Introduction
Like other acute myocardial infarctions, isolated lateral wall myocardial infarction (LMI) arises from acute atherosclerotic plaque rupture with subsequent thrombus formation in the left circumflex (LCx) coronary artery or one of its branches. Myocardial infarctions more commonly result from extensive anterolateral wall involvement due to blockage of the left anterior descending (LAD) coronary artery. LMI is less common than anterior or inferior myocardial infarction, with the LCx involved in approximately 15% to 20% of all myocardial infarctions. LMI presents like other types of myocardial infarction. The condition is often detected through lateral electrocardiogram (ECG) lead changes; acute treatment includes immediate reperfusion.
Myocardial infarctions are classified based on presenting ECG findings and the location of ischemia. Branches of the LAD and LCx supply the left ventricular lateral wall. Isolated lateral wall involvement is uncommon and typically occurs as part of multiterritorial infarctions, including anterolateral, posterolateral, and inferolateral myocardial infarctions (see Image. Anterolateral Myocardial Infarction on Electrocardiography). Occlusion of the obtuse LCx marginal branch or the diagonal LAD branch can cause isolated LMI.
The 2018 collaborative expert consensus from the European Society of Cardiology, American College of Cardiology, American Heart Association, and World Heart Federation issued the fourth universal definition of myocardial infarction, defining type I myocardial infarction as a rise or fall in cardiac troponin, with at least 1 value exceeding the ninety-ninth percentile and accompanied by at least 1 of the following factors:
- Symptoms of acute myocardial infarction
- New signs of ischemia on ECG
- The occurrence of pathological Q waves
- New wall motion abnormality or loss of viable myocardium, as evident on imaging
- Coronary thrombus identification on angiography [1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Causes of LMI include several conditions that can lead to the occlusion of the arteries supplying the lateral segments. These conditions include:
- Acute atherosclerotic plaque rupture with subsequent thrombus formation in the LCx or its branches or as part of a multiterritorial infarction, as occurs in pathologies involving the anterolateral, posterolateral, or inferolateral regions
- Coronary artery spasm
- Spontaneous coronary artery dissection
- Coronary artery embolism that may arise from a condition such as an atrial myxoma, atrial fibrillation, infective endocarditis, rheumatic valve disease, or mitral stenosis
- Autoimmune conditions such as Takayasu arteritis
- Myocardial bridging
- Congenital coronary artery anomalies
- Coronary microvascular disease
Epidemiology
While LMI is less commonly reported in isolation than anterior or inferior myocardial infarctions, it may also be underdiagnosed due to subtler presentations and challenges in detecting LMIs on ECG. LMIs are most often related to blockages in the LCx or its branches. The LCx is involved in approximately 15% to 20% of all myocardial infarctions. The LAD is involved more frequently, in around 40% to 50% of myocardial infarctions, while the right coronary artery is responsible for 30% to 40%. Therefore, LMI, associated with the LCx, tends to represent a smaller subset of myocardial infarctions than those involving the LAD or the right coronary artery.
The global incidence of myocardial infarction varies by region, age, gender, and risk factors. In high-income countries, the incidence of myocardial infarction is approximately 100 to 200 cases per 100,000 population per year, with rates decreasing due to improvements in preventive measures. Recent trends suggest that the incidence of ST-elevation myocardial infarction (STEMI) has declined, and the incidence of non ST-elevation myocardial infarction has increased.[2] Around 25% to 40% of myocardial infarction cases present as STEMI; among affected individuals, 23% have diabetes. Results from a study based on atherosclerosis risk in communities reported an overall LMI incidence of 13.4% among patients presenting with STEMI.[3]
Pathophysiology
Atherosclerotic plaques with large lipid-rich cores and covered by a thin, fibrous cap are extremely unstable and susceptible to rupture. Such plaques may not necessarily cause obstruction. Metalloproteases and cytokines released by T lymphocytes and macrophages present at the plaque site weaken the fibrous tissue, rendering it vulnerable to erosion.[4] Sudden acute plaque rupture exposes subendothelial collagen, which serves as a nidus for future platelet adhesion and activation. Thromboxane A2, 5-hydroxytryptamine, platelet-activating factor, and adenosine diphosphate released by platelets promote platelet aggregation and vessel vasoconstriction. Activation of the coagulation cascade results in fibrin formation and stabilization of occlusive thrombus.[5]
Prolonged ischemia leads to tissue infarction and necrosis. The subendocardial region of the ventricular wall is most prone to ischemia. However, ischemic damage can involve the entire wall thickness over time. Such ischemic events spanning the entire myocardial wall thickness present as STEMI. Infarcted tissue undergoes a series of changes from necrosis to granulation tissue and subsequent scar formation. Infarcted myocardium is extremely prone to rupture during the interval from the appearance of granulation tissue to scar formation (between 4 to 14 days post-infarction).
History and Physical
Most myocardial infarctions, regardless of location, present with a similar array of symptoms. Some of the common manifestations include left-sided chest pain radiating to the arm or neck, shortness of breath, nausea, vomiting, palpitations, diaphoresis, and fatigue. People with a prior history of myocardial infarction can relate current symptoms to previous episodes and tend to seek care sooner.
All patients suspected of having LMI warrant obtaining a thorough medical history and physical examination. Details regarding the characteristics of the chest pain, including onset, aggravating or relieving factors, and radiation, can help make an important clinical decision. Patients should be examined for signs of excessive lipid accumulation, such as xanthoma and xanthelasma.[6] Physical examination findings such as diaphoresis, extra heart sounds, heart murmurs, and elevated jugular venous pressure can guide the diagnosis of LMI.
Evaluation
Patients suspected of having acute LMI should be promptly evaluated with an ECG and a serial cardiac troponins measurement.[7][8] Recognizing distinct ST-T involvement patterns can aid in the early diagnosis of myocardial infarction.
ECG Findings
LMI-associated ECG findings include:
- ST-segment elevation LMI: ST-segment elevation in leads I, aVL, V5, and V6, with reciprocal ST depression in the inferior leads III and aVF
- High lateral STEMI: Presents with ST-segment elevation in leads I and aVL, subtle ST-segment elevation in V5 and V6, and reciprocal changes in leads III and aVF, often caused by occlusion of the first diagonal branch of the LAD (sometimes referred to as the South African flag sign)
- Old LMI: Deep and broad Q waves in leads I and aVL
- Inferolateral STEMI: ST-segment elevation in the lateral (I, aVL, V5, V6) and inferior (II, III, aVF) leads, commonly due to proximal LCx artery occlusion
- Anterolateral STEMI: ST-segment elevation in the lateral (I, aVL, V5, V6) and anterior (V1, V2, V3) leads, highly indicative of proximal LAD occlusion
Echocardiography
This modality has a high sensitivity and a low specificity when diagnosing myocardial infarction.[9] Severe ischemia produces regional wall motion abnormalities, which may be visualized on an echocardiogram.[10] However, differentiating between acute ischemia and an old infarct based on regional wall motion abnormalities is difficult. Patients with normal echocardiograms but moderate pretest probability should be evaluated with a stress test.[11] A coronary angiogram remains the most definitive diagnostic test of choice.
Treatment / Management
ST-segment elevation LMI should be treated immediately.[12] Early reperfusion has shown benefits with improved clinical outcomes.[13] Percutaneous intervention (PCI) has shown better outcomes than fibrinolytic therapy. [14] Guidelines from the American College of Cardiology and the American Heart Association for STEMI management recommend early PCI, preferably with a door-to-balloon time of less than 90 minutes at PCI-capable facilities and less than 120 minutes at non–PCI-capable facilities.[15](A1)
Antiplatelet therapy with aspirin and either a P2Y12 (clopidogrel, ticagrelor, or prasugrel) or glycoprotein IIb/IIIa inhibitor is recommended before and after PCI. Multiple study results have demonstrated mortality benefits with β-blockers (metoprolol, carvedilol, bisoprolol) and high-intensity statins (rosuvastatin).[16] Patients presenting with cardiogenic shock or mitral valve rupture postmyocardial infarction may need the placement of a mechanical supportive device, such as an intraaortic balloon pump, after PCI. Symptomatic management includes morphine for pain control, oxygen for hypoxemia, and nitrates such as nitroglycerin for improvement of myocardial perfusion.(B3)
Differential Diagnosis
The differential diagnosis for myocardial infarction includes:
- Acute pericarditis
- Acute gastritis
- Peptic ulcer disease
- Aortic dissection
- Esophagitis
- Cardiac tamponade
- Costochondritis
- Myocarditis
- Pneumonia
- Pneumothorax
- Prinzmetal angina
- Pulmonary embolism
- Cocaine-induced vasospasm
A careful clinical evaluation and the judicious use of diagnostic examinations help determine the appropriate interventions.
Prognosis
LMI has generally favorable outcomes. Long-term outcomes in patients with STEMI and nonSTEMI have improved over the last decade.[17] Hreybe et al reported a marginally elevated risk of ventricular fibrillation in patients presenting with an anterior or lateral myocardial wall infarction.[18] The prognosis tends to be worse in patients presenting with life-threatening complications such as arrhythmias, sudden cardiac arrest, free wall or papillary muscle rupture, and cardiogenic shock. Risk stratification using the thrombolysis in myocardial infarction score can help identify patients with increased in-hospital mortality.[19] Thirty-day mortality rates for STEMI are 13% with medical therapy alone, 6% to 7% with optimal fibrinolytic therapy, and 3% to 5% with primary PCI when performed within 2 hours of hospital arrival. Patients with nonSTEMI have an even lower risk of death of only 2% after 30 days, as compared to individuals who have had a recent STEMI.
Complications
Complications of LMI are similar to those of other myocardial infarction types and include:
- Left ventricle dysfunction
- Arrhythmias
- Mitral regurgitation
- Pericarditis
- Ventricular aneurysm
- Left ventricular thrombus
- Dressler syndrome
Timely intervention and patient education can help minimize complications.
Deterrence and Patient Education
Patient education is the cornerstone of preventing future myocardial infarction events. Interventions such as smoking cessation, weight reduction, medication adherence, and dietary modification have all been well-established in improving overall cardiovascular mortality.[20] Targeting strict blood pressure, glycemic, and lipid goals can help decrease the risk of complications after myocardial infarction. Patients should be encouraged to participate in cardiac rehabilitation programs to improve overall cardiac function and achieve better heart rate control.
Enhancing Healthcare Team Outcomes
Healthcare team coordination plays an integral role in managing LMI, from emergency care and immediate interventions to long-term rehabilitation and prevention. The paramedics and emergency medical technicians provide initial care and rapid transport to the hospital. A cardiologist takes the lead in diagnosing and treating the LMI. An interventional cardiologist performs PCI.
Critical care and cardiac nurses or nurse practitioners monitor patients throughout their stay, administer medications, provide immediate treatment for acute complications, and educate patients and their families about lifestyle changes, medications, and long-term recovery after the acute event. Physical therapists arrange for cardiac rehabilitation, and nutritionists develop heart-healthy diets to manage patients' risk factors.
Effective communication and coordination between all team members ensure that patients receive comprehensive care that addresses both the acute and long-term consequences of myocardial infarction, ultimately improving outcomes and reducing the risk of recurrence. An interprofessional approach has been shown to improve healthcare outcomes in patients admitted with myocardial infarction.[21][22] Adherence to guideline-directed therapy is equally important. Establishing a cardiac alert response team for emergencies can help provide timely, dedicated care.
Media
(Click Image to Enlarge)
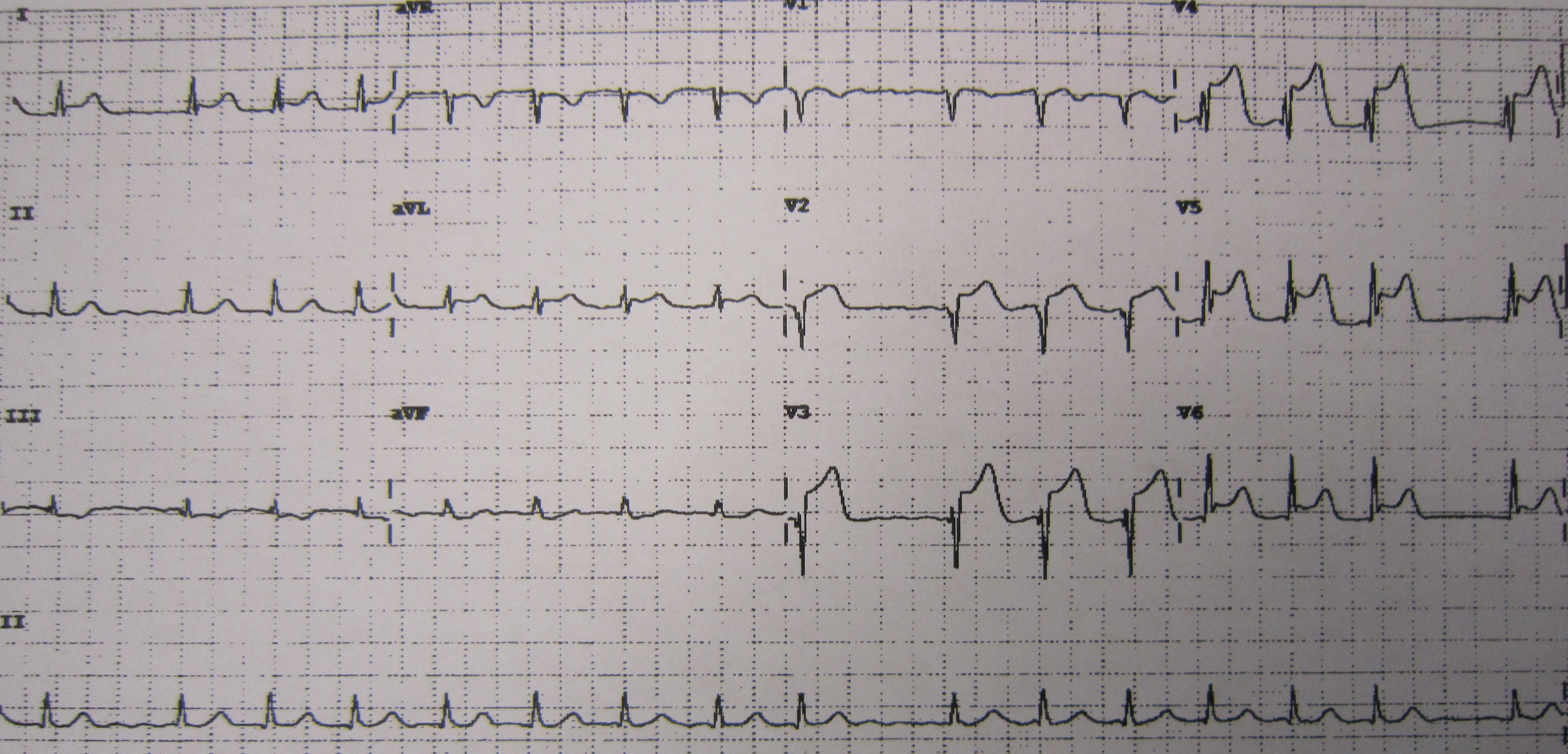
Anterolateral Myocardial Infarction on Electrocardiography. A 12-lead electrocardiogram shows anterolateral wall myocardial infarction with ST-elevation in leads V2 to V6, I, and aVL and reciprocal ST-depression in inferior leads.
Attribution: James Heilman, MD (https://creativecommons.org/licenses/by-sa/3.0/)
References
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, ESC Scientific Document Group. Fourth universal definition of myocardial infarction (2018). European heart journal. 2019 Jan 14:40(3):237-269. doi: 10.1093/eurheartj/ehy462. Epub [PubMed PMID: 30165617]
Roger VL, Weston SA, Gerber Y, Killian JM, Dunlay SM, Jaffe AS, Bell MR, Kors J, Yawn BP, Jacobsen SJ. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010 Feb 23:121(7):863-9. doi: 10.1161/CIRCULATIONAHA.109.897249. Epub 2010 Feb 8 [PubMed PMID: 20142444]
Newman JD, Shimbo D, Baggett C, Liu X, Crow R, Abraham JM, Loehr LR, Wruck LM, Folsom AR, Rosamond WD, ARIC Study Investigators. Trends in myocardial infarction rates and case fatality by anatomical location in four United States communities, 1987 to 2008 (from the Atherosclerosis Risk in Communities Study). The American journal of cardiology. 2013 Dec 1:112(11):1714-9. doi: 10.1016/j.amjcard.2013.07.037. Epub 2013 Sep 21 [PubMed PMID: 24063834]
Level 2 (mid-level) evidenceTibaut M, Mekis D, Petrovic D. Pathophysiology of Myocardial Infarction and Acute Management Strategies. Cardiovascular & hematological agents in medicinal chemistry. 2017:14(3):150-159. doi: 10.2174/1871525714666161216100553. Epub [PubMed PMID: 27993119]
Libby P. Pathogenesis of Atherothrombotic Events: From Lumen to Lesion and Beyond. Circulation. 2024 Oct 15:150(16):1217-1219. doi: 10.1161/CIRCULATIONAHA.124.070087. Epub 2024 Oct 14 [PubMed PMID: 39401281]
Esmat S, Abdel-Halim MR, Fawzy MM, Nassef S, Esmat S, Ramzy T, El Fouly ES. Are normolipidaemic patients with xanthelasma prone to atherosclerosis? Clinical and experimental dermatology. 2015 Jun:40(4):373-8. doi: 10.1111/ced.12594. Epub 2015 Feb 16 [PubMed PMID: 25683563]
Level 2 (mid-level) evidenceKaier TE, Alaour B, Marber M. Cardiac troponin and defining myocardial infarction. Cardiovascular research. 2021 Aug 29:117(10):2203-2215. doi: 10.1093/cvr/cvaa331. Epub [PubMed PMID: 33458742]
Bose A, Jain V, Kawthekar G, Chhabra C, Hemvani N, Chitnis DS. The Importance of Serial Time Point Quantitative Assessment of Cardiac Troponin I in the Diagnosis of Acute Myocardial Damage. Indian journal of critical care medicine : peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2018 Sep:22(9):629-631. doi: 10.4103/ijccm.IJCCM_8_16. Epub [PubMed PMID: 30294127]
Sabia P, Afrookteh A, Touchstone DA, Keller MW, Esquivel L, Kaul S. Value of regional wall motion abnormality in the emergency room diagnosis of acute myocardial infarction. A prospective study using two-dimensional echocardiography. Circulation. 1991 Sep:84(3 Suppl):I85-92 [PubMed PMID: 1884510]
Taggart C, Wereski R, Mills NL, Chapman AR. Diagnosis, Investigation and Management of Patients with Acute and Chronic Myocardial Injury. Journal of clinical medicine. 2021 May 26:10(11):. doi: 10.3390/jcm10112331. Epub 2021 May 26 [PubMed PMID: 34073539]
Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, Douglas PS, Foody JM, Gerber TC, Hinderliter AL, King SB 3rd, Kligfield PD, Krumholz HM, Kwong RY, Lim MJ, Linderbaum JA, Mack MJ, Munger MA, Prager RL, Sabik JF, Shaw LJ, Sikkema JD, Smith CR Jr, Smith SC Jr, Spertus JA, Williams SV, American College of Cardiology Foundation. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012 Dec 18:126(25):3097-137. doi: 10.1161/CIR.0b013e3182776f83. Epub 2012 Nov 19 [PubMed PMID: 23166210]
Level 1 (high-level) evidenceKunkel KJ, Lemor A, Mahmood S, Villablanca P, Ramakrishna H. 2021 Update for the Diagnosis and Management of Acute Coronary Syndromes for the Perioperative Clinician. Journal of cardiothoracic and vascular anesthesia. 2022 Aug:36(8 Pt A):2767-2779. doi: 10.1053/j.jvca.2021.07.032. Epub 2021 Jul 22 [PubMed PMID: 34400062]
Anderson JL, Karagounis LA, Califf RM. Metaanalysis of five reported studies on the relation of early coronary patency grades with mortality and outcomes after acute myocardial infarction. The American journal of cardiology. 1996 Jul 1:78(1):1-8 [PubMed PMID: 8712096]
Level 1 (high-level) evidenceThrane PG, Kristensen SD, Olesen KKW, Mortensen LS, Bøtker HE, Thuesen L, Hansen HS, Abildgaard U, Engstrøm T, Andersen HR, Maeng M. 16-year follow-up of the Danish Acute Myocardial Infarction 2 (DANAMI-2) trial: primary percutaneous coronary intervention vs. fibrinolysis in ST-segment elevation myocardial infarction. European heart journal. 2020 Feb 14:41(7):847-854. doi: 10.1093/eurheartj/ehz595. Epub [PubMed PMID: 31504424]
O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW, American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Jan 29:127(4):e362-425. doi: 10.1161/CIR.0b013e3182742cf6. Epub 2012 Dec 17 [PubMed PMID: 23247304]
Level 3 (low-level) evidenceO'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso JE, Tracy CM, Woo YJ, Zhao DX, CF/AHA Task Force. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Jan 29:127(4):529-55. doi: 10.1161/CIR.0b013e3182742c84. Epub 2012 Dec 17 [PubMed PMID: 23247303]
Level 3 (low-level) evidenceMcManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. The American journal of medicine. 2011 Jan:124(1):40-7. doi: 10.1016/j.amjmed.2010.07.023. Epub [PubMed PMID: 21187184]
Hreybe H, Saba S. Location of acute myocardial infarction and associated arrhythmias and outcome. Clinical cardiology. 2009 May:32(5):274-7. doi: 10.1002/clc.20357. Epub [PubMed PMID: 19452487]
Morrow DA, Antman EM, Parsons L, de Lemos JA, Cannon CP, Giugliano RP, McCabe CH, Barron HV, Braunwald E. Application of the TIMI risk score for ST-elevation MI in the National Registry of Myocardial Infarction 3. JAMA. 2001 Sep 19:286(11):1356-9 [PubMed PMID: 11560541]
Saito Y, Oyama K, Tsujita K, Yasuda S, Kobayashi Y. Treatment strategies of acute myocardial infarction: updates on revascularization, pharmacological therapy, and beyond. Journal of cardiology. 2023 Feb:81(2):168-178. doi: 10.1016/j.jjcc.2022.07.003. Epub 2022 Jul 23 [PubMed PMID: 35882613]
Fanari Z, Barekatain A, Kerzner R, Hammami S, Weintraub WS, Maheshwari V. Impact of a Multidisciplinary Team Approach Including an Intensivist on the Outcomes of Critically Ill Patients in the Cardiac Care Unit. Mayo Clinic proceedings. 2016 Dec:91(12):1727-1734. doi: 10.1016/j.mayocp.2016.08.004. Epub 2016 Oct 27 [PubMed PMID: 28126152]
Batchelor WB, Anwaruddin S, Wang DD, Perpetua EM, Krishnaswami A, Velagapudi P, Wyman JF, Fullerton D, Keegan P, Phillips A, Ross L, Maini B, Bernacki G, Panjrath GS, Lee J, Geske JB, Welt F, Thakker PD, Deswal A, Park K, Mack MJ, Leon M, Lewis S, Holmes D. The Multidisciplinary Heart Team in Cardiovascular Medicine: Current Role and Future Challenges. JACC. Advances. 2023 Jan:2(1):100160. doi: 10.1016/j.jacadv.2022.100160. Epub 2023 Jan 11 [PubMed PMID: 38939019]
Level 3 (low-level) evidence