Introduction
The Amsler Grid is a square-shaped grid used to detect or monitor metamorphopsia or scotoma involving the central visual field in various disorders of the macula and optic nerve head. Specifically, it is used as an inexpensive home monitoring device for early detection of metamorphopsia due to wet age-related macular degeneration. Also, it may be used as a macular function test before cataract surgery.
The grid gets its name from Marc Amsler (1891-1968), a Swiss ophthalmologist, who described the chart in 1947.[1] He was a student of Jules Gonin (1870-1935). He might have gotten the idea of the grid from Edmund Landolt (1846-1926), who devised a similar small card with a grid pattern to be kept in the center of the perimeter.[1] Jacob Hermann Knapp (1832-1911) described scotoma and metamorphopsia in traumatic maculopathy with choroidal rupture using horizontal lines in 1869. Richard Forster (1825-1902) demonstrated metamorphopsia using a square grid in 1874.[1]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The location of the fovea is approximately two disc diameters (3 mm on average) temporal to the temporal margin of the optic disc. The physiological blind spot on the visual field corresponds anatomically with the optic disc. In the visual field, the blind spot is located usually at 15 degrees temporal to the point of fixation (anatomically corresponding to fovea).[2] The shape of the blind spot is vertically oval measuring 7.5 degrees vertically and 5.5 degrees horizontally.[2] Another anatomically important fact is that the density of cones at the center of the fovea is maximum, extrapolated to around 150000 to 180000 cells/mm, which reduces rapidly to 6000 cones/mm at 1.5 mm from the fovea,[3] which leads to the best visual acuity at the fovea.
The Oxford dictionary defines metamorphopsia as 'defective visual perception in which objects appear distorted in shape, size, etc.' The proposed mechanism of metamorphopsia include[4][5][6]:
- Displacement of photoreceptors causing a defective localization of perceived image
- Using optical coherence tomography (OCT), it has been noted that in epiretinal membrane thickening of the inner nuclear layer (INL) is associated with metamorphopsia while inner segment-outer segment junction status affects visual acuity
- The hypothesis is that 'the structures of horizontal, bipolar, amacrine, and Muller cell bodies, which comprise INL, may change
- This inhibits the function of synaptic junctions and lowers photoreceptor sensitivity, causing metamorphopsia
- Additionally, thickening of GCL (ganglion cell layer) and INL may induce aberration in the retina, and quality of vision may undergo 'deterioration'
- Other visual processing may be involved in the perception of metamorphopsia; this includes cortical processing, and the details of the stimulus/scene might have a role
Indications
The Amsler grid is valid in the following scenarios[7]:
- Wet age-related macular degeneration (wAMD) - The choroidal neovascular membrane (CNVM) causes metamorphopsia and new scotoma
- Central serous chorioretinopathy (CSCR) - Causes a central scotoma which may be round or oval depending on the shape of neurosensory retinal detachment
- Epiretinal membrane and other vitreoretinal interface diseases, which causes metamorphopsia.
- Acute macular neuroretinopathy - Flower petal-like scotoma is seen corresponding to fundus lesions which become more prominent in near-infrared (NIR) or multicolor imaging
- Cystoid macular edema - The distance between the photoreceptors increase due to macular edema, and things appear smaller (micropsia); cystoid macular edema may result from diabetic maculopathy, retinal vein occlusion, intermediate uveitis, CNVM, and other diseases
- Non-arteritic anterior ischemic optic neuropathy- The grid might reveal an altitudinal defect in the visual field
- Pituitary tumor - The Amsler grid may be used to demonstrate bitemporal hemianopia
- Hydroxychloroquine retinopathy may cause central scotoma; however, Amsler grid is currently not recommended as a screening tool for hydroxychloroquine retinopathy
Contraindications
There is no contraindication to using Amsler grid. There should be a reasonable vision level to discern the lines of the grid. However, the sensitivity to detect wAMD changes may be low, and the Amsler grid does not replace the need for ophthalmic examination. As the grid evaluates only 10 degrees temporal to fixation, the physiological blind spot is not appreciated in Amsler grid. Glaucomatous visual field defects may not be detected in Amsler grid until the disease is advanced and field defect reaches close to fixation.
Equipment
The grid measures 10 cm × 10 cm. When used at 33 cm from the eye, the grid can check for changes in a 20° field. This field spans 10° on each side (above, below, and on the left and right side) of the fixation.
There are 7 charts of the Amsler Grid each with a dimension of 10 cm × 10 cm.
- Chart 1- The lines are white in a black background. There are 20 small squares in each side of the grid. Thus each side of the small squares measures 10cm/20= 5mm. Each small square cast an angle of 20°/20=1° field when the grid is held at 33 cm from the eye.
- Chart 2- Four diagonal white lines are placed over the chart 1 to help fixation in an eye with a central scotoma.
- Chart 3- It is similar to chart 1, except the fact that there are red (in place of white) lines over a black background. Red specifically stimulates the long wavelength cones. This chart is to pick up subtle red desaturation in diseases including bitemporal hemianopia in a pituitary tumor, toxic optic neuropathy, and toxic maculopathy.
- Chart 4- There is no line. Over a black background, there is a central large round white dot. In other spaces, there are multiple small random white dots. This chart is used to differentiate scotoma from metamorphopsia as there is no form appreciable for distortion.
- Chart 5- There is a square with 21 horizontal white lines on black background 5mm apart. A central white dot is present for fixation. It is used to determine any specific meridian of metamorphopsia specifically in patients with reading difficulties.
- Chart 6- This is a modification of chart 5. Of the 7 charts, only this chart has black lines on white background. The central lines are closer than the chart 5, helping to evaluate fine metamorphopsia near fixation.
- Chart 7- This is a modification of chart 1. There is a central area with smaller squares each one subtending 0.5° field. Small scotoma or area of metamorphopsia near the fixation can be demonstrated with this chart.
Technique or Treatment
The grid is kept at 33 cm from the eye. The illumination of the chart should be good. Light exposure directly over the eye (in the form of slit-lamp examination, indirect ophthalmoscopy, and others) should be avoided immediately before using the grid to avoid a photostress effect. The patient wears near correction if any. Pupils should not be dilated. The patient is asked to close one eye. With the open eye through the near glasses, the patient is instructed to look at the central dot of the grid. In patients with poor fixation, the eye should focus at the center of the grid so that all the 4 corners are simultaneously visible. While keeping the eye fixated over the center of the grid, the patient has to appreciate is the lines are parallel or seem distorted (metamorphopsia). Also, he/she should note if some of the small squares are missing or blurry. The patient should mark the grid with the area of abnormality so that it can be compared later for any progression, stabilization, or improvement. If the patient can not see the corners, diseases like glaucoma and retinitis pigmentosa should be ruled out. Amsler grid should be checked at least once weekly.
Alternative techniques to document metamorphopsia include:
- M chart[8] or metamorphopsia chart- There are 19 dotted lines with separation between the dots between 0.2° (fine) to 2° (coarse) visual angles. As the patient sees more coarsely separated dots, the metamorphopsia usually reduces and disappears. The metamorphopsia is quantified by 'the minimum visual angle of the dotted lines needed to cause the metamorphopsia to disappear'. This can measure both horizontal and vertical metamorphopsia. However, the shape and size of the metamorphopsia cannot be quantified using this test.
- Preferential hyperacuity perimeter PHP- Hyperacuity or Vernier acuity is a cortically mediated function to detect very subtle misalignments which may be as less as 3-6 seconds of arc. [9] It is defined as 'the ability to perceive a difference in the relative spatial localization of 2 or more visual stimuli'.[10]
- Foresee Home (Notal Vision, Tel Aviv, Israel) is a type of PHP. It has been approved by the FDA (Food and Drug Administration, USA) for 'use in the detection and characterization of central and paracentral metamorphopsia (visual distortion) in patients with age-related macular degeneration, as an aid in monitoring progression of disease factors causing metamorphopsia including but not limited to choroidal neovascularization (CNV). It is intended to be used at home for patients with stable fixation.' This device tests the central 14° of the visual field and total 500 data points are tested, 3-5 times each. However, it is not suitable for patients with cognitive decline (Alzheimer's disease) or if the patient can not establish a baseline in 2 attempts.
- Macular Computerized Psychophysical Test (MCPT) uses hyperacuity to detect metamorphopsia.[11]
- PreView PHP (Carl Zeiss Meditec, Dublin, CA)- This device also uses the principles of PHP. In a study, it was concluded that it can 'detect recent-onset CNV resulting from AMD and can differentiate it from an intermediate stage of AMD with high sensitivity and specificity'.[10]
- Shape discrimination hyperacuity (SDH)- Very minor sinusoidal deviation from circularity is detected by human eyes.[12] The threshold for SDH is <10 seconds of arc and is not affected by age or reduction of contrast at low radial frequencies.[9] Using this principle, radial shape discrimination testing may be used to detect new onset wet AMD.[13] Handheld SDH is available (myVisionTrack; Vital Art and Science, Inc., Richardson, TX) for smartphones (iOS; Apple, Inc., Cupertino, CA).[14] It has been cleared by FDA to be used as an Ophthalmic medical device, 'for the detection and characterization of central three degrees metamorphopsia (visual distortion) in patients with maculopathy, including age-related macular degeneration and diabetic eye disease, and as an aid in monitoring disease factors causing metamorphopsia. It is intended to be used by patients who have the capability to regularly perform a simple self-test at home'. The patient uses the software twice weekly and it notifies the eye care professional in case of any change in visual function.
- Differential perimetry[15] - In case of displacement of photoreceptors, the visual field projection changes. This leads to loss of correspondence of the visual field with the normal fellow eye. This can help document metamorphopsia using binocular perimetry with Goldmann perimeter.
- Three-dimensional computer-automated threshold Amsler grid test (3D CTAG)- This test has been described by Fink and Sadun from Doheny Eye Institute, California.[16] It characterizes the scotoma in 3 dimensions with excellent detail ('location, extent, slope, depth, and shape').[16]
Other techniques/instruments which may be used to document scotoma include-
- Perimeter- Static (Humphrey field analyzer, the 10-2 protocol for central scotoma) or dynamic (Goldmann perimeter, tangent screen), or both static and kinetic (Octopus)
- Microperimetry- This machine checks the visual threshold of a specific area of the retina so that a correlation between structure and function is possible in a pictorial manner on an overlay of the fundus image. It also identifies any preferred retinal loci. The available machines are Nidek MP-3 (Nidek Co. Ltd., Aichi, Japan), and Macular Integrity Assessment microperimeter (MAIA, CentreVue, Padova, Italy).[17]
Clinical Significance
Amsler grid is an important simple tool to detect or monitor macular diseases.
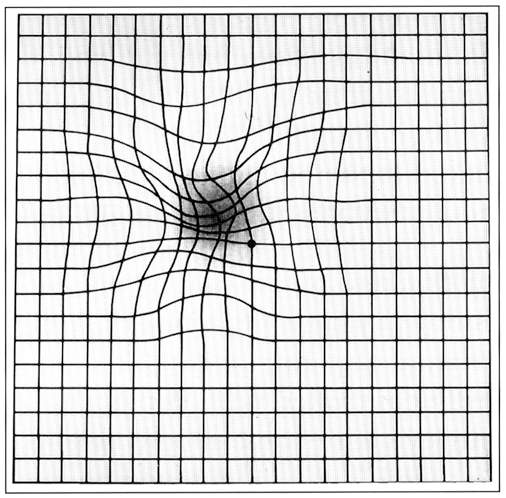
Metamorphopsia- Macropsia is denoted by the widening of the small squares compared to the nearby small squares. The parallel lines seem to be curved away from each other at this area. In the area of micropsia, the parallel lines seem to be drawn towards each other.
Scotoma- Merriam Webster dictionary defines scotoma as 'a spot in the visual field in which vision is absent or deficient.' A scotoma is surrounded by an area of the normal field of vision. A scotoma may be absolute (absent visual recognition of that area in spite of increasing the stimulus intensity) or relative (the stimulus presented at the scotoma becomes visible if stimulus intensity is increased). In Amsler grid, the relative scotoma appears as a veil partially obscuring the smaller squares and may be of different shapes. Such scotoma may be better appreciated if the illumination of the grid is reduced. Scotomas may be positive (something like spot or haze or smoke obscures central vision) or negative (the patient is unaware of scotoma unless tested).
Amsler grid home monitoring has various limitations including:
- Suprathreshold stimulus
- No monitor for fixation- stability of fixation is not monitored.
- No quantification of metamorphopsia
- Not interactive
- Scotoma detection and mapping may be suboptimal
- Need for good near vision to discern the grids
- Poor repeatability of scotoma[18]- Size, shape, and location of the scotoma detected on Amsler grid may not be same if the same patient is re-examined with Amsler grid even within 15 minutes. This may be related to 'perceptual completion phenomenon' which results from 'a filling in of the missing information when part of an image falls on a blind area of the visual field' which may be cortically mediated.[18][19] Due to the same phenomenon, the blind spot due to the optic disc is not usually appreciated. It has been noted that scotoma less than 6 degrees may not be detected by Amsler grid.[20]
- Low sensitivity for detection of peripheral changes due to the crowding effect of the peripheral lines
- Poor compliance
The modifications of the Amsler chart include:
- Threshold Amsler chart- The effective luminance of the white on black Amsler Grid may be lowered by placing a cross polarizing lens in front of the eye[21] and this may be better in picking up scotoma than the standard Amsler chart.[18]
- The sensitivity of the Amsler grid may also be improved with the use of red grids.[22]
- A Modified Amsler Chart with 'a grid of black lines on a white background measuring 12 × 12 cm with grid squares of 2 × 2 cm' has been reported by Shinoda and colleagues.[23] There are 6X6 or 36 squares. The patient with metamorphopsia is asked to trace the lines as they see it. The length of all the distorted lines drawn by the patient is measured in milimeters except the outer margin of the chart.
- Sine Amsler chart[24] uses 8 modified Amsler grids with central sine waves instead of lines. The frequency of the sine wave is constant in each chart, but the amplitude is different. The patient is asked to note the amount of metamorphopsia in an Amsler grid. Then he/she is asked to corroborate the magnitude of metamorphopsia to a specific sine Amsler chart
- Morphision[25]- It consists of 50 modified Amsler grids in an A5 sized booklet. 'The control plate (1) allows detection and localization of distortion, the second plate (2) identifies the pattern of distortion, and the remaining 48 plates quantify metamorphopsia'.[25] Various charts consist of sine waves replacing lines, and cushion or barrel-like distortion.
Enhancing Healthcare Team Outcomes
Appropriate use of the Amsler grid requires an interprofessional team. The nurses and optometrists who are involved in patient care should be taught how to handle the instrument properly without any damage. Also, the nurses should assist the clinician with giving proper instructions to the patient so that the final result will not be ambiguous. Often patients will use the Amsler grid at home. The nurse should monitor compliance and report to the ophthalmologist or optometrist if the patient is not compliant or inappropriately using the grid. It is also important to not to apply any mydriatic in the eye prior to the test. If the nurse or clinician accidentally uses a mydriatic, the team should be informed of the application and the test rescheduled on a later date. Interprofessional application and education of patients using the Amsler grid will result in the best outcomes. [Level V]
Media
(Click Image to Enlarge)
References
Marmor MF. A brief history of macular grids: from Thomas Reid to Edvard Munch and Marc Amsler. Survey of ophthalmology. 2000 Jan-Feb:44(4):343-53 [PubMed PMID: 10667441]
Level 3 (low-level) evidenceAbadi RV, Jeffery G, Murphy JS. Awareness and filling-in of the human blind spot: linking psychophysics with retinal topography. Investigative ophthalmology & visual science. 2011 Jan 25:52(1):541-8. doi: 10.1167/iovs.10-5910. Epub 2011 Jan 25 [PubMed PMID: 20847110]
Jonas JB, Schneider U, Naumann GO. Count and density of human retinal photoreceptors. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 1992:230(6):505-10 [PubMed PMID: 1427131]
Watanabe A, Arimoto S, Nishi O. Correlation between metamorphopsia and epiretinal membrane optical coherence tomography findings. Ophthalmology. 2009 Sep:116(9):1788-93. doi: 10.1016/j.ophtha.2009.04.046. Epub 2009 Jul 30 [PubMed PMID: 19643494]
Level 2 (mid-level) evidenceOkamoto F, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T. Associations between metamorphopsia and foveal microstructure in patients with epiretinal membrane. Investigative ophthalmology & visual science. 2012 Oct 3:53(11):6770-5. doi: 10.1167/iovs.12-9683. Epub 2012 Oct 3 [PubMed PMID: 22969078]
Wiecek E, Lashkari K, Dakin SC, Bex P. Novel quantitative assessment of metamorphopsia in maculopathy. Investigative ophthalmology & visual science. 2014 Nov 18:56(1):494-504. doi: 10.1167/iovs.14-15394. Epub 2014 Nov 18 [PubMed PMID: 25406293]
Marmor MF, Kellner U, Lai TY, Melles RB, Mieler WF, American Academy of Ophthalmology. Recommendations on Screening for Chloroquine and Hydroxychloroquine Retinopathy (2016 Revision). Ophthalmology. 2016 Jun:123(6):1386-94. doi: 10.1016/j.ophtha.2016.01.058. Epub 2016 Mar 16 [PubMed PMID: 26992838]
Matsumoto C, Arimura E, Okuyama S, Takada S, Hashimoto S, Shimomura Y. Quantification of metamorphopsia in patients with epiretinal membranes. Investigative ophthalmology & visual science. 2003 Sep:44(9):4012-6 [PubMed PMID: 12939323]
Midena E, Vujosevic S. Metamorphopsia: An Overlooked Visual Symptom. Ophthalmic research. 2015:55(1):26-36. doi: 10.1159/000441033. Epub 2015 Nov 11 [PubMed PMID: 26554918]
Alster Y, Bressler NM, Bressler SB, Brimacombe JA, Crompton RM, Duh YJ, Gabel VP, Heier JS, Ip MS, Loewenstein A, Packo KH, Stur M, Toaff T, Preferential Hyperacuity Perimetry Research Group. Preferential Hyperacuity Perimeter (PreView PHP) for detecting choroidal neovascularization study. Ophthalmology. 2005 Oct:112(10):1758-65 [PubMed PMID: 16154198]
Loewenstein A, Malach R, Goldstein M, Leibovitch I, Barak A, Baruch E, Alster Y, Rafaeli O, Avni I, Yassur Y. Replacing the Amsler grid: a new method for monitoring patients with age-related macular degeneration. Ophthalmology. 2003 May:110(5):966-70 [PubMed PMID: 12750099]
Level 3 (low-level) evidenceWilkinson F, Wilson HR, Habak C. Detection and recognition of radial frequency patterns. Vision research. 1998 Nov:38(22):3555-68 [PubMed PMID: 9893789]
Pitrelli Vazquez N, Harding SP, Heimann H, Czanner G, Knox PC. Radial shape discrimination testing for new-onset neovascular age-related macular degeneration in at-risk eyes. PloS one. 2018:13(11):e0207342. doi: 10.1371/journal.pone.0207342. Epub 2018 Nov 8 [PubMed PMID: 30408127]
Wang YZ, He YG, Mitzel G, Zhang S, Bartlett M. Handheld shape discrimination hyperacuity test on a mobile device for remote monitoring of visual function in maculopathy. Investigative ophthalmology & visual science. 2013 Aug 13:54(8):5497-505. doi: 10.1167/iovs.13-12037. Epub 2013 Aug 13 [PubMed PMID: 23860761]
Level 2 (mid-level) evidenceJensen OM, Larsen M. Objective assessment of photoreceptor displacement and metamorphopsia: a study of macular holes. Archives of ophthalmology (Chicago, Ill. : 1960). 1998 Oct:116(10):1303-6 [PubMed PMID: 9790627]
Fink W, Sadun AA. Three-dimensional computer-automated threshold Amsler grid test. Journal of biomedical optics. 2004 Jan-Feb:9(1):149-53 [PubMed PMID: 14715067]
Cassels NK, Wild JM, Margrain TH, Chong V, Acton JH. The use of microperimetry in assessing visual function in age-related macular degeneration. Survey of ophthalmology. 2018 Jan-Feb:63(1):40-55. doi: 10.1016/j.survophthal.2017.05.007. Epub 2017 Jun 1 [PubMed PMID: 28579549]
Level 3 (low-level) evidenceAchard OA, Safran AB, Duret FC, Ragama E. Role of the completion phenomenon in the evaluation of Amsler grid results. American journal of ophthalmology. 1995 Sep:120(3):322-9 [PubMed PMID: 7661204]
Level 1 (high-level) evidenceRamachandran VS, Gregory RL. Perceptual filling in of artificially induced scotomas in human vision. Nature. 1991 Apr 25:350(6320):699-702 [PubMed PMID: 2023631]
Schuchard RA. Validity and interpretation of Amsler grid reports. Archives of ophthalmology (Chicago, Ill. : 1960). 1993 Jun:111(6):776-80 [PubMed PMID: 8512478]
Wall M, Sadun AA. Threshold Amsler grid testing. Cross-polarizing lenses enhance yield. Archives of ophthalmology (Chicago, Ill. : 1960). 1986 Apr:104(4):520-3 [PubMed PMID: 3954654]
Slavin ML. The use of the red Amsler grid and red-green lenses in detecting spurious paracentral visual field defects. American journal of ophthalmology. 1987 Mar 15:103(3 Pt 1):338-9 [PubMed PMID: 3826248]
Level 3 (low-level) evidenceShinoda K, Ishida S, Kawashima S, Matsuzaki T, Yamada K, Katsura H. A new method for quantification of metamorphopsia in patients with epiretinal membrane. Japanese journal of ophthalmology. 2000 Jul-Aug:44(4):424-7 [PubMed PMID: 10974300]
Bouwens MD, Van Meurs JC. Sine Amsler Charts: a new method for the follow-up of metamorphopsia in patients undergoing macular pucker surgery. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2003 Feb:241(2):89-93 [PubMed PMID: 12605261]
Ugarte M, Shunmugam M, Laidlaw DA, Williamson TH. Morphision: a method for subjective evaluation of metamorphopsia in patients with unilateral macular pathology (i.e., full thickness macular hole and epiretinal membrane). Indian journal of ophthalmology. 2013 Nov:61(11):653-8. doi: 10.4103/0301-4738.117804. Epub [PubMed PMID: 24008785]
Level 2 (mid-level) evidence