Definition/Introduction
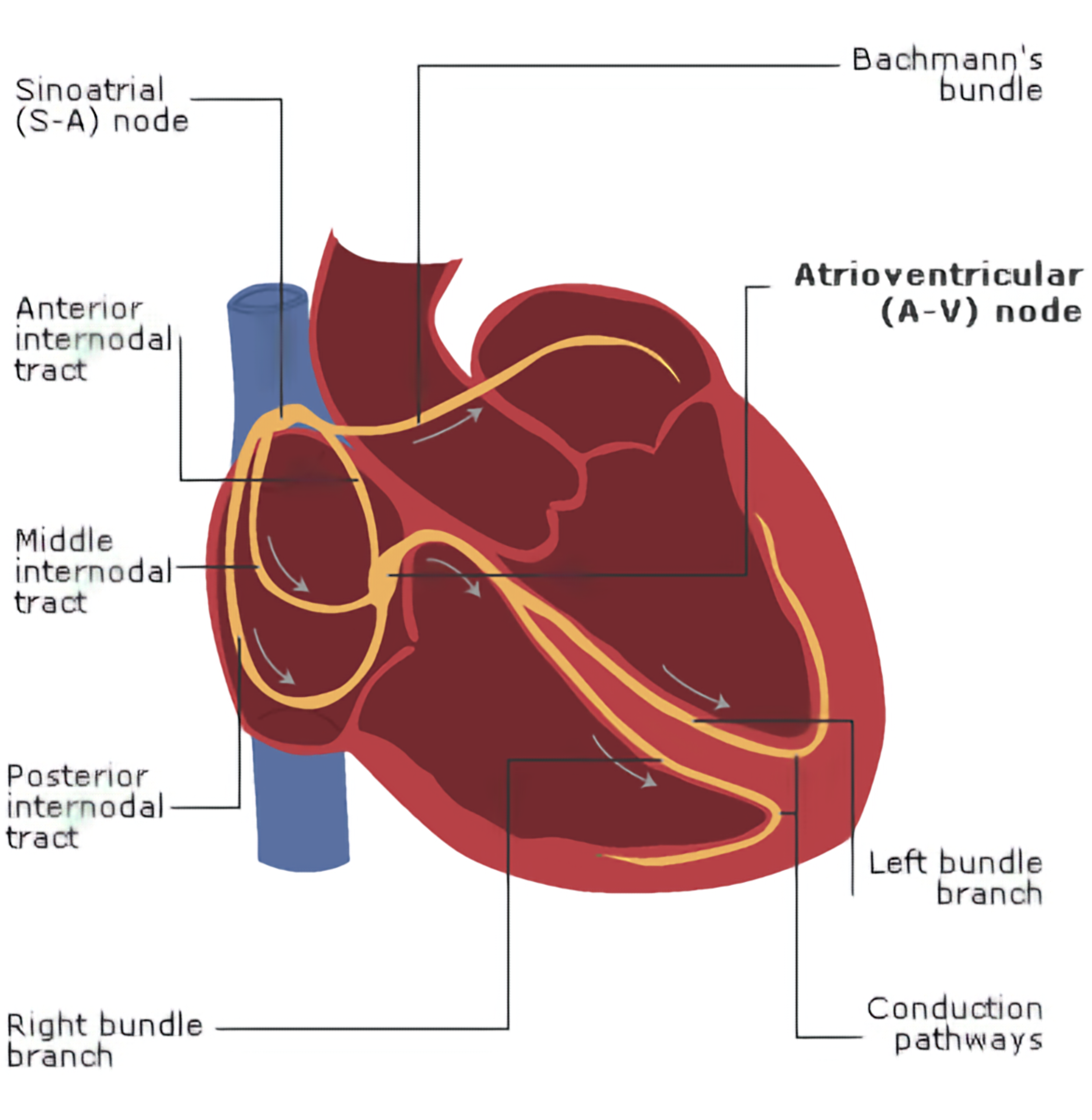
The atrioventricular (AV) node is a small structure in the heart, located in the Koch triangle,[1] near the coronary sinus on the interatrial septum. In a right-dominant heart, the atrioventricular node is supplied by the right coronary artery. The purpose of this structure is to connect the electrical systems of the atria and the ventricles, providing electrical impedance from the atria and an intrinsic pacemaker in its absence. The intrinsic rate of the AV node is 40 to 60 beats per minute (bpm).
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
AV Block
The AV node can hinder electrical conduction, causing a pathologic state. In heart block, a 2-degree heart block is specifically related to the AV node.[2] The first type, Mobitz I or Wenckebach heart block, is when the AV node becomes increasingly refractory to impulses, resulting in a dropped beat.[3] This phenomenon is preceded by increasing PR intervals, giving a characteristic electrocardiogram (EKG) finding.
Though similar by name, the cause of Mobitz I is distinctly different from Mobitz II. In Mobitz II, a lesion within the His-Purkinje system causes dropped beats.[4] The EKG finding is distinct through the presentation of dropped beats without an increasing PR interval. This rhythm can easily lead to a complete heart block.
Cystic Tumor of the Atrioventricular Nodal Region (CTAVN)
Primary tumors of the cardiac system are rare. Cystic tumors of the AV nodal region (CTAVN) is an example for which only about 70 cases have been identified.[5] The tumor grows at the base of the interatrial septum and can disrupt the electrical conduction pathway, leading to sudden cardiac death.[6] Terminal events may be preceded by syncopal episodes and identified as heart block on an EKG.
Clinical Significance
Understanding the anatomy and function of the AV node is crucial for understanding pathologic conditions that may present in the clinical setting.
Junctional Escape Beat
A junctional escape beat originates in the AV node when impulses from pacemakers upstream are not enough to overtake the AV node's intrinsic activity. Due to this bradycardia, an ectopic beat is generated in the AV node, which then conducts downstream along the normal pathway, causing synchronized ventricular depolarization. This condition can be provoked due to excessive vagal tone, pathologies associated with the SA node, or in the setting of heart block. Classic EKG findings include pulse rates of 40 to 60 bpm, regular rhythm, and a narrow QRS complex. Additionally, inverted P-waves may be present, though they can be hidden within the QRS complex. This is due to retrograde conduction to the atria from the AV node generated impulse.
Accelerated Junctional Rhythm and Junctional Tachycardia
Accelerated junctional rhythm and junctional tachycardia are two forms of an accelerated rhythm originating from the AV node. In accelerated junctional rhythm, a pathologic AV node generates an electrical impulse at a rate of 60 to 100 bpm; in junctional tachycardia, the accelerate rate is higher than 100 bpm.[7] In both cases, the AV node becomes a generator of ventricular depolarization, providing a narrow QRS complex, and a regular rhythm on EKG. In the setting of heart block, accelerated AV nodal rhythms may be concurrent with other forms of supraventricular tachycardia (SVT).
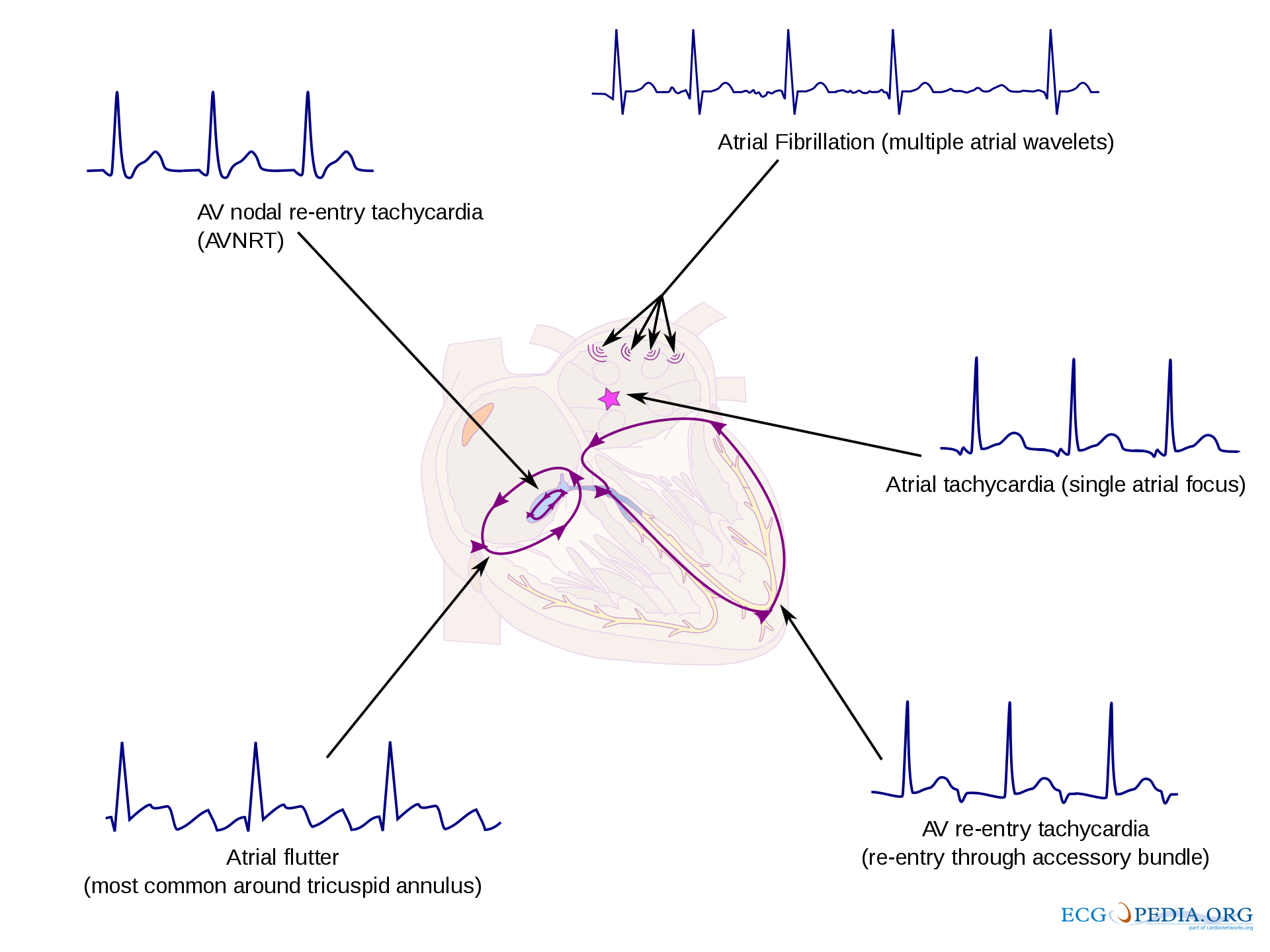
Atrioventricular Nodal Reentry Tachycardia (AVNRT)
In or near the AV node, fast and slow pathways conduct electrical activity similar to a healthy AV node. In typical AVNRT, the P wave is conducted through the fast pathway, anterograde towards the ventricles; the signal is then conducted through the slow pathway, retrograde back to the atria. This can be seen on EKG as a P wave after the QRS complex. Multiple atypical AVNRT variations exist, depending on the pathway configurations. Ablation therapy may resolve AVNRT.[8]
Junctional Ectopic Tachycardia (JET)
Junctional ectopic tachycardia is a rare condition typically seen in newborns and post-cardiac surgery.[9][10] In JET, there is a short circuit through the AV node, which bypasses the normal gatekeeper function. Consequently, impulses generated by the atria can be conducted to the ventricles without impedance, up to a 1 to 1 ratio. JET can be distinguished from AVNRT using adenosine; in JET, the tachycardia will continue without AV dissociation; however, in AVNRT, adenosine should terminate the arrhythmia.
Wolff–Parkinson–White Syndrome (WPW)
Wolff–Parkinson–White syndrome is a pathologic state of cardiac electrical conducting system, insomuch as it averts the AV node. An accessory or extra pathway, known as the Bundle of Kent, allows impulses from the sinoatrial (SA) node to bypass the AV node and cause excitation of the ventricles.[11] Without the gatekeeping function of the AV node, the ventricles can conduct up to the rate of the atrium, which is particularly dangerous in SVTs. Wolff–Parkinson–White syndrome can be differentiated from AVNRT and JET as the accessory pathway is outside of the AV node. On EKG, WPW can be identified through the characteristic delta wave.[12]
Atrioventricular Reentry Tachycardia (AVRT)
ANRT may occur only when an accessory bundle is present. In typical AVRT, the impulse conducts through the normal pathway, from the sinoatrial node to the bundle branches; instead of the impulse terminating at the bundle branches, it conducts through the accessory pathway towards the AV node. When the original impulse arrives at the AV node, it reenters the normal conduction pathway, forming a loop and causing additional action potentials. This condition is differentiated from AVNRT by the conduction path. In AVRT, the conduction travels through the bundle branches and reenters the AV node through an accessory pathway. In AVNRT, the loop is contained within the AV node and does not require an accessory pathway outside the AV node. Attached media provides a visual representation.
Nursing, Allied Health, and Interprofessional Team Interventions
Identification of an AV nodal pathology is crucial to the diagnosis and management of potentially fatal syndrome from nonspecific symptoms. Often the presentation of these potentially fatal syndromes is with apparently benign symptoms such as palpitations. In some cases, patients may present with syncope as well. However, upon evaluation, the EKG may only have subtle signs of disease which require astute observation and a high index of suspicion. Thus, an interprofessional team, including physicians, electrophysiological, and telemetry trained nurses, are required in the care of these patients. Each member of the interprofessional team plays an important role in diagnosing these patients in a timely manner. When clinical suspicion is high, cardiac specialists should be consulted for evaluation and consideration of diagnostic or therapeutic procedures. A collaborative interprofessional team can greatly improve outcomes in patients with AV nodal disease and arrhythmias.
Media
(Click Image to Enlarge)
References
Kurian T, Ambrosi C, Hucker W, Fedorov VV, Efimov IR. Anatomy and electrophysiology of the human AV node. Pacing and clinical electrophysiology : PACE. 2010 Jun 1:33(6):754-62. doi: 10.1111/j.1540-8159.2010.02699.x. Epub 2010 Feb 18 [PubMed PMID: 20180918]
Level 3 (low-level) evidenceScheinman MM. Atrioventricular nodal conduction and refractoriness. Pacing and clinical electrophysiology : PACE. 1993 Mar:16(3 Pt 2):592-8 [PubMed PMID: 7681963]
Roberts NK, Cabeen WR. Atrioventricular nodal function in progressive systemic sclerosis: electrophysiological and morphological findings. British heart journal. 1980 Nov:44(5):529-33 [PubMed PMID: 7437193]
Benson DW. Genetics of atrioventricular conduction disease in humans. The anatomical record. Part A, Discoveries in molecular, cellular, and evolutionary biology. 2004 Oct:280(2):934-9 [PubMed PMID: 15372490]
Level 3 (low-level) evidenceSharma G, Linden MD, Schultz DS, Inamdar KV. Cystic tumor of the atrioventricular node: an unexpected finding in an explanted heart. Cardiovascular pathology : the official journal of the Society for Cardiovascular Pathology. 2010 May-Jun:19(3):e75-8. doi: 10.1016/j.carpath.2008.10.011. Epub 2009 Jan 14 [PubMed PMID: 19144541]
Level 3 (low-level) evidenceSuzuki K, Matsushita S, Suzuki H, Kuroda K, Inaba H, Arakawa A, Hayashi T, Amano A, Kuwatsuru R. Cystic tumor of the atrioventricular node: computed tomography and magnetic resonance imaging findings. Journal of thoracic imaging. 2014 Nov:29(6):W97-9. doi: 10.1097/RTI.0000000000000111. Epub [PubMed PMID: 25303965]
Level 3 (low-level) evidenceHafeez Y, Grossman SA. Junctional Rhythm. StatPearls. 2023 Jan:(): [PubMed PMID: 29939537]
Lee PC, Chen SA, Hwang B. Atrioventricular node anatomy and physiology: implications for ablation of atrioventricular nodal reentrant tachycardia. Current opinion in cardiology. 2009 Mar:24(2):105-12. doi: 10.1097/HCO.0b013e328323d83f. Epub [PubMed PMID: 19225293]
Level 3 (low-level) evidenceKylat RI, Samson RA. Junctional ectopic tachycardia in infants and children. Journal of arrhythmia. 2020 Feb:36(1):59-66. doi: 10.1002/joa3.12282. Epub 2019 Dec 3 [PubMed PMID: 32071621]
Catton KG, Peterson JK. Junctional Ectopic Tachycardia: Recognition and Modern Management Strategies. Critical care nurse. 2020 Feb 1:40(1):46-55. doi: 10.4037/ccn2020793. Epub [PubMed PMID: 32006036]
Chhabra L, Goyal A, Benham MD. Wolff-Parkinson-White Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 32119324]
Kesler K, Lahham S. Tachyarrhythmia in Wolff-Parkinson-White Syndrome. The western journal of emergency medicine. 2016 Jul:17(4):469-70. doi: 10.5811/westjem.2016.4.30323. Epub 2016 Jun 16 [PubMed PMID: 27429700]