Introduction
Brachium is a Latin word meaning the upper arm. This part of the upper limb contains powerful muscles that carry a considerable portion of the upper limb function. Also, vital peripheral nerves pass through the upper limb, namely the brachial plexus neurons. The brachial artery is the single most important blood vessel that gives branches to supply the whole upper limb. Because of the previously mentioned valuable structures, injury to the upper arm can cause severe problems in the entire upper limb.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The upper limb can be divided anatomically into the shoulder, arm, elbow, forearm, wrist, and hand, respectively. The hand muscles can also divide into two compartments separated by two fascial septa, one on the medial side and the other on the lateral side. Muscles of the anterior fascial compartment contain biceps brachii, coracobrachialis, brachialis. The muscle of the posterior fascial compartment contains the three head of the triceps muscle.[1]
The subdivision into compartments and fascial planes, in reality, is a didactic approach, as we know that in vivo, the muscular, vasculonervous, and purely connective structures are a continuum.
Embryology
During embryological development, the upper limb starts to develop before the lower limb and occurs approximately in the sixth week of intrapartum development. As a result of the proliferation of the mesenchymal cells, the limb buds start to appear. At this stage, there are two borders, each innervated by a specific segment of the brachial plexus, cephalic portion mainly supplied by the lower five cervical nerve, and the caudal portion, which will be innervated by the eighth cervical and first thoracic nerve. The cephalic portion will differentiate into the upper arm as part of embryonic development.
The upper limbs develop from a proliferation of the mesoderm of the somatopleure in the lateral region of the body, which forms outgrowths in correspondence of the cervical tract (5 degrees to 8 degrees somite cervical).The individual growths, consisting of a core of mesenchymal cells covered by a layer of cubic ectodermal cells, constitute the outline of the limb. When this bud lengthens, the cells of the ectodermal surface at the distal edge proliferate and synthesize bone morphogenetic factors (BMP), forming a thickened apical ectodermal crest (AER). AER overlooks a vascular canal whose integrity is essential for limb growth. The development of the limb is dependent on the interaction between the mesenchyme of the limb bud and the AER, which induces proliferation of the underlying mesenchyme and ensures growth and differentiation of the draft of the limb along the near-distal axis.
The proliferating mesenchyme zone immediately below the apical ectodermal crest is called the advancement zone (PZ). The AER induces the proliferation of the underlying mesenchyme thanks to the production of fibroblast growth factor (FGF). The dorsal epidermis supports this mechanism by expressing the factor Wnt family member 7a (Wnt7a). The distal growth of the limb completes via the cells of the progression zone (ZP), which produces large quantities of FGF factors. The medial-lateral specification of the limb is regulated by the polarizing zone (ZPA), which expresses the sonic hedgehog factor (Shh). The muscular component of each limb originates from the abaxial myotomes in the corresponding region. Myoblasts comprise the abaxial myotome, in the portion of the somite furthest from the neural tube.
Blood Supply and Lymphatics
Blood Supply
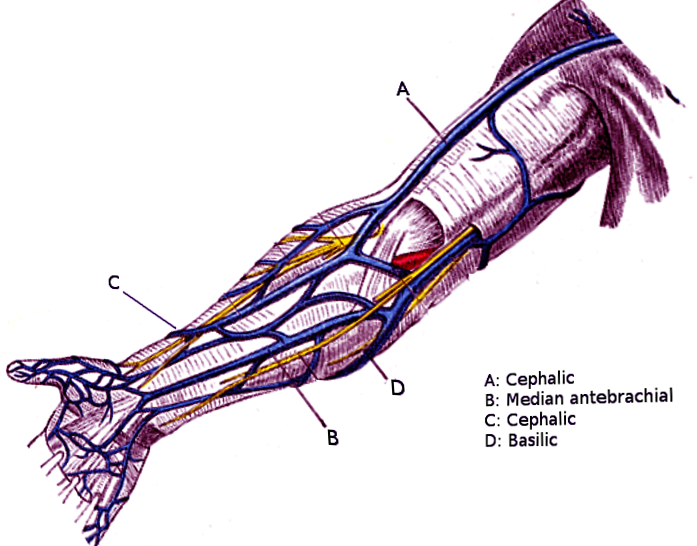
The brachial artery is the main arterial supply to the arm. It starts from the lower border of teres major muscle as a continuation of the axillary artery, and it ends opposite to the neck of the radius by dividing it to ulnar and radial arteries. The brachial artery branches are the nutrient branch to the humerus, the profunda artery and ulnar collateral arteries that supply the posterior fascial compartment.[2] The venous return of the arm is guaranteed in particular by the cephalic, basilica, and brachial veins.
Lymphatics
The superficial lymphatic vessels drain the superficial tissue upward to the axilla, those from the lateral side of the arm follow the cephalic vein to the infraclavicular nodes; those from the medial side the arm follow basilic vein to the lateral group of axillary nodes. Whereas the deep lymphatic vessels drain the muscles and deeper structures to the lateral group of axillary nodes.[3]
Nerves
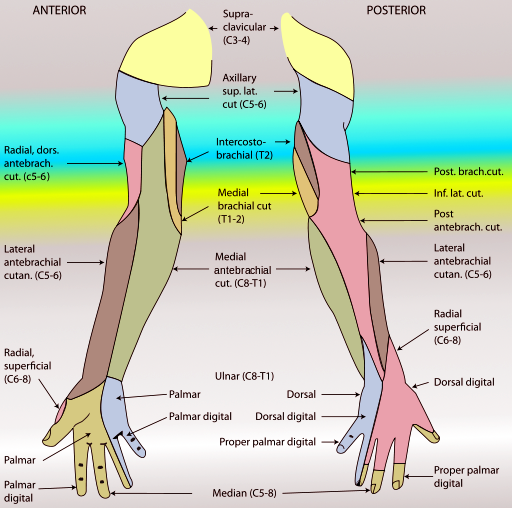
Most of the brachial plexus branches pass through the arm; the following nerves pass through the upper arm[4][5]:
Musculocutaneous nerve: which innervates the biceps, coracobrachialis, and brachialis muscles. Plus, it gives a sensory branch to the lateral forearm and articular branch to the elbow. Its origin is the lateral cord of the brachial plexus (C5,6,7). The nerve runs downward and laterally piercing the coracobrachialis muscle then runs between the biceps and brachialis muscles. It terminates as the lateral cutaneous nerve of the forearm.
Median nerve: originates from the medial and lateral cord of the brachial plexus. It runs downward and lateral to the brachial artery in the upper arm halfway its course crosses the artery to reside on its medial side. The median nerve gives no branches to the arm except for small vasomotor branches to the brachial artery.
Ulnar nerve: this nerve gives no branches in the arm, mainly innervates the hand. The origin of the ulnar nerve is from the eighth cervical and first thoracic roots of the brachial plexus. The ulnar nerve runs downward at the medial side of the brachial artery. At the level of the insertion of the coracobrachialis, it pierces the medial fascial septum to enter the posterior compartment then the nerve runs posteriorly to the medial epicondyle of the humerus.
Radial nerve: originates from the posterior cord of the brachial plexus. The nerve rotates around the humerus in the spinal groove accompanied by the profunda artery, and it lies directly in contact with the humerus shaft. It goes through the lateral fascial septum downward and in front of the cubital fossa between the brachialis and brachioradialis. It gives cutaneous branches as the posterior cutaneous nerve of the arm, inferior lateral cutaneous nerve of the arm and posterior cutaneous nerve of the forearm. And muscular branches to triceps brachii, anconeus, brachioradialis, and extensor carpi radialis longus.
Muscles
The anterior compartment of the arm contains (biceps brachii, coracobrachialis, brachialis)[1]:
The biceps brachii: the long head originates from the supraglenoid tubercle of the scapula, and the short head originates from the tip of the coracoid process of the scapula. The insertion of this muscle will be on the posterior part of the radius tuberosity and by the bicipital aponeurosis to the medial aspect of the forearm. It serves as a powerful supinator of the forearm and flexion of the elbow joint and plays a minimal role in flexion of the shoulder. Innervated by the musculocutaneous nerve.
The coracobrachialis: the name of the muscle explains it very well; it starts from the coracoid process and inserts into the middle of the medial side of the humerus. It flexes the arm and serves as a weak adductor. The musculocutaneous nerve innervates it.
The brachialis: it started from the front of the lower half of the humerus and inserted in the anterior aspect of the coronoid process of the ulna. It is a strong elbow flexor. Innervated by musculocutaneous nerve and a small part of the muscle by the radial nerve.[6]
The posterior fascial compartment contains ( three heads of the triceps muscle)[1]:
The triceps muscle: long head from infraglenoid tubercle, the lateral head from the upper half of the posterior surface of humerus shaft above the spiral grove, and the medial from the lower half of the shaft of the humerus at the posterior surface below the spiral grove. They all inserted into the ulna olecranon as a common tendon. The action of this muscle is the extension of the elbow joint and supplied by the radial nerve.
Physiologic Variants
The literature shows several anatomical variants, in particular supernumerary head of the biceps brachii (one or two more). The same-origin of the muscle can have multiple branches; there is also a trifurcate intra-articular of the long head of the biceps tendon.
There is a rare formation, a strip of muscle which departs from the pectoralis major muscle and which inserts on the epicondyle of the humeral bone; it is called chondroepitrochlearis.
Another rare formation is the elevator muscle of the tendon of latissimus dorsi muscle, which arises from the coracoid process (with a fusiform shape and a short tendon), and inserts in a portion of the tendon of the latissimus muscle (dorsal and upper area of the tendon).
There are anatomical variants of the coracobrachialis muscle, where additional bellies may occur.
The brachialis muscle may have a fascial sheet, which could become one of the causes that compress the median nerve.
The brachial triceps muscle can have a four-headed triceps and/or receive innervation by the median nerve or the musculocutaneous nerve.
Surgical Considerations
The Surgical Neck
Fractures at the surgical neck are more frequent than fractures at the anatomical neck, very important structures pass through the surgical neck, the axillary nerve, and the posterior circumflex humeral artery. Damage to those structures may cause paralysis of the deltoid and teres minor muscles and loss of dermal sensation over the lower half of the deltoid muscle.[7]
The Spiral Groove
Injuries to the radial nerve in the spiral groove, the injury to the radial nerve occurs most commonly in the distal part of the groove, beyond the origin of the nerves to the triceps, the anconeus and the origin of the cutaneous nerves. The patient is unable to extend the wrist, and the fingers “wrist drop” and a variable, small area of loss of the sensation is present over the dorsal surface of the hand and the dorsal surface the lateral three and a half fingers except the tips of the fingers.[8]
Clinicians can treat the presence of adhesion neuropathy of the median nerve with neurolysis; as with other nerves, it can be transferred to restore the function of neighboring non-functional nerves for various causes (arthrogryposis multiplex congenita, penetrating injuries, palsy, etc.).
Clinical Significance
Biceps Brachii and Osteoarthritis of the Shoulder Joint
The tendon of the long head of biceps attaches to the supraglenoid tubercle in the shoulder joint. Advanced osteoarthritic changes of the joint can lead to erosion and fraying of the tendon by osteophytes outgrowth, and the rupture of the tendon can occur.[9]
Volkmann Ischemic Contracture
In cases like fracture of the humerus or bones of the forearm, spasmatic effects to the brachial artery either from a tight cast application or from the fracture itself can cause a decrease in blood supply to the arm muscles, eventually leading to necrosis and fibrosis of the muscles. Because the muscles on the flexor side are larger than the extensor muscles, they are more vulnerable to ischemia and necrosis. The result is permanent flexion deformity involving the upper limb due to ischemic contractures, and the deformity resembles a claw-like deformity.[10]
The presence of trigger points in the muscular areas of the arm can create dysfunctions in the function of the muscles themselves and peripheral neurological alterations (allodynia, hyperalgesia).
Other Issues
One of the strategies used in rehabilitation to help recover arm muscles (for example, after surgery) is to stimulate the healthy contralateral arm. The basis for this therapy is the phenomenon known as crossed facilitation. When the healthy arm is in motion, through corticospinal projections, it activates the nerve fibers of the arm to be recovered are activated. If the spinal cord is injured, this mechanism may have decreased.[11][12]
Constant pain in the cervical area for various causes could alter the arthro-kinematics of the arm, prolonging or causing chronic neck dysfunction.[13]
The fascial osteopathic approach to the arm muscles can raise the pain threshold by acting on the peripheral receptors of the connective tissue. When the problem causing muscle pain is long-lasting, the proprioceptors can send nociceptive information; by changing the mechanical status of the muscle area, it is possible to improve mechanical afferents and reduce the sensation of pain.[14][15]
Media
(Click Image to Enlarge)
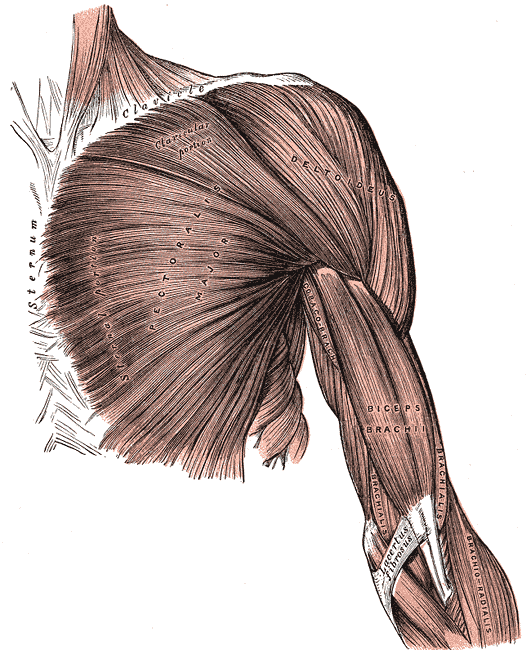
Superficial Muscles of the Chest and Shoulder. This illustration shows the pectoralis major, deltoid, coracobrachialis biceps brachii, brachialis, and brachioradialis. Other structures included in this image are the clavicle, sternum, and lacertus fibrosus.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
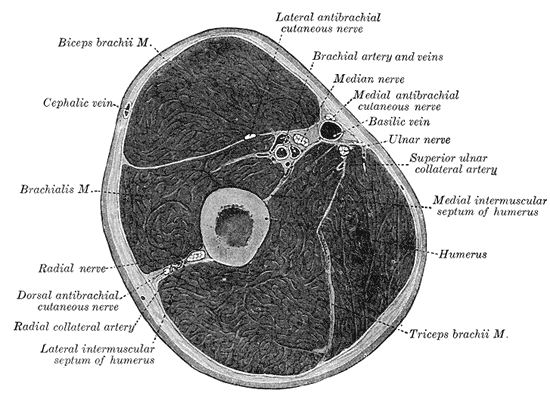
Fascial Compartments of the Arm, Biceps Brachii, Cephalic vein, Brachialis, Radial Nerve, Radial Nerve, Dorsal antebrachial cutaneous nerve, Radial Collateral artery, Lateral intermuscular septum of humerus, Triceps Brachii, Humerus, Medial intermuscular septum of humerus, Superior ulnar collateral artery, Ulnar nerve, Basilic vein, Medial antebrachial cutaneous nerve, Brachial artery and vein, Lateral antebrachial cutaneous nerve.
Henry Vandyke Carter, Public domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Javed O, Maldonado KA, Ashmyan R. Anatomy, Shoulder and Upper Limb, Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 29494017]
de la Garza O, Lierse W, Steiner D. Anatomical study of the blood supply in the human shoulder region. Acta anatomica. 1992:145(4):412-5 [PubMed PMID: 10457786]
Cuadrado GA, de Andrade MFC, Akamatsu FE, Jacomo AL. Lymph drainage of the upper limb and mammary region to the axilla: anatomical study in stillborns. Breast cancer research and treatment. 2018 Jun:169(2):251-256. doi: 10.1007/s10549-018-4686-1. Epub 2018 Jan 29 [PubMed PMID: 29380209]
Okwumabua E, Thompson JH. Anatomy, Shoulder and Upper Limb, Nerves. StatPearls. 2023 Jan:(): [PubMed PMID: 30252312]
Becker RE, Manna B. Anatomy, Shoulder and Upper Limb, Ulnar Nerve. StatPearls. 2023 Jan:(): [PubMed PMID: 29763067]
Ilayperuma I, Uluwitiya SM, Nanayakkara BG, Palahepitiya KN. Re-visiting the brachialis muscle: morphology, morphometry, gender diversity, and innervation. Surgical and radiologic anatomy : SRA. 2019 Apr:41(4):393-400. doi: 10.1007/s00276-019-02182-2. Epub 2019 Feb 28 [PubMed PMID: 30820647]
Lee W, Park JY, Chun YM. Operative Treatment of 2-Part Surgical Neck Fracture of the Humerus: Intramedullary Nail Versus Locking Compression Plate With Technical Consideration. Journal of orthopaedic trauma. 2017 Sep:31(9):e270-e274. doi: 10.1097/BOT.0000000000000916. Epub [PubMed PMID: 28622154]
Mostafa E, Imonugo O, Varacallo M. Anatomy, Shoulder and Upper Limb, Humerus. StatPearls. 2023 Jan:(): [PubMed PMID: 30521242]
Ibrahim M, Kartus JT, Steigen SE, Olsen R, Meknas K. More tendon degeneration in patients with shoulder osteoarthritis. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2019 Jan:27(1):267-275. doi: 10.1007/s00167-018-5186-x. Epub 2018 Oct 3 [PubMed PMID: 30284007]
Jaryal A, Vikrant S, Thakur P. Volkmann's ischemic contracture: An unusual complication of arterio-venous fistula. Hemodialysis international. International Symposium on Home Hemodialysis. 2017 Jan:21(1):E1-E3. doi: 10.1111/hdi.12444. Epub 2016 Jun 21 [PubMed PMID: 27329788]
Bunday KL, Perez MA. Impaired crossed facilitation of the corticospinal pathway after cervical spinal cord injury. Journal of neurophysiology. 2012 May:107(10):2901-11. doi: 10.1152/jn.00850.2011. Epub 2012 Feb 22 [PubMed PMID: 22357796]
Chiou SY, Strutton PH, Perez MA. Crossed corticospinal facilitation between arm and trunk muscles in humans. Journal of neurophysiology. 2018 Nov 1:120(5):2595-2602. doi: 10.1152/jn.00178.2018. Epub 2018 May 30 [PubMed PMID: 29847230]
Zabihhosseinian M, Holmes MW, Howarth S, Ferguson B, Murphy B. Neck muscle fatigue differentially alters scapular and humeral kinematics during humeral elevation in subclinical neck pain participants versus healthy controls. Journal of electromyography and kinesiology : official journal of the International Society of Electrophysiological Kinesiology. 2017 Apr:33():73-82. doi: 10.1016/j.jelekin.2017.02.002. Epub 2017 Feb 14 [PubMed PMID: 28226297]
Bordoni B, Marelli F, Morabito B, Castagna R. Chest pain in patients with COPD: the fascia's subtle silence. International journal of chronic obstructive pulmonary disease. 2018:13():1157-1165. doi: 10.2147/COPD.S156729. Epub 2018 Apr 12 [PubMed PMID: 29695899]
Bordoni B, Bordoni G. Reflections on osteopathic fascia treatment in the peripheral nervous system. Journal of pain research. 2015:8():735-40. doi: 10.2147/JPR.S89393. Epub 2015 Oct 30 [PubMed PMID: 26586962]