 Anatomy, Head and Neck: Eye, Superior Tarsal Muscle (Müller Muscle)
Anatomy, Head and Neck: Eye, Superior Tarsal Muscle (Müller Muscle)
Introduction
The superior tarsal muscle, also known as the Müller muscle, is an accessory smooth muscle that allows for the retraction and elevation of the upper eyelid. This muscle receives sympathetic innervation from fibers originating from the sympathetic cervical ganglion, and vascular supply from the superior branches of the ophthalmic artery.
The superior tarsal muscle is often affected in thyroid eye disease-associated ophthalmopathy as the disease-mediated inflammation and fibrosis occurring within the muscle cause further upper lid retraction. Injury to the innervation of the superior tarsal muscle, as seen in Horner Syndrome, results in ptosis.
The superior tarsal muscle is routinely encountered in oculoplastic surgery, including ptosis-correcting procedures. Different approaches can be used to correct ptosis, but the Müller muscle-conjunctival resection involves removing a portion of the superior tarsal muscle to remedy the ptosis (see Image. Eye—Superior Tarsal Muscle).[1][2] Understanding the anatomy and function of the superior tarsal muscle is essential in managing conditions that affect upper eyelid movement.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The superior tarsal muscle is composed of thin fibers of smooth muscle tissue and is approximately 15 mm wide and 10 mm long. The muscle originates from the inferior aspect of the levator palpebrae superioris and inserts onto the superior tarsal plate of the upper eyelid.[3] The superior tarsal plate is made of dense connective tissue and functions to support the upper eyelid and maintain its shape.
The superior tarsal muscle has the unique function of assisting the levator palpebrae superioris by maintaining upper eyelid elevation after being raised by the levator palpebrae superioris.[4] The superior tarsal muscle also lifts the upper eyelid to an additional 2 mm beyond the range of the levator palpebrae superioris, following a sympathetic nervous system response.[5]
The superior tarsal muscle has a much more significant role in levator action when compared to the levator palpebrae superioris than previously thought. Research has determined that the superior tarsal muscle transmits considerable power to the levator palpebrae superioris when elevating the eyelid, furthering the synergistic interaction between itself and the levator palpebrae superioris.[6]
Embryology
The eyelid develops as a whole from a combination of secondary mesenchymal (mesoderm invaded by cranial neural crest cells) and surface ectodermal tissues. The superior tarsal muscle, along with the orbital septum, the tarsal plate, and the levator palpebrae superioris, develop from secondary mesenchymal tissues.
Eyelid formation is first seen at the 5-week mark, and the levator aponeurosis (point of origin of the superior tarsal muscle) is first seen at week 12. The superior tarsal muscle is then seen at week 14.[7]
Blood Supply and Lymphatics
Although considerable variation exists in the arterial supply of the eyelid, the superior tarsal muscle is most commonly supplied by the superior (lateral) branch of the ophthalmic artery. This branch also provides blood flow to the levator muscle, superior rectus, superior oblique, and lateral rectus. The ophthalmic artery also has a medial muscular branch that supplies blood to the remaining extraocular muscles.[8]
Venous drainage of the superior tarsal muscle occurs through the vortex veins, which originate from the posterior aspect of the eye. Blood from the vortex veins then flows into the superior and inferior orbital veins before reaching the cavernous sinus.
Nerves
The sympathetic nervous system innervates the superior tarsal muscle. More specifically, the muscle is innervated by postganglionic sympathetic fibers that have synapses in the superior sympathetic cervical ganglia. These fibers wrap around the internal carotid artery, forming the internal carotid plexus, and enter the skull. From here, the plexus fibers reach the orbit via the ophthalmic artery and subsequently innervate the superior tarsal muscle [9].
Muscles
The superior tarsal muscle is made of smooth muscle but displays several characteristics that differentiate it from the smooth muscle found elsewhere in the body. Histological analyses of the muscle reveal an area of gradual transition between the striated skeletal muscle of the levator palpebrae superioris and the smooth muscle of the superior tarsal muscles. Thus, smooth muscle fibers mix with striated muscle fibers beyond this transition zone. Fibers of both muscles are also interspersed with connective tissue.[10]
Physiologic Variants
The superior tarsal muscle has specific physiologic variants that differ based on their attachment to the superior tarsal plate. Four variations exist, as listed below.
- Pattern 1: The superior tarsal muscle attaches to the upper border of the superior tarsal plate.
- Pattern 2M (medial): The superior tarsal muscle attaches to the medial aspect of the plate.
- Pattern 2L (lateral): The superior tarsal muscle attaches to the lateral aspect of the plate.
- Pattern 3: The superior tarsal muscle attaches along the whole extent of the superior tarsal plate.
Pattern 3 is the most frequently observed variant.[10]
Surgical Considerations
Specific surgeries that encounter the superior tarsal muscle include procedures that correct elevation dysfunctions of the upper eyelid. Müller muscle-conjunctival resection is a surgical procedure used to treat blepharoptosis. The surgery is performed using a conjunctival approach where the conjunctiva, the Müller muscle, and sometimes, a portion of the tarsal plate are resected.
Levator advancement or resection is another surgical procedure used to treat blepharoptosis. Here, the surgery is completed through an external eyelid crease incision, and a portion of the levator palpebrae superioris is imbricated or advanced. Given its proximity to the superior tarsal muscle, care is taken not to damage the superior tarsal muscle, which can result in overcorrection of the blepharoptosis.
The type of surgery chosen relies on a multitude of factors, including the etiology of the ptosis, the current function of the levator muscle, and the response to sympathomimetic eye drops.
A recent meta-analysis comparing the outcomes of Müller muscle conjunctival resection with those of external levator advancement in patients undergoing ptosis surgery demonstrated that both procedures were efficacious in treating ptosis. While this study found no statistical difference between the 2 procedures regarding the postoperative marginal reflex distance (the distance from the upper lid margin to the corneal light reflex), it did reveal that rates of overcorrection and reoperations were higher in the levator advancement group.[11] However, the most important factors for determining the type of surgery required include the degree and type of ptosis, the amount of levator function, and the surgeon's experience or comfort with the procedure.[12]
Clinical Significance
The superior tarsal muscle plays an accessory but pertinent role in lid elevation and retraction. The clinical significance of this muscle is greatly elevated in conditions such as thyroid eye disease and Horner syndrome.
In thyroid eye disease, including Graves orbitopathy, lymphocytes infiltrate the extraocular muscles and superior tarsal muscle, causing enlargement of these structures. While chronic infiltration and inflammation in the extraocular muscles lead to proptosis and restrictions in extraocular movements, the same process in the superior tarsal muscle can lead to lid retraction.
In Horner syndrome, a constellation of upper eyelid ptosis, miosis, and anhidrosis occurs due to lesions along the sympathetic pathway. Ptosis arises from superior tarsal muscle paralysis.[13]
Media
(Click Image to Enlarge)
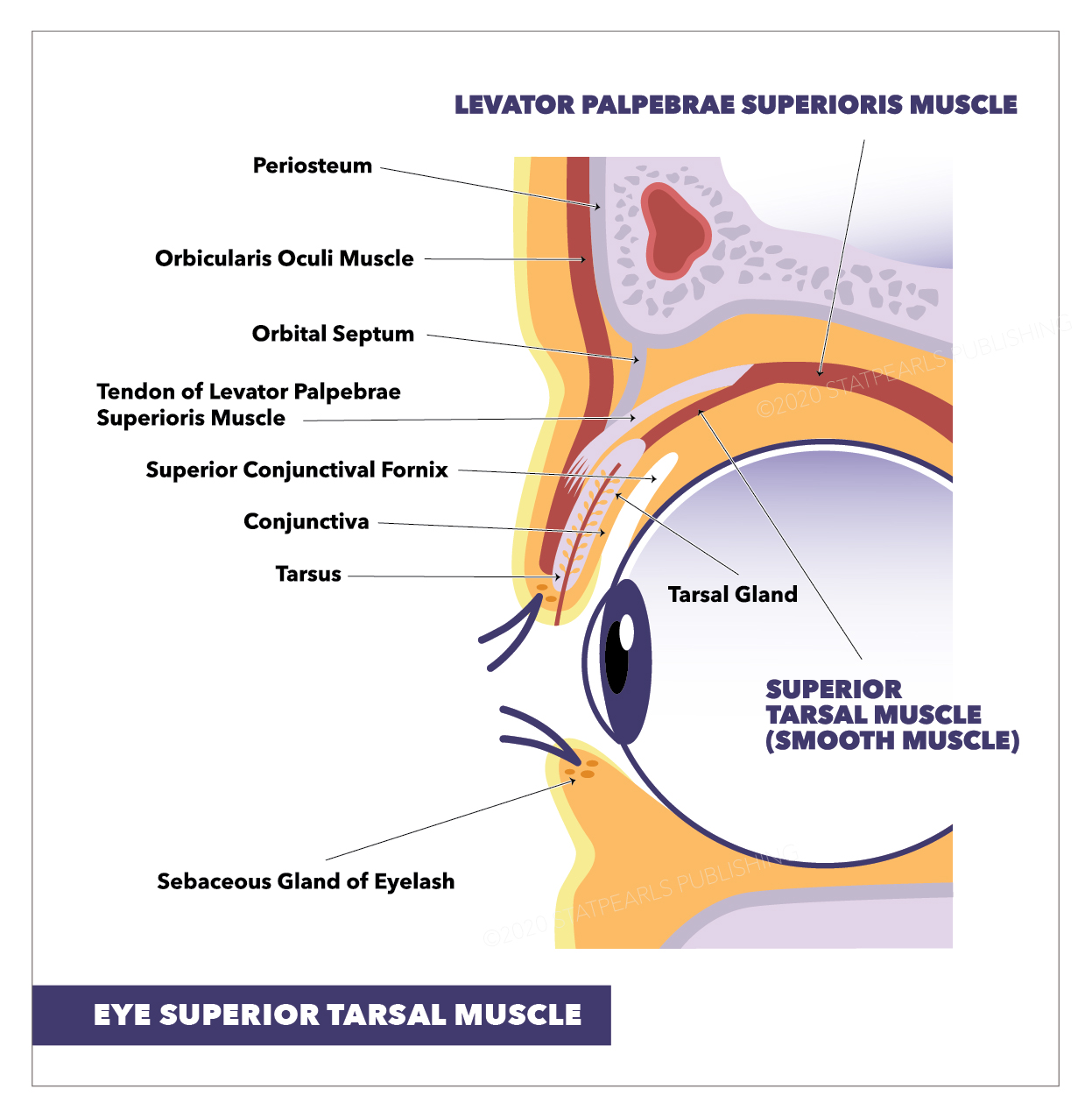
Eye—Superior Tarsal Muscle. The illustration shows the tarsal gland, levator palpebrae superioris muscle, sebaceous gland of an eyelash, tarsus, conjunctiva, superior conjunctival fornix, tendon of levator palpebrae superioris muscle, orbital septum, superior tarsal muscle (smooth muscle), orbicularis oculi muscle, and periosteum.
StatPearls Publishing Illustration
References
Koka K, Patel BC. Ptosis Correction. StatPearls. 2024 Jan:(): [PubMed PMID: 30969650]
Osaki TH, Monteiro LG, Osaki MH. Management of eyelid retraction related to thyroid eye disease. Taiwan journal of ophthalmology. 2022 Jan-Mar:12(1):12-21. doi: 10.4103/tjo.tjo_57_21. Epub 2022 Feb 14 [PubMed PMID: 35399960]
Kakizaki H, Madge SN, Selva D. Insertion of the levator aponeurosis and Müller's muscle on the tarsus: a cadaveric study in Caucasians. Clinical & experimental ophthalmology. 2010 Aug:38(6):635-7. doi: 10.1111/j.1442-9071.2010.02283.x. Epub 2010 Mar 2 [PubMed PMID: 20584021]
Putterman AM, Fett DR. Müller's muscle in the treatment of upper eyelid ptosis: a ten-year study. Ophthalmic surgery. 1986 Jun:17(6):354-60 [PubMed PMID: 3737107]
Beard C. Müller's superior tarsal muscle: anatomy, physiology, and clinical significance. Annals of plastic surgery. 1985 Apr:14(4):324-33 [PubMed PMID: 3994278]
Bang YH, Park SH, Kim JH, Cho JH, Lee CJ, Roh TS. The role of Müller's muscle reconsidered. Plastic and reconstructive surgery. 1998 Apr:101(5):1200-4 [PubMed PMID: 9529201]
Tawfik HA, Abdulhafez MH, Fouad YA, Dutton JJ. Embryologic and Fetal Development of the Human Eyelid. Ophthalmic plastic and reconstructive surgery. 2016 Nov/Dec:32(6):407-414 [PubMed PMID: 27124372]
Hayreh SS. THE OPHTHALMIC ARTERY: III. BRANCHES. The British journal of ophthalmology. 1962 Apr:46(4):212-47 [PubMed PMID: 18170772]
Pan E, Nie YF, Wang ZJ, Peng LX, Wu YH, Li Q. Aponeurosis of the levator palpebrae superioris in Chinese subjects: A live gross anatomy and cadaveric histological study. Medicine. 2016 Aug:95(31):e4469. doi: 10.1097/MD.0000000000004469. Epub [PubMed PMID: 27495084]
Esperidião-Antonio V, Conceição-Silva F, De-Ary-Pires B, Pires-Neto MA, de Ary-Pires R. The human superior tarsal muscle (Müller's muscle): a morphological classification with surgical correlations. Anatomical science international. 2010 Mar:85(1):1-7. doi: 10.1007/s12565-009-0043-0. Epub 2009 Apr 17 [PubMed PMID: 19373523]
Karam M, Alsaif A, Abul A, Alkhabbaz A, Alotaibi A, Shareef E, Behbehani R. Muller's muscle conjunctival resection versus external levator advancement for ptosis repair: systematic review and meta-analysis. International ophthalmology. 2023 Jul:43(7):2563-2573. doi: 10.1007/s10792-023-02633-1. Epub 2023 Jan 24 [PubMed PMID: 36692699]
Level 1 (high-level) evidenceAakalu VK, Setabutr P. Current ptosis management: a national survey of ASOPRS members. Ophthalmic plastic and reconstructive surgery. 2011 Jul-Aug:27(4):270-6. doi: 10.1097/IOP.0b013e31820ccce1. Epub [PubMed PMID: 21346664]
Level 3 (low-level) evidenceMartin TJ. Horner Syndrome: A Clinical Review. ACS chemical neuroscience. 2018 Feb 21:9(2):177-186. doi: 10.1021/acschemneuro.7b00405. Epub 2017 Dec 20 [PubMed PMID: 29260849]