Introduction
After a laparotomy, primary closure of the abdominal fascia is typically the preferred approach. However, situations may arise where complete fascial closure becomes unattainable, necessitating the surgeon to leave the abdomen open. This open abdomen poses a significant challenge and is associated with mortality rates exceeding 30%. Common scenarios leading to an open abdomen include peritonitis-induced bowel edema, abdominal compartment syndrome, and damage control surgery for trauma patients with intraabdominal bleeding. Temporary abdominal closure (TAC) techniques become imperative in such cases, aiming to provide a provisional solution until the abdominal fascia can be closed. Various TAC techniques are employed to address the challenges posed by the open abdomen. These techniques include negative pressure wound therapy, dynamic retention sutures, plastic silo (Bogotá bag), mesh/sheet, loose packing, skin approximation, and zipper. Each technique offers distinct advantages in maintaining tension on the fascial edges while accommodating varying clinical scenarios. Understanding and mastering these TAC techniques are critical for clinicians managing patients with an open abdomen, as failure to achieve delayed primary fascial closure puts patients at risk of developing ventral hernias with associated burdens and potential surgical complications. While the strategy for TAC or permanent abdominal closure should consider individual patient factors and risks, evidence-based comparative trials are lacking, highlighting the need for further research in this domain. The subsequent article explores TAC techniques' intricacies, mechanisms, applications, and potential complications.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
In an emergency laparotomy setting with a patient who is unstable, the surgeon may decide to temporarily close the abdomen to facilitate the resuscitation of the patient. The anatomy most relevant to temporary closure includes the following layers of the midline abdominal wall:
- Skin
- Subcutaneous tissue
- Superficial fascia
- The linea alba or midline of the rectus sheath (aponeuroses of the external oblique and internal oblique)
- Transversalis fascia
- Preperitoneal space
- Peritoneum
A key concept in temporary abdominal closure is to prevent the lateral retraction of the oblique musculature to preserve the ability to reapproximate the linea alba.
Indications
The indications for TAC encompass a spectrum of critical scenarios in surgical practice, mainly when primary fascial closure is unfeasible or counterproductive. The decision to leave the abdomen open can arise in the following situations:
- Severe abdominal infection
- Open management becomes necessary when a single laparotomy is insufficient to control the source of infection, as seen in cases of infected pancreatic necrosis or other necrotizing infections of the abdominal wall.
- Trauma and hemorrhage
- In instances of severe trauma, TAC may be employed as part of damage control surgery to control bleeding and contamination.
- Ischemic gut and second-look laparotomy
- Patients with ischemic bowel, requiring a mandatory "second look" operation to assess bowel viability, may have the abdomen left open; this allows for reassessment and potential resection of additional ischemic bowel segments.
- Abdominal compartment syndrome
- Decompressive laparotomy is crucial when increased intraabdominal pressure leads to abdominal compartment syndrome. Prophylactic decompressive laparotomy may also be considered in patients with acutely elevated intraabdominal pressures without acute organ dysfunction.
- Transplantation with size discrepancy
These indications underscore the pivotal role of TAC in addressing diverse challenges. TAC allows for effective management of an open abdomen until delayed primary fascial closure or alternative closure strategies are feasible. The decision to implement TAC depends on the specific clinical circumstances and the surgeon's assessment of the patient's stability and potential for further operative intervention.
Contraindications
While TAC is a valuable technique in various surgical scenarios, specific contraindications must be considered. Contraindications to TAC include:
- Improving patient condition
- If the patient stabilizes during the initial surgery, immediate primary fascial closure may be achievable, and TAC may not be needed.
- Controlled hemorrhage and contamination
- If bleeding and contamination are effectively controlled during the initial surgery, and there is no ongoing need for damage control, TAC may not be necessary.
- Significant risk of consequences
- Alternative closure methods should be considered in cases where TAC could worsen the patient's condition or lead to unintended consequences.
- Adequate tissue for primary closure
- TAC should be avoided when primary closure is feasible without compromising the patient's well-being.
- Absence of abdominal compartment syndrome or increased intraabdominal pressure
- If there is no evidence of abdominal compartment syndrome or significantly elevated intraabdominal pressure, the prophylactic use of TAC may not be warranted.
These contraindications emphasize the importance of individualized decision-making, considering the patient's specific clinical condition and the potential risks and benefits of using TAC. The decision should be based on a thorough assessment of the patient's stability, ongoing surgical needs, and the likelihood of achieving primary fascial closure.
Equipment
TAC requires specific equipment to manage an open abdomen effectively. The choice of equipment may vary based on the surgeon's preference, the clinical scenario, and the particular TAC technique employed.
Personnel
Performing TAC involves a collaborative effort, and the personnel required may vary based on the specific technique used and the clinical scenario. Here are key personnel typically involved in TAC:
- Surgeon
- Surgical assistant
- Scrub technician or scrub nurse
- Operating room nurses
- An anesthesiologist or nurse anesthetist
- Wound care specialist
- For specific TAC techniques (such as negative pressure wound therapy), a wound care specialist may be involved in applying and managing the vacuum system.
- Intensive care unit nurses for postoperative care
Technique or Treatment
When a decision is made to leave the abdomen open after surgery, the exposed area must be covered temporarily with a TAC. This process controls fluid loss and provides tension across the fascia so that it does not shrink or retract, a phenomenon called loss of domain. Over the past 30 years, surgical approaches to managing an open abdomen have significantly improved. The best method of TAC remains unclear, as no single method fits every clinical situation. The following are various techniques of TAC:
Simple Packing
This method involves placing nonadherent wet gauze or hydrophilic dressings directly on the abdominal contents without sutures, leaving the abdomen open for peritoneal drainage. Dressing changes and abdominal lavage were performed daily in the intensive care unit.
Skin-Only Closures
Temporary skin-only closure techniques utilize the skin to stabilize the abdominal wall while containing the abdominal viscera. These methods employ either a series of towel clips or a running monofilament suture. The towel clip closure stands are the fastest technique for temporary closure. The application involves placing towel clips on the skin approximately 1 cm apart, with the handles oriented towards the center, allowing for coverage by an adhesive plastic drape and minimizing artifact interference in subsequent radiographs (see Image. Skin-Only Closure). Whether using towel clips or suture closure, both methods are rapid, cost-effective, and readily accessible. However, due to the skin's relatively low bursting pressure, these techniques come with increased risks of complications such as evisceration, skin injury or loss, infection, and recurrent abdominal compartment syndrome. Other issues include the inability to check the abdominal contents, and if towel clips are used, artifacts in imaging (ie, chest x-rays) are unavoidable. Given the elevated complication rates, including abdominal compartment syndrome incidence ranging from 13% to 36%, these techniques have largely fallen out of favor in contemporary practice.[2]
Dynamic Retention Sutures
This is also known as an abdominal reapproximation anchor (ABRA®) and involves plastic tubes inserted through the abdominal wall away from the fascial edge and held with an adhesive button (see Image. ABRA® System). By pulling on the tubes on both sides of the defect, a staged approximation can be achieved. This placement of a temporary retention suture that could sequentially tighten the abdominal wall to minimize loss of domain in the open abdomen was first described more than 20 years ago.[3] The advantage is that it provides fascial tension while preserving the fascial edge for delayed primary closure. Furthermore, it is relatively easy to apply. The drawbacks are the costs, the possibility of abdominal compartment syndrome formation, and the increased risk of enteric fistula formation by tube pressure onto the bowel.
Silo Techniques
Silo techniques in TAC involve suturing a large, sterilized, translucent bag to the abdominal fascia or skin. A dialysate, irrigation, or intravenous (IV) bag can be used. The latter is more commonly known as a Bogotá bag, named after its observation in Bogotá, Colombia; it involves utilizing a pre-sterilized, soft 3 L IV bag that is cut to an oval shape and stapled with a standard skin stapling device or sutured with monofilament suture to the skin edges of the wound (see Image. Silo Technique). Sterile, antibiotic-soaked towels are placed over the silo, which is then covered with an iodine-impregnated adhesive plastic drape. The wound is inspected, and the dressing is changed every 24 hours. Despite its simplicity and low cost, this technique is time-consuming and poses challenges in controlling fluid losses. These potential challenges may require upsizing due to increased intraabdominal pressure, leading to operative replacement with a larger bag. While offering a cost-effective solution for containment when skin-only closure is impossible, it has limitations. The Bogotá bag does not prevent abdominal wall retraction or allow effective removal of abdominal fluids, necessitating a subsequent procedure for removal and definitive closure. Despite its drawbacks, the Bogotá bag technique has been associated with a wide range of primary closure rates (12% to 82%), low enteric fistula rates (0% to 14.4%), and considerable hospital morbidity, particularly in cases of intraabdominal sepsis, with a 39% primary fascial closure rate and a 12% in-hospital mortality rate reported in 1 study. Sixty percent of patients developed ventral hernias within a 48-month follow-up.[2]
Mesh
Repair materials in TAC for open abdomen management include absorbable and permanent synthetic options. Permanent synthetic prostheses, such as polypropylene and polytetrafluoroethylene mesh, offer protection to abdominal wall tissues, prevent lateral fascial retraction, and reduce incisional abdominal wall hernia incidence (see Image. Polypropylene Mesh Abdominal Closure and Image. Polytetrafluoroethylene Mesh Abdominal Closure). However, complications like wrinkling, infection, hernia, mesh extrusion, and enteric fistula may arise. These complications can also make reoperation more challenging. Absorbable meshes like polyglactin 910 and polyglycolic acid are resistant to infection and pliable, but their use in TAC may result in fistula formation and intraabdominal abscesses. The absorbable mesh forms a granulation tissue bed for skin grafting, while nonabsorbable meshes can be initially loosely sutured, allowing for visceral swelling prevention. Nonabsorbable meshes enhance primary closure rates of 33% to 89%. Careful consideration of material properties and potential complications is crucial in selecting an appropriate strategy for TAC.
Mesh bridging: Using a rapidly absorbable, biologic, or synthetic mesh placed as an interposition graft between the fascial edges has been described in the literature. In the setting of massive loss of domain, it may be the only technique to facilitate coverage of the intestines and facilitate granulation to allow skin grafting and later reconstruction.[4][5]
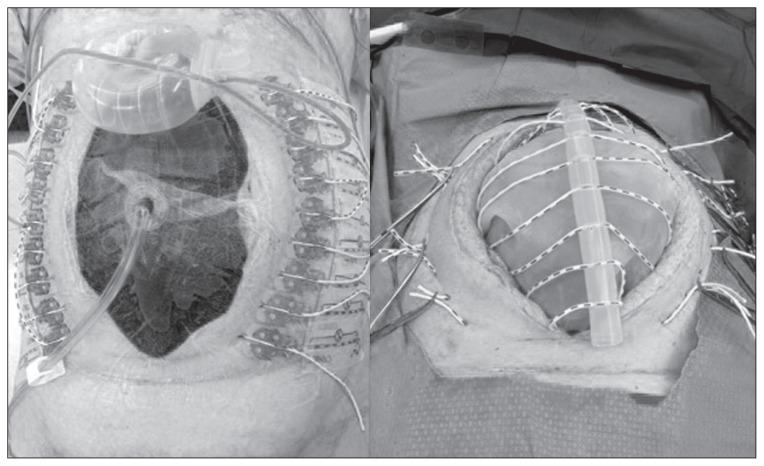
Mesh-mediated fascial traction is a technique where the mesh is sewn to the opposing fascial edges and sequentially tightens the anterior abdominal wall.[6] The most commonly known version is the Wittmann patch (see below). Various meshes have also been sewn in an underlay fashion, as well as an overlay on top of the fascia.[7][8][9] Additional benefits may come from combining this therapy with a fluid removal system such as the vacuum-based dressing (see Image. Vacuum-Assisted Mesh-Mediated Fascial Traction).
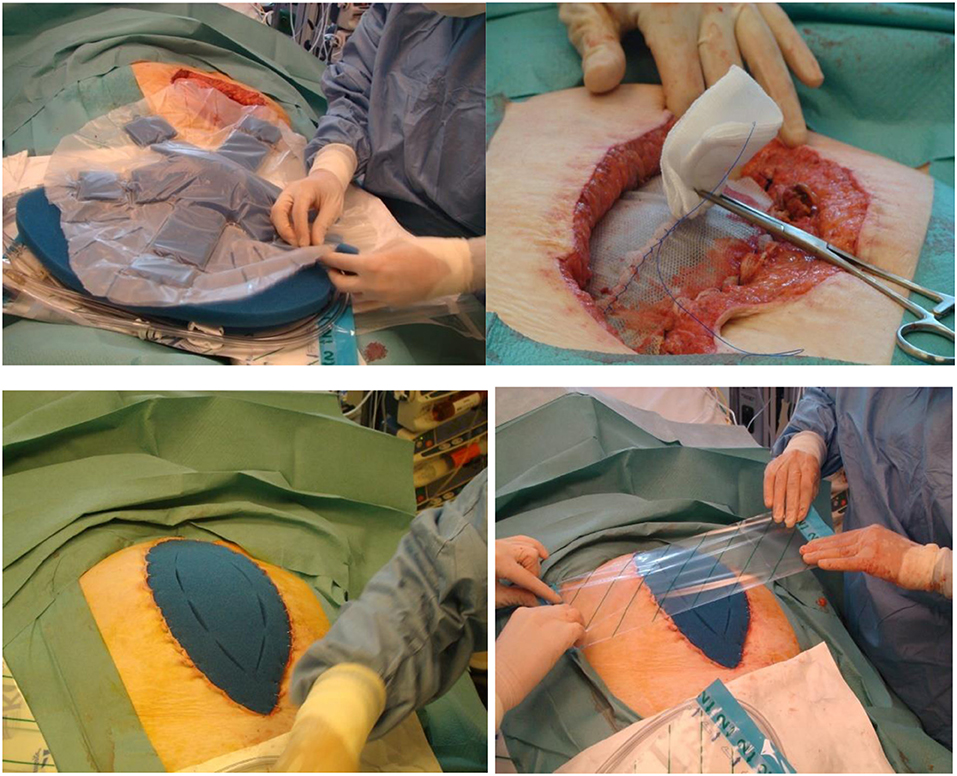
Wittmann Patch
The technique involves a detachable system where the Wittmann patch sheet is laterally sutured to the abdominal fascia, and closure at the midline is achieved with a velcro-like mechanism by tightening it every 24 to 48 hours until the fascia is approximately 2 to 4 cm apart (see Image. Wittmann Patch). The sheet is removed, and definitive closure is primarily used to close the fascia. This facilitates delayed fascial closure, showing a high success rate ranging from 78% to 100%. Despite its popularity, the Wittmann patch is more expensive (about $1440 per patient), requires suturing to the abdominal fascia, and may not effectively evacuate peritoneal fluid, presenting potential challenges in abdominal wound drainage.
Zipper
A mesh or sheet with a sterilized zipper is sutured between the fascial edges. This technique is comparable to the mesh technique and allows for easy access.
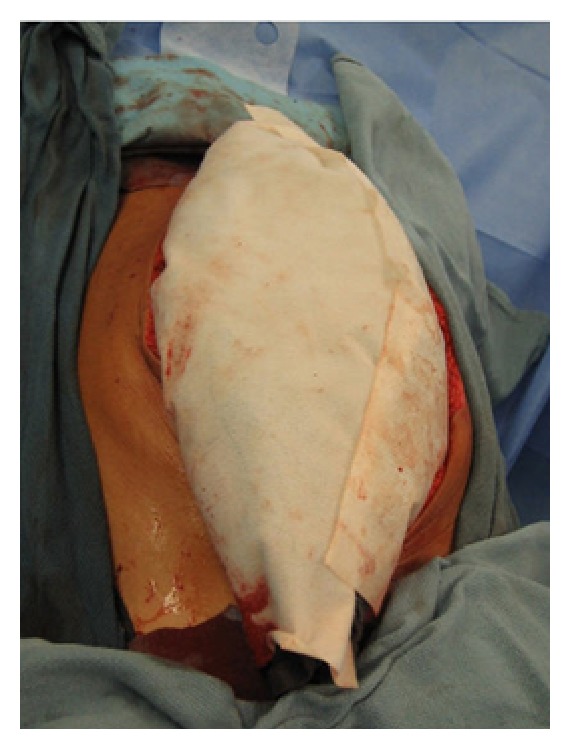
Negative Pressure Wound Therapies
Towel-based negative pressure wound therapies (NPWTs), also known as vacuum packs, were first described by Barker's group in 1995. This technique uses a surgical towel affixed to a polyethylene sheet strategically positioned between the anterior abdominal wall's viscera and the posterior aspect. Small slit perforations are cut in the elastic drape to facilitate fluid drainage from the abdomen. Drainage tubing, situated over the towel, is connected to a closed-suction drainage system, ensuring effective capture of the expelled fluid. Applying an outer adherent elastic layer adeptly covers the abdominal wall defect (see Image. Vacuum Pack Dressing). There are institution-specific variations as well.
The dressings associated with towel-based systems are known for their simplicity and cost-effectiveness. While proficient in controlling abdominal fluid, this system lacks comprehensive suction capabilities throughout the entire abdomen, potentially resulting in fluid accumulation within the abdominal cavity. Notwithstanding this limitation, the system demonstrates relative compliance, enabling it to accommodate mild increases in intraabdominal volume without inducing elevated intraabdominal pressure.
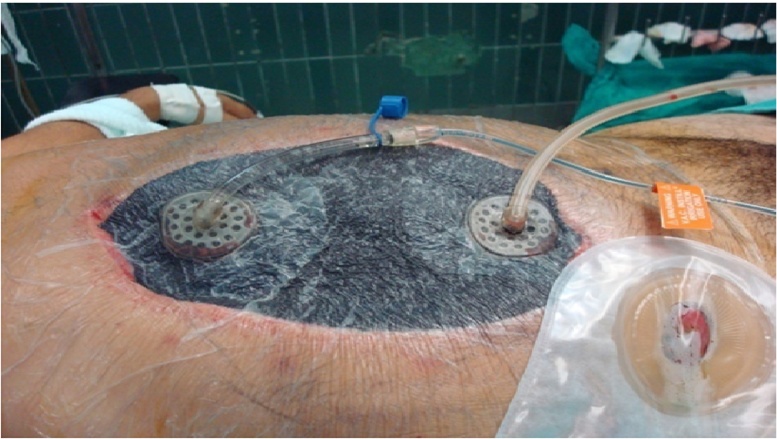
Sponge-based NPWTs use a perforated silastic sheet positioned between the bowel and abdominal wall, and a trimmed sponge is utilized to fill the subcutaneous abdominal defect. An outer self-adherent skin drape incorporates a suction port connected to a proprietary suction device. Although more expensive than the towel-based negative pressure system, the sponge-based approach provides more uniform suction throughout the peritoneal cavity. This approach may be more effective in preventing intraabdominal fluid accumulation.
NPWT remains preferable to simple silastic dressings such as the Bogotá bag to achieve fascial closure.[10] Numerous studies endorse these techniques, reporting high fascial closure rates, particularly with the AB-Thera®. Randomized controlled studies have demonstrated that dynamic therapy (ie, ABRA and MMFT) with NPWT is better for fascial closure than just NPWT alone (see Image. Dynamic Closure of Open Abdomen).[11] The studies comparing the different dynamic techniques are mostly retrospective observational studies. Most recently, an observational cohort study meta-analysis demonstrated 93% fascial closure with NPWT+ABRA versus 72% with NPWT+MMFT.[12]
In addition to increased fascial closure rates, another distinct advantage of this technique is the ability to allow for NPWT irrigation (NPWT-I), which has been suggested to help clear inflammatory cytokines in treating a septic cause for the open abdomen (see Image. VAC® Plus Instillation Assembly).[13][14] One review of 48 cases where NPWT-I was used showed added benefits compared to traditional methods such as the Bogotá bag, Wittmann patch, or NPWT alone in managing the open abdomen for severe abdominal sepsis. NPWT-I in patients with severe abdominal sepsis had promising results of higher fascia closure rates, lower mortality, and reduced hospital and intensive care unit length of stay with no complications attributed to this therapeutic approach.[15]
Commercially available sponge-based NPWT kits include:
- V.A.C.® Therapy (KCI (now part of 3M), San Antonio, Texas, USA)
- This comprises an inner plastic-encased sponge in direct contact with the viscera. This plastic interface shields the bowel, prevents adhesion formation, and is perforated to allow fluid passage. A macroporous "black" sponge is applied over the inner layer, in contact with the fascia, and can be secured with skin staples for approximation. This layer is then covered with an adhesive occlusive dressing, and a suction drainage device evacuates the superficial foam layer.
- AB-Thera® (ABThera system, KCI (now part of 3M), San Antonio, Texas, USA)
- This improvement on the system described above involves a large visceral protective layer with a polyurethane film-covered central foam structure. Six arms of polyurethane foam extend from the center to envelop the viscera, reaching into the paracolic gutters and draining fluid from various abdominal areas. This component, known as the "spider drape," is crucial in effective peritoneal fluid evacuation. Other system parts include an oval-shaped sponge that fits atop the exposed viscera, a large adhesive drape for an airtight seal, and a connecting pad allowing for negative suction (see Image. AB-Thera® and Suprasorb-CNP® Placements).
- Suprasorb-CNP® (Suprasorb CNP system, Lohmann & Rauscher, Austria-Germany)
- This system comes in an abdominal kit and works with closely spaced pores in a double-layer film placed around the viscera, shielding the intestine, liver surface, and pelvic cavity. The film was covered with polyurethane film-covered foam. In this system, however, a perforated silicon drainage tube was placed in this plane and connected with the suction pump, which served as the suction line. The subcutaneous space is then filled with rolled 6-inch gauze, and the skin around the wound is covered with a few layers of rolled gauze and then closed with the adhesive drape (see Image. AB-Thera® and Suprasorb-CNP® Placements).[16]
Proper utilization of negative pressure wound therapy is pivotal for successful abdominal closure, the prevention of enteric fistulas, and enhanced fluid removal from paracolic gutters. Ensuring the visceral protective layer envelops all visceral content without any foam contact is critical to achieving optimal results. The foam should be placed beneath the abdominal wall, atop the protective layer, to provide medial tension and closure while applying negative pressure through the foam. This method effectively minimizes fascial retraction and prevents loss of domain. In cases of compartment syndrome, use only a minimal strip of foam, or enough to cover the gap, on the incision to deliver negative pressure to the larger foam beneath the abdominal wall. The wound foam must be thicker than the subcutaneous layer.
Additionally, cutting the drape into strips aids in providing traction on the skin, facilitating the closure of the abdominal wall. To accomplish this, begin with 1 side of the strip and apply it to the skin, and then pull the other half to hold the wound together securely. Avoid the common error of having a tiny protective layer atop the viscera with a large foam opening, as this may inadvertently exacerbate the wound instead of achieving the intended temporary closure. Always follow these guidelines carefully to optimize the effectiveness of NPWT.
Facilitation of Fascial Closure
Hypertonic saline resuscitation: A protocol developed using hypertonic saline for resuscitation and NPWT has had improved success in early fascial closure in damage control laparotomy patients.[17][18]
Botulinum toxin A: This has been used as a method of chemical paralysis of the strong opposing forces of the lateral abdominal wall musculature used in complex abdominal wall reconstruction. One study by Zielinski et al described using this technique in the open abdomen to facilitate primary fascial closure.[19][20]
Complications
TAC is an important intervention in specific clinical scenarios, but like any medical procedure, it carries potential complications. The complications can vary based on the technique used and the patient's underlying condition. Here are some possible complications associated with TAC:
- Infection
- The risk of surgical site infection is present with any abdominal surgery, including TAC. One study showed an increase in fungal intraabdominal infections in postoperative trauma patients for whom TAC is being utilized.[21]
- Delayed primary fascial closure
- The primary goal after TAC is achieving delayed primary fascial closure. However, achieving primary closure may be challenging due to persistent inflammation, infection, or extensive tissue damage.
- Enteric fistula formation
- When dealing with bowel injuries or inflammatory conditions, there is a risk of abnormal connections forming between the bowel and other structures, leading to enteric fistula formation. Enteric fistulas are notoriously difficult to manage because the enteric succus flows through the wound area, making it hard for the wound to heal. The output of the fistula may be thin with high levels of biliopancreatic content if it's proximal in the intestines or thick, brown, and highly contaminated with gut bacteria if it's distal. Each type of fistula output presents its challenges.
- A common misconception is that NPWT is associated with fistula formation when, in fact, enteric fistula is lower in NPWT than other abdominal packing strategies.[11]
- Bleeding
- Hemorrhage can occur during or after the TAC procedure. Adequate hemostasis during the initial surgery and vigilant postoperative monitoring are crucial to prevent and address bleeding.
- Wound dehiscence
- The wound may reopen, especially if there's increased intraabdominal pressure, compromised wound healing, or the patient cannot tolerate abdominal closure.
- Hernia formation
- In cases where the abdominal wall cannot be closed primarily, there is a risk of hernia formation, either planned (intentional, as in some cases) or unplanned.
- Early closure within 10 to 14 days is the easiest way to prevent hernia. Few studies follow the long-term development of hernias after an open abdomen, but the incidence has been reported to be as high as 21% at 2 years and >50% at 5 years.[22] Whether component separation techniques should be used in the open abdomen to achieve fascial closure initially remains controversial, as hernias still develop about 20% of the time. Also, the fascial planes are distorted for more complex abdominal wall reconstruction later by doing component separation.
- Adhesion formation
- Adhesions between intraabdominal organs and the abdominal wall may develop, potentially causing complications during subsequent surgeries.
- Abdominal compartment syndrome
- In some cases, the TAC procedure itself or underlying conditions may contribute to abdominal compartment syndrome, causing increased intraabdominal pressure and compromising organ perfusion.
- Pain
- The patient may experience pain and discomfort associated with the open abdomen and the TAC devices. Pain management is an essential aspect of postoperative care.
- Complications related to specific techniques
- Different TAC techniques (eg, vacuum-assisted closure and mesh placement) have unique complications. For example, issues like device malfunction, skin necrosis, or adhesion formation may be associated with specific methods.
- Complications related to prolonged open abdomen
- Prolonged open abdomen may lead to physiological derangements, including fluid and electrolyte imbalances, respiratory compromise, and challenges in maintaining the abdominal domain.
Healthcare providers must be vigilant, closely monitor patients, and promptly address complications to optimize outcomes following TAC. The choice of TAC technique, timing, and ongoing patient management contribute to the overall success and prevention of complications.
Clinical Significance
The clinical significance of TAC lies in its pivotal role in managing a spectrum of critical abdominal conditions, ranging from trauma and vascular emergencies to severe infections and complications of abdominal surgery. TAC is a strategic approach to controlling hemorrhage, preventing contamination, and alleviating abdominal compartment syndrome by providing a staged and controlled environment for surgical interventions. In severe infections, such as infected pancreatic necrosis or peritonitis, TAC allows for repeated access, debridement, and drainage, promoting effective source control. Additionally, TAC facilitates damage control surgery, enabling a staged approach in trauma scenarios to address immediate life-threatening issues before definitive closure. The technique is particularly valuable in managing ischemic bowel conditions, offering a "second-look" option to assess bowel viability and prevent unnecessary extensive resection. Overall, TAC is critical in optimizing patient outcomes, enhancing survival rates, and providing a tailored approach to complex abdominal pathologies.
Enhancing Healthcare Team Outcomes
Effective TAC management requires a collaborative and interprofessional approach involving physicians, advanced practitioners, nurses, and pharmacists. Physicians, particularly surgeons, play a pivotal role in decision-making regarding the timing and type of TAC, considering factors such as the patient's physiologic state and the underlying condition necessitating abdominal closure. Advanced practitioners, such as physician assistants and nurse practitioners, contribute by assessing patients, monitoring their response to treatment, and ensuring timely interventions. Nurses are crucial for day-to-day patient care, including wound management, infection control, and monitoring vital signs. Pharmacists are essential in medication management, ensuring appropriate antibiotic therapy, pain control, and addressing potential drug interactions.
Interprofessional communication is paramount for the cohesive functioning of the healthcare team. Regular and clear communication between team members helps ensure everyone is on the same page regarding the patient's condition, treatment plan, and any changes in care. Care coordination involves synchronizing efforts among professionals to provide seamless, patient-centered care. This includes scheduling procedures, managing follow-up appointments, and ensuring the patient receives comprehensive care. Healthcare professionals can improve outcomes, prioritize patient safety, and optimize team performance in TAC by fostering effective teamwork, open communication, and coordinated efforts.
Media
(Click Image to Enlarge)
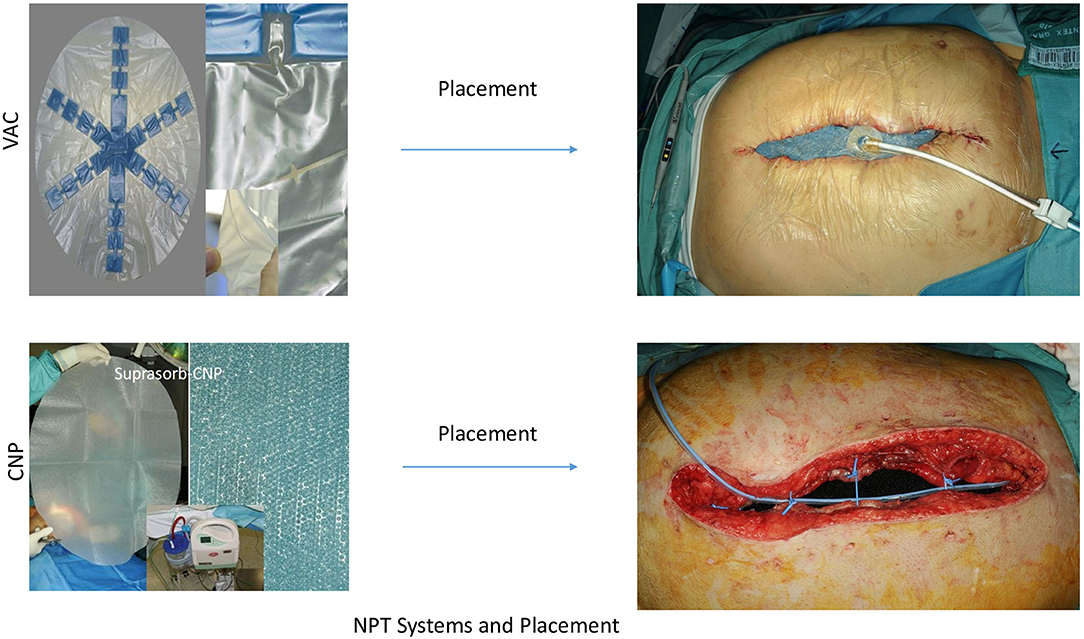
AB-Thera® and Suprasorb-CNP® Placements. These negative pressure wound-therapy systems are available for temporary abdominal closure.
Contributed by Frontiers in Surgery.
(Click Image to Enlarge)
Vacuum-Assisted Mesh-Mediated Fascial Traction. This dynamic therapy is used for temporary closure of the abdomen.
Contributed by Frontiers in Surgery.
(Click Image to Enlarge)

Polypropylene Mesh Abdominal Closure. Polypropylene mesh is sutured to the fascial edges with a running suture to temporarily close the abdomen.
Huang Q, Li J. Techniques for abdominal wall closure after damage control laparotomy: from temporary abdominal closure to early/delayed fascial closure—a review. Gastroenterol Res Pract. 2016:2016:2073260. doi: 10.1155/2016/2073260.
(Click Image to Enlarge)

Polytetrafluoroethylene Mesh Abdominal Closure. Polytetrafluoroethylene mesh is sutured to the fascial edges to temporarily close the abdomen.
Huang Q, Li J. Techniques for abdominal wall closure after damage control laparotomy: from temporary abdominal closure to early/delayed fascial closure—a review. Gastroenterol Res Pract. 2016:2016:2073260. doi: 10.1155/2016/2073260.
(Click Image to Enlarge)

Skin-Only Closure. Towel clips are placed into the skin to close the abdomen temporarily.
Huang Q, Li J. Techniques for abdominal wall closure after damage control laparotomy: from temporary abdominal closure to early/delayed fascial closure—a review. Gastroenterol Res Pract. 2016:2016:2073260. doi: 10.1155/2016/2073260.
(Click Image to Enlarge)
(Click Image to Enlarge)
Wittmann Patch. Two sheets of Wittmann Patch, which adhere to each other, are used to close the abdomen temporarily.
Huang Q, Li J. Techniques for abdominal wall closure after damage control laparotomy: from temporary abdominal closure to early/delayed fascial closure—a review. Gastroenterol Res Pract. 2016:2016:2073260. doi: 10.1155/2016/2073260.
(Click Image to Enlarge)
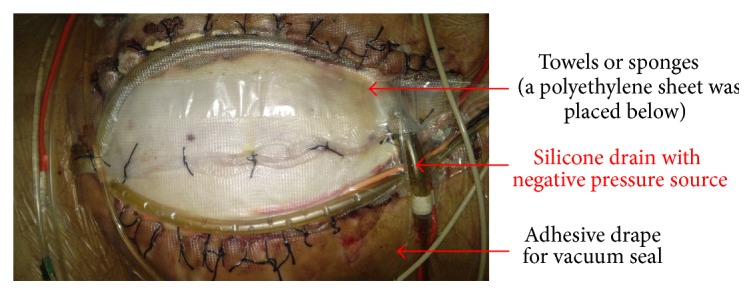
Vacuum Pack Dressing. The component layers of the vacuum pack dressing that are used in temporary abdominal closure.
Huang Q, Li J. Techniques for abdominal wall closure after damage control laparotomy: from temporary abdominal closure to early/delayed fascial closure—a review. Gastroenterol Res Pract. 2016:2016:2073260. doi: 10.1155/2016/2073260.
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
VAC® Plus Instillation Assembly. The instillation line is on the left, and the retrieval line is on the right, both overlying the foam dressing.
Sibaja P, Sanchez A, Villegas G, Apestegui A, Mora E. Management of the open abdomen using negative pressure wound therapy with instillation in severe abdominal sepsis: a review of 48 cases in Hospital Mexico, Costa Rica. Int J Surg Case Rep. 2017;30:26-30. doi: 10.1016/j.ijscr.2016.11.024.
References
Cheng Y, Wang K, Gong J, Liu Z, Gong J, Zeng Z, Wang X. Negative pressure wound therapy for managing the open abdomen in non-trauma patients. The Cochrane database of systematic reviews. 2022 May 6:5(5):CD013710. doi: 10.1002/14651858.CD013710.pub2. Epub 2022 May 6 [PubMed PMID: 35514120]
Level 1 (high-level) evidenceHuang Q, Li J, Lau WY. Techniques for Abdominal Wall Closure after Damage Control Laparotomy: From Temporary Abdominal Closure to Early/Delayed Fascial Closure-A Review. Gastroenterology research and practice. 2016:2016():2073260. doi: 10.1155/2016/2073260. Epub 2015 Dec 27 [PubMed PMID: 26819597]
Koniaris LG, Hendrickson RJ, Drugas G, Abt P, Schoeniger LO. Dynamic retention: a technique for closure of the complex abdomen in critically ill patients. Archives of surgery (Chicago, Ill. : 1960). 2001 Dec:136(12):1359-62; discussion 1363 [PubMed PMID: 11735859]
Como JJ, Gunter OL, Diaz JJ, Ho VP, Miller PR. Use of posterior component separation and transversus abdominis release in trauma and emergency general surgery patients: a case report and review of the literature. Trauma surgery & acute care open. 2019:4(1):e000268. doi: 10.1136/tsaco-2018-000268. Epub 2019 Jan 24 [PubMed PMID: 30793037]
Level 3 (low-level) evidencePetro CC, Como JJ, Yee S, Prabhu AS, Novitsky YW, Rosen MJ. Posterior component separation and transversus abdominis muscle release for complex incisional hernia repair in patients with a history of an open abdomen. The journal of trauma and acute care surgery. 2015 Feb:78(2):422-9. doi: 10.1097/TA.0000000000000495. Epub [PubMed PMID: 25757132]
Petersson U, Acosta S, Björck M. Vacuum-assisted wound closure and mesh-mediated fascial traction--a novel technique for late closure of the open abdomen. World journal of surgery. 2007 Nov:31(11):2133-7 [PubMed PMID: 17879112]
Villalobos Mori R, Maestre González Y, Mias Carballal M, Gas Ruiz C, Protti Ruiz G, Escartin Arias A, Olsina Kissler JJ. Novel method for delayed primary closure and incisional hernia prevention in open abdomen: COmbined and MOdified Definitive Abdominal wall closure (COMODA). Hernia : the journal of hernias and abdominal wall surgery. 2020 Apr:24(2):395-401. doi: 10.1007/s10029-019-01948-2. Epub 2019 Apr 9 [PubMed PMID: 30968285]
Salamone G, Licari L, Guercio G, Comelli A, Mangiapane M, Falco N, Tutino R, Bagarella N, Campanella S, Porrello C, Gullo R, Cocorullo G, Gulotta G. Vacuum-Assisted Wound Closure with Mesh-Mediated Fascial Traction Achieves Better Outcomes than Vacuum-Assisted Wound Closure Alone: A Comparative Study. World journal of surgery. 2018 Jun:42(6):1679-1686. doi: 10.1007/s00268-017-4354-3. Epub [PubMed PMID: 29147897]
Level 2 (mid-level) evidencePetersson P, Montgomery A, Petersson U. Vacuum-Assisted Wound Closure and Permanent Onlay Mesh-Mediated Fascial Traction: A Novel Technique for the Prevention of Incisional Hernia after Open Abdomen Therapy Including Results From a Retrospective Case Series. Scandinavian journal of surgery : SJS : official organ for the Finnish Surgical Society and the Scandinavian Surgical Society. 2019 Sep:108(3):216-226. doi: 10.1177/1457496918818979. Epub 2018 Dec 21 [PubMed PMID: 30574843]
Level 2 (mid-level) evidenceHu P, Uhlich R, Gleason F, Kerby J, Bosarge P. Impact of initial temporary abdominal closure in damage control surgery: a retrospective analysis. World journal of emergency surgery : WJES. 2018:13():43. doi: 10.1186/s13017-018-0204-3. Epub 2018 Sep 15 [PubMed PMID: 30237824]
Level 2 (mid-level) evidenceCristaudo A, Jennings S, Gunnarsson R, DeCosta A. Complications and Mortality Associated with Temporary Abdominal Closure Techniques: A Systematic Review and Meta-Analysis. The American surgeon. 2017 Feb 1:83(2):191-216 [PubMed PMID: 28228207]
Level 1 (high-level) evidencePoortmans N, Berrevoet F. Dynamic closure techniques for treatment of an open abdomen: an update. Hernia : the journal of hernias and abdominal wall surgery. 2020 Apr:24(2):325-331. doi: 10.1007/s10029-020-02130-9. Epub 2020 Feb 5 [PubMed PMID: 32020342]
Turza KC, Campbell CA, Rosenberger LH, Politano AD, Davies SW, Riccio LM, Sawyer RG. Options for closure of the infected abdomen. Surgical infections. 2012 Dec:13(6):343-51. doi: 10.1089/sur.2012.014. Epub 2012 Dec 10 [PubMed PMID: 23216525]
Shah SK, Jimenez F, Letourneau PA, Walker PA, Moore-Olufemi SD, Stewart RH, Laine GA, Cox CS Jr. Strategies for modulating the inflammatory response after decompression from abdominal compartment syndrome. Scandinavian journal of trauma, resuscitation and emergency medicine. 2012 Apr 3:20():25. doi: 10.1186/1757-7241-20-25. Epub 2012 Apr 3 [PubMed PMID: 22472164]
Sibaja P, Sanchez A, Villegas G, Apestegui A, Mora E. Management of the open abdomen using negative pressure wound therapy with instillation in severe abdominal sepsis: A review of 48 cases in Hospital Mexico, Costa Rica. International journal of surgery case reports. 2017:30():26-30. doi: 10.1016/j.ijscr.2016.11.024. Epub 2016 Nov 17 [PubMed PMID: 27898352]
Level 3 (low-level) evidenceHeo Y, Kim DH. The temporary abdominal closure techniques used for trauma patients: a systematic review and meta-analysis. Annals of surgical treatment and research. 2023 Apr:104(4):237-247. doi: 10.4174/astr.2023.104.4.237. Epub 2023 Mar 31 [PubMed PMID: 37051156]
Level 1 (high-level) evidenceLoftus TJ, Efron PA, Bala TM, Rosenthal MD, Croft CA, Smith RS, Moore FA, Mohr AM, Brakenridge SC. Hypertonic saline resuscitation after emergent laparotomy and temporary abdominal closure. The journal of trauma and acute care surgery. 2018 Feb:84(2):350-357. doi: 10.1097/TA.0000000000001730. Epub [PubMed PMID: 29140948]
Loftus TJ, Efron PA, Bala TM, Rosenthal MD, Croft CA, Walters MS, Smith RS, Moore FA, Mohr AM, Brakenridge SC. The impact of standardized protocol implementation for surgical damage control and temporary abdominal closure after emergent laparotomy. The journal of trauma and acute care surgery. 2019 Apr:86(4):670-678. doi: 10.1097/TA.0000000000002170. Epub [PubMed PMID: 30562327]
Zendejas B, Khasawneh MA, Srvantstyan B, Jenkins DH, Schiller HJ, Zielinski MD. Outcomes of chemical component paralysis using botulinum toxin for incisional hernia repairs. World journal of surgery. 2013 Dec:37(12):2830-7. doi: 10.1007/s00268-013-2211-6. Epub [PubMed PMID: 24081529]
Zielinski MD, Goussous N, Schiller HJ, Jenkins D. Chemical components separation with botulinum toxin A: a novel technique to improve primary fascial closure rates of the open abdomen. Hernia : the journal of hernias and abdominal wall surgery. 2013 Feb:17(1):101-7. doi: 10.1007/s10029-012-0995-1. Epub 2012 Sep 22 [PubMed PMID: 23001400]
Level 2 (mid-level) evidenceZhang CX, Rasane RR, Zhang Q, Fonseca RA, Aldana JA, Rincon JE, Sorini MJ, Bochicchio KM, Leonard JM, Ilahi ON, Bochicchio GV. Temporary Abdominal Closure Is Associated with Increased Risk for Fungal Intra-Abdominal Infections in Trauma Patients. Surgical infections. 2020 Nov:21(9):745-751. doi: 10.1089/sur.2019.286. Epub 2020 Mar 18 [PubMed PMID: 32186973]
Berrevoet F. Prevention of Incisional Hernias after Open Abdomen Treatment. Frontiers in surgery. 2018:5():11. doi: 10.3389/fsurg.2018.00011. Epub 2018 Feb 26 [PubMed PMID: 29536013]