenberg SJ, de Boer NK. Double-duct sign: do not forget the gallstones. Journal of gastrointestinal and liver diseases : JGLD. 2013 Dec:22(4):447-50 [PubMed PMID: 24369328]
Level 3 (low-level) evidenceHerwick S, Miller FH, Keppke AL. MRI of islet cell tumors of the pancreas. AJR. American journal of roentgenology. 2006 Nov:187(5):W472-80 [PubMed PMID: 17056877]
Lee JE, Choi SY, Min JH, Yi BH, Lee MH, Kim SS, Hwang JA, Kim JH. Determining Malignant Potential of Intraductal Papillary Mucinous Neoplasm of the Pancreas: CT versus MRI by Using Revised 2017 International Consensus Guidelines. Radiology. 2019 Oct:293(1):134-143. doi: 10.1148/radiol.2019190144. Epub 2019 Sep 3 [PubMed PMID: 31478800]
Level 3 (low-level) evidenceBalthazar EJ. Acute pancreatitis: assessment of severity with clinical and CT evaluation. Radiology. 2002 Jun:223(3):603-13 [PubMed PMID: 12034923]
Iglesias-García J, Lariño-Noia J, Lindkvist B, Domínguez-Muñoz JE. Endoscopic ultrasound in the diagnosis of chronic pancreatitis. Revista espanola de enfermedades digestivas. 2015 Apr:107(4):221-8 [PubMed PMID: 25824921]
El Hajj II, LeBlanc JK, Sherman S, Al-Haddad MA, Cote GA, McHenry L, DeWitt JM. Endoscopic ultrasound-guided biopsy of pancreatic metastases: a large single-center experience. Pancreas. 2013 Apr:42(3):524-30. doi: 10.1097/MPA.0b013e31826b3acf. Epub [PubMed PMID: 23146924]
Level 2 (mid-level) evidenceRust E, Hubele F, Marzano E, Goichot B, Pessaux P, Kurtz JE, Imperiale A. Nuclear medicine imaging of gastro-entero-pancreatic neuroendocrine tumors. The key role of cellular differentiation and tumor grade: from theory to clinical practice. Cancer imaging : the official publication of the International Cancer Imaging Society. 2012 May 21:12(1):173-84. doi: 10.1102/1470-7330.2012.0026. Epub 2012 May 21 [PubMed PMID: 22743056]
Hope TA, Bergsland EK, Bozkurt MF, Graham M, Heaney AP, Herrmann K, Howe JR, Kulke MH, Kunz PL, Mailman J, May L, Metz DC, Millo C, O'Dorisio S, Reidy-Lagunes DL, Soulen MC, Strosberg JR. Appropriate Use Criteria for Somatostatin Receptor PET Imaging in Neuroendocrine Tumors. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2018 Jan:59(1):66-74. doi: 10.2967/jnumed.117.202275. Epub 2017 Oct 12 [PubMed PMID: 29025982]