Introduction
The Eustachian tube (ET), named after Italian anatomist Bartolomeo Eustachio, is a fibrocartilaginous duct connecting the middle ear (posterior to the eardrum) to the nasopharynx. Also known as the pharyngotympanic tube, the Eustachian tube is approximately 36 mm long, 2-3 mm wide, and functions primarily in optimizing middle ear sound transmission and equalizing pressures within the ear. Normally a closed structure, the Eustachian tube opens in response to movement of the mandible and pharynx, such as during chewing or swallowing.[1]
Structurally, the Eustachian tube has osseous (anteroinferior) and cartilaginous (posterosuperior) portions, is comprised of cartilage and mucosa, and is supported by surrounding soft tissue, the sphenoid sulcus, and peritubal muscles (tensor veli palatini, levator veli palatini, salpingopharyngeus, and tensor tympani).[2] See Image. Temporal Bone, Coronal View.
Cellular Level
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Cellular Level
The anteroinferior portion of the Eustachian tube, which includes the protympanum, mesotympanum, and hypotympanum, is covered by a pseudostratified epithelial layer with numerous mucous and ciliated cells that aid in the mucociliary clearance of pathogens. The connective tissue in this portion of the ET is thick and dense.
The posterosuperior portion of the Eustachian tube contains loose connective tissue and is covered by richly vascularized cuboidal epithelium devoted primarily to gas exchange. There are no ciliated or mucous cells in this portion of the ET.[2]
Development
The Eustachian tube develops as a connection between the lateral extension of the first pharyngeal pouch endoderm and the first branchial cleft ectoderm. The expansion of the pouch forms the tubotympanic recess, which will eventually develop into the middle ear.[3] The surrounding fibrocartilaginous tissue and muscles associated with the Eustachian tube form from the mesoderm.
During normal growth and maturity into early adulthood, an individual's skull base extends caudally, causing the angle of the Eustachian tube to change from horizontal to oblique. This results in elongation and an increased angle of the Eustachian tube with respect to the horizontal plane. From childhood to adulthood, the eustachian tube volume increases from approximately 62 cubic mm to 111 cubic mm (+/- 22 cubic mm in both childhood and adulthood).[4]
Function
The primary function of the Eustachian tube is to equalize air pressure between the atmosphere and the middle ear. Yawning and swallowing cause contraction of the muscles connected to the Eustachian tube, enabling the tube to open to small amounts of air. This opening allows for the equalization of pressure between the atmosphere and the middle ear, resulting in a “popping” sound. The equalizing of middle ear pressure is crucial to the proper workings of the eardrum. With equalized air pressure, the eardrum can vibrate appropriately and transmit sound. Additionally, by functioning as microturbinates, mucosal folds in the Eustachian tube lumen work in conjunction with the surface cilia to promote the clearance of secretions from the middle ear to the nasopharynx.
Furthermore, the Eustachian tube functions in the protection of inner ear structures. The ET links the sterile middle ear to the unsterile outside world, performing four additional specific functions.[2]
- Local immune defense
- Mechanical protection against rhinopharyngeal secretions and pathogenic microorganism reflux
- Protection against the retrograde propagation of vocal sounds
- Mucociliary clearance of middle ear secretions into the rhinopharynx
In simple terms, the anteroinferior portion of the Eustachian tubes primarily functions in the mucociliary clearance process. In contrast, the posterosuperior portion of the Eustachian tube primarily functions in gas exchange.
Mechanism
While the Eustachian tube is closed at rest, it relies on its interaction with two muscles to help facilitate its opening; the tensor veli palatini and the levator veli palatini. The tensor veli palatini contracts the anterolateral wall to cause dilation and opening of the distal Eustachian tube. Contraction of the levator veli palatini results in elevation of the soft palate and medial rotation of the cartilaginous lamina. Simultaneous contractions of these muscles during swallowing or yawning allow air to pass through the ET to equilibrate pressure in the middle ear with the atmosphere.[5]
The pressure discrepancy between the middle ear and the atmosphere is due to the diffusion of atmospheric gases across venous capillary cell membranes in the middle ear. Carbon dioxide and oxygen readily pass through the venous capillary membranes, creating a net pressure vacuum in relation to atmospheric pressure. This explains why dilation of the Eustachian tube allows air at atmospheric pressure to equilibrate with the lower partial pressures of gas in the middle ear that develop. This mechanism also clarifies why exaggerated Eustachian tube dysfunction will result in hearing deficits if a gas exchange deficit occurs in the middle ear, causing the tympanic membrane to tauten. Two additional muscles associated with the Eustachian tube that have not been shown to play a significant role in the opening of the lumen include the tensor tympani and salpingopharyngeus muscles.
Intermittent brief tubal dilation of the ET occurs multiple times per day, occurring approximately 1.4 times/minute and remaining open for approximately 0.4 seconds.
Of note, tubal dilation is facilitated by the presence of surfactants, surface tension-reducing substances found in the mucus of the ET. It is these surfactants that aid in reducing the surface tension of the ET lumen and thus reduce the work required to dilate the tube.[2]
Also of importance in the proper function of the Eustachian tube is the mucociliary clearance of middle ear secretions to the nasopharynx. This process is enhanced as the tube matures and becomes more oblique in angle, allowing gravity to play a role in the drainage process.[6]
Related Testing
The diagnosis of Eustachian tube dysfunction is poorly defined, with no existing comprehensive guidelines. Diagnosis is based on a clinical exam and symptoms specific to Eustachian tube dysfunction. Ideally, a full clinical assessment should include the use of an otoscope, Rinne and Weber tuning forks or pure tone audiometry, and nasopharyngoscopy.[7]
In addition, various imaging studies can aid clinical examination in diagnosing dysfunction. One study, using real-time MRI, was able to visualize the Eustachian tube opening with the Valsalva maneuver in patients with documented dysfunction. Cases of unilateral dysfunction demonstrated normal opening on the unaffected side and failure to open on the affected side. Studies using CT imaging show a reduced cross-sectional area of the osseous portion of the Eustachian tube in patients with documented dysfunction. Another imaging study that shows promising results in diagnosing Eustachian tube dysfunction is scintigraphy, which uses radiolabeled albumin tracers introduced through the tympanic membrane to visualize the patency of drainage from the middle ear.[5]
Tympanogram is another test related to middle ear function that measures tympanic membrane compliance, with an abnormal tympanogram finding indicating increased pressure within the middle ear. Tympanogram is also used to measure the improvement of middle ear function following interventions for Eustachian tube dysfunction.[8]
Pathophysiology
Eustachian tube dysfunction (ETD) is a broad diagnostic category that involves the inability of the ET to open or close appropriately. ETD is often due to an inflammatory response of the epithelium within the lumen caused by two main etiologies; irritant and infectious reactions. Irritant reactions include the response to allergens and chemicals such as smoke, while infectious reactions typically involve a viral or bacterial infection. Both processes release proinflammatory cytokines that promote edema of the epithelium in response to injury. Inflammation resulting in the inability of the Eustachian tube to open results in the failure of gas equilibrium between the middle ear and nasopharynx, leading to hearing impairment or a feeling of fullness in the ear. Whether cause or effect, inflammation of the Eustachian tube also leads to an inability to clear middle ear secretions, resulting in stasis and the potential for developing otitis media.
Common Eustachian tube disorders include:
Patulous Eustachian Tube (tuba aperta) Dysfunction
- A condition in which the ET remains patent (open). While this condition is benign, it can be relatively distressing for the patient, as they experience hearing their voice abnormally loud (autophony) and hearing their own breathing (aerophony). The diagnosis of this condition is made by a history of the symptoms mentioned above and a feeling of ear fullness. These symptoms typically arise during periods of stress or exercise, and patients will typically state that their symptoms resolve with lying down. A patulous ET is usually unilateral, with the ipsilateral eardrum atrophic and moving with respiration. The typical patient scenario is an individual who has undergone severe weight loss, which causes a loss of the fatty tissue surrounding the ET and loss of support. In addition, one-third of women diagnosed with patulous ET dysfunction were pregnant or taking estrogen.[9]
Obstructive Eustachian Tube Dysfunction
- A condition caused by either a functional or anatomical obstruction in which the patency of the ET is decreased. Obstructive ETD typically involves inflammation and mucosal edema caused by environmental allergies, sinusitis, upper respiratory tract infections, or gastroesophageal reflux disease. Due to anatomic differences in the ET between children and adults, acid reflux leading to ETD is found more frequently in infants and children. Repeated exposure to acidic contents can lead to ET inflammation, edema, and obstruction.[10]
- Neoplasms, such as nasopharyngeal carcinoma, can present with unilateral ET obstruction and must be excluded. Benign anatomical obstructive causes may include nasal polyps or adenoid hypertrophy.[11]
- Impaired muscle coordination may also contribute to obstructive ET dysfunction and can be seen in patients with cleft palate.[12]
Baro-Challenge-Induced Eustachian Tube Dysfunction
- A condition caused by failure of the ET to adequately open and regulate middle-ear pressure during ambient pressure changes.[13] Symptoms typically develop when an individual changes altitudes, such as in an airplane, SCUBA diving, or hiking at an increased elevation.
Clinical Significance
The anatomy of the Eustachian tube in infants and young children differs from that of adults in that the ET runs horizontally rather than sloping downward from the middle ear. Because of this anatomical difference, bottle-feeding of infants should be performed with the head elevated to decrease the risk of reflux into the middle ear space. The horizontal course of an infant's ET makes it more difficult for fluid to drain out of the ear and creates a more accessible avenue for bacteria to travel from the mouth to the middle ear space, both of which can culminate in an ear infection. After the age of six, the frequency of ear infections substantially decreases.
As previously discussed, Eustachian tube dysfunction often manifests in the setting of an inflammatory process such as otitis media or rhinosinusitis. Symptoms include tinnitus, distorted or diminished hearing, and pressure in the ear. These symptoms are typically mild and respond to actions that facilitate the normal opening of the tube, such as swallowing or yawning. Theoretically, medications aimed at reducing inflammation, which include corticosteroids, antihistamines, and antibiotics in the setting of an infectious process, may temporarily improve Eustachian tube function; however, the research and evidence for this are underwhelming.[14]
Severe or refractory Eustachian tube dysfunction may require more aggressive treatment that involves healthcare team-based approaches and surgical intervention.
Eustachian Tuboplasty
- The most evidence related to Eustachian tube dysfunction interventional techniques involves Eustachian tuboplasty. One reported approach involves inserting a deflated balloon catheter into the ET using a transnasal endoscopic visualization. The balloon is then filled with saline and remains in situ for two minutes before removal. Results of the procedure were measured regarding the improvement of symptoms, including ear pressure, pain, fullness, and tolerance to pressure changes such as air travel. High levels of symptomatic improvement were noted in patients who had not undergone previous surgery; the intervention demonstrated mixed efficacy for patients with chronic otitis media symptoms. In some studies, Tympanometry was used as an additional objective measure of functional improvement, resulting in a high conversion rate of abnormal tympanogram tracings back to type A (normal function) tympanogram tracings.[15]
Myringotomy
- Myringotomy involves producing an opening in the tympanic membrane designed to relieve pressure buildup in the middle ear. This typically is done with a laser for increased accuracy and control and may involve ventilation tube placement. Studies regarding the efficacy of this technique in relieving middle ear symptoms appear promising; many are too short-term and poorly reported to appropriately conclude the value of the technique.[16]
Tympanostomy
- Tympanostomy is a variation of myringotomy that involves the placement of a tube that traverses the tympanic membrane to ventilate the middle ear space. Tympanostomy tube placement is the most common ambulatory pediatric surgery in the United States. Indications for the procedure include recurrent otitis media refractory to antibiotic use. Otitis media is more common in children because the overall function of the Eustachian tube is decreased due to the natural horizontal angle of childhood. Tympanostomy tube placement is considered a safe and efficacious procedure, providing relief of recurrent otitis media in most patients; otitis media still can occur following placement. Risks related to the procedure involve typical risks associated with anesthesia induction.[16]
Media
(Click Image to Enlarge)
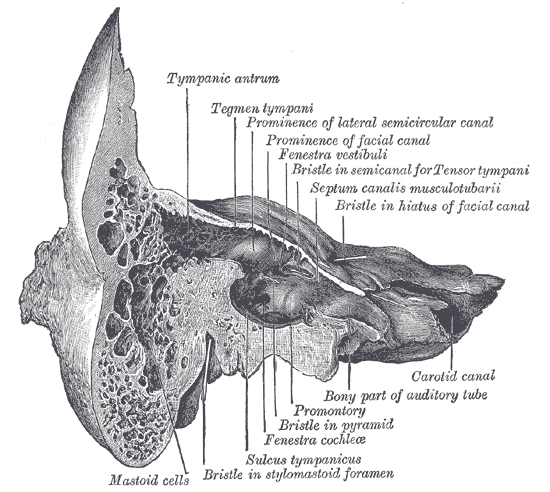
Temporal Bone, Coronal View. This coronal-view illustration of the right temporal bone shows the tympanic antrum, tegmen tympani, prominence of the lateral semicircular canal, prominence of the facial canal, fenestra vestibuli, bristle in semicanal for tensor tympani, septum canalis musculotubarii, bristle in hiatus of the facial canal, carotid canal, bony part of auditory tube, promontory, bristle in pyramid, fenestra cochleae, sulcus tympanicus, bristle in the stylomastoid foramen, and mastoid cells.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Komune N, Matsuo S, Miki K, Akagi Y, Kurogi R, Iihara K, Nakagawa T. Surgical Anatomy of the Eustachian Tube for Endoscopic Transnasal Skull Base Surgery: A Cadaveric and Radiologic Study. World neurosurgery. 2018 Apr:112():e172-e181. doi: 10.1016/j.wneu.2018.01.003. Epub 2018 Jan 8 [PubMed PMID: 29325963]
Ars B, Dirckx J. Eustachian Tube Function. Otolaryngologic clinics of North America. 2016 Oct:49(5):1121-33. doi: 10.1016/j.otc.2016.05.003. Epub 2016 Jul 26 [PubMed PMID: 27468632]
Szymanski A, Geiger Z. Anatomy, Head and Neck, Ear. StatPearls. 2025 Jan:(): [PubMed PMID: 29262017]
Ishijima K, Sando I, Miura M, Balaban CD, Takasaki K, Sudo M. Postnatal development of static volume of the eustachian tube lumen. A computer-aided three-dimensional reconstruction and measurement study. The Annals of otology, rhinology, and laryngology. 2002 Sep:111(9):832-5 [PubMed PMID: 12296340]
Smith ME, Scoffings DJ, Tysome JR. Imaging of the Eustachian tube and its function: a systematic review. Neuroradiology. 2016 Jun:58(6):543-556. doi: 10.1007/s00234-016-1663-4. Epub 2016 Feb 27 [PubMed PMID: 26922743]
Level 1 (high-level) evidenceTarabichi M, Najmi M. Site of eustachian tube obstruction in chronic ear disease. The Laryngoscope. 2015 Nov:125(11):2572-5. doi: 10.1002/lary.25330. Epub 2015 May 9 [PubMed PMID: 25958818]
Schilder AG, Bhutta MF, Butler CC, Holy C, Levine LH, Kvaerner KJ, Norman G, Pennings RJ, Poe D, Silvola JT, Sudhoff H, Lund VJ. Eustachian tube dysfunction: consensus statement on definition, types, clinical presentation and diagnosis. Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2015 Oct:40(5):407-11. doi: 10.1111/coa.12475. Epub [PubMed PMID: 26347263]
Level 3 (low-level) evidenceRosenfeld RM, Schwartz SR, Pynnonen MA, Tunkel DE, Hussey HM, Fichera JS, Grimes AM, Hackell JM, Harrison MF, Haskell H, Haynes DS, Kim TW, Lafreniere DC, LeBlanc K, Mackey WL, Netterville JL, Pipan ME, Raol NP, Schellhase KG. Clinical practice guideline: Tympanostomy tubes in children. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2013 Jul:149(1 Suppl):S1-35. doi: 10.1177/0194599813487302. Epub [PubMed PMID: 23818543]
Level 1 (high-level) evidenceReiss M, Reiss G. [Patulous eustachian tube--diagnosis and therapy]. Wiener medizinische Wochenschrift (1946). 2000:150(22):454-6 [PubMed PMID: 11191956]
De Benedetto M, Monaco G, Marra F. Extra-laryngeal manifestations of gastro-oesophageal reflux. Acta otorhinolaryngologica Italica : organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale. 2006 Oct:26(5):256-9 [PubMed PMID: 17345928]
Hamrang-Yousefi S, Ng J, Andaloro C. Eustachian Tube Dysfunction. StatPearls. 2024 Jan:(): [PubMed PMID: 32310368]
Frisina A, Piazza F, Pasanisi E, Bacciu S, Cerasoli G. [Cleft palate and dysfunction of the eustachian tube]. Acta bio-medica de L'Ateneo parmense : organo della Societa di medicina e scienze naturali di Parma. 1998:69(5-6):129-32 [PubMed PMID: 10702840]
Tailor BV, Smith ME, Hutchinson PJA, Tysome JR. Outcome Measures for Baro-Challenge-Induced Eustachian Tube Dysfunction: A Systematic Review. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2018 Feb:39(2):138-149. doi: 10.1097/MAO.0000000000001666. Epub [PubMed PMID: 29315176]
Level 1 (high-level) evidenceGriffin G, Flynn CA. Antihistamines and/or decongestants for otitis media with effusion (OME) in children. The Cochrane database of systematic reviews. 2011 Sep 7:2011(9):CD003423. doi: 10.1002/14651858.CD003423.pub3. Epub 2011 Sep 7 [PubMed PMID: 21901683]
Level 1 (high-level) evidenceRandrup TS, Ovesen T. Balloon eustachian tuboplasty: a systematic review. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2015 Mar:152(3):383-92. doi: 10.1177/0194599814567105. Epub 2015 Jan 20 [PubMed PMID: 25605694]
Level 1 (high-level) evidenceMcCoul ED, Weinreich HM, Mulder H, Man LX, Schulz K, Shin JJ. Utilization of Invasive Procedures for Adult Eustachian Tube Dysfunction. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2020 Nov:163(5):963-970. doi: 10.1177/0194599820931467. Epub 2020 Jun 11 [PubMed PMID: 32525448]