Introduction
Otitis media with effusion (OME) is a condition in which there is fluid in the middle ear but no signs of acute infection. As fluid builds up in the middle ear and Eustachian tube, it places pressure on the tympanic membrane. The pressure prevents the tympanic membrane from vibrating properly, decreases sound conduction, and therefore results in a decrease in patient hearing. Chronic OME is defined as OME that persists for 3 or more months on examination or tympanometry, although some clinicians recommend reserving the term ‘chronic otitis media’ for patients in which the tympanic membrane has perforated.[1]
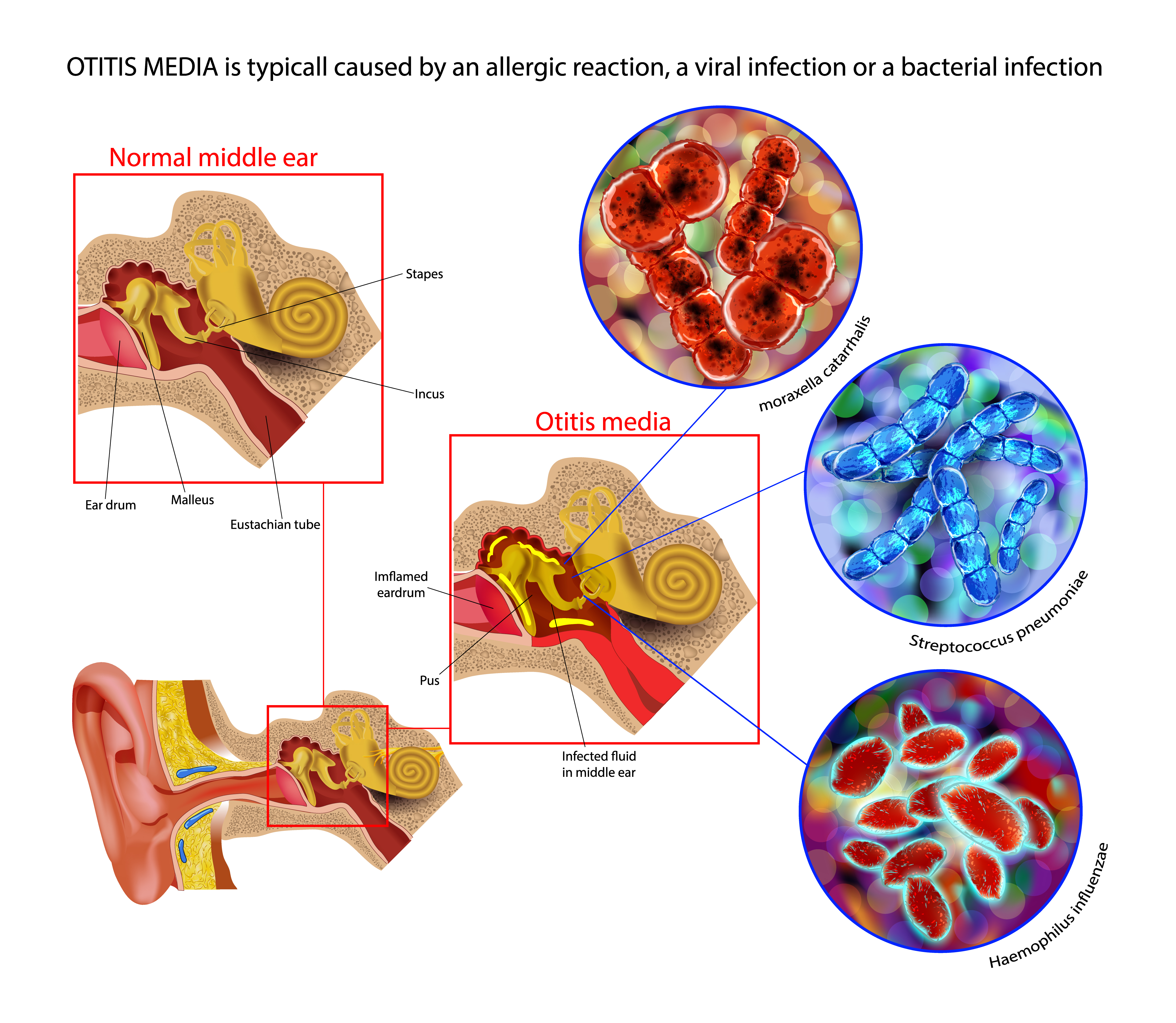
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Risk factors for OME include passive smoking, bottle feeding, daycare nursery, and atopy. [2] Both children and adults can develop OME. However, the etiology of these populations is different. The Eustachian tube is positioned more horizontally in younger children. As the child develops into an adult, the tube elongates and angles caudally. Therefore, OME is more common in children, and the position of the head at this age can influence the development of OME. [3] Children with development anomalies including the palate, palate muscles, decreased muscle tone for palate muscles, or bone development variations are at increased risk of development of OME, e.g., cleft palate, Down Syndrome. [4] Beyond these anatomical variations, patients with Downs syndrome can have mucociliary function disorders that increase the risk of developing OME. [2][5]
Epidemiology
OME is one of the most frequent infectious diseases in children and is the most common cause of acquired hearing loss in childhood. [6] The disease commonly affects children between the ages of 1 and 6. There is a higher prevalence at the age of 2, which drops after the age of 5. OME is more prevalent during the winter months, corresponding to higher patient rates of upper respiratory infections.
Pathophysiology
After an acute otitis media in children, fluid builds up in the middle ear, inhibiting vibration of the tympanic membrane and subsequent transmission of sound into the inner ear. With this deficit, children may have a decreased ability to communicate in noisy environments. The child may show signs of inattention or decreased academic performance.
In patients with large adenoids, the adenoids can obstruct the Eustachian tube resulting in a poorly ventilated middle ear. This type of blockage may result in OME. Because the adenoids are a lymphatic structure, it is possible that they can transmit bacteria into the Eustachian tube and allow the growth of biofilms. Such bacterial growth can cause inflammation that would also facilitate blockage and fluid build-up within the middle ear.
Histopathology
The first line of defense in the middle ear is thought to be the mucociliary defense system in the Eustachian tube. Immunoglobulins produced by the mucosa contribute to this defense system. Due to the significant elevation of these immunoglobulins in effusions, these defense systems may be overactive in OME. [7]
Toxicokinetics
Otitis may also be caused by inflammation driven by viruses or allergies. While allergy is a significant risk factor for otitis media, clinical practice guidelines (2004) concluded that there was little evidence to support specific management strategies for allergy-induced OME. However, it is logical to conclude that aggressive treatment of allergic rhinitis may assist patients that develop OME in conjunction with allergies.[8]
History and Physical
Hearing loss, although not always present, is the most common complaint in OME patients. Patients or parents of patients may complain of communication difficulties, withdrawal, and lack of attention. During an exam, a clinician may notice impaired speech and language development. Otalgia and earache can be intermittent in these patients. In many instances, they will have the symptom of aural fullness or a sensation that the ear is popping. In adults, OME is more often unilateral. Adult patients may report tinnitus and the sensation of a foreign body in the external auditory canal. In either children or adults, OME commonly occurs concurrently with upper respiratory infections. Therefore, it is good to ask patients about prior or recurrent ear infections, nasal obstruction, and upper respiratory tract infections.
During a physical examination, signs of OME include opacification of the tympanic membrane and loss of the light reflex. There may also be a retraction of the tympanic membrane with decreased mobility. If gross retraction of the tympanic membrane is observed, intervention may be required to prevent the formation of a retraction pocket, such as modified cartilage augmentation tympanoplasty.[9][1]
Evaluation
Age appropriate audiometry and tympanometry should be tested in patients with otitis media with effusion. A ‘flat’ tympanogram will support a diagnosis of otitis media with effusion. [10]Hearing can be tested in infants with the use of auditory brainstem responses (ABR). This exam tests the electrical activity of the brainstem to acoustic stimuli. The test detects both the frequency range and sound intensity levels in which the patient’s brain responds. Patients do not need to be able to speak and do not even need to be awake to perform the test. Therefore, it is ideal for children from birth to 5 years of age. [11]
With older children and adults, although ABR testing can still be performed, it is more common to do a classic audiology exam. This exam consists of playing sounds to the patient’s left and right ears at different tones and intensities. Patients are requested to raise either the right or left hand when they hear a sound in the right or left ears, respectively. Results will identify the frequency range and normal hearing levels of the patient.
Individuals with normal hearing can detect lower frequencies at a lower decibel (i.e., intensity) than higher frequencies, meaning that a normal individual needs a sound to be louder to perceive high frequencies than lower frequencies. During an audiology exam, the range of frequencies that an individual can perceive is plotted on an audiograph. The decibel (dB) range of individuals with OME is decreased in the audiograph.
Hearing loss levels (reduction in hearing thresholds from normal levels):
- Slight impairment: 26-40 dB
- Moderate impairment: 41-60 dB
- Severe impairment: 61-80 dB
- Severe hearing loss: 71-90 dB
- Profound impairment, including deafness: 81 dB or higher.[12]
Treatment / Management
Otitis media with effusion generally resolves spontaneously with watchful waiting. However, if it is persistent, myringotomy with tympanostomy tube insertion is considered an effective treatment.[13] In this treatment, a ventilation tube allows for air entry into the middle ear, preventing the re-accumulation of fluid. After this procedure, many patients do not need additional therapy due to the growth and development of the Eustachian tube angle, which will allow for drainage. The most common complication is the development of persistent otorrhea. Otorrhea is seen in nearly 1 in 6 (16%) of children within 4 weeks of surgery, and in 26% of children during the entire period, the tube is in place.
Adenoidectomy is currently utilized in cases of OME that involve enlarged adenoids and is an important addition to management in patients with OME. [14]
Childhood hearing loss can affect language development.[15] Therefore hearing aids may be considered a non-invasive option to treat OME.[16]
Clinician decisions for the correct interventional treatment of OME for a specific patient include a variety of factors.
- Comorbidities of the patient
- The severity of hearing loss
- OME presence unilaterally or bilaterally
- Effusion duration
- Age of patient
Social factors
- Cost to patient
- Patient’s likelihood of adherence to treatment
- Familial assistance with treatment
A patient-focused approach should be adopted when assessing hearing disability. How the child is coping socially and at school is more important than the results of audiometry investigations.[17][18][19] Although most OME patients will warrant a conservative management approach as opposed to more invasive interventions, all physical and social factors should be examined to provide a patient-centered treatment plan that optimizes outcomes for the patient.[20][21][22](A1)
Differential Diagnosis
OME needs to be distinguished from acute otitis media [23], and in adults, OME can be caused by a nasopharyngeal carcinoma infiltrating the Eustachian tube. [24]
Surgical Oncology
Although patients with OME may show no signs or symptoms except for the loss of hearing associated with OME, 5.7% of patients develop the OME due to an obstruction caused by a nasopharyngeal carcinoma. Examination of the nasopharynx, as well as the external acoustic meatus, is suggested with OME patients. If abnormalities are observed within the nasopharynx, a biopsy of the postnasal space is suggested. [25]
Radiation Oncology
In patients with nasopharyngeal carcinoma, OME can be induced by radiation treatments. This type of OME may persist over several months. [26] More research is needed to determine the risks of developing OME post-radiotherapy and how irradiation dosages may influence this complication. [27]
Pertinent Studies and Ongoing Trials
Several different therapies have been tried to find effective treatment options for OME. The use of oral steroids in children has shown some benefits. However, it is unknown whether these benefits are clinically significant.[28] Otic drops have also been utilized to maintain tympanostomy tube patency. These trials showed no statistical differences in the occlusion rate between patients that received the drug therapy and control (no drug) conditions.[29]
Treatment Planning
OME is most commonly caused by either viral or allergy-related factors, not bacterial infection. Therefore, the use of antibiotics is not recommended. Also, corticoids for the treatment of allergies have not been significantly proven to impact the outcomes of OME in patients. For these reasons, antibiotics and corticoids are not recommended to treat OME. The best practice for OME patients is watchful waiting for three months as a first-line measure. In cases where OME persists, a specialist referral may be made to assess for surgical treatment options.[30]
Toxicity and Adverse Effect Management
Ototopical drops can be ototoxic if they enter the middle ear and reach the inner ear.[31] However, ototopical drops are not routinely used to treat OME.
Medical Oncology
Radiotherapy after nasopharyngeal carcinoma can produce various complications. The most common complication is xerostomia (i.e., dry mouth caused by a lack of saliva). In some cases, a persistent OME may develop, facilitating the need for additional therapy or surgical intervention.[31]
Prognosis
Most cases of OME resolve on their own. In persistent cases, the condition impedes a patient's ability to hear. Therefore, communication and socialization can be affected. In young children, hearing deficits can cause learning problems or delayed language development. The impact of OME on these factors has not been fully studied.[32] Unusual complications of OME include dizziness, behavioral disorders, and clumsiness.[33]
Complications
Long-term changes of the middle ear and tympanic membrane may occur with persistent OME, resulting in permanent hearing loss. Ventilation tubes are used to try and prevent these long-term complications. However, even in treated patients, complications such as tympanosclerosis may occur. [34]
Postoperative and Rehabilitation Care
Alongside medical and surgical treatment of OME, Eustachian tube rehabilitation may also be useful in management. Rehabilitation of the Eustachian tube can include muscle strengthening exercises for the tensor veli palatini and levator veli palatini muscles via auto-insufflation, breathing exercises, and education for the improvement of nasal hygiene.[35]
Consultations
Contact with a wide range of medical professionals, including audiologists and otolaryngologists, is important in OME to ensure holistic care for these patients.
Deterrence and Patient Education
To avoid the potential of ventilation tube complications, many doctors and parents prefer non-invasive therapies, e.g., hearing aid usage. Reassurance and explanation of the ‘watchful waiting’ approach is an important part of management for patients who do not have speech, language, or developmental problems and for those in whom audiometry shows normal hearing. If ‘watchful waiting” is utilized, the patient should be watched closely for changes in symptoms or signs of increased pressure on the tympanic membrane, as rupture would induce a poor prognosis for future hearing in these patients.
Parents of children with recurrent OME should be informed and educated about the anatomy of the middle ear. Clinicians should identify the family activities of the child in relation to the head position (e.g., breastfeeding, sleeping patterns). Manipulation of the head position during these activities may allow for optimal drainage and assist the child in the prevention of subsequent episodes of OME in the future.
Enhancing Healthcare Team Outcomes
Management goals of OME include: eliminating middle ear fluid, improving hearing, and preventing future episodes. In all cases, communication between health care providers, nurse practitioners, patients, and patients' families will assist clinicians to identify optimal treatment plans for patients with OME.
Children in whom ‘watchful waiting’ is the adopted strategy should be reassessed every 3-6 months until there is a resolution of the effusion or intervention is required. Also, families should be informed about signs and symptoms indicative of progressed pathology. In these instances, subsequent conversations about alterations to the treatment plan may be needed. The outcome for most children is good.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Emmett SD, Kokesh J, Kaylie D. Chronic Ear Disease. The Medical clinics of North America. 2018 Nov:102(6):1063-1079. doi: 10.1016/j.mcna.2018.06.008. Epub 2018 Sep 20 [PubMed PMID: 30342609]
Zernotti ME, Pawankar R, Ansotegui I, Badellino H, Croce JS, Hossny E, Ebisawa M, Rosario N, Sanchez Borges M, Zhang Y, Zhang L. Otitis media with effusion and atopy: is there a causal relationship? The World Allergy Organization journal. 2017:10(1):37. doi: 10.1186/s40413-017-0168-x. Epub 2017 Nov 14 [PubMed PMID: 29158869]
Nemade SV, Shinde KJ, Rangankar VP, Bhole P. Evaluation and significance of Eustachian tube angles and pretympanic diameter in HRCT temporal bone of patients with chronic otitis media. World journal of otorhinolaryngology - head and neck surgery. 2018 Dec:4(4):240-245. doi: 10.1016/j.wjorl.2017.12.012. Epub 2018 Mar 15 [PubMed PMID: 30564785]
Ghadersohi S, Ida JB, Bhushan B, Billings KR. Outcomes of tympanoplasty in children with down syndrome. International journal of pediatric otorhinolaryngology. 2017 Dec:103():36-40. doi: 10.1016/j.ijporl.2017.10.004. Epub 2017 Oct 5 [PubMed PMID: 29224762]
Kucur C, Şimşek E, Kuduban O, Özbay İ. Prevalence of and risk factors for otitis media with effusion in primary school children: case control study in Erzurum, Turkey. The Turkish journal of pediatrics. 2015 May-Jun:57(3):230-5 [PubMed PMID: 26701940]
Level 2 (mid-level) evidenceColeman A, Cervin A. Probiotics in the treatment of otitis media. The past, the present and the future. International journal of pediatric otorhinolaryngology. 2019 Jan:116():135-140. doi: 10.1016/j.ijporl.2018.10.023. Epub 2018 Oct 19 [PubMed PMID: 30554684]
Lim DJ. Functional morphology of the mucosa of the middle ear and Eustachian tube. The Annals of otology, rhinology, and laryngology. 1976 Mar-Apr:85(2 Suppl 25 Pt 2):36-43 [PubMed PMID: 1267366]
Level 3 (low-level) evidenceSkoner AR, Skoner KR, Skoner DP. Allergic rhinitis, histamine, and otitis media. Allergy and asthma proceedings. 2009 Sep-Oct:30(5):470-81. doi: 10.2500/aap.2009.30.3272. Epub [PubMed PMID: 19843400]
Level 3 (low-level) evidenceKasbekar AV, Patel V, Rubasinghe M, Srinivasan V. The Surgical Management of Tympanic Membrane Retraction Pockets Using Cartilage Tympanoplasty. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 2014 Dec:66(4):449-54. doi: 10.1007/s12070-014-0764-9. Epub 2014 Aug 13 [PubMed PMID: 26396960]
Cai T, McPherson B, Li C, Yang F. Pure tone hearing profiles in children with otitis media with effusion. Disability and rehabilitation. 2018 May:40(10):1166-1175. doi: 10.1080/09638288.2017.1290698. Epub 2017 Feb 25 [PubMed PMID: 28637148]
Warren MP. The auditory brainstem response in pediatrics. Otolaryngologic clinics of North America. 1989 Jun:22(3):473-500 [PubMed PMID: 2657580]
Zahnert T. The differential diagnosis of hearing loss. Deutsches Arzteblatt international. 2011 Jun:108(25):433-43; quiz 444. doi: 10.3238/arztebl.2011.0433. Epub 2011 Jun 24 [PubMed PMID: 21776317]
Teschner M. Evidence and evidence gaps in the treatment of Eustachian tube dysfunction and otitis media. GMS current topics in otorhinolaryngology, head and neck surgery. 2016:15():Doc05. doi: 10.3205/cto000132. Epub 2016 Dec 15 [PubMed PMID: 28025605]
Miller BJ, Gupta G. Adenoidectomy. StatPearls. 2025 Jan:(): [PubMed PMID: 30570973]
Lederberg AR, Schick B, Spencer PE. Language and literacy development of deaf and hard-of-hearing children: successes and challenges. Developmental psychology. 2013 Jan:49(1):15-30. doi: 10.1037/a0029558. Epub 2012 Jul 30 [PubMed PMID: 22845829]
Gan RWC, Overton P, Benton C, Daniel M. Hearing aids for otitis media with effusion: Do children use them? International journal of pediatric otorhinolaryngology. 2017 Aug:99():117-119. doi: 10.1016/j.ijporl.2017.05.027. Epub 2017 Jun 14 [PubMed PMID: 28688552]
Albrecht P. Antibiotic therapy for an ENT specialist. Otolaryngologia polska = The Polish otolaryngology. 2018 Sep 11:72(6):1-9. doi: 10.5604/01.3001.0012.4704. Epub [PubMed PMID: 30647195]
Frost HM, Gerber JS, Hersh AL. Antibiotic Recommendations for Acute Otitis Media and Acute Bacterial Sinusitis. The Pediatric infectious disease journal. 2019 Feb:38(2):217. doi: 10.1097/INF.0000000000002085. Epub [PubMed PMID: 30640191]
Ahmed A, Kolo E, Aluko A, Abdullahi H, Ajiya A, Bello-Muhammad N, Raji H, Tsiga-Ahmed F. Diagnosis and management of otitis media with effusion in a tertiary hospital in Kano: a best practice implementation project. JBI database of systematic reviews and implementation reports. 2018 Oct:16(10):2050-2063. doi: 10.11124/JBISRIR-2017-003717. Epub [PubMed PMID: 30335043]
Level 1 (high-level) evidenceAlper CM, Teixeira MS, Swarts JD. Eustachian Tube Function in Adults with Ventilation Tubes Inserted for Otitis Media with Effusion. The journal of international advanced otology. 2018 Aug:14(2):255-262. doi: 10.5152/iao.2018.4521. Epub [PubMed PMID: 30256199]
McLaren O, Toll EC, Easto R, Willis E, Harris S, Rainsbury J. Streamlining grommet pathways for otitis media with effusion and hearing loss in children: our experience. The Journal of laryngology and otology. 2018 Oct:132(10):881-884. doi: 10.1017/S0022215118001603. Epub 2018 Sep 13 [PubMed PMID: 30208983]
Simon F, Haggard M, Rosenfeld RM, Jia H, Peer S, Calmels MN, Couloigner V, Teissier N. International consensus (ICON) on management of otitis media with effusion in children. European annals of otorhinolaryngology, head and neck diseases. 2018 Feb:135(1S):S33-S39. doi: 10.1016/j.anorl.2017.11.009. Epub 2018 Feb 3 [PubMed PMID: 29398506]
Level 3 (low-level) evidenceRosenfeld RM, Culpepper L, Doyle KJ, Grundfast KM, Hoberman A, Kenna MA, Lieberthal AS, Mahoney M, Wahl RA, Woods CR Jr, Yawn B, American Academy of Pediatrics Subcommittee on Otitis Media with Effusion, American Academy of Family Physicians, American Academy of Otolaryngology--Head and Neck Surgery. Clinical practice guideline: Otitis media with effusion. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2004 May:130(5 Suppl):S95-118 [PubMed PMID: 15138413]
Level 1 (high-level) evidenceMills R, Hathorn I. Aetiology and pathology of otitis media with effusion in adult life. The Journal of laryngology and otology. 2016 May:130(5):418-24. doi: 10.1017/S0022215116000943. Epub 2016 Mar 15 [PubMed PMID: 26976514]
Ho KY, Lee KW, Chai CY, Kuo WR, Wang HM, Chien CY. Early recognition of nasopharyngeal cancer in adults with only otitis media with effusion. Journal of otolaryngology - head & neck surgery = Le Journal d'oto-rhino-laryngologie et de chirurgie cervico-faciale. 2008 Jun:37(3):362-5 [PubMed PMID: 19128640]
Level 2 (mid-level) evidenceCharusripan P, Khattiyawittayakun L. The effectiveness of myringotomy and ventilation tube insertion versus observation in post-radiation otitis media with effusion. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2017 Sep:274(9):3283-3290. doi: 10.1007/s00405-017-4617-5. Epub 2017 May 24 [PubMed PMID: 28540514]
Christensen JG, Wessel I, Gothelf AB, Homøe P. Otitis media with effusion after radiotherapy of the head and neck: a systematic review. Acta oncologica (Stockholm, Sweden). 2018 Aug:57(8):1011-1016. doi: 10.1080/0284186X.2018.1468085. Epub 2018 Apr 26 [PubMed PMID: 29698103]
Level 1 (high-level) evidenceFrancis NA, Waldron CA, Cannings-John R, Thomas-Jones E, Winfield T, Shepherd V, Harris D, Hood K, Fitzsimmons D, Roberts A, Powell CV, Gal M, Jones S, Butler CC. Oral steroids for hearing loss associated with otitis media with effusion in children aged 2-8 years: the OSTRICH RCT. Health technology assessment (Winchester, England). 2018 Nov:22(61):1-114. doi: 10.3310/hta22610. Epub [PubMed PMID: 30407151]
Dohar JE, Lu CH. Tube patency: Is there a difference following otic drop administration? American journal of otolaryngology. 2018 Jul-Aug:39(4):392-395. doi: 10.1016/j.amjoto.2018.03.027. Epub 2018 Mar 29 [PubMed PMID: 29631747]
Núñez-Batalla F, Jáudenes-Casaubón C, Sequí-Canet JM, Vivanco-Allende A, Zubicaray-Ugarteche J. Diagnosis and treatment of otitis media with effusion: CODEPEH recommendations. Acta otorrinolaringologica espanola. 2019 Jan-Feb:70(1):36-46. doi: 10.1016/j.otorri.2017.07.004. Epub 2017 Oct 13 [PubMed PMID: 29033123]
Lee CC, Ho CY. Post-treatment late complications of nasopharyngeal carcinoma. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2012 Nov:269(11):2401-9. doi: 10.1007/s00405-011-1922-2. Epub 2012 Jan 15 [PubMed PMID: 22249834]
Butler CC, MacMillan H. Does early detection of otitis media with effusion prevent delayed language development? Archives of disease in childhood. 2001 Aug:85(2):96-103 [PubMed PMID: 11466181]
van Cauwenberge P, Watelet JB, Dhooge I. Uncommon and unusual complications of otitis media with effusion. International journal of pediatric otorhinolaryngology. 1999 Oct 5:49 Suppl 1():S119-25 [PubMed PMID: 10577789]
Schilder AG. Assessment of complications of the condition and of the treatment of otitis media with effusion. International journal of pediatric otorhinolaryngology. 1999 Oct 5:49 Suppl 1():S247-51 [PubMed PMID: 10577815]
Level 1 (high-level) evidenceD'Alatri L,Picciotti PM,Marchese MR,Fiorita A, Alternative treatment for otitis media with effusion: eustachian tube rehabilitation. Acta otorhinolaryngologica Italica : organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale. 2012 Feb [PubMed PMID: 22500063]