Introduction
The musculoskeletal system comprises one of the body's major tissue/organ systems. The three main types of muscle tissue are skeletal, cardiac, and smooth muscle groups.[1][2][3] Skeletal muscle attaches to the bone by tendons, and together they produce all body movements. The skeletal muscle fibers are crossed with a regular pattern of fine red and white lines, giving the muscle a distinctive striated appearance. Hence they are also known as striated muscles.[4][5][6][7][8]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
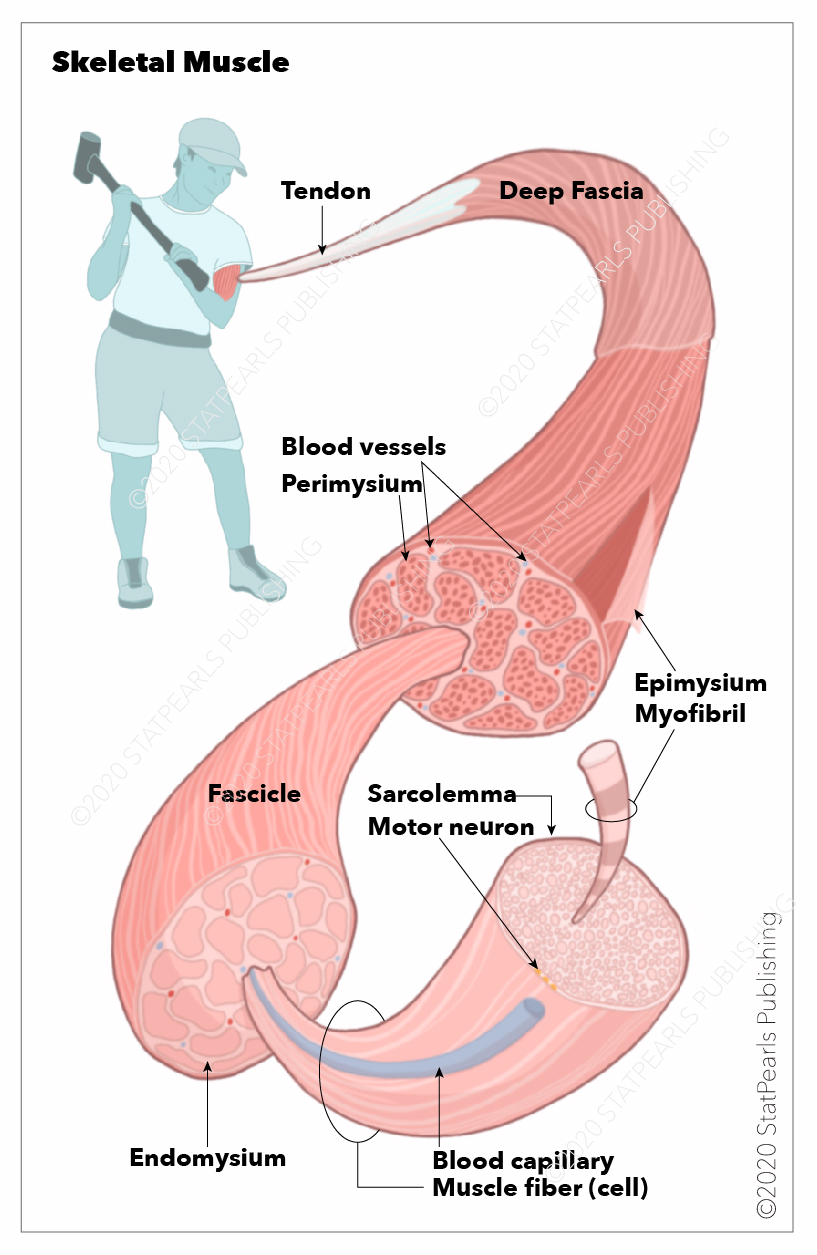
Skeletal muscle is one of the three significant muscle tissues in the human body. Each skeletal muscle consists of thousands of muscle fibers wrapped together by connective tissue sheaths. The individual bundles of muscle fibers in a skeletal muscle are known as fasciculi. The outermost connective tissue sheath surrounding the entire muscle is known as epimysium. The connective tissue sheath covering each fasciculus is known as perimysium, and the innermost sheath surrounding individual muscle fiber is known as endomysium.[9] Each muscle fiber is comprised of a number of myofibrils containing multiple myofilaments.
When bundled together, all the myofibrils get arranged in a unique striated pattern forming sarcomeres which are the fundamental contractile unit of a skeletal muscle. The two most significant myofilaments are actin and myosin filaments arranged distinctively to form various bands on the skeletal muscle. The stem cells which differentiate into mature muscle fibers are known as satellite cells which can be found between the basement membrane and the sarcolemma (the cell membrane surrounding the striated muscle fiber cell).[10] When stimulated by growth factors, they differentiate and multiply to form new muscle fiber cells.[11]
The primary functions of the skeletal muscle take place via its intrinsic excitation-contraction coupling process. As the muscle is attached to the bone tendons, the contraction of the muscle leads to movement of that bone that allows for the performance of specific movements. The skeletal muscle also provides structural support and helps in maintaining the posture of the body. The skeletal muscle also acts as a storage source for amino acids that different organs of the body can use for synthesizing organ-specific proteins.[12] The skeletal muscle also plays a central role in maintaining thermostasis and acts as an energy source during starvation.[9]
Embryology
Distinct transcriptional mechanisms and specific gene regulatory activity control the differentiation of muscle fibers.[13] During embryogenesis, the para-axial mesoderm undergoes stepwise differentiation to generate the muscle tissue. The para-axial mesoderm on either side of the neural tube starts to differentiate and undergoes segmentation to form the somites. The somites get stimulated by the myogenic regulatory factors to differentiate into a dermomyotome and sclerotome. These regulatory factors include the Wnt, Shh, and BMP4 proteins. The neural tube and the surface ectoderm are the primary sources of Wnt proteins, the Shh proteins(Sonic hedgehog) source from the notochord, and the lateral mesoderm plate produces the BMP4 protein.[14] The lateral aspect of the dermomyotome undergoes epithelial to mesenchymal transition as it proceeds to migrate on the ventral side to form a unique myotome below the dermatome.
The myotome then differentiates to form the skeletal muscles in the body after receiving stimulation from the Sonic Hedgehog (Shh) signaling molecule from the notochord, resulting in the Myf5 expression and subsequent differentiation.[15] The dorsomedial aspect of the myotome differentiates into epaxial myotome giving rise to back muscles. The ventrolateral aspect differentiates into hypaxial myotome that gives rise to muscles of the body wall.
Several signaling molecules like the Wnt and the BMP and some transcription factors like sine oculis homeobox are responsible for this differentiation. The development of skeletal muscles in the limb and the trunk depends on the expression of MyoD and Myf5 and their effects on the different myoblasts.[16] These embryonic myoblasts undergo further differentiation to form the primary muscle fibers and eventually secondary myofibers by the union of myoblasts in the fetus. After birth, the satellite cells act as stem cells and are responsible for the further growth and development of skeletal muscles.
Blood Supply and Lymphatics
The primary artery supplying blood to a particular skeletal muscle generally courses parallel to the longitudinal axis of the muscle fiber.[17] The primary artery gives off tributaries known as feed arteries that run perpendicularly to the primary artery and proceed towards the external connective tissue sheath of the muscle fiber called perimysium.[18] The feed artery branches into primary arterioles, which after two more orders of branching, give rise to transverse arterioles, which in turn give rise to terminal arterioles.[19] The terminal arterioles are the final vascular branches, and they perfuse the capillaries that are present within the endomysium and travel parallel to the longitudinal axis of the muscle fiber. The terminal arteriole, along with the capillaries that it supplies, is known as a microvascular unit. It is the smallest unit in the skeletal muscle where the blood flow can be regulated.
Lymph capillaries originate in skeletal muscle in the microvascular unit within the endomysium near the main capillary bed and drain the tissue fluid. These capillaries merge to form the lymphatic vessels as they drain the tissue fluid. These lymphatic vessels go through the perimysium and join with the larger lymphatic vessels. Unlike the blood vessels, the wall of the lymph vessels within the muscle does not have contractile property due to a lack of smooth muscles(in the wall), so they depend on the muscle movement and arteriolar pulsations to drain the lymph out.
Nerves
The neuronal innervation of a skeletal muscle typically comprises sensory nerve fibers, motor nerve fibers, and the neuromuscular junction. The nerve fibers are composed of myelinated as well as non-myelinated nerve fibers. The cell bodies of the neurons give rise to large axons, which are generally unbranched and travel to the target muscles for innervation. Near the target muscle, the axons divide into multiple smaller branches to innervate multiple muscle fibers. The motor nerve terminal has abundant mitochondria, endoplasmic reticulum, and numerous membrane-bound synaptic vesicles containing neurotransmitter- acetylcholine.[20] Once the action potential travels to the neuromuscular junction, a series of processes occur, culminating in the fusion of the membrane of the synaptic vesicles with the presynaptic membrane and the subsequent release of the neurotransmitter into the synaptic cleft.[21][22]
The postsynaptic membrane of the muscle fibers has a massive concentration of neurotransmitters (AchR) receptors. These receptors are transmembrane ligand-gated ion channels.[23] Once the neurotransmitter activates these ion channels, there is a rapid depolarization of the motor endplate, which initiates an action potential in the muscle fiber resulting in muscle contraction.[21]
Muscles
Each muscle comprises multiple tissues, including blood vessels, lymphatics, contractile muscle fibers, and connective tissue sheaths. The outermost sheath of connective tissue covering each muscle is called epimysium. Each muscle is made up of groups of muscle fibers called fascicles surrounded by a connective tissue layer called perimysium. Multiple units of individual muscle fibers within each fascicle are surrounded by endomysium, a connective tissue sheath. The two most essential myofilaments that make up the contractile elements of the muscle fiber are actin and myosin. They are arranged distinctively in a striated pattern to form the dark A band, the light I band, and the fundamental unit of contraction, also referred to as a sarcomere.
The sarcomere consists of a central M line, and attached to it on either side are the thick myofilaments of myosin. This forms the dark A band. The sarcomere is bordered by the Z-line, which serves as the site of origin of the thin myofilaments of actin that project towards each other as they partially overlap the myosin filaments.[9]The regulatory proteins, namely troponin C, I, T, and tropomyosin, play a key role in the myofilaments sliding mechanism leading to contraction. Titin and nebulin are the other major proteins that contribute to the mechanical properties of the muscle.[24] There is a unique T-tubule system in place for the conduction of neuronal action potential to the interior of the muscle cell via invaginations of the sarcolemma to enhance coordination and uniform muscle contraction.[25]
Clinical Significance
Skeletal muscles enable humans to move and perform daily activities. They play an essential role in respiratory mechanics and help maintain posture and balance. They also protect the vital organs in the body.
Various medical conditions result from abnormalities in the skeletal muscles' function. These diseases include myopathy, paralysis, myasthenia gravis, urinary and/or bowel incontinence, ataxia, weakness, tremors, and others. Disorders of the nerves can cause neuropathy and cause disturbances in the functionality of the skeletal muscles. In addition, skeletal muscle/tendon ruptures can occur acutely in high-level athletes or recreational sports participants and generate significant disability in all patients regardless of activity status.[26]
Muscle Cramps
Muscle cramps result in continuous, involuntary, painful, and localized contraction of an entire muscle group, individual single muscle, or select muscle fibers.[3] Generally, the cramp can last from minutes to a few seconds for idiopathic or known causes in healthy subjects or the presence of diseases. Palpating the muscle area of the cramp will present a knot.
Exercise-associated muscle cramps are the most frequent condition requiring medical/therapeutic intervention during sports.[27] The specific etiology is not well understood, and possible causes depend on the physiological or pathological situation in which the cramps appear. It is important to note that a painful contraction limited to a specific area does not mean that the cause of the onset of the cramp is necessarily local.
In specific clinical scenarios, the underlying etiology may relate to persistent, spastic muscle contractions that can significantly impact human function. A typical example of this condition manifests in the sternocleidomastoid muscle. Clinically, this is recognized in congenital torticollis or spasmodic torticollis.[28]
Other relevant conditions in this realm include, but are not limited to the following:
- Exercise-induced and heat-related muscle cramping
- Piriformis syndrome[6][29]
- Thoracic outlet syndrome (scalene muscle hypertrophy/spasticity)[5]
Palsy/Compression Neuropathy
At the opposite end of the spectrum, various muscle palsies exist secondary to the long-term, downstream effects of various nerve conditions and neuropathies, potentially resulting in flaccid conditions (which may be permanent or temporary). These syndromes and conditions include but are not limited to the following:
Media
(Click Image to Enlarge)
References
Goodman CA, Hornberger TA, Robling AG. Bone and skeletal muscle: Key players in mechanotransduction and potential overlapping mechanisms. Bone. 2015 Nov:80():24-36. doi: 10.1016/j.bone.2015.04.014. Epub [PubMed PMID: 26453495]
Wilke J, Engeroff T, Nürnberger F, Vogt L, Banzer W. Anatomical study of the morphological continuity between iliotibial tract and the fibularis longus fascia. Surgical and radiologic anatomy : SRA. 2016 Apr:38(3):349-52. doi: 10.1007/s00276-015-1585-6. Epub 2015 Nov 2 [PubMed PMID: 26522465]
Bordoni B, Sugumar K, Varacallo MA. Muscle Cramps. StatPearls. 2025 Jan:(): [PubMed PMID: 29763070]
Bordoni B, Black AC, Varacallo M. Anatomy, Tendons. StatPearls. 2023 Jan:(): [PubMed PMID: 30020609]
Bordoni B, Varacallo M. Anatomy, Head and Neck, Scalenus Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 30085600]
Chang A, Ly N, Varacallo M. Piriformis Injection. StatPearls. 2023 Jan:(): [PubMed PMID: 28846327]
Bourne M, Talkad A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb, Foot Fascia. StatPearls. 2023 Jan:(): [PubMed PMID: 30252299]
Bordoni B, Mahabadi N, Varacallo M. Anatomy, Fascia. StatPearls. 2023 Jan:(): [PubMed PMID: 29630284]
Frontera WR, Ochala J. Skeletal muscle: a brief review of structure and function. Calcified tissue international. 2015 Mar:96(3):183-95. doi: 10.1007/s00223-014-9915-y. Epub 2014 Oct 8 [PubMed PMID: 25294644]
Hikida RS. Aging changes in satellite cells and their functions. Current aging science. 2011 Dec:4(3):279-97 [PubMed PMID: 21529324]
Level 3 (low-level) evidenceStone WL, Leavitt L, Varacallo M. Physiology, Growth Factor. StatPearls. 2023 Jan:(): [PubMed PMID: 28723053]
Wolfe RR. The underappreciated role of muscle in health and disease. The American journal of clinical nutrition. 2006 Sep:84(3):475-82 [PubMed PMID: 16960159]
Buckingham M, Rigby PW. Gene regulatory networks and transcriptional mechanisms that control myogenesis. Developmental cell. 2014 Feb 10:28(3):225-38. doi: 10.1016/j.devcel.2013.12.020. Epub [PubMed PMID: 24525185]
Level 3 (low-level) evidenceHernández-Hernández JM, García-González EG, Brun CE, Rudnicki MA. The myogenic regulatory factors, determinants of muscle development, cell identity and regeneration. Seminars in cell & developmental biology. 2017 Dec:72():10-18. doi: 10.1016/j.semcdb.2017.11.010. Epub 2017 Nov 15 [PubMed PMID: 29127045]
Borycki AG, Brunk B, Tajbakhsh S, Buckingham M, Chiang C, Emerson CP Jr. Sonic hedgehog controls epaxial muscle determination through Myf5 activation. Development (Cambridge, England). 1999 Sep:126(18):4053-63 [PubMed PMID: 10457014]
Level 3 (low-level) evidenceKablar B, Krastel K, Ying C, Asakura A, Tapscott SJ, Rudnicki MA. MyoD and Myf-5 differentially regulate the development of limb versus trunk skeletal muscle. Development (Cambridge, England). 1997 Dec:124(23):4729-38 [PubMed PMID: 9428409]
Level 3 (low-level) evidenceBagher P, Segal SS. Regulation of blood flow in the microcirculation: role of conducted vasodilation. Acta physiologica (Oxford, England). 2011 Jul:202(3):271-84. doi: 10.1111/j.1748-1716.2010.02244.x. Epub 2011 Mar 1 [PubMed PMID: 21199397]
Level 3 (low-level) evidenceSegal SS. Integration of blood flow control to skeletal muscle: key role of feed arteries. Acta physiologica Scandinavica. 2000 Apr:168(4):511-8 [PubMed PMID: 10759588]
Level 3 (low-level) evidenceDodd LR, Johnson PC. Diameter changes in arteriolar networks of contracting skeletal muscle. The American journal of physiology. 1991 Mar:260(3 Pt 2):H662-70 [PubMed PMID: 2000963]
Level 3 (low-level) evidenceHeuser JE, Salpeter SR. Organization of acetylcholine receptors in quick-frozen, deep-etched, and rotary-replicated Torpedo postsynaptic membrane. The Journal of cell biology. 1979 Jul:82(1):150-73 [PubMed PMID: 479296]
Level 3 (low-level) evidenceSlater CR. The Structure of Human Neuromuscular Junctions: Some Unanswered Molecular Questions. International journal of molecular sciences. 2017 Oct 19:18(10):. doi: 10.3390/ijms18102183. Epub 2017 Oct 19 [PubMed PMID: 29048368]
Caire MJ, Reddy V, Varacallo M. Physiology, Synapse. StatPearls. 2023 Jan:(): [PubMed PMID: 30252303]
Wu H, Xiong WC, Mei L. To build a synapse: signaling pathways in neuromuscular junction assembly. Development (Cambridge, England). 2010 Apr:137(7):1017-33. doi: 10.1242/dev.038711. Epub [PubMed PMID: 20215342]
Level 3 (low-level) evidenceOttenheijm CA, Granzier H. Lifting the nebula: novel insights into skeletal muscle contractility. Physiology (Bethesda, Md.). 2010 Oct:25(5):304-10. doi: 10.1152/physiol.00016.2010. Epub [PubMed PMID: 20940435]
Level 3 (low-level) evidenceJayasinghe I, Launikonis BS. Three-dimensional reconstruction and analysis of the tubular system of vertebrate skeletal muscle. Journal of cell science. 2013 Sep 1:126(Pt 17):4048-58. doi: 10.1242/jcs.131565. Epub 2013 Jun 26 [PubMed PMID: 23813954]
Level 3 (low-level) evidenceShamrock AG, Dreyer MA, Varacallo M. Achilles Tendon Rupture. StatPearls. 2023 Jan:(): [PubMed PMID: 28613594]
Giuriato G, Pedrinolla A, Schena F, Venturelli M. Muscle cramps: A comparison of the two-leading hypothesis. Journal of electromyography and kinesiology : official journal of the International Society of Electrophysiological Kinesiology. 2018 Aug:41():89-95. doi: 10.1016/j.jelekin.2018.05.006. Epub 2018 May 26 [PubMed PMID: 29857264]
Bordoni B, Jozsa F, Varacallo M. Anatomy, Head and Neck, Sternocleidomastoid Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 30422476]
Hicks BL, Lam JC, Varacallo M. Piriformis Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 28846222]
Hohman MH, Warner MJ, Varacallo MA. Bell Palsy. StatPearls. 2025 Jan:(): [PubMed PMID: 29493915]
Aleksenko D, Varacallo M. Guyon Canal Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 28613717]
Pester JM, Varacallo M. Ulnar Nerve Block Techniques. StatPearls. 2023 Jan:(): [PubMed PMID: 29083721]
Akhondi H, Varacallo M. Anterior Interosseous Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 30247831]
Buchanan BK, Maini K, Varacallo M. Radial Nerve Entrapment. StatPearls. 2023 Jan:(): [PubMed PMID: 28613749]
Sevy JO, Varacallo M. Carpal Tunnel Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 28846321]
Pester JM, Bechmann S, Varacallo M. Median Nerve Block Techniques. StatPearls. 2023 Jan:(): [PubMed PMID: 29083641]
Bishop KN, Varacallo M. Anatomy, Shoulder and Upper Limb, Dorsal Scapular Nerve. StatPearls. 2023 Jan:(): [PubMed PMID: 29083775]
Merryman J, Varacallo M. Klumpke Palsy. StatPearls. 2023 Jan:(): [PubMed PMID: 30285395]