Introduction
Rapid eye movement behavior disorder (RBD) is a parasomnia involving dream enactment behavior associated with loss of atonia during rapid eye movement (REM) sleep. These symptoms may bring serious harm to the individual themselves and their sleeping partners. RBD has been associated with antidepressant use as well as narcolepsy. The strongest correlation exists between RBD and comorbid neurodegenerative alpha-synucleinopathies (i.e., Parkinson's disease, dementia with Lewy bodies, and multiple system atrophy). Symptoms of RBD may precede neurodegenerative disorders by decades; therefore, a careful history is significant in assessing these patients.[1]
The diagnosis requires confirmation by an in-laboratory sleep study (polysomnography) with video recording, which helps assert abnormal behaviors during REM sleep and excludes other sleep disorders. Counseling and management of RBD focus on injury prevention and the treatment of underlying precipitating disorders in addition to pharmacological treatment of severe cases using oral medications such as melatonin or clonazepam. This topic will review the etiology, epidemiology, pathogenesis, clinical features, evaluation, management, and prognosis of RBD in adults.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Predisposing factors that increase RBD diathesis include elderly age, male sex, narcolepsy, antidepressant use, and neurological disorders. RBD can be divided into three categories:
- Idiopathic RBD
- Drug-induced RBD
- Secondary RBD due to medical condition
Idiopathic RBD is most suggestive in neurodegenerative synucleinopathies, including dementia with Lewy bodies, Parkinson's disease, olivopontocerebellar degeneration, multiple-system atrophy, and Shy-Drager syndrome.[1] The literature suggests that RBD is precipitated by aberrant connections between the brainstem control of muscle tonicity and the cortex.[2] Studies have also suggested associations with traumatic brain injury (TBI), post-traumatic stress syndrome (PTSD), and congenital and neurodevelopmental disorders.[3][4][2]
Drug-induced RBD is common in individuals who are taking antidepressants. The most likely antidepressants that will incite an RBD episode are serotonin reuptake inhibitors (fluoxetine), tricyclic antidepressants (mirtazapine, protriptyline, amitriptyline, nortriptyline, desipramine, imipramine), and monoamine oxidase inhibitors (phenelzine and selegiline).[5][6] Other acute transient forms of RBD involve toxic metabolic encephalopathy—most commonly involving ethanol use.[7]
RBD with concomitant narcolepsy may be considered a distinct phenotype of RBD. It is characterized by less violent or complex behavior during REM sleep, earlier age of onset, equal sex distribution, and hypocretin (orexin) deficiency (a lab diagnosis specific for narcolepsy type 1).[8]
Epidemiology
Studies on RBD, although limited in quantity, suggest a prevalence of 0.5% in the general population.[9][10][11] The prevalence significantly increases in the elderly population, with RBD presenting between 5% and 13% in adults aged 60 to 99.[12]
Among the elderly population, approximately 60% of cases are idiopathic, while 40% of cases are suggestive of an underlying neurologic disorder.[13] The onset of symptoms is typically seen during the sixth or seventh decade of life. There is a male predominance amongst the older population, but there is an equal distribution between males and females under 50 years.[11][14][15]
There is a strong link between RBD and psychiatric disorders. RBD is found to be 5-fold and 10-fold more likely to develop in patients receiving antidepressants and patients with psychiatric disorders, respectively.[16] Some reports linked RBD in childhood to narcolepsy or idiopathic hypersomnia.[17]
RBD has been found in nearly 30 % of young individuals with narcolepsy type I.[18] REM sleep without atonia (RSWA) without clinical symptoms of RBD is not uncommon (2% of the general population)[19] and is more common in those on antidepressants (12%) and older men (25%).[20]
Pathophysiology
A prime feature of rapid eye movement behavior disorder is the intermittent loss of atonia during REM sleep, which leads to dreaming-related motor behaviors. Muscle atonia during normal REM sleep is controlled within the pontine tegmentum and medial medulla. Excitatory glutamatergic neurons within the dorsal pre-coeruleus nucleus activate the spinal cord inhibitory interneurons, thereby initiating REM sleep atonia. Animal models and diagnostic imaging of case reports suggesting interruption or disinhibition of these brainstem areas is the pathophysiology of RBD.[2]
The relationship between RBD and neurodegenerative synucleinopathies is very strong, with an estimated conversion rate from RBD to a neurodegenerative syndrome of 6.3% per year and a total of 74% converting after a 12-year follow-up.[21]
The neurodegenerative alpha-synucleinopathies consist of glial cytoplasmic inclusions aggregates of insoluble alpha-synuclein protein.[2] However, whether the link between this neurodegenerative classification and RBD results from these accumulated aggregates or through another pathology is unclear. Animal studies showed that progressive alpha-synuclein aggregation and neuronal apoptosis occurred in the ventricular reticular nucleus in the brainstem and resulted in RBD symptoms in a chronic rat model of Parkinson disease.[22] There was also a strong association described recently between RBD and synucleinopathies in an extensive series of RBD cases that had an autopsy.[23]
While the relationship between RBD and synucleinopathies is more frequently described, other non-synucleinopathies such as progressive supranuclear palsy (PSP), familial amyotrophic lateral sclerosis, frontotemporal dementia, myotonic dystrophy were also reported but less commonly.[24][25][26][27]
RBD has also been associated with Wilson disease, cerebellar degeneration, and autoimmune encephalitis.[28][29] Some studies suggested that secondary RBD due to paraneoplastic cerebellar degeneration could be immune-mediated, which improved after immunotherapy.[30]
More recently, a novel association between antibodies (mainly IgG4) to a neuronal antigen against IgLON5 (a neuronal cell adhesion molecule) and RBD has been reported suggesting a tauopathy. The more usual presentation includes gait instability followed by dysarthria, dysphagia, ataxia, or chorea, which progress gradually (the median duration between the symptom onset and death is five years).[31] Neural histopathology studies in cases of autoimmune-mediated RBD showed neuronal loss and extensive deposits of hyperphosphorylated tau in the tegmentum of the brainstem and hypothalamus.
The pathogenesis of RBD is distinct in cases of narcolepsy as it is linked to orexin deficiency. In contrast to idiopathic RBD, in cases of RBD-narcolepsy combination, alpha-synuclein biomarkers are usually not detected.[32]
Autoimmune disorder plays an important role in the pathogenesis of RBD (such as in anti-IgLON5 disease).[33] Anti-IgLON5 is a degenerative neurological disorder characterized by neurological (bulbar symptoms, gait abnormalities, cognitive dysfunction) in addition to sleep manifestations (sleep apnea, non-rapid eye movement sleep parasomnia, and RBD.)[33] Serotonergic agents can lead to dream enactment.[34]
Stertenrogic RBD can also present in patients with alpha-synuclein neurodegeneration (such as abnormalities in color vision, anosmia, constipation, and motor impairments).[70] These deficits are not well explained by serotonergic mechanisms, suggesting that serotonergic antidepressants may unmask RBD in individuals at risk of underlying neurodegeneration.
History and Physical
Rapid eye movement behavior disorder exhibits abnormal behaviors during REM sleep that may disrupt sleep and cause injury. Dream enactment is the most distinct abnormal behavior associated with RBD, characterized by purposeful movements during REM sleep with or without vocalization linked to a dream. These sleep-related movements could be violent and lead to self-injuries or injuries to the bed partner. These complex behaviors could result in walking out of bed or falling. Symptoms are usually associated with enacting undesirable or violent dreams where the patient is attacked, chased, or compromised. The patient often wakes up abruptly with prompt alertness and can recount the dream coherently. More than half of the patients are usually aware of their dream-enactment behaviors.[35]
The dream enactment events are variable in frequency (nightly to annually) and usually appear at least 90 minutes after sleep onset and more frequently during the latter half of sleep due to the typical pattern of REM sleep.[36] The eyes are typically closed during an event, and the patient would not normally interact with the environment but rather only behave with the dream. Increased periodic limb movement may occur that may disrupt the sleeping partner.[9] Other sleep behaviors were reported, including stereotypical hand motions, reaching gestures, and punching or kicking.[36]
Acute forms of RBD can be exhibited with intense REM sleep rebound due to withdrawal effects from REM-suppressing drugs. These include alcohol, sedative-hypnotic medications, drug intoxication, or antidepressants.[11] In cases of idiopathic RBD, associated neurological findings could be present such as gait abnormalities or signs of parkinsonism (cogwheel sign, rigidity, or resting tremor).[37]
The cognitive impairments associated with RBD are similar to Parkinson disease and dementia with Lewy bodies.[38] However, the progression of cognitive impairment related to the RBD-PD combination has been reported to be more rapid with less response to treatment than in patients without RBD.[39]
Evaluation
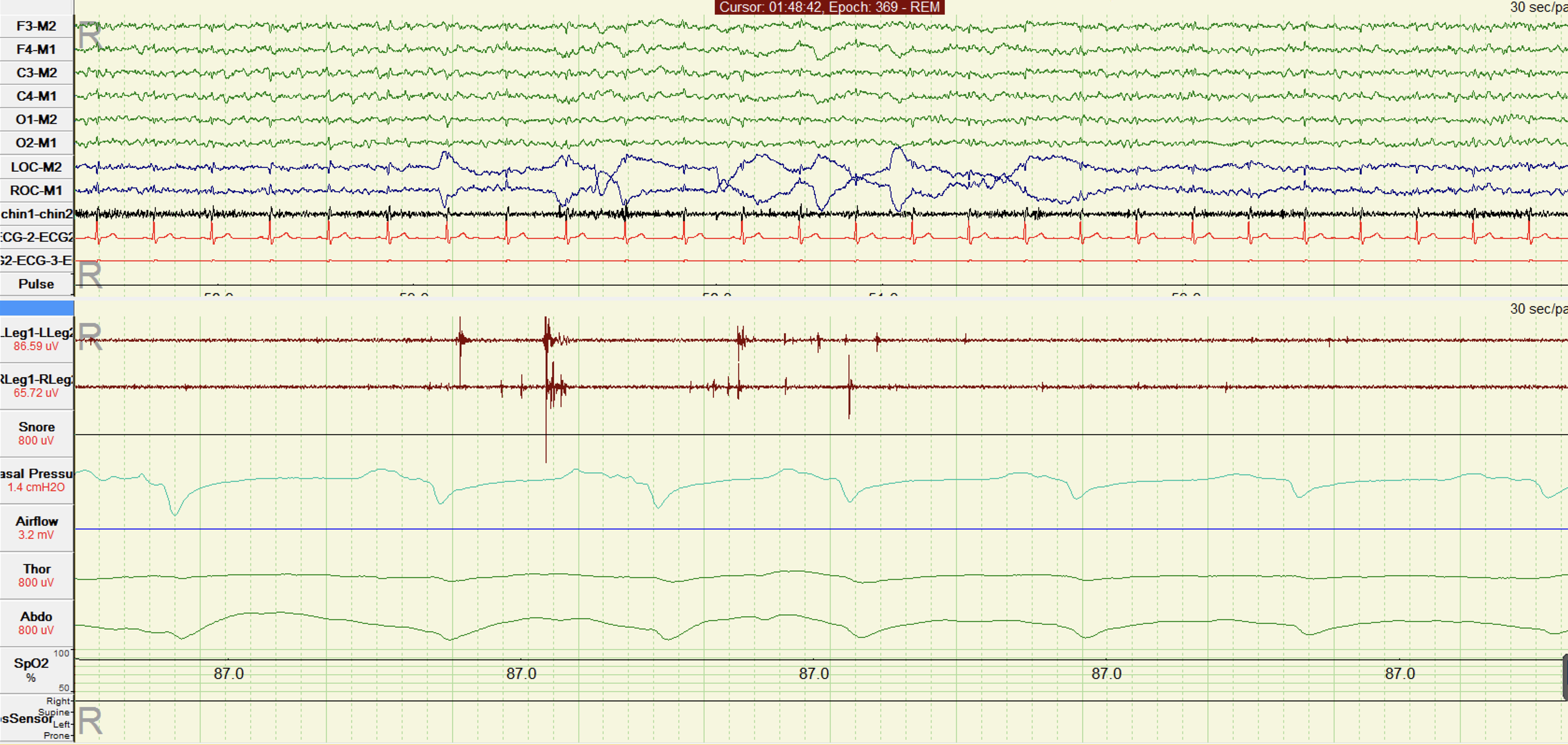
The diagnosis of rapid eye movement behavior disorder comprises two features: loss of normal atonia during REM sleep and dream enactment behavior. The suspicion of RBD is usually due to presentation consistent with dream enactment behavior. The diagnosis requires, however, confirmation with in-lab polysomnography (PSG) with video recording.[40]
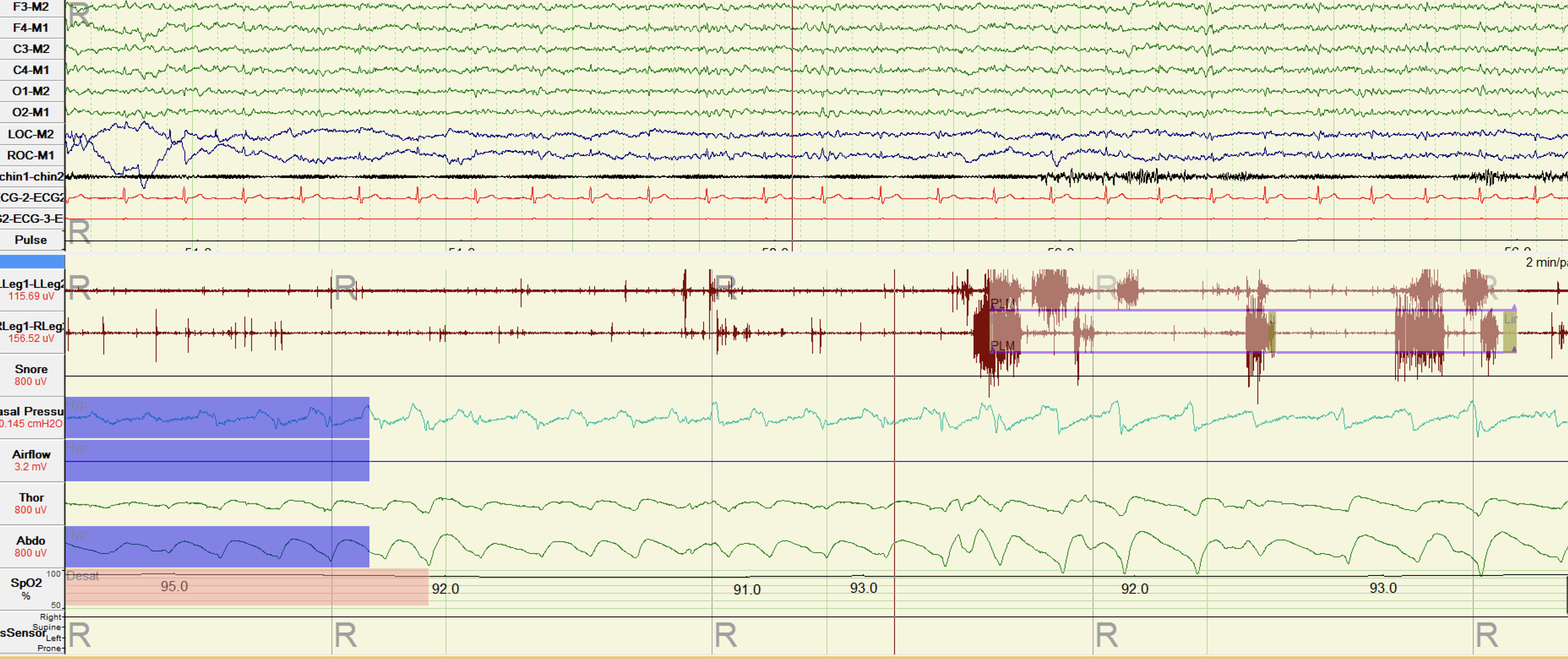
Polysomnography involves simultaneously recording many physiologic variables, including electroencephalography (EEG); therefore, home sleep tests can not be used. PSG is also helpful in excluding other sleep disorders such as sleep-disordered breathing, seizure, and other non-REM sleep disorders or parasomnia. In cases when abnormal behavior does not occur during the sleep study, REM sleep without atonia is required for the diagnosis. REM sleep without atonia (RSWA) is defined as increased tone during REM sleep using electromyography (EMG) of the chin and/or limb leads (either sustained increased chin EMG during sleep or increased phasic chin or limb twitching).[41]
The presence of isolated RSWA is considered an incidental finding in normal individuals, especially in patients receiving antidepressant therapy (SSRI)[5], excessive caffeine or alcohol, or older men.[20] RSWA is often associated with neurodegenerative disorders, which include idiopathic Parkinson disease, Lewy body dementia, and multiple system atrophy.[42]
The scoring of ESWA requires at least 1 of the following features developed by the American Academy of Sleep Medicine (AASM):
- Sustained muscle activity in the chin EMG during the REM sleep stage.[41]
- Excessive transient muscle activity in the chin or limb EMG during REM sleep.[41]
The International Classification of Sleep Disorders, 3 ed., states that diagnostic criteria for RBD must include the following:
- Repeated episodes of sleep-related behaviors include vocalization and/or complex motor behaviors.
- Documenting behaviors by polysomnography during REM sleep or based on clinical history.
- Recordings of polysomnography that demonstrate REM sleep without atonia via submental or limb leads
- Behaviors are not better explained by another sleep disorder, mental disorder, medication, substance use, or epilepsy.
Validated questionnaires have been established to screen patients for RBD. Two single-question questionnaires have been established; the Mayo Sleep Questionnaire and the RBD1Q. The Mayo sleep question was tested in the general population and queried the bed partners (sensitivity 98% and specificity 74%); it asks, “Have you ever seen the patient appear to ‘act out his or her dreams’ (punched or flailed arms in the air, shouted, or screamed) while sleeping?”[43]
The RBD1Q was tested in a sleep center and queried the patient directly (sensitivity 98% and specificity 87%); it asks, “Have you ever been told, or suspected yourself, that you seem to ‘act out your dreams while asleep (for example, punching, flailing your arms in the air, making running movements, etc.)?”[44]
Other questionnaires included the 13-item RBDQ-HK (82% sensitivity and 87% specificity), 14-item RBDSQ (96% sensitivity and 56% specificity), and the 5-item Innsbruck Questionnaire (91% sensitivity, 86% specificity).[45][46][47]
Idiopathic RBD is uncommon. Therefore, the positive predictive value of questionnaires with the highest specificity may be low in the general population, which suggests the continued importance of evaluation with polysomnography. [21]
Treatment / Management
The primary treatment goal of rapid eye movement behavior disorder is to reduce the risk of injury to the patient and bed partners. Changing routine sleep habits may prove challenging for the patient and their bed partners. Their risk for injury, however, needs to be emphasized. Patients and sleeping partners should be educated on the following:
- Mitigating fall risk by lowering the bed closer to the floor
- Safe-guarding any firearms, knives, and other weapons
- Cushioning or padding the floor or sharp furniture surfaces.
- Placing patients in restraining clothes or sleeping bags
- Separating the sleeping partner from the patient to reduce the risk of injury
Based on current guidelines from the American Academy of Sleep Medicine (AASM), the recommended pharmacological treatment of isolated RBD in adults is immediate-release melatonin, clonazepam, or pramipexole (Conditional recommendation).[48] Melatonin is an endogenous hormone secreted from the pineal gland associated with circadian rhythm, and its secretion is influenced by light exposure. Although the mechanism of action is unclear, 3 to 12 mg of melatonin at bedtime is recommended and appears effective in reducing RBD symptoms.[49][50][51] (A1)
Ramelteon is a melatonin M1/M2 receptor agonist that resembles melatonin FDA FDA-approved for insomnia.[52] Ramelteon at a dose of 8mg at bedtime was studied in an open-label study on individuals with idiopathic RBD. Although there was no significant effect on rates of dream enactment or RSWA, subjective improvement was reported, and no side effects were noted.[53]
Clonazepam is an effective treatment for RBD and has been considered for a long time as first-line pharmacological therapy.[54] Clonazepam is a long-acting benzodiazepine with a half-life of 30 to 40 hours and a peak effect within 1 to 4 hours after ingestion. The recommended initial dose is 0.25 mg 30 minutes before bedtime, and a gradually increased dose to as high as 4 mg has been reported. Studies show that the low dose required for treatment offers a low concern for abuse and tolerance. However, common side effects have been observed, including residual morning sleepiness, increased fall risk, memory dysfunction, impotence, and unstable gait. Responders may note an initial period of symptomatic suppression with the re-emergence of more complex behavior. Caution should be considered in those with dementia, fall risk, and obstructive sleep apnea due to worsening associated symptoms. The efficacy was not confirmed in a randomized control trial as both Clonazepam 0.5 mg and placebo improved RBD symptoms.[55](A1)
Clonazepam can significantly reduce periodic limb movement syndrome but not normalize REM sleep atonia.[56][51] Other benzodiazepine agents that have been used in RBD include temazepam, triazolam, alprazolam, and the so-called "z-drugs" (such as zopiclone and zolpidem).[57](B2)
Other therapies for isolated RBD include dopaminergic agents (such as L-DOPA and pramipexole), paroxetine, acetylcholinesterase inhibitors (such as donepezil and rivastigmine), desipramine, clozapine, antiepileptic drugs (e.g., carbamazepine, levetiracetam), and antihypertensive medications (e.g., prazosin, clonidine).[57][58][59][60][61] While these medications may improve nightmares and some motor movements during wakefulness, they are rarely effective in RBD.(A1)
In secondary RBD due to medical conditions in adults, the recommended therapy includes immediate-release melatonin, clonazepam, or transdermal rivastigmine (conditional). While it is not recommended to use deep brain stimulation as a treatment for secondary RBD. [62] In older individuals with RBD (isolated or secondary), immediate-release melatonin remains the preferred choice for safety profile. (A1)
Other non-pharmacologic treatments under investigation include Plasma exchange and deep brain stimulation. In a study on patients with RBD due to Parkinson disease, deep brain stimulation had a different effect on complex behaviors and RSWA events.[63][64] (B2)
Treating comorbid obstructive sleep apnea with continuous positive airway pressure may decrease the frequency and severity of RBD symptoms. Medication reconciliation is necessary to identify medications prone to inducing loss of REM atonia. Management should be discussed with ordering providers and the patient that may require discontinuation, reduction of dose, or earlier medication intake.[56][51](B2)
Differential Diagnosis
Many conditions may mimic the presentation of rapid eye movement behavior disorder symptoms.[65] Take an appropriate history and conduct in-lab video polysomnography to distinguish the definitive diagnosis. For example, isolated REM sleep without atonia (RSWA) noted incidentally during (as increased EMG chin tone or as twitches in the limbs EMG) could occur in the context of OSA (as known pseudo-RBD).
The twitches in limbs EMG could mimic periodic leg movements (PLMS). However, PLMs are periodic and come as series (≥ four limb movements separated by 5 to 90 seconds), usually occur during non-REM sleep, and are not associated with abnormal behaviors (dream enactment). Dream enactment behavior (DEB) does not exclusively present in patients with RBD. Other manifestations that have been associated with DEB include:
- Substance use and/or withdrawal
- Benign childhood epilepsy
- Complex partial seizures
- Confusional arousals
- Delirium
- Epilepsia partialis continua
- Epileptic encephalopathy
- Juvenile myoclonic epilepsy
- Malingering
- Obstructive sleep apnea (OSA)
- Parasomnia overlap syndrome
- Periodic limb movement disorder
- Posttraumatic stress disorder
- Psychogenic nonepileptic seizure
- Sleep terror
- Sleepwalking
- Trauma-associated sleep disorder
Non-REM sleep parasomnias are common and could mimic RBD, including confusional arousals, sleepwalking, and sleep terrors. These disorders typically occur during childhood in the first half of the night during non-REM sleep without dream recall. However, these clinical findings may be observed concomitantly with objective results of REM without atonia and have been characterized as parasomnia overlap syndrome.
In contrast to RBD, sleep terrors occur predominantly in children and present with sudden screening during sleep that can last for several minutes. Sleep talking can be confused with RBD. However, the tone of voice mimics usual conversation and occurs during NREM and REM sleep. Nightmares are vivid dreams that do not have a motor activity. Other associated parasomnias may include sleep-related eating disorders, sexsomnia, or rhythmic movement disorder.[66]
Trauma-associated sleep disorder has recently been characterized as a novel parasomnia. The patient demographics tend to be younger males with traumatic experiences as the temporal onset of disturbing nocturnal behaviors and nightmares. They may or may not have posttraumatic disorders. Objective findings include REM without atonia. Disruptive nocturnal behaviors captured in the lab are rare.[67]
It is important to differentiate RBD behaviors from nocturnal seizures, including juvenile myoclonic epilepsy, grand mal seizure, benign rolandic, Landau-Kleffner syndrome, and sleep-related hyper motor epilepsy (formerly known as nocturnal frontal lobe epilepsy). Patients with epilepsy may exhibit prodromal symptoms such as mood changes and auras, such as irregular blinking or bladder/bowel control loss. Another differentiating behavior between RBD and seizures is the presentation of postictal states that may appear as confusion, headaches, nausea, temporary neurological deficits, sensory deficits, and/or suppressed alertness following the seizure.[68]
Prognosis
The clinical progression of RBD is dependent on the etiology. Idiopathic RBD and RBD associated with neurodegenerative diseases are often slowly progressive. At the same time, medication-induced RBD may occur acutely and improve upon discontinuing the medication. In RBD related to neurodegenerative disorders, the prognosis depends on the underlying condition.
Among those with a confirmed diagnosis of neurodegenerative condition due to an underlying synucleinopathy, it is estimated that the correlation with RBD is significantly high: 30 to 50% of Parkinson disease, 75% of Lewy-body dementia, and 70% to 90% of multiple system atrophy.[69][70][71] The prognosis of RBD with Parkinson disease has a higher risk for dementia, and RBD with Lewy-body dementia has a higher mortality risk.[72][73][74][75]
Once RBD has been confirmed, discussing the associated neurodegenerative risks is appropriate if individual patient circumstances are considered and patients are closely monitored for neurodegenerative disorder findings. In these patients, early introduction to neuroprotective therapies should be discussed, including the importance of regular exercise ( a total of 120 to 150 minutes/week), which may decrease the risk of Parkinson disease as it does in cardiovascular disease.[76][77]
Complications
The primary complications concerning RBD are the risk of injury and the potential prodromal symptoms linking neurodegenerative alpha-synucleinopathies. The injuries sustained during an event may require immediate medical attention and/or involve sleeping partners causing legal implications. Management for RBD primarily involves injury risk mitigation through behavioral changes and/or pharmacological therapy. Early diagnosis and management of RBD provide a therapeutic window to treat the potential underlying neurodegenerative disorder.
Deterrence and Patient Education
Patients with rapid eye movement behavior disorder and their sleeping partners are prone to injuries during their sleep that can result in serious harm. The sleeping partner could target a violent dream enactment behavior leading to the patient being arrested on charges of domestic assault. Therapeutic management should include injury risk mitigation discussions with the patient and their sleeping partner.
It is ethically important to disclose potential risks for the development of neurodegenerative disease to patients diagnosed with RBD. An open discussion with family members allows for improved understanding and avoiding misinformation about the disease process. It is recommended to counsel patients that Parkinson disease and other neurodegenerative disorders can be treatable. The prompt diagnosis of RBD may provide an early therapeutic window for neuroprotective therapies. The International Rapid Eye Movement Sleep Behavior Disorder Study Group is conducting ongoing collaborative studies for symptomatic and neuroprotective treatment.[78]
Pearls and Other Issues
After ten years from diagnosis, there is a high risk with rapid eye movement behavior disorder for developing alpha-synucleinopathy pathology.
There are currently no guidelines on counseling and management regarding the potential conversion of RBD to alpha-synucleinopathy. The approach may include a discussion with the patient to understand this risk. The patient should seek consultation from their primary care provider, sleep specialist, or neurologist if associated symptoms manifest, such as memory issues, constipation, gait abnormalities, orthostatic hypotension, or neurological deficits.
Prodromal alpha-synucleinopathy is possible in younger patients less than 50 years old, but nondegenerative disorders should be considered, including autoimmunity, narcolepsy, and REM-suppressing medication use.
There is a lack of controlled, randomized, double-blind studies for RBD treatment. However, injury prevention is critical in the management of RBD. Clonazepam is highly effective in treating RBD to reduce injury risks.
Low risk for adverse reaction favors melatonin over clonazepam as initial pharmacological therapy for RBD.
Other etiology may resemble RBD symptoms and behaviors, necessitating evaluation with a formal PSG to rule out malingering, psychogenic movement disorder, NREM parasomnias, sleep-related epilepsy syndrome, and obstructive sleep apnea. As physicians may be called upon for legal proceedings, this becomes more paramount when an illegal act is presented to occur during sleep.
Enhancing Healthcare Team Outcomes
Evaluating and managing newly diagnosed rapid eye movement behavior disorder requires a multi-disciplinary and interprofessional effort involving the patient's primary care provider, a sleep specialist, a neurologist, nursing staff, and pharmacists to maximize these patients' well-being. Injury prevention is paramount and may require both pharmacological and non-pharmacological interventions. The looming prognosis of a neurodegenerative disorder associated with RBD will likely provoke anxiety and mood disruption and require management on its own. Including family members is also a key element of support for these patients.
Clinicians from various disciplines will weigh in from their areas of expertise. Pharmacists must be involved because of the number of possible drug options; they can counsel the patient on their medications and perform medication reconciliation, alerting the prescriber of any interactions or other concerns. Nurses often take patient histories and should inform the clinician of any indications of the patient experiencing rapid eye movement sleep behavior disorder. These interventions require open communication among all team members, which will continue throughout the management process once the patient is diagnosed. Given the challenges of this condition, all interprofessional team members must be free to communicate with any other team member with no barriers to ensure optimal patient care.
Unfortunately, there are no established means of predicting the development of neurodegenerative disease or effective management to slow down the disease process. This makes the discussion with patients on the prognostic timeline and the decision of optimal treatment management truly difficult. Close follow-ups and interprofessional communication are critical.
Future research is needed to identify potential biomarkers and neuroprotective strategies to prevent further neurodegeneration in high-risk individuals.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Barone DA, Henchcliffe C. Rapid eye movement sleep behavior disorder and the link to alpha-synucleinopathies. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 2018 Aug:129(8):1551-1564. doi: 10.1016/j.clinph.2018.05.003. Epub 2018 May 29 [PubMed PMID: 29883833]
Boeve BF, Silber MH, Saper CB, Ferman TJ, Dickson DW, Parisi JE, Benarroch EE, Ahlskog JE, Smith GE, Caselli RC, Tippman-Peikert M, Olson EJ, Lin SC, Young T, Wszolek Z, Schenck CH, Mahowald MW, Castillo PR, Del Tredici K, Braak H. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain : a journal of neurology. 2007 Nov:130(Pt 11):2770-88 [PubMed PMID: 17412731]
Level 3 (low-level) evidenceVerma A, Anand V, Verma NP. Sleep disorders in chronic traumatic brain injury. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2007 Jun 15:3(4):357-62 [PubMed PMID: 17694723]
Level 2 (mid-level) evidenceElliott JE, Opel RA, Pleshakov D, Rachakonda T, Chau AQ, Weymann KB, Lim MM. Posttraumatic stress disorder increases the odds of REM sleep behavior disorder and other parasomnias in Veterans with and without comorbid traumatic brain injury. Sleep. 2020 Mar 12:43(3):. doi: 10.1093/sleep/zsz237. Epub [PubMed PMID: 31587047]
McCarter SJ, St Louis EK, Sandness DJ, Arndt K, Erickson M, Tabatabai G, Boeve BF, Silber MH. Antidepressants Increase REM Sleep Muscle Tone in Patients with and without REM Sleep Behavior Disorder. Sleep. 2015 Jun 1:38(6):907-17. doi: 10.5665/sleep.4738. Epub 2015 Jun 1 [PubMed PMID: 25325487]
Gagnon JF, Postuma RB, Montplaisir J. Update on the pharmacology of REM sleep behavior disorder. Neurology. 2006 Sep 12:67(5):742-7 [PubMed PMID: 16966533]
Ma C, Pavlova M, Li J, Liu Y, Sun Y, Huang Z, Wu S, Gao X. Alcohol consumption and probable rapid eye movement sleep behavior disorder. Annals of clinical and translational neurology. 2018 Oct:5(10):1176-1183. doi: 10.1002/acn3.630. Epub 2018 Aug 18 [PubMed PMID: 30349852]
Knudsen S, Gammeltoft S, Jennum PJ. Rapid eye movement sleep behaviour disorder in patients with narcolepsy is associated with hypocretin-1 deficiency. Brain : a journal of neurology. 2010 Feb:133(Pt 2):568-79. doi: 10.1093/brain/awp320. Epub 2010 Feb 3 [PubMed PMID: 20129934]
Frauscher B, Gschliesser V, Brandauer E, Marti I, Furtner MT, Ulmer H, Poewe W, Högl B. REM sleep behavior disorder in 703 sleep-disorder patients: the importance of eliciting a comprehensive sleep history. Sleep medicine. 2010 Feb:11(2):167-71. doi: 10.1016/j.sleep.2009.03.011. Epub [PubMed PMID: 20022299]
Ohayon MM, Schenck CH. Violent behavior during sleep: prevalence, comorbidity and consequences. Sleep medicine. 2010 Oct:11(9):941-6. doi: 10.1016/j.sleep.2010.02.016. Epub [PubMed PMID: 20817553]
Haba-Rubio J, Frauscher B, Marques-Vidal P, Toriel J, Tobback N, Andries D, Preisig M, Vollenweider P, Postuma R, Heinzer R. Prevalence and determinants of rapid eye movement sleep behavior disorder in the general population. Sleep. 2018 Feb 1:41(2):. pii: zsx197. doi: 10.1093/sleep/zsx197. Epub [PubMed PMID: 29216391]
Kang SH, Yoon IY, Lee SD, Han JW, Kim TH, Kim KW. REM sleep behavior disorder in the Korean elderly population: prevalence and clinical characteristics. Sleep. 2013 Aug 1:36(8):1147-52. doi: 10.5665/sleep.2874. Epub 2013 Aug 1 [PubMed PMID: 23904674]
Pujol M, Pujol J, Alonso T, Fuentes A, Pallerola M, Freixenet J, Barbé F, Salamero M, Santamaría J, Iranzo A. Idiopathic REM sleep behavior disorder in the elderly Spanish community: a primary care center study with a two-stage design using video-polysomnography. Sleep medicine. 2017 Dec:40():116-121. doi: 10.1016/j.sleep.2017.07.021. Epub 2017 Aug 24 [PubMed PMID: 29042180]
Bodkin CL, Schenck CH. Rapid eye movement sleep behavior disorder in women: relevance to general and specialty medical practice. Journal of women's health (2002). 2009 Dec:18(12):1955-63. doi: 10.1089/jwh.2008.1348. Epub [PubMed PMID: 20044857]
Ju YE. Rapid eye movement sleep behavior disorder in adults younger than 50 years of age. Sleep medicine. 2013 Aug:14(8):768-74. doi: 10.1016/j.sleep.2012.09.026. Epub 2013 Jan 21 [PubMed PMID: 23347910]
Teman PT, Tippmann-Peikert M, Silber MH, Slocumb NL, Auger RR. Idiopathic rapid-eye-movement sleep disorder: associations with antidepressants, psychiatric diagnoses, and other factors, in relation to age of onset. Sleep medicine. 2009 Jan:10(1):60-5. doi: 10.1016/j.sleep.2007.11.019. Epub 2008 Jan 28 [PubMed PMID: 18226952]
Level 2 (mid-level) evidenceLloyd R, Tippmann-Peikert M, Slocumb N, Kotagal S. Characteristics of REM sleep behavior disorder in childhood. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2012 Apr 15:8(2):127-31. doi: 10.5664/jcsm.1760. Epub 2012 Apr 15 [PubMed PMID: 22505856]
Level 2 (mid-level) evidenceNevsimalova S, Pisko J, Buskova J, Kemlink D, Prihodova I, Sonka K, Skibova J. Narcolepsy: clinical differences and association with other sleep disorders in different age groups. Journal of neurology. 2013 Mar:260(3):767-75. doi: 10.1007/s00415-012-6702-4. Epub 2012 Oct 16 [PubMed PMID: 23070467]
Level 2 (mid-level) evidenceLee K, Baron K, Soca R, Attarian H. The Prevalence and Characteristics of REM Sleep without Atonia (RSWA) in Patients Taking Antidepressants. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2016 Mar:12(3):351-5. doi: 10.5664/jcsm.5582. Epub [PubMed PMID: 26446247]
Feemster JC, Jung Y, Timm PC, Westerland SM, Gossard TR, Teigen LN, Buchal LA, Cattaneo EFD, Imlach CA, Mccarter SJ, Smith KL, Boeve BF, Silber MH, St Louis EK. Normative and isolated rapid eye movement sleep without atonia in adults without REM sleep behavior disorder. Sleep. 2019 Oct 9:42(10):. doi: 10.1093/sleep/zsz124. Epub [PubMed PMID: 31587043]
Postuma RB, Iranzo A, Hu M, Högl B, Boeve BF, Manni R, Oertel WH, Arnulf I, Ferini-Strambi L, Puligheddu M, Antelmi E, Cochen De Cock V, Arnaldi D, Mollenhauer B, Videnovic A, Sonka K, Jung KY, Kunz D, Dauvilliers Y, Provini F, Lewis SJ, Buskova J, Pavlova M, Heidbreder A, Montplaisir JY, Santamaria J, Barber TR, Stefani A, St Louis EK, Terzaghi M, Janzen A, Leu-Semenescu S, Plazzi G, Nobili F, Sixel-Doering F, Dusek P, Bes F, Cortelli P, Ehgoetz Martens K, Gagnon JF, Gaig C, Zucconi M, Trenkwalder C, Gan-Or Z, Lo C, Rolinski M, Mahlknecht P, Holzknecht E, Boeve AR, Teigen LN, Toscano G, Mayer G, Morbelli S, Dawson B, Pelletier A. Risk and predictors of dementia and parkinsonism in idiopathic REM sleep behaviour disorder: a multicentre study. Brain : a journal of neurology. 2019 Mar 1:142(3):744-759. doi: 10.1093/brain/awz030. Epub [PubMed PMID: 30789229]
Du L, Xu L, Liang T, Wing YK, Ke Y, Yung WH. Progressive Pontine-Medullary Dysfunction Leads to REM Sleep Behavior Disorder Symptoms in a Chronic Model of Parkinson's Disease. Nature and science of sleep. 2021:13():1723-1736. doi: 10.2147/NSS.S328365. Epub 2021 Oct 5 [PubMed PMID: 34675721]
Boeve BF, Silber MH, Ferman TJ, Lin SC, Benarroch EE, Schmeichel AM, Ahlskog JE, Caselli RJ, Jacobson S, Sabbagh M, Adler C, Woodruff B, Beach TG, Iranzo A, Gelpi E, Santamaria J, Tolosa E, Singer C, Mash DC, Luca C, Arnulf I, Duyckaerts C, Schenck CH, Mahowald MW, Dauvilliers Y, Graff-Radford NR, Wszolek ZK, Parisi JE, Dugger B, Murray ME, Dickson DW. Clinicopathologic correlations in 172 cases of rapid eye movement sleep behavior disorder with or without a coexisting neurologic disorder. Sleep medicine. 2013 Aug:14(8):754-62. doi: 10.1016/j.sleep.2012.10.015. Epub 2013 Mar 7 [PubMed PMID: 23474058]
Level 3 (low-level) evidenceNomura T, Inoue Y, Takigawa H, Nakashima K. Comparison of REM sleep behaviour disorder variables between patients with progressive supranuclear palsy and those with Parkinson's disease. Parkinsonism & related disorders. 2012 May:18(4):394-6. doi: 10.1016/j.parkreldis.2011.10.018. Epub 2011 Nov 23 [PubMed PMID: 22115673]
Ebben MR, Shahbazi M, Lange DJ, Krieger AC. REM behavior disorder associated with familial amyotrophic lateral sclerosis. Amyotrophic lateral sclerosis : official publication of the World Federation of Neurology Research Group on Motor Neuron Diseases. 2012 Sep:13(5):473-4. doi: 10.3109/17482968.2012.673172. Epub 2012 Jun 7 [PubMed PMID: 22670878]
Level 3 (low-level) evidenceLo Coco D, Cupidi C, Mattaliano A, Baiamonte V, Realmuto S, Cannizzaro E. REM sleep behavior disorder in a patient with frontotemporal dementia. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2012 Apr:33(2):371-3. doi: 10.1007/s10072-011-0702-5. Epub 2011 Jul 13 [PubMed PMID: 21751100]
Level 3 (low-level) evidenceChokroverty S, Bhat S, Rosen D, Farheen A. REM behavior disorder in myotonic dystrophy type 2. Neurology. 2012 Jun 12:78(24):2004. doi: 10.1212/WNL.0b013e318259e28c. Epub [PubMed PMID: 22689737]
Level 3 (low-level) evidenceTribl GG, Trindade MC, Bittencourt T, Lorenzi-Filho G, Cardoso Alves R, Ciampi de Andrade D, Fonoff ET, Bor-Seng-Shu E, Machado AA, Schenck CH, Teixeira MJ, Barbosa ER. Wilson's disease with and without rapid eye movement sleep behavior disorder compared to healthy matched controls. Sleep medicine. 2016 Jan:17():179-85. doi: 10.1016/j.sleep.2015.09.003. Epub 2015 Sep 11 [PubMed PMID: 26763676]
Iranzo A, Graus F, Clover L, Morera J, Bruna J, Vilar C, Martínez-Rodriguez JE, Vincent A, Santamaría J. Rapid eye movement sleep behavior disorder and potassium channel antibody-associated limbic encephalitis. Annals of neurology. 2006 Jan:59(1):178-81 [PubMed PMID: 16278841]
Vale TC, Fernandes do Prado LB, do Prado GF, Povoas Barsottini OG, Pedroso JL. Rapid Eye Movement Sleep Behavior Disorder in Paraneoplastic Cerebellar Degeneration: Improvement with Immunotherapy. Sleep. 2016 Jan 1:39(1):117-20. doi: 10.5665/sleep.5330. Epub 2016 Jan 1 [PubMed PMID: 26414894]
Sabater L, Gaig C, Gelpi E, Bataller L, Lewerenz J, Torres-Vega E, Contreras A, Giometto B, Compta Y, Embid C, Vilaseca I, Iranzo A, Santamaría J, Dalmau J, Graus F. A novel non-rapid-eye movement and rapid-eye-movement parasomnia with sleep breathing disorder associated with antibodies to IgLON5: a case series, characterisation of the antigen, and post-mortem study. The Lancet. Neurology. 2014 Jun:13(6):575-86. doi: 10.1016/S1474-4422(14)70051-1. Epub 2014 Apr 3 [PubMed PMID: 24703753]
Level 2 (mid-level) evidenceAntelmi E, Pizza F, Donadio V, Filardi M, Sosero YL, Incensi A, Vandi S, Moresco M, Ferri R, Marelli S, Ferini-Strambi L, Liguori R, Plazzi G. Biomarkers for REM sleep behavior disorder in idiopathic and narcoleptic patients. Annals of clinical and translational neurology. 2019 Sep:6(9):1872-1876. doi: 10.1002/acn3.50833. Epub 2019 Aug 6 [PubMed PMID: 31386270]
Heidbreder A, Philipp K. Anti-IgLON 5 Disease. Current treatment options in neurology. 2018 Jun 23:20(8):29. doi: 10.1007/s11940-018-0515-4. Epub 2018 Jun 23 [PubMed PMID: 29936617]
Baltzan M, Yao C, Rizzo D, Postuma R. Dream enactment behavior: review for the clinician. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2020 Nov 15:16(11):1949-1969. doi: 10.5664/jcsm.8734. Epub [PubMed PMID: 32741444]
Fernández-Arcos A, Iranzo A, Serradell M, Gaig C, Santamaria J. The Clinical Phenotype of Idiopathic Rapid Eye Movement Sleep Behavior Disorder at Presentation: A Study in 203 Consecutive Patients. Sleep. 2016 Jan 1:39(1):121-32. doi: 10.5665/sleep.5332. Epub 2016 Jan 1 [PubMed PMID: 26940460]
Schenck CH, Bundlie SR, Ettinger MG, Mahowald MW. Chronic behavioral disorders of human REM sleep: a new category of parasomnia. Sleep. 1986 Jun:9(2):293-308 [PubMed PMID: 3505730]
Level 3 (low-level) evidenceVidenovic A, Marlin C, Alibiglou L, Planetta PJ, Vaillancourt DE, Mackinnon CD. Increased REM sleep without atonia in Parkinson disease with freezing of gait. Neurology. 2013 Sep 17:81(12):1030-5. doi: 10.1212/WNL.0b013e3182a4a408. Epub 2013 Aug 14 [PubMed PMID: 23946301]
Level 2 (mid-level) evidenceFereshtehnejad SM, Yao C, Pelletier A, Montplaisir JY, Gagnon JF, Postuma RB. Evolution of prodromal Parkinson's disease and dementia with Lewy bodies: a prospective study. Brain : a journal of neurology. 2019 Jul 1:142(7):2051-2067. doi: 10.1093/brain/awz111. Epub [PubMed PMID: 31111143]
Postuma RB, Gagnon JF, Vendette M, Charland K, Montplaisir J. Manifestations of Parkinson disease differ in association with REM sleep behavior disorder. Movement disorders : official journal of the Movement Disorder Society. 2008 Sep 15:23(12):1665-72. doi: 10.1002/mds.22099. Epub [PubMed PMID: 18709686]
Neikrug AB, Ancoli-Israel S. Diagnostic tools for REM sleep behavior disorder. Sleep medicine reviews. 2012 Oct:16(5):415-29. doi: 10.1016/j.smrv.2011.08.004. Epub 2011 Dec 14 [PubMed PMID: 22169258]
Berry RB, Brooks R, Gamaldo C, Harding SM, Lloyd RM, Quan SF, Troester MT, Vaughn BV. AASM Scoring Manual Updates for 2017 (Version 2.4). Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2017 May 15:13(5):665-666. doi: 10.5664/jcsm.6576. Epub 2017 May 15 [PubMed PMID: 28416048]
McCarter SJ, St Louis EK, Boeve BF. REM sleep behavior disorder and REM sleep without atonia as an early manifestation of degenerative neurological disease. Current neurology and neuroscience reports. 2012 Apr:12(2):182-92. doi: 10.1007/s11910-012-0253-z. Epub [PubMed PMID: 22328094]
Level 3 (low-level) evidenceBoeve BF, Molano JR, Ferman TJ, Lin SC, Bieniek K, Tippmann-Peikert M, Boot B, St Louis EK, Knopman DS, Petersen RC, Silber MH. Validation of the Mayo Sleep Questionnaire to screen for REM sleep behavior disorder in a community-based sample. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2013 May 15:9(5):475-80. doi: 10.5664/jcsm.2670. Epub 2013 May 15 [PubMed PMID: 23674939]
Level 1 (high-level) evidencePostuma RB, Arnulf I, Hogl B, Iranzo A, Miyamoto T, Dauvilliers Y, Oertel W, Ju YE, Puligheddu M, Jennum P, Pelletier A, Wolfson C, Leu-Semenescu S, Frauscher B, Miyamoto M, Cochen De Cock V, Unger MM, Stiasny-Kolster K, Fantini ML, Montplaisir JY. A single-question screen for rapid eye movement sleep behavior disorder: a multicenter validation study. Movement disorders : official journal of the Movement Disorder Society. 2012 Jun:27(7):913-6. doi: 10.1002/mds.25037. Epub 2012 May 30 [PubMed PMID: 22729987]
Level 2 (mid-level) evidenceStiasny-Kolster K, Mayer G, Schäfer S, Möller JC, Heinzel-Gutenbrunner M, Oertel WH. The REM sleep behavior disorder screening questionnaire--a new diagnostic instrument. Movement disorders : official journal of the Movement Disorder Society. 2007 Dec:22(16):2386-93 [PubMed PMID: 17894337]
Li SX, Wing YK, Lam SP, Zhang J, Yu MW, Ho CK, Tsoh J, Mok V. Validation of a new REM sleep behavior disorder questionnaire (RBDQ-HK). Sleep medicine. 2010 Jan:11(1):43-8. doi: 10.1016/j.sleep.2009.06.008. Epub 2009 Nov 30 [PubMed PMID: 19945912]
Level 1 (high-level) evidenceFrauscher B, Ehrmann L, Zamarian L, Auer F, Mitterling T, Gabelia D, Brandauer E, Delazer M, Poewe W, Högl B. Validation of the Innsbruck REM sleep behavior disorder inventory. Movement disorders : official journal of the Movement Disorder Society. 2012 Nov:27(13):1673-8. doi: 10.1002/mds.25223. Epub [PubMed PMID: 23192924]
Level 2 (mid-level) evidenceHowell M, Avidan AY, Foldvary-Schaefer N, Malkani RG, During EH, Roland JP, McCarter SJ, Zak RS, Carandang G, Kazmi U, Ramar K. Management of REM sleep behavior disorder: an American Academy of Sleep Medicine clinical practice guideline. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2023 Apr 1:19(4):759-768. doi: 10.5664/jcsm.10424. Epub [PubMed PMID: 36515157]
Level 1 (high-level) evidenceMcGrane IR, Leung JG, St Louis EK, Boeve BF. Melatonin therapy for REM sleep behavior disorder: a critical review of evidence. Sleep medicine. 2015 Jan:16(1):19-26. doi: 10.1016/j.sleep.2014.09.011. Epub 2014 Oct 13 [PubMed PMID: 25454845]
Kunz D, Mahlberg R. A two-part, double-blind, placebo-controlled trial of exogenous melatonin in REM sleep behaviour disorder. Journal of sleep research. 2010 Dec:19(4):591-6. doi: 10.1111/j.1365-2869.2010.00848.x. Epub [PubMed PMID: 20561180]
Level 1 (high-level) evidenceMcCarter SJ, Boswell CL, St Louis EK, Dueffert LG, Slocumb N, Boeve BF, Silber MH, Olson EJ, Tippmann-Peikert M. Treatment outcomes in REM sleep behavior disorder. Sleep medicine. 2013 Mar:14(3):237-42. doi: 10.1016/j.sleep.2012.09.018. Epub 2013 Jan 23 [PubMed PMID: 23352028]
Level 2 (mid-level) evidenceSavage RA, Zafar N, Yohannan S, Miller JMM. Melatonin. StatPearls. 2023 Jan:(): [PubMed PMID: 30521244]
Esaki Y, Kitajima T, Koike S, Fujishiro H, Iwata Y, Tsuchiya A, Hirose M, Iwata N. An Open-Labeled Trial of Ramelteon in Idiopathic Rapid Eye Movement Sleep Behavior Disorder. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2016 May 15:12(5):689-93. doi: 10.5664/jcsm.5796. Epub 2016 May 15 [PubMed PMID: 26857053]
Aurora RN, Zak RS, Maganti RK, Auerbach SH, Casey KR, Chowdhuri S, Karippot A, Ramar K, Kristo DA, Morgenthaler TI, Standards of Practice Committee, American Academy of Sleep Medicine. Best practice guide for the treatment of REM sleep behavior disorder (RBD). Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2010 Feb 15:6(1):85-95 [PubMed PMID: 20191945]
Level 3 (low-level) evidenceShin C, Park H, Lee WW, Kim HJ, Kim HJ, Jeon B. Clonazepam for probable REM sleep behavior disorder in Parkinson's disease: A randomized placebo-controlled trial. Journal of the neurological sciences. 2019 Jun 15:401():81-86. doi: 10.1016/j.jns.2019.04.029. Epub 2019 Apr 23 [PubMed PMID: 31035190]
Level 1 (high-level) evidenceFerri R, Zucconi M, Marelli S, Plazzi G, Schenck CH, Ferini-Strambi L. Effects of long-term use of clonazepam on nonrapid eye movement sleep patterns in rapid eye movement sleep behavior disorder. Sleep medicine. 2013 May:14(5):399-406. doi: 10.1016/j.sleep.2013.01.007. Epub 2013 Mar 9 [PubMed PMID: 23490738]
Level 2 (mid-level) evidenceJung Y, St Louis EK. Treatment of REM Sleep Behavior Disorder. Current treatment options in neurology. 2016 Nov:18(11):50 [PubMed PMID: 27752878]
Schmidt MH, Koshal VB, Schmidt HS. Use of pramipexole in REM sleep behavior disorder: results from a case series. Sleep medicine. 2006 Aug:7(5):418-23 [PubMed PMID: 16815751]
Level 2 (mid-level) evidenceKumru H, Iranzo A, Carrasco E, Valldeoriola F, Marti MJ, Santamaria J, Tolosa E. Lack of effects of pramipexole on REM sleep behavior disorder in Parkinson disease. Sleep. 2008 Oct:31(10):1418-21 [PubMed PMID: 18853939]
Moraes Wdos S, Poyares DR, Guilleminault C, Ramos LR, Bertolucci PH, Tufik S. The effect of donepezil on sleep and REM sleep EEG in patients with Alzheimer disease: a double-blind placebo-controlled study. Sleep. 2006 Feb:29(2):199-205 [PubMed PMID: 16494088]
Level 1 (high-level) evidenceBrunetti V, Losurdo A, Testani E, Lapenta L, Mariotti P, Marra C, Rossini PM, Della Marca G. Rivastigmine for refractory REM behavior disorder in mild cognitive impairment. Current Alzheimer research. 2014 Mar:11(3):267-73 [PubMed PMID: 24597506]
Howell M, Avidan AY, Foldvary-Schaefer N, Malkani RG, During EH, Roland JP, McCarter SJ, Zak RS, Carandang G, Kazmi U, Ramar K. Management of REM sleep behavior disorder: an American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2023 Apr 1:19(4):769-810. doi: 10.5664/jcsm.10426. Epub [PubMed PMID: 36515150]
Level 1 (high-level) evidenceMontagna M, Amir R, De Volder I, Lammens M, Huyskens J, Willekens B. IgLON5-Associated Encephalitis With Atypical Brain Magnetic Resonance Imaging and Cerebrospinal Fluid Changes. Frontiers in neurology. 2018:9():329. doi: 10.3389/fneur.2018.00329. Epub 2018 May 17 [PubMed PMID: 29867738]
Cavalloni F, Debove I, Lachenmayer ML, Krack P, Pollo C, Schuepbach WMM, Bassetti CLA, Bargiotas P. A case series and systematic review of rapid eye movement sleep behavior disorder outcome after deep brain stimulation in Parkinson's disease. Sleep medicine. 2021 Jan:77():170-176. doi: 10.1016/j.sleep.2020.11.025. Epub 2020 Nov 29 [PubMed PMID: 33412362]
Level 2 (mid-level) evidenceAntelmi E, Lippolis M, Biscarini F, Tinazzi M, Plazzi G. REM sleep behavior disorder: Mimics and variants. Sleep medicine reviews. 2021 Dec:60():101515. doi: 10.1016/j.smrv.2021.101515. Epub 2021 Jun 10 [PubMed PMID: 34186416]
Soca R, Keenan JC, Schenck CH. Parasomnia Overlap Disorder with Sexual Behaviors during Sleep in a Patient with Obstructive Sleep Apnea. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2016 Aug 15:12(8):1189-91. doi: 10.5664/jcsm.6066. Epub 2016 Aug 15 [PubMed PMID: 27166304]
Mysliwiec V, Brock MS, Creamer JL, O'Reilly BM, Germain A, Roth BJ. Trauma associated sleep disorder: A parasomnia induced by trauma. Sleep medicine reviews. 2018 Feb:37():94-104. doi: 10.1016/j.smrv.2017.01.004. Epub 2017 Jan 30 [PubMed PMID: 28363448]
Al-Biltagi MA. Childhood epilepsy and sleep. World journal of clinical pediatrics. 2014 Aug 8:3(3):45-53. doi: 10.5409/wjcp.v3.i3.45. Epub 2014 Aug 8 [PubMed PMID: 25254184]
Boot BP, Boeve BF, Roberts RO, Ferman TJ, Geda YE, Pankratz VS, Ivnik RJ, Smith GE, McDade E, Christianson TJ, Knopman DS, Tangalos EG, Silber MH, Petersen RC. Probable rapid eye movement sleep behavior disorder increases risk for mild cognitive impairment and Parkinson disease: a population-based study. Annals of neurology. 2012 Jan:71(1):49-56. doi: 10.1002/ana.22655. Epub [PubMed PMID: 22275251]
Level 2 (mid-level) evidenceMahlknecht P, Seppi K, Frauscher B, Kiechl S, Willeit J, Stockner H, Djamshidian A, Nocker M, Rastner V, Defrancesco M, Rungger G, Gasperi A, Poewe W, Högl B. Probable RBD and association with neurodegenerative disease markers: A population-based study. Movement disorders : official journal of the Movement Disorder Society. 2015 Sep:30(10):1417-21. doi: 10.1002/mds.26350. Epub 2015 Jul 24 [PubMed PMID: 26208108]
Galbiati A, Verga L, Giora E, Zucconi M, Ferini-Strambi L. The risk of neurodegeneration in REM sleep behavior disorder: A systematic review and meta-analysis of longitudinal studies. Sleep medicine reviews. 2019 Feb:43():37-46. doi: 10.1016/j.smrv.2018.09.008. Epub 2018 Nov 8 [PubMed PMID: 30503716]
Level 1 (high-level) evidencePostuma RB, Gagnon JF, Bertrand JA, Génier Marchand D, Montplaisir JY. Parkinson risk in idiopathic REM sleep behavior disorder: preparing for neuroprotective trials. Neurology. 2015 Mar 17:84(11):1104-13. doi: 10.1212/WNL.0000000000001364. Epub 2015 Feb 13 [PubMed PMID: 25681454]
Level 2 (mid-level) evidenceKim Y, Kim YE, Park EO, Shin CW, Kim HJ, Jeon B. REM sleep behavior disorder portends poor prognosis in Parkinson's disease: A systematic review. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2018 Jan:47():6-13. doi: 10.1016/j.jocn.2017.09.019. Epub 2017 Nov 6 [PubMed PMID: 29102236]
Level 1 (high-level) evidenceZahirovic I, Torisson G, Wattmo C, Londos E. Survival among the older adults with clinical signs of Lewy body dementia in 40 Swedish nursing homes: a 6-year follow-up study. BMJ open. 2019 May 30:9(5):e028010. doi: 10.1136/bmjopen-2018-028010. Epub 2019 May 30 [PubMed PMID: 31152036]
Zhou J, Zhang J, Lam SP, Mok V, Chan A, Li SX, Liu Y, Tang X, Yung WH, Wing YK. Mortality and Its Risk Factors in Patients with Rapid Eye Movement Sleep Behavior Disorder. Sleep. 2016 Aug 1:39(8):1543-50. doi: 10.5665/sleep.6016. Epub 2016 Aug 1 [PubMed PMID: 27306273]
McCarter SJ, Boeve BF, Graff-Radford NR, Silber MH, St Louis EK. Neuroprotection in idiopathic REM sleep behavior disorder: a role for exercise? Sleep. 2019 Jun 11:42(6):. pii: zsz064. doi: 10.1093/sleep/zsz064. Epub [PubMed PMID: 31184756]
Schaeffer E, Rogge A, Nieding K, Helmker V, Letsch C, Hauptmann B, Berg D. Patients' views on the ethical challenges of early Parkinson disease detection. Neurology. 2020 May 12:94(19):e2037-e2044. doi: 10.1212/WNL.0000000000009400. Epub 2020 Apr 14 [PubMed PMID: 32291296]
Schenck CH, Montplaisir JY, Frauscher B, Hogl B, Gagnon JF, Postuma R, Sonka K, Jennum P, Partinen M, Arnulf I, Cochen de Cock V, Dauvilliers Y, Luppi PH, Heidbreder A, Mayer G, Sixel-Döring F, Trenkwalder C, Unger M, Young P, Wing YK, Ferini-Strambi L, Ferri R, Plazzi G, Zucconi M, Inoue Y, Iranzo A, Santamaria J, Bassetti C, Möller JC, Boeve BF, Lai YY, Pavlova M, Saper C, Schmidt P, Siegel JM, Singer C, St Louis E, Videnovic A, Oertel W. Rapid eye movement sleep behavior disorder: devising controlled active treatment studies for symptomatic and neuroprotective therapy--a consensus statement from the International Rapid Eye Movement Sleep Behavior Disorder Study Group. Sleep medicine. 2013 Aug:14(8):795-806. doi: 10.1016/j.sleep.2013.02.016. Epub 2013 Jul 22 [PubMed PMID: 23886593]
Level 3 (low-level) evidence