Introduction
Vision is perhaps the most useful of the senses for humans. More than 50% of the sensory receptors in the human body are located in the eyes, and a significant portion of the cerebral cortex is devoted to interpreting visual information. The eyes are responsible for detecting visible light, which ranges from 400 to 700 nanometers in wavelength. Objects can absorb and reflect different wavelengths of light. An object appears white if it reflects all wavelengths of light, and it appears black if it absorbs all wavelengths of light.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Accessory Structures of the Eye
The accessory structures of the eye include the eyelids, eyelashes, eyebrows, the lacrimal apparatus, and extrinsic eye muscles.[1][2][3][4]
Functions of the Accessory Structures of the Eye
The eyelids, also known as the palpebrae, cover the eyes during sleep, protect the eyes from excess light and possibly objects, and spread lubricating secretions over the eyeball. The upper eyelid exhibits a greater range of movement than the lower eyelid as it contains the levator palpebrae superioris muscle, a muscle innervated by cranial nerve 3 in charge of lifting the eyelid. Beneath this layer is a donut-shaped muscle that encircles the eye called orbicularis oculi, which is innervated by the 7th cranial nerve, and is in charge of closing the eyelids. Twitches of the eyelids are a common and usually harmless symptom that can be caused by stress and fatigue. The space between the upper and lower eyelid that exposes the eyeball is the palpebral fissure. The lacrimal caruncle is the small, pink, globular spot at the inner corner, or the medial canthus, of the eye. It contains both oil and sweat glands. The whitish material that sometimes accumulates in that region is from these glands. The tarsal plate is composed of connective tissue that gives support to the eyelids. The conjunctiva is a thin, protective mucous that covers the sclera of the eye. It does not cover the cornea, which is a transparent region that forms the outer anterior surface of the eye.
The lacrimal apparatus produces and drains lacrimal fluid, or tears, from the eye. The lacrimal glands, each about the size of an almond, secrete the lacrimal fluid that drains into six to 12 excretory ducts that empty the fluid onto the surface of the conjunctiva of the upper eyelid. From there, the tears enter two small openings called lacrimal punta, and then they pass into two ducts knowns as the lacrimal canals. The two lacrimal canals lead to the lacrimal sac and then into the nasolacrimal duct. The nasolacrimal duct carries lacrimal fluid into the nasal cavity. This is why the nose gets stuffy when an individual cries.[6]
The extrinsic eye muscles extend from the bony orbit to the sclera of the eye and are surrounded by a significant amount of periorbital fat. Together, these muscles are capable of moving the eye in almost any direction.
Anatomy and Function of the Eyeball
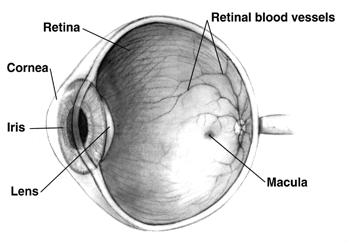
The adult eyeball measures about 2.5 centimeters in diameter and only one-sixth of the eyeball is exposed to the outside air. The rest of the eyeball is protected by the orbit into which it fits. Anatomically, the wall of the eyeball is composed of three layers: the fibrous tunic, the vascular tunic, and the retina. The fibrous tunic is the outermost layer and consists of the anterior cornea and the posterior sclera. The cornea is transparent and covers the colored iris. The outer surface of the cornea is composed of non-keratinized stratified squamous epithelium. The middle coat of the cornea is composed of collagen fibers and fibroblasts, while the inner surface is simple squamous epithelium. The central part of the cornea receives oxygen from the outside air, so it is important for contact lenses to be permeable to oxygen. The sclera is the white of the eye and covers the entire eyeball except for the cornea. It protects its inner parts, gives shape to the eyeball, and makes it more rigid.[5]
The vascular tunic, also known as the uvea, is the middle layer of the eyeball. It is composed of three parts: the choroid, the ciliary body, and the iris. The choroid is the posterior portion of the vascular tunic, and it lines the internal surface of the sclera. Its numerous blood vessels provide nutrients to the retina. Also, the choroid contains melanocytes that produce the pigment melanin. Melanin in the choroid absorbs excess light, which prevents reflection and scattering of light within the eyeball. Albinos lack melanin in all parts of their body; therefore, they often need to wear sunglasses because bright light is perceived as a bright glare. In the anterior portion of the vascular tunic, the choroid becomes the ciliary body, which is composed of ciliary processes and ciliary muscle. The ciliary processes contain blood capillaries that secrete aqueous humor. Furthermore, the zonular fibers that attach to the lens extend from the ciliary processes. The ciliary muscle contracts and relaxes in order to change the tightness of the zonular fibers which in turn alters the shape of the lens, adjusting it for near or far vision. The iris is the colored portion of the eye. It is located between the cornea and the lens and it attached to the ciliary processes. The amount of melanin in the iris determines eye color. The main function of the iris is to regulate how much light passes through the pupil, the hole in the center of the iris.
The third and innermost layer of the eyeball is the retina. It consists of a pigmented layer and a neural layer. The pigmented layer is a sheet of melanin-containing epithelial cells that is located between the choroid and the neural part of the retina. The neural, or sensory, layer is an outgrowth of the brain that processes visual data extensively before sending electrical impulses to the axons of the optic nerve. The three distinct layers of the retinal neurons are the ganglion cell layer, the bipolar cell layer, and the photoreceptor layer. Light passes through both the ganglion and bipolar cell layers before it reaches the photoreceptor layer. Photoreceptors are specialized cells that convert light rays into nerve impulses. The two types of photoreceptor cells are rods and cones. Each retina contains about 6 million cones and more than 100 million rods. Cones produce color vision, while rods enable us to see in dim light. Color vision results from the stimulation of different combinations of blue, green, and red cones. Eventually, the visual information reaches the optic disk, also called the blind spot because it contains no rod or cone cells. The macula lutea is a flat spot that is located in the exact center of the posterior portion of the retina. The fovea centralis is located in the center of the macula lutea and it contains only cones. It is the area of highest visual acuity or resolution with highest density of cone photoreceptors and exclusion of rod receptors. This is the part of the eye we use to focus on something we are looking at.
The lens is located in the cavity of the eyeball, behind the pupil and iris. It is suspended from ciliary body muscles via zonule fibers. Ciliary body muscles provideaccomodation during the near vision. The lens divides the interior of the eyeball into two cavities: the anterior cavity and the vitreous cavity. The anterior cavity, the space anterior to the lens, is divided into the anterior chamber and the posterior chamber. The anterior chamber is located between the cornea and the iris. The posterior chamber is located behind the iris and in front of the zonular fibers and lens. Both chambers of the anterior cavity are filled with aqueous humor, a watery fluid that nourishes the cornea and lens. The aqueous humor is produced by epithelium of the ciliary body and is replaced every 90 minutes. The final destination of this fluid inside of the eye is schlemm's canal which drain the fluid into the body circulation. [6] The larger cavity of the eyeball is the vitreous cavity, located between the lens and the retina. Within the vitreous chamber is the vitreous body, a transparent jellylike substance that holds the retina against the choroid. Unlike the aqueous humor, the vitreous body does not undergo rapid replacement. It contains phagocytic cells that remove debris to maintain unobstructed vision.
Occasionally, some debris may cast a shadow on the field of vision and these are known as vitreal floaters. They are much more common in older individuals.
Embryology
Formation of the eye in the human embryo begins approximately three weeks into embryonic development and continues through the tenth week. Cells from both the ectodermal and the mesodermal tissues contribute to its development. Specifically, the eye is derived from the neuroepithelium, the surface ectoderm, and the extracellular mesenchyme which consists of both the neural crest and mesoderm. Neuroepithelium forms the retina, ciliary body, iris, and optic nerves. Surface ectoderm forms the lens, corneal epithelium, and eyelid. The extracellular mesenchyme forms the sclera, the corneal endothelium, stroma, blood vessels, muscles, and vitreous.
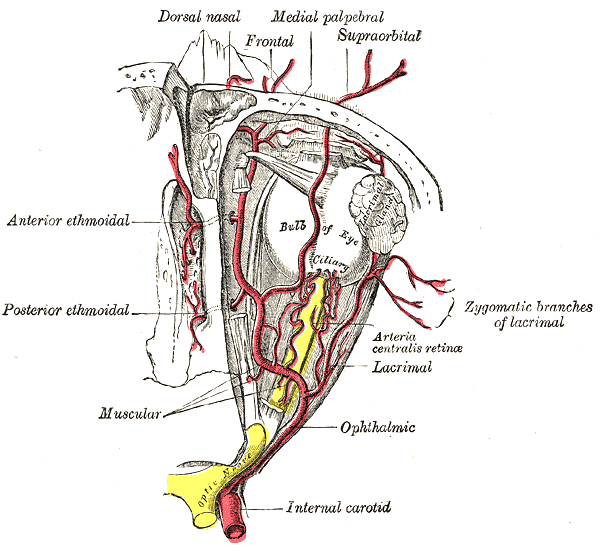
Blood Supply and Lymphatics
All eye structures, except for the eyelids and conjunctiva, are supplied by branches of the internal carotid artery. The external carotid artery supplies the eyelids and conjunctiva. The internal carotid artery has many branches; one is the ophthalmic artery. This artery branches into the posterior ciliary, retinal, and muscular arteries. These arteries supply blood to the ciliary bodies, retina, and muscles, respectively. The central retinal artery is a branch of ophthalmic artery which runs within the optic nerve.
Nerves
The optic nerve is the sensory nerve that transmits impulses from the retina to the brain. The oculomotor , trochlear, and abducens nerve innervate the extraocular muscles. The oculomotor nerve has The ophthalmic nerve branches into the lacrimal, frontal, and nasociliary nerves. The lacrimal nerve runs to the lacrimal glands and branches off to other areas. The frontal nerve supplies sensation to the superior eyelid and forehead. The nasociliary nerve is the sensory nerve to the eyeball.[7][8]
Muscles
Six extrinsic eye muscles that move each eye: (1) superior rectus, (2) inferior rectus, (3) lateral rectus, (4) medial rectus, (5) superior oblique, and (6) inferior oblique. Lateral rectus is innervated by trochlear and superior oblique is innervated by abducens nerve; The oculomotor nerve innervates the remaining four muscles. The motor units in these muscles tend to be small with neurons serving only two or three muscle fibers at times. Such small motor units allow precise and rapid eye movement. Portions of the brainstem and cerebellum coordinate eye movements.
Clinical Significance
The eyeball is a complex structure with many small organs that are essential for vision and movement of the eye. An injury to any part of the eye can result in discomfort, reduced vision, and in some cases blindness. The eye is a source of injury, infection, and multiple medical diseases. It is important for all health practitioners to be able to identify and describe the anatomical features of the eye.
One complication that can occur in an eye is a detached retina, which can be caused by both trauma to the head and time. The detachment occurs between the neural portion of the retina and pigment epithelium. Fluid accumulates between these layers, and the result is distorted vision or partial blindness. Reattachment of the retina can be accomplished through laser surgery and should be done as quickly as possible to avoid permanent damage to the retina.
Another eye-related disease is age-related macular disease, which is also known as macular degeneration (AMD). AMD is a degenerative disorder of the retina that affects the macula lutea. Individuals with AMD retain their peripheral vision but lose their ability to see straight ahead. AMD is the most common cause of blindness for people over the age of 75. It afflicts over 13 million Americans, and there is no effective treatment.[9]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
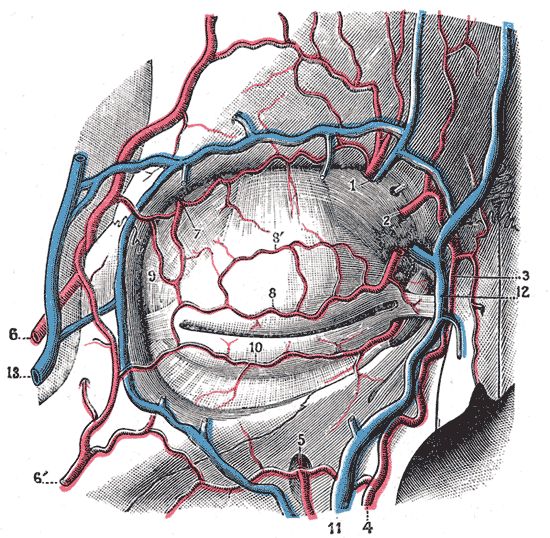
Blood Vessels of the Eyelids, Front View. Labeled structures include the following: 1. supraorbital artery and vein; 2. nasal artery; 3. angular artery, the terminal branch of 4. the facial artery; 5. suborbital artery; 6. anterior branch of the superficial temporal artery; 6’. malar branch of the transverse artery of the face; 7. lacrimal artery; 8. superior palpebral artery with 8’. superior palpebral artery's external arch; 9. anastomoses of the superior palpebral with the superficial temporal and lacrimal; 10. inferior palpebral artery; 11. facial vein; 12. angular vein; 13. branch of the superficial temporal vein.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
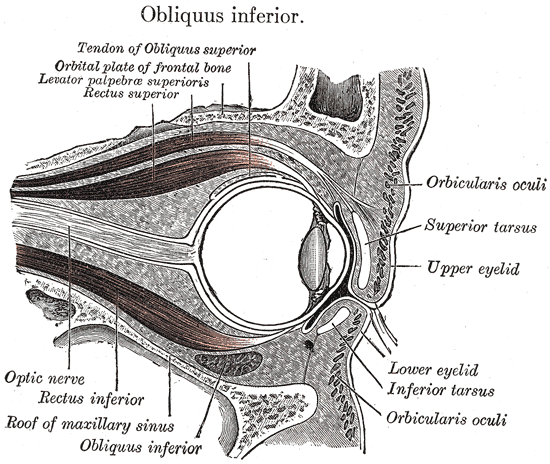
The Accessory Organs of the Eye, Sagittal section of right orbital cavity, Upper and lower Eyelid, Inferior Tarsus, Orbicularis oculi, Optic Nerve, Rectus inferior, Roof of maxillary sinus, Obliquus inferior, Tendon of obliquus superior, Rectus superior
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
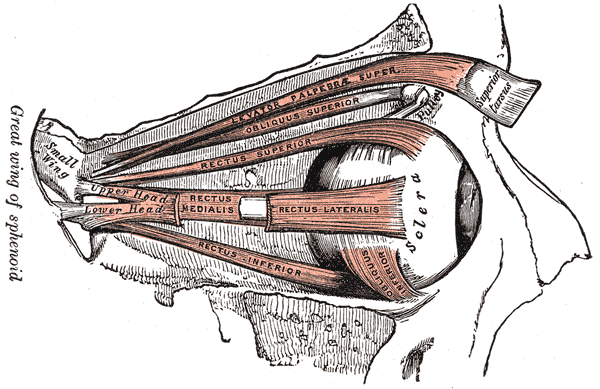
Orbital Muscles. This image shows the anatomical relationships between the levator palpebrae superioris, superior and inferior obliques, and superior, lateral, inferior, and medial recti. The sphenoid's greater wing, the sclera, and the superior tarsus are also referenced.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Ali MJ, Paulsen F. Human Lacrimal Drainage System Reconstruction, Recanalization, and Regeneration. Current eye research. 2020 Mar:45(3):241-252. doi: 10.1080/02713683.2019.1580376. Epub 2019 Feb 22 [PubMed PMID: 30793623]
Patel BC, Lopez MJ, Joos ZP. Anatomy, Head and Neck: Eyelash. StatPearls. 2023 Jan:(): [PubMed PMID: 30725963]
Abdelhady A, Patel BC, Aslam S, Al Aboud DM. Anatomy, Head and Neck: Eye Superior Oblique Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 30725837]
Gupta N, Motlagh M, Singh G. Anatomy, Head and Neck, Eye Arteries. StatPearls. 2023 Jan:(): [PubMed PMID: 30725748]
Knight B, Lopez MJ, Patel BC. Anatomy, Head and Neck: Eye Levator Palpebrae Superioris Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 30725606]
Karpinich NO, Caron KM. Schlemm's canal: more than meets the eye, lymphatics in disguise. The Journal of clinical investigation. 2014 Sep:124(9):3701-3. doi: 10.1172/JCI77507. Epub 2014 Jul 25 [PubMed PMID: 25061871]
Kim SY, Motlagh M, Naqvi IA. Neuroanatomy, Cranial Nerve 4 (Trochlear). StatPearls. 2023 Jan:(): [PubMed PMID: 30725929]
Belliveau AP, Somani AN, Dossani RH. Pupillary Light Reflex. StatPearls. 2024 Jan:(): [PubMed PMID: 30725865]
Zhao S, Lan X, Wu J, Yue S, Zhang H, Wu Q, Zhang G, Liu L. Protocol of global incidence and progression of age-related macular degeneration: A systematic review. Medicine. 2019 Mar:98(10):e14645. doi: 10.1097/MD.0000000000014645. Epub [PubMed PMID: 30855452]
Level 1 (high-level) evidence