Introduction
Acute myocardial infarction (AMI) is one of the leading causes of death in the developed world. The prevalence of the disease approaches 3 million people worldwide, with more than 1 million deaths in the United States annually. AMI can be divided into 2 categories: non–ST-segment elevation myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI). Unstable angina resembles an NSTEMI, but normal cardiac markers distinguish it.[1][2][3]
Myocardial infarction (MI) causes permanent damage to the heart muscle due to inadequate oxygen supply. MI can impair diastolic and systolic function, increasing the risk of arrhythmias. Additionally, an MI can lead to various serious complications. Prompt reperfusion and restoration of blood flow to the heart are crucial. Early treatment within 6 hours of symptom onset significantly improves prognosis.
An MI is diagnosed when 2 of the following criteria are met:
- Symptoms of ischemia
- New ST-segment changes or a left bundle branch block (LBBB)
- Presence of pathological Q waves on electrocardiogram (ECG)
- New regional wall motion abnormality on imaging study
- Presence of an intracoronary thrombus at autopsy or angiography
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Acute myocardial infarction occurs due to decreased coronary blood flow, leading to insufficient oxygen supply to the heart and cardiac ischemia. Decreased coronary blood flow is multifactorial. Atherosclerotic plaques classically rupture and lead to thrombosis, contributing to acutely decreased blood flow in the coronary. Other etiologies of myocardial ischemia include coronary artery embolism, which accounts for 2.9% of patients, cocaine-induced ischemia, coronary dissection, and coronary vasospasm.[4][5]
Nonmodifiable Risk Factors
- Sex
- Age
- Family history
- Male pattern baldness
Modifiable Risk Factors
- Smoking
- Dyslipidemia
- Diabetes mellitus
- Hypertension
- Obesity
- Sedentary lifestyle
- Poor oral hygiene
- Presence of peripheral vascular disease
- Elevated levels of homocysteine
Other Causes of MI
- Trauma
- Vasculitis
- Drug use (cocaine)
- Coronary artery anomalies
- Coronary artery emboli
- Aortic dissection
- Excess demand on the heart (hyperthyroidism, anemia)
Epidemiology
Approximately 70% of fatal AMI cases are attributed to occlusion caused by atherosclerotic plaques. As atherosclerosis is the predominant cause of AMI, risk-factors for atherosclerotic disease are often mitigated in disease prevention. Modifiable risk factors account for 90% of AMI cases in men and 94% in women. These modifiable risk factors include cigarette smoking, physical inactivity, hypertension, obesity, elevated cholesterol levels (particularly LDL), and high triglyceride levels. In contrast, age, sex, and family history are nonmodifiable risk factors for atherosclerosis and AMI.[6][7]
Pathophysiology
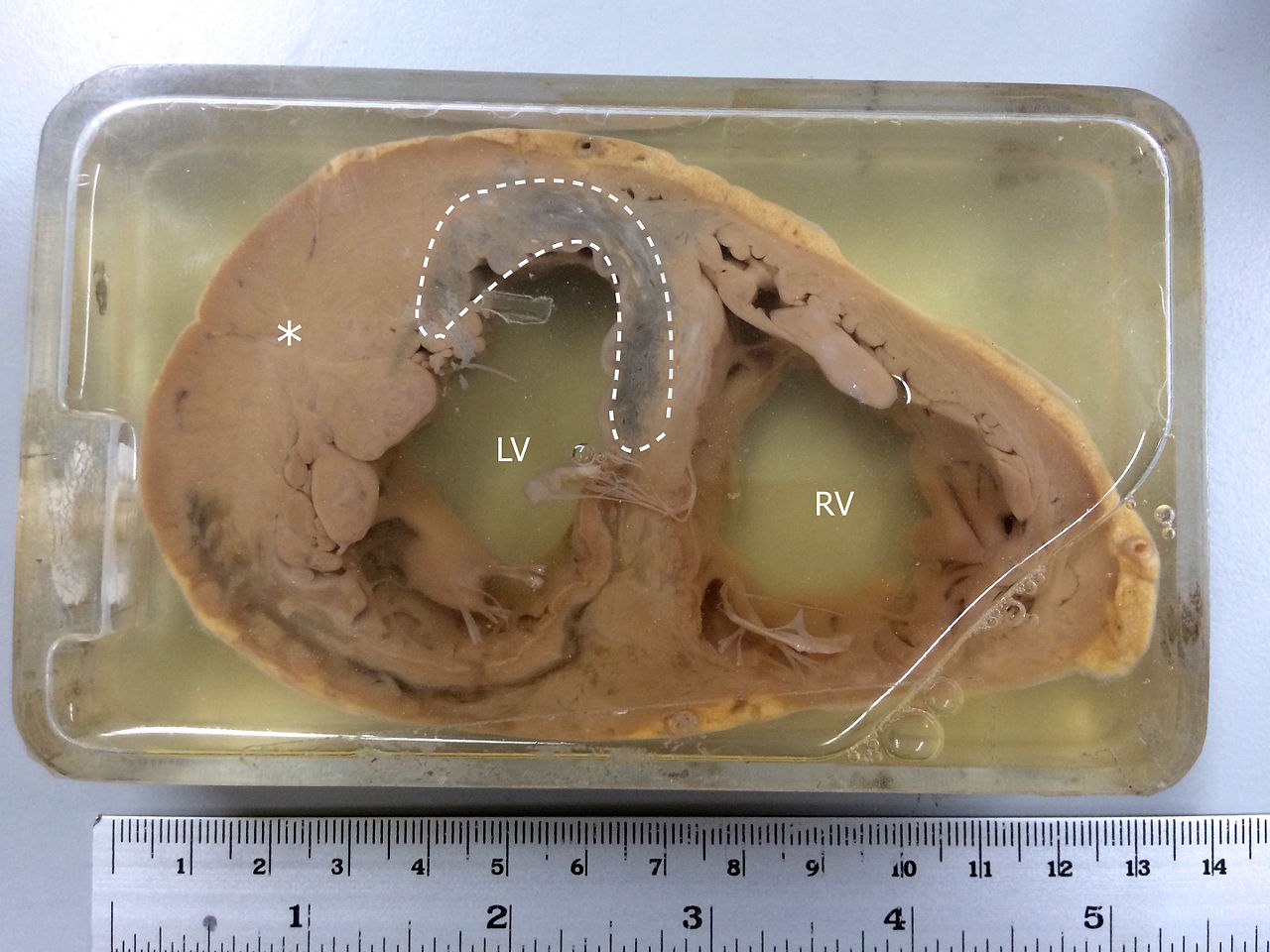
The rupture of an atherosclerotic plaque initiates an inflammatory response of monocytes and macrophages, leading to thrombus formation and platelet aggregation. This process decreases oxygen delivery through the coronary artery, resulting in inadequate oxygenation of the myocardium (see Image. Specimen Showing MI). The subsequent inability to produce ATP in the mitochondria triggers an ischemic cascade, ultimately leading to apoptosis (cell death) of the endocardium or myocardial infarction.
With some exceptions due to genetic variation, coronary arteries exhibit unique and diagnostic territorial distributions. For example, the left anterior descending coronary artery supplies blood flow to the interventricular septum, anterolateral wall, and ventricular apex. The left circumflex artery supplies blood to the inferolateral wall. The right coronary artery supplies the right ventricle. The inferior wall is supplied either by the left circumflex or right coronary artery.[8]
Histopathology
The histological changes observed in MI evolve throughout the disease course. At time 0, no microscopic histologic changes are observed. Within 0.5 to 4 hours, light microscopy reveals the waviness of fibers at the tissue periphery along with glycogen depletion. At 4 to 12 hours, the myocardium undergoes coagulation necrosis and edema. At 12 to 24 hours, the gross specimen appears dark and mottled, with contraction band necrosis and neutrophil predominance observed on histopathology.
Subsequently, nuclei reduction occurs between 1 to 3 days, and then, within the next 3 to 7 days, macrophages emerge to clear apoptotic cells. Granulation tissue appears at 7 to 10 days, and collagen type I deposition occurs after 10 days. Ultimately, after 2 months, the myocardium undergoes scarring.
History and Physical
The history and physical examination alone may not always diagnose AMI definitively. The history should focus on the onset, quality, and associated symptoms. Recent studies suggest that diaphoresis and bilateral arm radiating pain are more commonly associated with MI in men. Other associated symptoms may include the following:
- Lightheadedness
- Anxiety
- Cough
- Choking sensation
- Diaphoresis
- Wheezing
- Irregular heart rate
The physical examination should include the patient’s vital signs and appearance, including diaphoresis, pulmonary evaluation, and cardiac auscultation. Specific vital aspects of the examination are as follows:
-
Heart rate: Tachycardia, atrial fibrillation, or ventricular arrhythmia may be present, indicating cardiac electrical disturbances.
-
Pulses: Unequal pulses may be observed if the patient has an aortic dissection, indicating a potential arterial problem.
-
Blood pressure: Blood pressure is typically high in AMI but may become hypotensive if the patient is in shock due to compromised cardiac function.
-
Respiratory findings: Tachypnea and fever may be present, indicating an inflammatory response.
-
Neck veins: Distended neck veins may be observed, suggesting right ventricular failure and increased central venous pressure.
-
Cardiac findings: The heart may exhibit lateral displacement of the apical impulse, a soft S1 sound, a palpable S4 sound, and a new mitral regurgitation murmur. A loud holosystolic murmur radiating to the sternum may indicate ventricular septal rupture.
-
Pulmonary findings: Wheezing and rales may be heard if the patient has developed pulmonary edema, indicating fluid accumulation in the lungs.
-
Extremities: Edema or cyanosis may be present in the extremities, with a sensation of coldness due to compromised circulation.
Evaluation
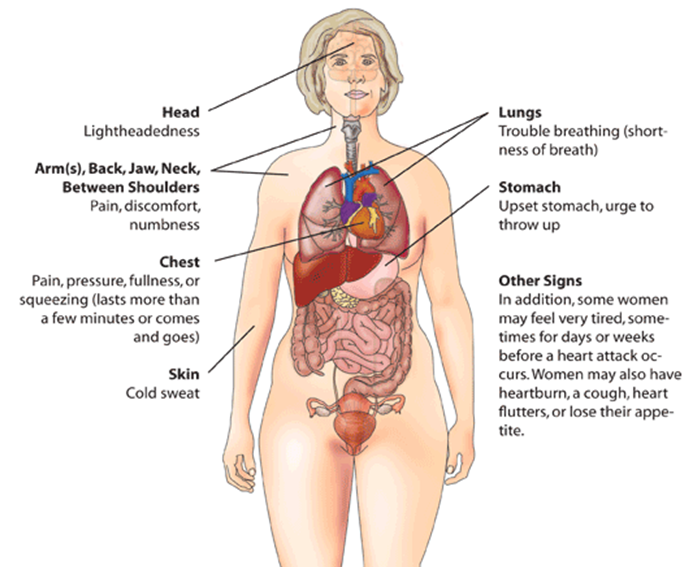
Early and prompt ECG testing should be employed in all patients presenting with chest pain. Women may experience atypical symptoms such as abdominal pain or dizziness and may present without chest pain (see Image. Myocardial Infarction Warning Signs in Women). Older patients often present with shortness of breath rather than chest pain in cases of MI. All of the aforementioned presentations should prompt ECG testing.[9][10][11]
The ECG is a highly specific diagnostic tool for MI, with a specificity of 95% to 97%. However, its sensitivity is relatively low, at approximately 30%. Right-sided, posterior lead placement and repeat ECG testing can increase ECG sensitivity. For example, peaked T-waves on ECG, known as "hyperacute T waves," often indicate early ischemia and will progress to ST elevation. When present, ST-elevation findings greater than 2 mm in 2 contiguous leads on ECG (inferior: leads II, III, aVF; septal: equal V1, V2; anterior: V3, V4; lateral: I, aVL, V5, V6) are indicative of a STEMI (see Image. ECG With Pardee Waves Indicating AMI). Often, ST depressions are visualized in opposite anatomical regions of the myocardium.
Diagnosing STEMI using the ECG can be challenging, particularly in patients with a left bundle branch block and pacemakers. However, specific criteria have been identified to aid in the diagnosis. Sgarbossa criteria suggest isolated ST elevations in lead aVR can indicate left main coronary artery occlusion in the appropriate clinical setting. Wellens criteria noted deeply biphasic T waves in leads V2 and V3, often predictive of an impending proximal left anterior descending artery occlusion, potentially leading to devastating anterior wall myocardial infarction.
Patients presenting with symptoms of MI may not exhibit diagnostic ST-elevation ECG abnormalities. In cases in which patients have typical chest pain but no obvious ST elevation, further investigation for NSTEMI is warranted. Subtle abnormalities on ECG, such as ST depressions and T-wave changes, may be present. Serial ECGs can be helpful in looking for dynamic changes. ECG findings without acute changes or any abnormalities are common in NSTEMI.
Diagnostic guidelines can aid practitioners in determining whether additional testing helps identify patients with NSTEMI. Considering the limited sensitivity of ECG in STEMI detection, troponin levels have become an almost universally employed diagnostic tool for patients with a clinical history suggestive of MI. The HEART score has been validated and popularized. The HEART score incorporates the clinician's suspicion, patient risk factors, ECG findings, and troponin levels to assess the patient's risk level.
Laboratory Studies
A cardiac troponin test should be the only cardiac marker test ordered. CDC, lipid profile, renal function, and metabolic panel are relevant labs.
Cardiac biomarkers are helpful in the diagnosis of AMI, particularly NSTEMI. Troponin, creatine kinase-MB (CK-MB), and LDH are cardiac markers observed.
A troponin test is the most specific lab test for early detection of AMI; levels of the troponin isoforms I and T are measured. Troponin levels peak at 12 hours and remain elevated for 7 days. High-sensitivity troponin has been approved for use in the United States after being heavily studied and utilized in Europe. Although it is more sensitive than conventional troponin, it is also less specific. Thus, potential challenges include numerous false-positive interpretations.[3]
The level of CK-MB, an isoenzyme of creatine kinase usually found in the myocardium, reaches its peak at 10 hours and normalizes within 2 to 3 days. CK-MB is also not clinically utilized due to its low specificity, rapid rise, and normalization.
LDH levels reach their peak after 72 hours and return to normal within 10 to 14 days. In clinical practice, LDH is not used to diagnose acute MI.
B-type natriuretic peptide (BNP) should not be ordered as a marker for MI; instead, it is more valuable for risk stratification, particularly in patients with MI who subsequently develop heart failure.
Cardiac Imaging
Cardiac angiography is used to perform the percutaneous coronary intervention (PCI) procedure or determine obstructions in the coronary vessels.
An echocardiogram is used to assess wall motion, degree of valve abnormality, ischemic mitral regurgitation, and presence of cardiac tamponade.
Treatment / Management
All patients with STEMI and NSTEMI require immediate administration of nonenteric-coated, chewable aspirin with a loading dose of 162 mg to 325 mg.[12] Additionally, patients should have intravenous access established, and oxygen supplementation should be administered if their oxygen saturation falls below 91%. Opioids may be used for pain control in addition to sublingual nitroglycerin if the patient's blood pressure is within an acceptable range.[13][14][15](B2)
The primary treatment approach for STEMI involves immediate reperfusion. The preferred method is emergent PCI. Before PCI, patients should receive dual antiplatelet therapy, which includes intravenous heparin infusion and an adenosine diphosphate inhibitor receptor (P2Y12 inhibitor), most commonly ticagrelor. A glycoprotein IIb/IIIa inhibitor or direct thrombin inhibitor may also be administered during the PCI procedure. If PCI is unavailable within 90 minutes of diagnosing STEMI, reperfusion using an intravenous thrombolytic agent should be attempted.
In stable asymptomatic patients with NSTEMI, the initial management approach is typically medical, focusing on using antiplatelet agents and other appropriate medications. However, PCI can be performed within 48 hours of admission if necessary. This delayed PCI strategy has been shown to potentially improve in-hospital mortality and decrease the length of hospital stay for NSTEMI patients.
In NSTEMI patients who experience refractory ischemia or ischemia with hemodynamic or electrical instability, PCI should be performed emergently.
Before discharge for acute MI, patients may routinely be prescribed aspirin, a high-dose statin, a beta-blocker, and possibly an ACE inhibitor.
If PCI is considered the treatment option for an acute MI, it is recommended to perform the procedure within 12 hours of symptom onset. If fibrinolytic therapy is considered the primary reperfusion strategy, it should be initiated within 120 minutes. In addition to reperfusion strategies, parenteral anticoagulation is recommended for all patients with acute MI, regardless of whether they undergo PCI or receive fibrinolytic therapy.
Differential Diagnosis
Differential diagnoses for AMI include the following:
- Aortic dissection: This is a life-threatening condition with a tear in the inner layer of the aorta, leading to the separation of the layers and potential obstruction of blood flow.
- Pericarditis: Inflammation of the pericardium can cause chest pain that may resemble an AMI.
- Acute gastritis: Inflammation of the stomach lining can cause upper abdominal pain that may be mistaken for cardiac-related chest pain.
- Acute cholecystitis: Inflammation of the gallbladder can cause right upper-quadrant abdominal pain that can radiate to the chest and mimic cardiac symptoms.
- Asthma: Acute asthma exacerbation can lead to shortness of breath, wheezing, and chest tightness, which may be mistaken for cardiac symptoms.
- Esophagitis: Inflammation of the esophagus can cause chest pain, mainly if it is related to gastroesophageal reflux disease (GERD) or other esophageal disorders.
- Myocarditis: Heart muscle inflammation can present with chest pain and other symptoms similar to AMI.
- Pneumothorax: A collapsed lung can cause sudden chest pain and difficulty breathing, mimicking cardiac-related symptoms.
- Pulmonary embolism: Blockage of a pulmonary artery by a blood clot can lead to chest pain, shortness of breath, and other symptoms that may resemble an AMI.
Prognosis
AMI carries a significant risk of mortality outside of the hospital environment. Data indicate that at least one-third of patients succumb to the condition before reaching the hospital, and an additional 40% to 50% do not survive upon arrival. Furthermore, another 5% to 10% of patients will experience mortality within the first 12 months after an MI.
The prognosis of AMI depends on the extent of muscle damage. Better outcomes are seen in patients who undergo early perfusion, including thrombolytic therapy within 30 minutes of arrival or PCI within 90 minutes. Patients with preserved ejection fraction have better outcomes than those with reduced ejection fraction.
Medical management following an AMI is crucial for improving long-term outcomes. Initiating medications, such as aspirin, beta-blockers, and ACE inhibitors, is standard practice to help prevent recurrent cardiovascular events.
Factors that negatively affect prognosis include the following:
- Diabetes
- Advanced age
- Prior MI, peripheral vascular disease, or stroke
- Delayed reperfusion
- Diminished ejection fraction (the strongest predictor)
- Presence of congestive heart failure
- Elevated C-reactive protein and BNP levels
- Depression
A high readmission rate affects about 50% of patients within the first 12 months after the initial MI. The overall prognosis depends on factors such as the ejection fraction, age, and comorbidities. Patients who do not undergo revascularization procedures have poorer outcomes than those who undergo revascularization. The most favorable prognosis is observed in patients with early and successful reperfusion and preserved left ventricular function.[16][17][18]
Complications
Primary complications of AMI include the following:
- New-onset mitral regurgitation
- Ventricular septal rupture
- Left ventricular aneurysm
- Arrhythmias
- Emboli
Postoperative and Rehabilitation Care
Cardiac rehabilitation plays a vital role in the recovery of patients following an AMI. Research has demonstrated the numerous benefits of cardiac rehabilitation, including improvements in quality of life, reduction of disability, and a decrease in mortality rates.[19][20]
The rehabilitation process should be individualized to meet each patient's specific needs, available resources, established goals, and physical abilities before and after the MI event. Collaboration among rehabilitation therapists and the rest of the interprofessional care team is vital for continuity of care.[19][21]
Cardiac rehabilitation has also been shown to reduce future risk factors for individuals following an AMI. Annual follow-up results demonstrate that cardiac rehab can reduce the risk of future cardiovascular events.[22]
Deterrence and Patient Education
For individuals experiencing symptoms of a possible AMI, the following actions are recommended:
-
Seek immediate medical attention if symptoms suggest an MI, such as chest pain or discomfort, shortness of breath, nausea, or lightheadedness. Go to the emergency department as soon as possible.
- Contact emergency services if nitroglycerin does not provide relief.
- Adhere to a low-salt diet to help manage high blood pressure and reduce the heart's workload.
- Enroll in cardiac rehabilitation designed to support individuals recovering from cardiac conditions, including AMI.
- Cease smoking, as it is a major risk factor for cardiovascular disease.
- Remain compliant with medication administration.
Enhancing Healthcare Team Outcomes
An interprofessional team specializing in heart disease manages AMI. In addition to the cardiologist, the team usually consists of a cardiac surgeon, an interventional cardiologist, an intensivist, a cardiac rehabilitation specialist, critical care or cardiology nurses, and physical therapists. Because AMI is potentially life-threatening, it is crucial to prioritize patient education regarding recognizing symptoms and the importance of seeking immediate medical attention. The pharmacist, nurse practitioner, and primary care providers should educate patients regarding nitroglycerin administration, emphasizing when to seek immediate medical attention if the medication does not provide relief.
Time to reperfusion is limited, and early initiation of treatment can significantly improve outcomes. The care team's initial assessment needs to be timely and cardiology consulted immediately. The cardiologist evaluates the patient's condition, considering the duration of symptoms and contraindications, to determine the appropriate treatment approach. This may involve thrombolysis or PCI to restore blood flow to the blocked coronary artery.
Patients with AMI require close monitoring and specialized care in the ICU. ICU nurses are crucial in monitoring vital signs, administering medications, assessing for complications, and promptly communicating abnormal clinical signs or laboratory parameters to the interprofessional team.
Avoiding premature discharge is crucial because complications of an MI can manifest up to a week after the initial event. The interprofessional team should collaborate to ensure patients are stabilized, monitored appropriately, and educated on signs and symptoms that may indicate worsening or recurrent MI.
Nurses play a vital role in educating patients about reducing risk factors for coronary artery disease. This education includes lifestyle modifications, medication adherence, and ongoing monitoring of blood pressure, cholesterol levels, and blood sugar control.
The involvement of a social worker or case manager is beneficial in facilitating home care arrangements, coordinating cardiac rehabilitation programs, and addressing the need for any support services patients may require at home.
Pharmacists play a crucial role in addressing medication-related aspects of patient care. They provide education on appropriate medication dosing, potential adverse effects, drug interactions, and medication adherence to optimize treatment outcomes.
Following discharge, the patient must participate in a cardiac rehabilitation program, adopt a healthy diet, cease smoking, abstain from alcohol consumption, achieve weight reduction (if appropriate), and manage cholesterol and blood glucose levels. The patient should be educated on the importance of medication compliance to lower blood pressure and cholesterol.[23][24][25] Pharmacists review prescribed medications, check for interactions, and provide patient education about the importance of compliance.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)

ECG With Pardee Waves Indicating AMI. Pardee waves indicate acute myocardial infarction in the inferior leads II, III, and aVF with reciprocal changes in the anterolateral leads.
Glenlarson, Public Domain, via Wikimedia Commons
(Click Video to Play)
Transesophageal Echocardiography, Pulmonary Embolism. Acute ECG segment elevation mimicking myocardial infarction in a patient with pulmonary embolism.
T Goslar, M Podbregar, Public Domain, via Wikimedia Commons
References
Nascimento BR, Brant LCC, Marino BCA, Passaglia LG, Ribeiro ALP. Implementing myocardial infarction systems of care in low/middle-income countries. Heart (British Cardiac Society). 2019 Jan:105(1):20-26. doi: 10.1136/heartjnl-2018-313398. Epub 2018 Sep 29 [PubMed PMID: 30269080]
Barberi C, van den Hondel KE. The use of cardiac troponin T (cTnT) in the postmortem diagnosis of acute myocardial infarction and sudden cardiac death: A systematic review. Forensic science international. 2018 Nov:292():27-38. doi: 10.1016/j.forsciint.2018.09.002. Epub 2018 Sep 17 [PubMed PMID: 30269044]
Level 1 (high-level) evidenceAlaour B, Liew F, Kaier TE. Cardiac Troponin - diagnostic problems and impact on cardiovascular disease. Annals of medicine. 2018 Dec:50(8):655-665. doi: 10.1080/07853890.2018.1530450. Epub 2018 Nov 21 [PubMed PMID: 30265127]
Massberg S, Polzin A. [Update ESC-Guideline 2017: Dual Antiplatelet Therapy]. Deutsche medizinische Wochenschrift (1946). 2018 Aug:143(15):1090-1093. doi: 10.1055/a-0549-8230. Epub 2018 Jul 30 [PubMed PMID: 30060279]
Scheen AJ. [From atherosclerosis to atherothrombosis : from a silent chronic pathology to an acute critical event]. Revue medicale de Liege. 2018 May:73(5-6):224-228 [PubMed PMID: 29926559]
Berg DD, Wiviott SD, Braunwald E, Guo J, Im K, Kashani A, Gibson CM, Cannon CP, Morrow DA, Bhatt DL, Mega JL, O'Donoghue ML, Antman EM, Newby LK, Sabatine MS, Giugliano RP. Modes and timing of death in 66 252 patients with non-ST-segment elevation acute coronary syndromes enrolled in 14 TIMI trials. European heart journal. 2018 Nov 7:39(42):3810-3820. doi: 10.1093/eurheartj/ehy556. Epub [PubMed PMID: 30239711]
Deng D, Liu L, Xu G, Gan J, Shen Y, Shi Y, Zhu R, Lin Y. Epidemiology and Serum Metabolic Characteristics of Acute Myocardial Infarction Patients in Chest Pain Centers. Iranian journal of public health. 2018 Jul:47(7):1017-1029 [PubMed PMID: 30182001]
Haig C, Carrick D, Carberry J, Mangion K, Maznyczka A, Wetherall K, McEntegart M, Petrie MC, Eteiba H, Lindsay M, Hood S, Watkins S, Davie A, Mahrous A, Mordi I, Ahmed N, Teng Yue May V, Ford I, Radjenovic A, Welsh P, Sattar N, Oldroyd KG, Berry C. Current Smoking and Prognosis After Acute ST-Segment Elevation Myocardial Infarction: New Pathophysiological Insights. JACC. Cardiovascular imaging. 2019 Jun:12(6):993-1003. doi: 10.1016/j.jcmg.2018.05.022. Epub 2018 Jul 18 [PubMed PMID: 30031700]
Alquézar-Arbé A, Sanchís J, Guillén E, Bardají A, Miró Ò, Ordóñez-Llanos J. Cardiac troponin measurement and interpretation in the diagnosis of acute myocardial infarction in the emergency department: a consensus statement. Emergencias : revista de la Sociedad Espanola de Medicina de Emergencias. 2018 Oct:30(5):336-349 [PubMed PMID: 30260119]
Level 3 (low-level) evidencePerera M, Aggarwal L, Scott IA, Logan B. Received care compared to ADP-guided care of patients admitted to hospital with chest pain of possible cardiac origin. International journal of general medicine. 2018:11():345-351. doi: 10.2147/IJGM.S166570. Epub 2018 Sep 3 [PubMed PMID: 30214268]
Riley RF, Miller CD, Russell GB, Soliman EZ, Hiestand BC, Herrington DM, Mahler SA. Usefulness of Serial 12-Lead Electrocardiograms in Predicting 30-Day Outcomes in Patients With Undifferentiated Chest Pain (the ASAP CATH Study). The American journal of cardiology. 2018 Aug 1:122(3):374-380. doi: 10.1016/j.amjcard.2018.04.031. Epub 2018 May 1 [PubMed PMID: 30196932]
Jneid H, Addison D, Bhatt DL, Fonarow GC, Gokak S, Grady KL, Green LA, Heidenreich PA, Ho PM, Jurgens CY, King ML, Kumbhani DJ, Pancholy S. 2017 AHA/ACC Clinical Performance and Quality Measures for Adults With ST-Elevation and Non-ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Journal of the American College of Cardiology. 2017 Oct 17:70(16):2048-2090. doi: 10.1016/j.jacc.2017.06.032. Epub 2017 Sep 21 [PubMed PMID: 28943066]
Level 2 (mid-level) evidenceLarson EA, German DM, Shatzel J, DeLoughery TG. Anticoagulation in the cardiac patient: A concise review. European journal of haematology. 2019 Jan:102(1):3-19. doi: 10.1111/ejh.13171. Epub 2018 Nov 14 [PubMed PMID: 30203452]
Bath PM, Woodhouse LJ, Appleton JP, Beridze M, Christensen H, Dineen RA, Flaherty K, Duley L, England TJ, Havard D, Heptinstall S, James M, Kasonde C, Krishnan K, Markus HS, Montgomery AA, Pocock S, Randall M, Ranta A, Robinson TG, Scutt P, Venables GS, Sprigg N. Triple versus guideline antiplatelet therapy to prevent recurrence after acute ischaemic stroke or transient ischaemic attack: the TARDIS RCT. Health technology assessment (Winchester, England). 2018 Aug:22(48):1-76. doi: 10.3310/hta22480. Epub [PubMed PMID: 30179153]
Adamski P, Adamska U, Ostrowska M, Navarese EP, Kubica J. Evaluating current and emerging antithrombotic therapy currently available for the treatment of acute coronary syndrome in geriatric populations. Expert opinion on pharmacotherapy. 2018 Sep:19(13):1415-1425. doi: 10.1080/14656566.2018.1510487. Epub 2018 Aug 22 [PubMed PMID: 30132731]
Level 3 (low-level) evidenceStone GW, Ellis SG, Gori T, Metzger DC, Stein B, Erickson M, Torzewski J, Williams J Jr, Lawson W, Broderick TM, Kabour A, Piegari G, Cavendish J, Bertolet B, Choi JW, Marx SO, Généreux P, Kereiakes DJ, ABSORB IV Investigators. Blinded outcomes and angina assessment of coronary bioresorbable scaffolds: 30-day and 1-year results from the ABSORB IV randomised trial. Lancet (London, England). 2018 Oct 27:392(10157):1530-1540. doi: 10.1016/S0140-6736(18)32283-9. Epub 2018 Sep 25 [PubMed PMID: 30266412]
Level 1 (high-level) evidenceLopes RD, de Barros E Silva PGM, de Andrade Jesuíno I, Santucci EV, Barbosa LM, Damiani LP, Nakagawa Santos RH, Laranjeira LN, Dall Orto FTC, Beraldo de Andrade P, de Castro Bienert IR, Alexander JH, Granger CB, Berwanger O. Timing of Loading Dose of Atorvastatin in Patients Undergoing Percutaneous Coronary Intervention for Acute Coronary Syndromes: Insights From the SECURE-PCI Randomized Clinical Trial. JAMA cardiology. 2018 Nov 1:3(11):1113-1118. doi: 10.1001/jamacardio.2018.3408. Epub [PubMed PMID: 30264159]
Level 1 (high-level) evidenceChoi AR, Jeong MH, Hong YJ, Sohn SJ, Kook HY, Sim DS, Ahn YK, Lee KH, Cho JY, Kim YJ, Cho MC, Kim CJ, other Korea Acute Myocardial Infarction Registry Investigators. Clinical characteristics and outcomes in acute myocardial infarction patients with versus without any cardiovascular risk factors. The Korean journal of internal medicine. 2019 Sep:34(5):1040-1049. doi: 10.3904/kjim.2018.056. Epub 2018 Sep 1 [PubMed PMID: 30257551]
Piotrowicz R, Wolszakiewicz J. Cardiac rehabilitation following myocardial infarction. Cardiology journal. 2008:15(5):481-7 [PubMed PMID: 18810728]
Ruano-Ravina A, Pena-Gil C, Abu-Assi E, Raposeiras S, van 't Hof A, Meindersma E, Bossano Prescott EI, González-Juanatey JR. Participation and adherence to cardiac rehabilitation programs. A systematic review. International journal of cardiology. 2016 Nov 15:223():436-443. doi: 10.1016/j.ijcard.2016.08.120. Epub 2016 Aug 13 [PubMed PMID: 27557484]
Contractor AS. Cardiac rehabilitation after myocardial infarction. The Journal of the Association of Physicians of India. 2011 Dec:59 Suppl():51-5 [PubMed PMID: 22624283]
Sjölin I, Bäck M, Nilsson L, Schiopu A, Leosdottir M. Association between attending exercise-based cardiac rehabilitation and cardiovascular risk factors at one-year post myocardial infarction. PloS one. 2020:15(5):e0232772. doi: 10.1371/journal.pone.0232772. Epub 2020 May 11 [PubMed PMID: 32392231]
Aeyels D, Seys D, Sinnaeve PR, Claeys MJ, Gevaert S, Schoors D, Sermeus W, Panella M, Bruyneel L, Vanhaecht K. Managing in-hospital quality improvement: An importance-performance analysis to set priorities for ST-elevation myocardial infarction care. European journal of cardiovascular nursing. 2018 Aug:17(6):535-542. doi: 10.1177/1474515118759065. Epub 2018 Feb 16 [PubMed PMID: 29448818]
Level 2 (mid-level) evidenceSchwaab B. [Cardiac Rehabilitation]. Die Rehabilitation. 2018 Apr:57(2):117-126. doi: 10.1055/s-0043-120904. Epub 2017 Dec 7 [PubMed PMID: 29216666]
El Hajj MS, Jaam MJ, Awaisu A. Effect of pharmacist care on medication adherence and cardiovascular outcomes among patients post-acute coronary syndrome: A systematic review. Research in social & administrative pharmacy : RSAP. 2018 Jun:14(6):507-520. doi: 10.1016/j.sapharm.2017.06.004. Epub 2017 Jun 13 [PubMed PMID: 28641999]
Level 1 (high-level) evidence