Introduction
An understanding of the histology of the retina is essential to consider for complete insight into diseases involving a vital sensory component in the eye. The complexity of the retina, from its precise multi-layered structure to its various cell types and function, will be discussed briefly in this overview. Also, understanding features involving both structure and function will help appreciate the pathophysiology of disorders affecting the retina. Acknowledging the elements in this article may help guide future investigations towards specific therapeutic targets to help prevent, preserve, and treat irreversible vision loss.
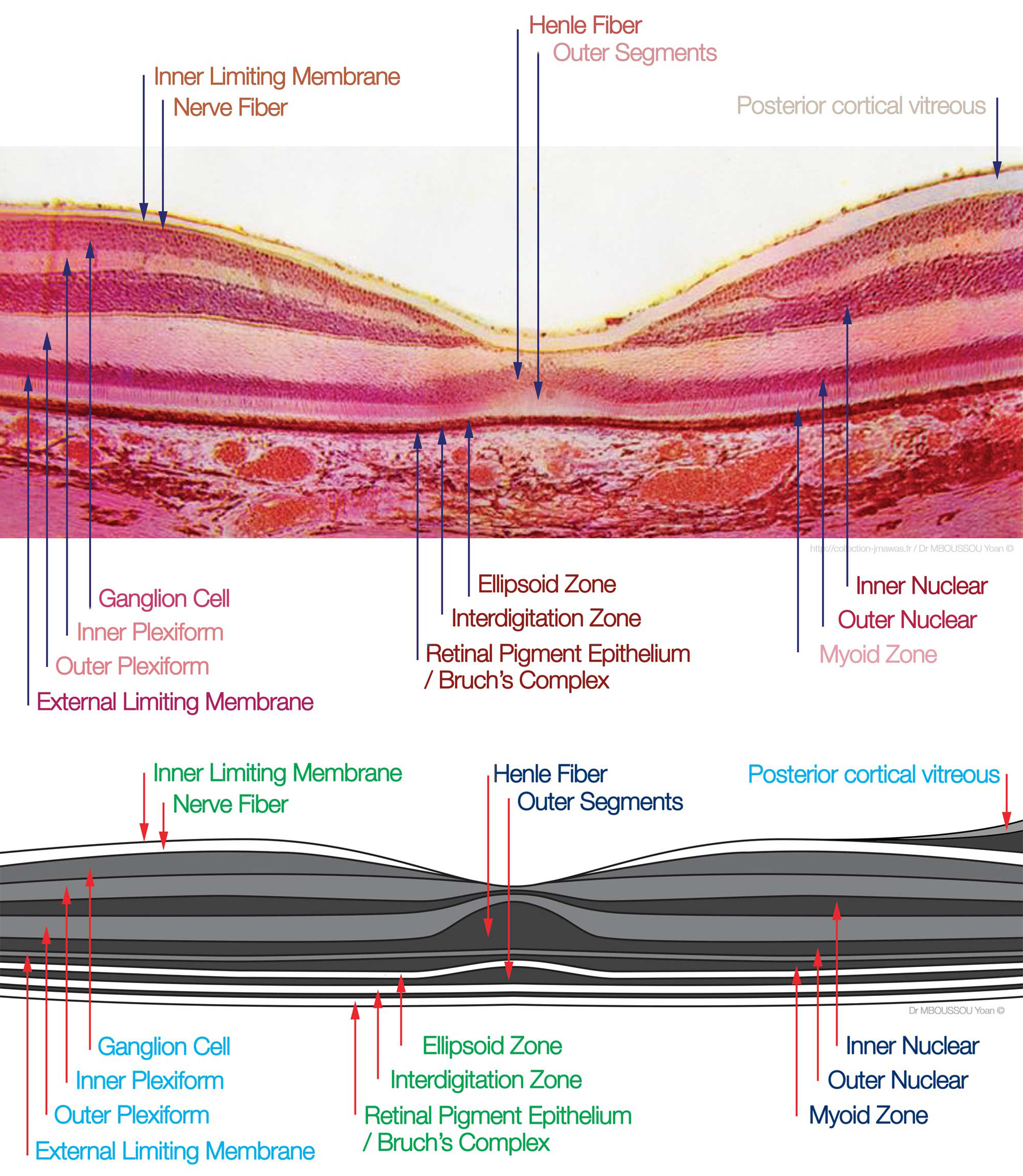
Structure
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure
Six major cell types form the various layers within the human retina [1]:
- Photoreceptors (rods and cones) - form the outer nuclear layer
- Synapse with bipolar cells at the outer plexiform layer
- Rods deal predominantly with peripheral and night vision
- Cones deal mainly with central vision
- Bipolar cells - make up the inner nuclear layer
- Synapse with amacrine cells and ganglion cells at the inner plexiform layer
- Amacrine cells
- Inhibitory cells which interact with bipolar cells and retinal ganglion cells
- Retinal ganglion cells - form the ganglion cell layer (innermost layer, furthest from the photoreceptors)
- Axons tract towards the back of the eye and form the optic nerve
- Horizontal cells
- Assist in operations such as contrast enhancement and preservation of spatial information.[2]
- Muller cells
- glial cells which support metabolism and homeostasis of the retina.[3]
Function
The retina transmits light signals into chemical signals that are sent to the brain. This process requires the ability to sense the stimulus of light and transmit that signal from cell to cell.[1]
Photoreceptors (rods and cones): The detection of light begins at the deepest cell layer in the retina, the photoreceptors, located in the outer nuclear layer. Rods are very light sensitive and are responsible for dim-light vision. Cones, on the other hand, are not very light sensitive but are specific for a particular wavelength of light. Thus, cones are responsible for high acuity color vision.
Bipolar cells: Photoreceptors use the neurotransmitter, glutamate, to communicate at the synapse with bipolar cells within the outer plexiform layer.[4] Bipolar cell bodies are just shallow to this layer at the inner nuclear layer. At the inner plexiform layer, bipolar cells are responsible for transmitting an impulse to retinal ganglion cells.
Retinal ganglion cells: These are the final receivers and transmitters of the initial stimulus. They send the information they receive down their axons, which eventually form the optic nerve and project to higher brain centers.
Amacrine cells: Amacrine cells modulate the excitation of the retinal ganglion cells through contact with ganglion cell dendrites or bipolar cell axon terminal bulbs, using the neurotransmitters GABA and glycine.
Horizontal cells: These cells function to modulate the communication between photoreceptors and bipolar cells. Bipolar cells contact ganglion and amacrine cells at the inner plexiform layer.
Müller cells: These are cells are of glial origin and are essential for proper retinal function. They contact almost every cell type in the retina, spanning the entire width from the photoreceptors to the inner retina. They serve to recycle neurotransmitters, prevent glutamate toxicity, and regulate nutrient homeostasis in the retina.[5]
Tissue Preparation
Retinal tissue can be utilized from post-mortem, enucleated eyes. Following dissection, the retina can undergo fixing via 4% paraformaldehyde (PFA) in 0.1 M phosphate buffer (PB), pH 7.4, for 10 or 30 minutes at room temperature (RT). They can then be stored in sucrose at −20°C for cryoprotection until use. Once vertically sliced, the retina is visualizable with the use of various lab microscopes.[6]
Histochemistry and Cytochemistry
Depending on the investigator's area of interest, various procedures can be used to visualize the retina.
- Haematoxylin-eosin staining - to better visualize cell nuclei and neuron components
- Golgi staining - to label cells based on their pH
- Fluorescent-labeled immunochemistry - to selectively target a specific protein using antibodies.
Fluorescent-labeled immunochemistry has played a significant role in retina histology as well as other fields for its ability to target a certain cell population. The following are proteins isolated in certain retinal cells that can be targetted via antibodies [6]:
- Blue-sensitive opsin (N-terminal peptide) - cones
- Na-K-Cl-Cotransporter (NKCC1) - outer segments of photoreceptors (rods and cones) and horizontal cells
- Calbindin and Parvalbumin (calcium-binding proteins) - horizontal cells
- Syntaxin-4 - outer plexiform layer
Microscopy, Electron
Photoreceptors (rods and cones): Rods and cones contain both an outer and inner segment, and their structural distinction are visible via an electron microscope. The outer segments of rod include a set of membranous discs that resemble a stack of coins.[7] On the other hand, the outer segments of cones contain infoldings of the surface membrane that taper slightly, giving the cones their name.[8] The outer plexiform layer, the connection between the photoreceptors and the bipolar cells, can also be appreciated under electron microscopy.
Bipolar cells: Bipolar cells are unique in that they have both a dendritic process above and an axon terminal below.[9]
Retinal ganglion cells: These cells present as having a large cell body with a dendritic tree.[10]
Amacrine cells: The processes of these cells have characteristics of both axons and dendrites, allowing for pre- and postsynaptic transmission.[11]
Muller cells: These are unique looking cells as they can be characterized by their length, extending from the outer nuclear layer to the most inner retina.[12]
Pathophysiology
Diseases of the retina divide into two categories, those involving the death of photoreceptors (rods and cones) at the outer nuclear layer and those involving cells in the inner retina such as the bipolar and ganglion cells.
Diseases of the photoreceptors (rods and cones) are characterizable by their pattern of cellular and visual loss.
- Retinitis pigmentosa - rods affected first, then cones; peripheral vision loss precedes central loss
- Leber’s congenital amaurosis - rods affected first, then cones OR both rods and cones; peripheral vision loss precedes central loss
- Macular degeneration - RPE (retinal pigment epithelium), cones, & rods affected; central vision loss precedes peripheral loss
- Stargardt disease - RPE, cones, & rods affected; central vision loss precedes peripheral loss
- Cone-rod dystrophy - cones affected first, then rods; peripheral vision loss precedes central loss
- Retinoschisis - rods, cones, & bipolar cells affected; both central and peripheral vision loss
- Congenital stationary night blindness - affects the connection between photoreceptors & bipolar cells, uniform vision loss
Diseases of the inner retina:
- Glaucoma - ganglion cells involved; peripheral vision loss
- Optic nerve neuropathy - ganglion cells involved; uniform vision loss
When viewed using histological methods, retinal pathology can appear structurally disorganized. For example, rosette-like structures can present in diseases of the retina, including retinitis pigmentosa, diabetic retinopathy, and retinoblastoma.[1]
Clinical Significance
When posterior uveitis secondary to infection or malignancy of unknown origin is suspected, chorioretinal biopsy and subsequent histopathological analysis along with appropriate history and physical exams and additional ancillary testing including B-scan ultrasonography, optical coherence tomography (OCT), and fluorescein angiography, can help aid coming to an appropriate diagnosis.[13]
Media
(Click Image to Enlarge)
References
Hoon M, Okawa H, Della Santina L, Wong RO. Functional architecture of the retina: development and disease. Progress in retinal and eye research. 2014 Sep:42():44-84. doi: 10.1016/j.preteyeres.2014.06.003. Epub 2014 Jun 28 [PubMed PMID: 24984227]
Level 3 (low-level) evidenceChapot CA, Euler T, Schubert T. How do horizontal cells 'talk' to cone photoreceptors? Different levels of complexity at the cone-horizontal cell synapse. The Journal of physiology. 2017 Aug 15:595(16):5495-5506. doi: 10.1113/JP274177. Epub 2017 May 18 [PubMed PMID: 28378516]
Lukowski SW, Lo CY, Sharov AA, Nguyen Q, Fang L, Hung SS, Zhu L, Zhang T, Grünert U, Nguyen T, Senabouth A, Jabbari JS, Welby E, Sowden JC, Waugh HS, Mackey A, Pollock G, Lamb TD, Wang PY, Hewitt AW, Gillies MC, Powell JE, Wong RC. A single-cell transcriptome atlas of the adult human retina. The EMBO journal. 2019 Sep 16:38(18):e100811. doi: 10.15252/embj.2018100811. Epub 2019 Aug 22 [PubMed PMID: 31436334]
Matsui K, Hosoi N, Tachibana M. Active role of glutamate uptake in the synaptic transmission from retinal nonspiking neurons. The Journal of neuroscience : the official journal of the Society for Neuroscience. 1999 Aug 15:19(16):6755-66 [PubMed PMID: 10436033]
Level 3 (low-level) evidenceCoughlin BA, Feenstra DJ, Mohr S. Müller cells and diabetic retinopathy. Vision research. 2017 Oct:139():93-100. doi: 10.1016/j.visres.2017.03.013. Epub 2017 Sep 5 [PubMed PMID: 28866025]
Puller C, Manookin MB, Neitz M, Neitz J. Specialized synaptic pathway for chromatic signals beneath S-cone photoreceptors is common to human, Old and New World primates. Journal of the Optical Society of America. A, Optics, image science, and vision. 2014 Apr 1:31(4):A189-94. doi: 10.1364/JOSAA.31.00A189. Epub [PubMed PMID: 24695169]
Level 3 (low-level) evidenceWensel TG, Zhang Z, Anastassov IA, Gilliam JC, He F, Schmid MF, Robichaux MA. Structural and molecular bases of rod photoreceptor morphogenesis and disease. Progress in retinal and eye research. 2016 Nov:55():32-51. doi: 10.1016/j.preteyeres.2016.06.002. Epub 2016 Jun 22 [PubMed PMID: 27352937]
Mustafi D, Engel AH, Palczewski K. Structure of cone photoreceptors. Progress in retinal and eye research. 2009 Jul:28(4):289-302. doi: 10.1016/j.preteyeres.2009.05.003. Epub 2009 Jun 6 [PubMed PMID: 19501669]
Level 3 (low-level) evidenceDowling JE, Boycott BB. Organization of the primate retina: electron microscopy. Proceedings of the Royal Society of London. Series B, Biological sciences. 1966 Nov 15:166(1002):80-111 [PubMed PMID: 4382694]
Level 3 (low-level) evidenceBoycott BB, Wässle H. The morphological types of ganglion cells of the domestic cat's retina. The Journal of physiology. 1974 Jul:240(2):397-419 [PubMed PMID: 4422168]
Level 3 (low-level) evidenceDowling JE. Synaptic organization of the frog retina: an electron microscopic analysis comparing the retinas of frogs and primates. Proceedings of the Royal Society of London. Series B, Biological sciences. 1968 Jun 11:170(1019):205-28 [PubMed PMID: 4385244]
Level 3 (low-level) evidenceUga S, Smelser. Comparative study of the fine structure of retinal Müller cells in various vertebrates. Investigative ophthalmology. 1973 Jun:12(6):434-48 [PubMed PMID: 4541022]
Level 3 (low-level) evidenceJohnston RL, Tufail A, Lightman S, Luthert PJ, Pavesio CE, Cooling RJ, Charteris D. Retinal and choroidal biopsies are helpful in unclear uveitis of suspected infectious or malignant origin. Ophthalmology. 2004 Mar:111(3):522-8 [PubMed PMID: 15019330]
Level 3 (low-level) evidence