Introduction
Cor triatriatum is a rare congenital heart condition where a child is born with a thin, fibromuscular, often fenestrated membrane subdividing the left or right atrium into 3 chambers (see Image. Cor Triatriatum Sinistrum). This condition was classified by Praagh et al into 3 types:
- Cor triatriatum sinister: The left cor triatriatum is the most common form, albeit very rare. The left atrium is divided by a fibromuscular band into an upper (pulmonary venous) and a lower (vestibular) compartment. The upper compartment receives blood from the pulmonary veins, and the atrial appendage is typically part of the lower compartment. This arrangement of cor triatriatum sinister is crucial in the differential diagnosis, particularly from conditions such as supravalvular mitral valve stenosis. According to the degree of blood flow impedance, the fibromuscular membrane can create significant left ventricular inflow obstruction and substantial pulmonary hypertension.[1]
- Cor triatriatum dextrum: The right valve of the sinus venosus persists, dividing the right atrium into 2 chambers. Cor triatriatum dextrum presents similarly to the Ebstein anomaly and is challenging to differentiate from it based on clinical features only.[2]
- Cor triatriatum intermedium: A largely theoretical entity that may occur due to a persistent interseptovalvular space. Thilenius et al first described this anomaly in 1976 as type C. Nevertheless, no real-life cases of a third intermediary atrial chamber have been reported in the surgical literature.[3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Cor triatriatum sinistrum results from the incomplete absorption of the common pulmonary vein, which is typically reabsorbed during fetal development and fuses with the left atrium. This phenomenon could explain why there often are concurrent anomalies of the atrial septum (atrioseptal defects) and the pulmonary venous connection. The incomplete absorption results in the formation of a diagonal membrane that subdivides the left atrium into 2 chambers—pulmonary venous and vestibular chambers. No known genetic mutations or risk factors are found to be associated with the development of this condition. Cor triatriatum dextrum develops from the persistence of a right sinus venosus valve.[4]
Epidemiology
Cor triatriatum sinister has an estimated incidence of 0.4%, resulting from abnormal left atrial septation.[5] Cor triatriatum sinisterum is associated with other congenital cardiac defects, such as tetralogy of Fallot, atrial septal defect, ventricular septal defect, and partial anomalous pulmonary venous connection, and represents only 0.1% to 0.4% of all congenital abnormalities.[6][7] The membrane may be complete or contain 1 or more fenestrations of differing sizes.
Cor triatriatum dextrum has an incidence of 0.025% among all congenital heart diseases. This anomaly often coexists with right-sided cardiac defects. The most common related heart defects include pulmonary valve stenosis or atresia, abnormalities of the tricuspid valve, and an atrial septal defect.[8]
Pathophysiology
A malincorporation theory presented by Parsons explains how cor triatriatum sinister occurs.[9] During normal fetal development, the pulmonary vein incorporates into the left atrium. When this process fails, the common pulmonary venous ostium remains narrow, resulting in a septum-like structure called the atrial appendage. The appendage then further divides the left atrium into 2 compartments. Although widely accepted, this theory fails to explain the presence of fossa ovalis and atrial muscle fibers in the proximal atrial chamber.[10]
Two other theories, malseptation and entrapment, also explain the pathophysiology of cor triatriatum. The malseptation theory suggests that the fibromuscular membrane is an abnormal growth of the septum primum. In contrast, the entrapment theory emphasizes the entrapment of the common pulmonary vein in the embryonic sinus venosus, thereby preventing its incorporation into the left atrium. The malincorporation theory remains the most widely accepted etiologic theory.
History and Physical
Classically, cor triatriatum presents in infancy with signs and symptoms of pulmonary hypertension and pulmonary venous obstruction. Due to low cardiac output, children can show poor growth and weight gain, feeding difficulties, respiratory distress, and tet spells. In childhood and adulthood, the signs and symptoms of pulmonary venous hypertension and right heart failure dominate as the membrane calcifies and the opening becomes smaller and smaller, decreasing cardiac output even further. Mitral valve regurgitation and atrial fibrillation impose serious dangers. Most patients present with the following features:
- Exertional dyspnea, dyspnea at rest, and orthopnea
- Easy fatigability
- Hemoptysis
- Palpitations [11]
Atrial fibrillation can cause systemic thromboembolism and present as pulmonary embolism or stroke. The left atrial enlarges due to the backing up of blood and can present as life-threatening arrhythmias.
Cor triatriatum sinister initially presenting in adulthood is rare but possible. The presentation is similar to mitral stenosis, but the absence of loud S1 and an opening snap helps to distinguish between the 2 conditions. Chest radiography revealing pulmonary congestion with an absence of left atrial enlargement is characteristic of cor triatriatum. A continuous gradient on Doppler echocardiography confirms the diagnosis.[10][12]
Physical Examination
The following physical examination findings are due to right heart failure and pulmonary congestion:
- Accentuated pulmonary component of S2
- A soft midsystolic murmur at the upper left sternal border
- Right ventricular heave
- Basilar rales
- Diminished peripheral pulses
- Hepatomegaly and right upper quadrant tenderness
- Ascites
- Peripheral edema
- Distended peripheral veins
- Jugular venous distension and elevated jugular venous pressure
- Pallor
- Poor weight gain
Evaluation
The mainstay of diagnosing and evaluating cor triatriatum includes imaging studies such as chest radiography, electrocardiography, echocardiography, angiography, and left and right heart catheterization.[13][14]
Chest Radiography
A chest radiograph is the initial diagnostic tool of choice. Typical findings include:
- Pulmonary congestion with haziness
- Ground glass appearance of acute pulmonary edema
- Prominent pulmonary vessels
- Pleural effusion
- Left atrial enlargement
- Cardiomegaly
Electrocardiography
Electrocardiography findings are nonspecific in cor triatriatum. Studies may reveal atrial fibrillation and no specific P-wave changes to right axis deviation due to pulmonary congestion and right ventricular hypertrophy.
Echocardiography
Echocardiography is the diagnostic modality of choice when cor triatriatum is suspected. This modality allows for definitive diagnosis; the 3-dimensional reconstruction of echocardiographic images pinpoints the exact location of the defect and appendage and helps direct the surgical approach to the disease. In the case of cor triatriatum sinisterum, the left atrial appendage and its fenestrations can be easily visualized with an atrial septal defect, pulmonary stenosis, mitral valve stenosis, or regurgitation. Pulmonary arterial and venous drainage patterns can also be observed on echocardiography. Echocardiography differentiates between cor triatriatum and supravalvular mitral stenosis by clearly visualizing the left atrial appendage in the left atrium.
Sometimes, ambiguous anatomy not properly elucidated on a transthoracic window warrants further investigation with transesophageal echocardiography with or without bubble study.[15][16]
Cardiac Catheterization and Angiography
Angiography helps determine the severity of obstruction and the timing of surgical intervention. In addition, catheterization helps quantify pulmonary hypertension, the degree of shunting between the left and right hearts, and oxygen saturation changes in the cardiac chambers.
Computed Tomography and Magnetic Resonance Imaging
Such advanced imaging techniques are typically reserved for complex anatomy, such as multiple combined cardiac anomalies, or to help formulate an intraoperative strategy for a stratified case.
Treatment / Management
Medical Management
Asymptomatic patients: Asymptomatic patients require no specific treatment. Observe them for the development of signs and symptoms and schedule regular medical follow-ups.
Symptomatic patients: Treatment options for symptomatic patients include conservative medical management and surgical repair. Medical treatment is reserved mainly for preoperative management of unstable or symptomatic patients and includes:
- Hemodynamic stabilization of fluid overload and pulmonary edema.[17]
- Rate and rhythm control, along with anticoagulation for patients with atrial fibrillation.[18]
- Thromboembolic prophylaxis with anticoagulation against deep vein thrombosis, pulmonary embolism, and stroke.[19] (B3)
American Heart Association Guidelines for Adults with Cor Triatriatum (2018)
- Adult patients (symptomatic or asymptomatic) with evidence of cor triatriatum should be screened for other congenital anomalies, particularly septal defects, such as atrial septal and ventricular septal defects. Pulmonary vein defects are also associated with cor triatriatum and should be suspected.
- Investigating pulmonary vein stenosis is prudent in symptomatic patients who have undergone successful repair of cor triatriatum in the past.
- Symptoms attributed to pulmonary venous inflow obstruction or a high-pressure gradient across a restrictive fibromuscular membrane are reasonable indications for surgical repair.[20] (A1)
Surgical Management
Surgery is the definitive treatment for cor triatriatum.[6][21] Complete surgical resection of the atrial accessory membrane with optional left atrial appendage exclusion is performed through a midline sternotomy under aorto-bicaval cardiopulmonary bypass. If an atrial septal defect is present, it is closed with a pericardial patch, providing the optimum cure. Typically, these patients have prolonged mitral stenosis and an enlarged left atrium, making access through the heart through the interatrial groove a better choice. Achieving the right visibility of the surgical area involves making a large cut in the left atrium and using special sutures to pull the edge of the heart closer into the surgical field to remove the membrane. A Beaver blade is used to carefully separate the fibrous ring from the atrial wall in a manner similar to endarterectomy. Meticulous dissection is essential to remove the fibrous ring safely without damaging the mitral valve apparatus or the conduction system.
Once the membrane is completely removed, mitral regurgitation is expected. The function of the mitral valve is then checked by injecting it with saline using a syringe. The left atrium is then stitched up carefully, de-airing is done, and the aortic clamp is removed. After the patient is warmed up and taken off the bypass machine, transesophageal echocardiography is used to examine the repaired area to ensure the surgery is successful. The 10-year survival rate following surgery is 83%, whereas patients with coexisting congenital heart diseases have a greater risk of adverse outcomes and a lower survival rate.[22][23](B2)
Differential Diagnosis
Many congenital heart diseases can present similarly to cor triatriatum and should be taken into consideration when making a diagnosis of this disorder. These include:
- Supravalvular mitral stenosis: This condition is the closest entity to cor atriatum sinistrum, both clinically and anatomically. Healthcare providers should be able to distinguish between the 2 conditions to arrive at a conclusive diagnosis more quickly and reduce unnecessary healthcare expenses. Typically, the fibromuscular membrane in cor triatriatum sinistrum is diagonal and separates the atrial appendage from the pulmonary veins with no continuity with the mitral valve annulus. In contrast, supravalvar mitral stenosis is continuous with the mitral valve annulus and does not separate the left atrial appendage from the pulmonary veins. Noteworthily, although cor triatriatum is still not associated with any genetic mutation or disease, the supravalvular mitral stenosis is a recognized component of the Shone complex.
- Mitral stenosis
- Idiopathic pediatric pulmonary arterial hypertension
- Pulmonary venous hypertension
- Total anomalous pulmonary venous return
- Partial anomalous pulmonary venous return
- Atrial septal defect/ventricular septal defect
- Ventricular septal defect
- Idiopathic pulmonary hypertension
- Tricuspid stenosis
- Atrial myxoma
An experienced surgical team should evaluate imaging results, as high suspicion can accelerate diagnosis and delay or prevent unfavorable outcomes.
Complications
Complications of cor triatriatum include:
- Right-sided heart failure
- Reduced cardiac output
- Stunted growth
- Pulmonary edema/hypertension
- Atrial arrhythmias
- Thromboembolism
- Death
Deterrence and Patient Education
Clinicians involved in the care of cor triatriatum include:
- Pediatric cardiologist
- Pediatric cardiac surgeon
- Intensivist
Enhancing Healthcare Team Outcomes
Diagnosing and treating cor triatriatum requires an interprofessional approach. Cor triatriatum is a very rare congenital heart disorder. However, most infants are symptomatic at birth and require neonatal intensive care unit care. Nurses play a crucial role in monitoring these infants both pre- and post-surgery, particularly for arrhythmias, pulmonary edema, or right heart failure. The outcomes for untreated infants are poor, whereas the outcomes for other infants with cor triatriatum depend on the presence of other co-existing heart defects. For infants with only the cor triatriatum defect, the outcomes are excellent.
Surgery should be at centers with experience with this disorder. Althotugh it appears that only the accessory membrane needs to be resected, the small size of the left atrium and the collapse of the structure during cardiopulmonary bypass can make visualization difficult.[22][24]
Media
(Click Image to Enlarge)
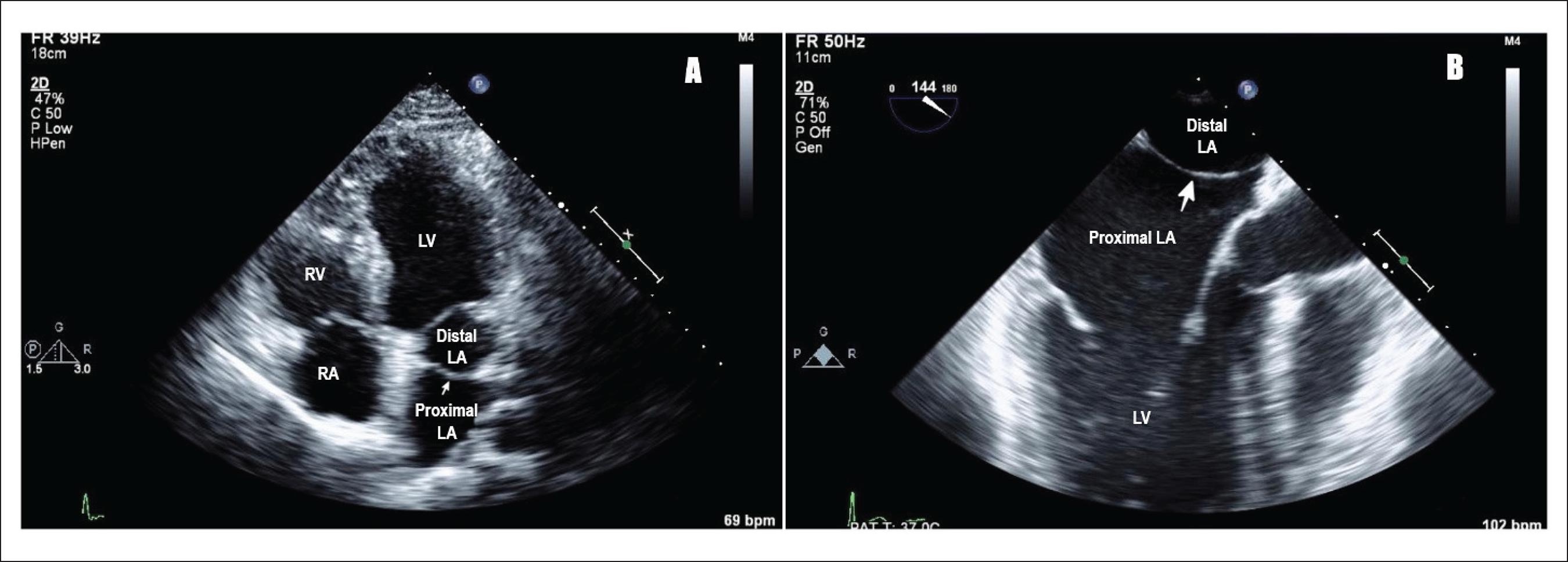
Cor Triatriatum. A) Transthoracic echocardiogram showing cor triatriatum: proximal and distal left atrium separated by a membrane (pointing white arrow), LA (left atrium), LV (left ventricle), RV (right ventricle), RA (right atrium). B) Transesophageal echocardiogram showing cor triatriatum: proximal and distal left atrium separated by a membrane (pointing white arrow), LA (left atrium), and LV (left ventricle).
Raheja H, Namana V, Moskovits N, Hollander G, Shani J. Cor triatriatum sinistrum. Arq. Bras. Cardiol. 2018;110(1). doi: 10.5935/abc.20170138. CC license 4.0.
References
Jha AK, Makhija N. Cor Triatriatum: A Review. Seminars in cardiothoracic and vascular anesthesia. 2017 Jun:21(2):178-185. doi: 10.1177/1089253216680495. Epub 2017 Apr 19 [PubMed PMID: 27913770]
Elagizi A, Marvin R, O'Bryan G, Vyas V, Arcement L. Three's a Crowd - An Extremely Rare Case of Cor Triatriatum Dexter. The Journal of the Louisiana State Medical Society : official organ of the Louisiana State Medical Society. 2017 Mar-Apr:169(2):50-51 [PubMed PMID: 28414671]
Level 3 (low-level) evidenceThilenius OG, Bharati S, Lev M. Subdivided left atrium: an expanded concept of cor triatriatum sinistrum. The American journal of cardiology. 1976 Apr:37(5):743-52 [PubMed PMID: 1266740]
Goel A, Viswamitra S, Reddy BN, Gaduputi J. Computed tomography features of cor triatriatum: an institutional review. The British journal of radiology. 2021 Mar 1:94(1119):20201252. doi: 10.1259/bjr.20201252. Epub 2021 Jan 5 [PubMed PMID: 33400560]
Mashadi AH, Narasimhan SL, Said SM. Cor triatriatum sinister: Long-term surgical outcomes in children and a proposal for a new classification. Journal of cardiac surgery. 2022 Dec:37(12):4526-4533. doi: 10.1111/jocs.17032. Epub 2022 Nov 2 [PubMed PMID: 36321701]
Kilkenny K, Frishman W. Cor Triatriatum: A Review. Cardiology in review. 2023 Nov 15:():. doi: 10.1097/CRD.0000000000000626. Epub 2023 Nov 15 [PubMed PMID: 37966218]
Nassar PN, Hamdan RH. Cor Triatriatum Sinistrum: Classification and Imaging Modalities. The European journal of cardiovascular medicine. 2011 Jan:1(3):84-87 [PubMed PMID: 22379596]
Aldawoodi NN, Arora H, Kumar PA. Incidental discovery of an unusual right atrial membrane in an adult patient. Annals of cardiac anaesthesia. 2012 Oct-Dec:15(4):309-11. doi: 10.4103/0971-9784.101870. Epub [PubMed PMID: 23041691]
PARSONS CG. Cor triatriatum; concerning the nature of an anomalous septum in the left auricle. British heart journal. 1950 Oct:12(4):327-38 [PubMed PMID: 14777837]
Narayanapillai J. Cor triatriatum sinister with severe obstruction: a rare presentation in an adult. BMJ case reports. 2016 Aug 5:2016():. doi: 10.1136/bcr-2016-215718. Epub 2016 Aug 5 [PubMed PMID: 27495175]
Level 3 (low-level) evidenceHumpl T, Reineker K, Manlhiot C, Dipchand AI, Coles JG, McCrindle BW. Cor triatriatum sinistrum in childhood. A single institution's experience. The Canadian journal of cardiology. 2010 Aug-Sep:26(7):371-6 [PubMed PMID: 20847964]
Level 2 (mid-level) evidenceChen Q, Guhathakurta S, Vadalapali G, Nalladaru Z, Easthope RN, Sharma AK. Cor triatriatum in adults: three new cases and a brief review. Texas Heart Institute journal. 1999:26(3):206-10 [PubMed PMID: 10524744]
Level 3 (low-level) evidenceOstman-Smith I, Silverman NH, Oldershaw P, Lincoln C, Shinebourne EA. Cor triatriatum sinistrum. Diagnostic features on cross sectional echocardiography. British heart journal. 1984 Feb:51(2):211-9 [PubMed PMID: 6691871]
Level 3 (low-level) evidenceThakrar A, Shapiro MD, Jassal DS, Neilan TG, King ME, Abbara S. Cor triatriatum: the utility of cardiovascular imaging. The Canadian journal of cardiology. 2007 Feb:23(2):143-5 [PubMed PMID: 17311121]
Level 3 (low-level) evidenceHamdan R, Mirochnik N, Celermajer D, Nassar P, Iserin L. Cor Triatriatum Sinister diagnosed in adult life with three dimensional transesophageal echocardiography. BMC cardiovascular disorders. 2010 Oct 28:10():54. doi: 10.1186/1471-2261-10-54. Epub 2010 Oct 28 [PubMed PMID: 21029431]
Level 3 (low-level) evidenceSlight RD, Nzewi OC, Mankad PS. Echocardiographic diagnosis of cor triatriatum sinister in the adult. Heart (British Cardiac Society). 2004 Jan:90(1):63 [PubMed PMID: 14676245]
Level 3 (low-level) evidenceSentilhes L, Verspyck E, Bauer F, Marpeau L. Management of maternal cor triatriatum during pregnancy. Obstetrics and gynecology. 2004 Nov:104(5 Pt 2):1212-5 [PubMed PMID: 15516457]
Hayes C, Liu S, Tam JW, Kass M. Cor Triatriatum Sinister: An Unusual Cause of Atrial Fibrillation in Adults. Case reports in cardiology. 2018:2018():9242519. doi: 10.1155/2018/9242519. Epub 2018 Mar 31 [PubMed PMID: 29808125]
Level 3 (low-level) evidencePark KJ, Park IK, Sir JJ, Kim HT, Park YI, Tsung PC, Chung JM, Park KI, Cho WH, Choi SK. Adult cor triatriatum presenting as cardioembolic stroke. Internal medicine (Tokyo, Japan). 2009:48(13):1149-52 [PubMed PMID: 19571448]
Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM, Crumb SR, Dearani JA, Fuller S, Gurvitz M, Khairy P, Landzberg MJ, Saidi A, Valente AM, Van Hare GF. 2018 AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Apr 2:139(14):e698-e800. doi: 10.1161/CIR.0000000000000603. Epub [PubMed PMID: 30586767]
Level 1 (high-level) evidenceAl Kindi HN, Shehata M, Ibrahim AM, Roshdy M, Simry W, Aguib Y, Yacoub MH. Cor Triatriatum Sinister (Divided Left Atrium): Histopathologic Features and Clinical Management. The Annals of thoracic surgery. 2020 Oct:110(4):1380-1386. doi: 10.1016/j.athoracsur.2020.01.025. Epub 2020 Feb 28 [PubMed PMID: 32114046]
Fuchs MM, Connolly HM, Said SM, Egbe AC. Outcomes in patients with cor triatriatum sinister. Congenital heart disease. 2018 Jul:13(4):628-632. doi: 10.1111/chd.12624. Epub 2018 Jul 22 [PubMed PMID: 30033682]
Ozyuksel A, Yildirim O, Avsar M, Hayirlioglu M, Demiroluk S, Kucukosmanoglu O, Bilal MS. Surgical correction of cor triatriatum sinister in the paediatric population: mid-term results in 15 cases. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2015 Jan:47(1):e25-8. doi: 10.1093/ejcts/ezu390. Epub 2014 Oct 13 [PubMed PMID: 25312520]
Level 2 (mid-level) evidenceAn G, Zhang H, Zheng S, Wang W, Ma L. Mid-term Outcomes of Common Congenital Heart Defects Corrected Through a Right Subaxillary Thoracotomy. Heart, lung & circulation. 2017 Apr:26(4):376-382. doi: 10.1016/j.hlc.2015.05.028. Epub 2016 Feb 17 [PubMed PMID: 27876287]