EMS Pneumothorax Identification Without Ancillary Testing
EMS Pneumothorax Identification Without Ancillary Testing
Introduction
Prehospital providers are responsible for identifying and treating various conditions that may need rapid intervention. Pneumothorax is one potentially life-threatening condition that may be quickly identified with high-quality physical examination skills. The condition develops when air accumulates in the pleural space, causing partial or complete lung collapse. Continuous air accumulation can increase intrathoracic pressure. Tension pneumothorax arises when intrathoracic air pressure is high enough to shift mediastinal contents contralaterally. Up to 1 in 20 major trauma patients develop tension pneumothorax.[1] Treating pneumothorax can be relatively simple, though complications like cardiac or major blood vessel injury can occur.[2]
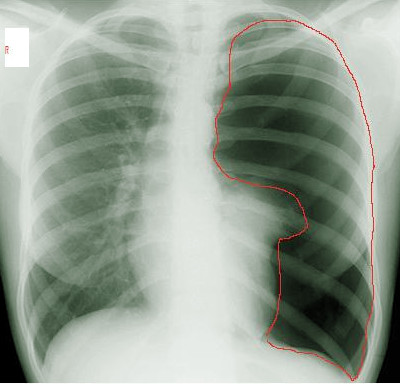
Identifying this condition in the prehospital setting is challenging. Unlike the resource-rich emergency department, prehospital providers cannot rely on imaging studies or thoracic surgery consultation when evaluating individuals with a possible pneumothorax (see Image. Left Pneumothorax on X-ray). Additionally, comorbid conditions like chronic obstructive pulmonary disease (COPD), asthma, congestive heart failure, and pleural effusion can mimic a pneumothorax clinically. Understanding the nuances in the clinical presentation of this condition can improve prehospital diagnostic accuracy and time to initial intervention.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
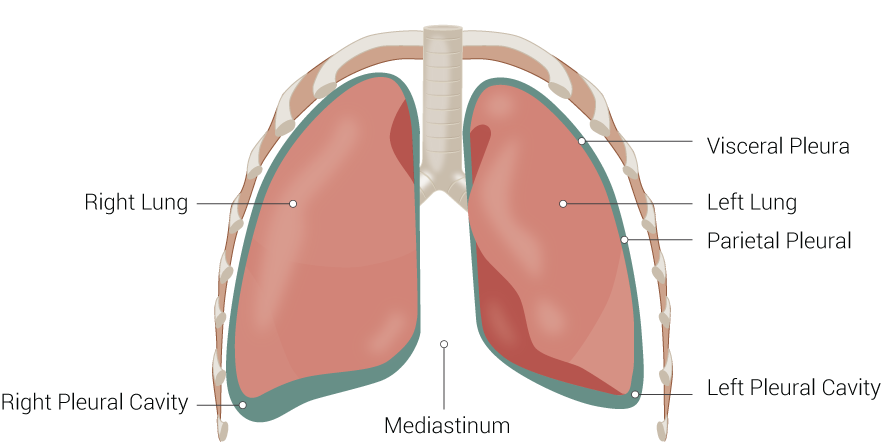
In healthy patients, the pleurae are impermeable membranes acting as a barrier between the lungs and chest wall (see Image. Lung Anatomy). The visceral pleura is directly in contact with the lung parenchyma, while the parietal pleura lines the inner chest wall surface. These 2 membranes are continuous with each other. Normally, negative pressure between the 2 pleurae keeps them closely apposed, so chest wall expansion inflates the lungs. The pleural cavity is a potential space that can form between the pleurae when the pressure between them increases, as when air or fluid accumulates between the lung and thoracic cavity.[3]
Pneumothorax results from air accumulating in the pleural space. The condition is often due to trauma, though it can also occur spontaneously. Spontaneous pneumothorax can be due to the rupture of a bleb or weakness in the pleural tissue, iatrogenic injury, or complication from barometric changes. Conditions like COPD, interstitial lung disease, cystic fibrosis, and Marfan syndrome predispose patients to spontaneous pneumothorax.[4]
Traumatic pneumothorax may result from blunt and penetrating chest injuries and should be considered in blast or concussive injuries.[5] Hypoxia arises due to the collapsed lung's inability to absorb oxygen from ambient air. Tension pneumothorax develops when intrathoracic pressure is high enough to cause a contralateral mediastinal shift. Elevated pressure against the mediastinum can compress the great blood vessels and heart, compromising venous return and cardiac output.
Tension pneumothorax is a medical emergency. The treatment involves releasing the trapped air to restore negative pressure within the pleural space and facilitate lung reinflation. Providers should be comfortable with the standard approach to tension pneumothorax needle decompression and be aware of the procedure's potential complications and contraindications.
Indications
Patients presenting with a traumatic pneumothorax have been traditionally managed in-hospital with thoracostomy tube placement using a small 'pig tail' catheter or larger-bore 28-36 French devices. Many of these thoracostomy procedures were performed in the trauma bay with prehospital providers observing, which may lead many to believe that all traumatic pneumothoraces require intervention.
However, studies show that most pneumothorax cases do not warrant treatment, and monitoring by serial computed tomography (CT) imaging is usually sufficient.[6][7][8] Judicious assessment enables providers to determine if treatment is required in the prehospital setting. Inappropriate patient selection may result in unneeded further surgical management and hospitalization. When patients are selected appropriately, prehospital needle decompression is associated with lower 24-hour mortality among trauma patients.[9]
Individuals with a pneumothorax and who are in extremis or may decompensate in the prehospital setting should be treated with needle decompression. The most common symptoms are breathlessness and unilateral chest pain. On physical examination, patients may be tachycardic, though the vital signs may remain normal until significant pressure accumulates within the chest cavity.
Decreased or absent breath sounds are typically appreciated on the affected side. Other findings may include subcutaneous emphysema from air permeating the soft tissues and jugular venous distension. Hypoxia and hypotension may manifest if the condition is not appropriately managed promptly. Some sources recommend aggressive prehospital treatment of suspected pneumothorax based on mechanism and degree of respiratory distress.[10] Ideally, needle decompression should be reserved for those who show signs of shock, hypotension, poor perfusion, respiratory distress, or altered mental status.
Patients with a suspected pneumothorax that may have resulted from positive pressure ventilation should be strongly considered for needle decompression.
Contraindications
Needle decompression may be contraindicated in specific sites due to burns, infection, or body habitus. Stable patients should be monitored closely, though needle decompression should be considered if cardiorespiratory distress worsens. Refraining from unneeded intervention limits unnecessary hospitalizations and additional procedures.
Equipment
Catheter Selection
Most literature recommends a 14-gauge 3.25-inch catheter for needle decompression in adults.[11] CT imaging measurements show many patients likely have chest wall soft tissue thicker than the recommended needle length, making larger gauge devices of the same length appropriate. Lateral chest catheter insertion is favored over the anterior approach, as the lateral chest region typically has less soft tissue than the anterior chest. Colorimetric capnography devices and one-way valves may be used to assess placement.[12] A standard intravenous catheter-style device is usually more cost-effective and sufficient.
Point-of-Care Ultrasound
The feasibility and effectiveness of prehospital point-of-care ultrasound (POCUS) have been well-reviewed in the literature. A key to successfully using POCUS for pneumothorax is a structured training program that includes supervised examinations and image review.[13][14][15]
The provider applies a handheld ultrasound device to identify the normal pleural movement during cardiac contraction or breathing, known as lung sliding (see Image. Normal Lung Ultrasound).[16] Patients with a pneumothorax will not demonstrate lung sliding.
Several views can be obtained for each lung, allowing for a rough pneumothorax size estimation. Depending on user skill, POCUS pulmonary assessment can be more sensitive than a chest x-ray (see Image. Lung Ultrasound M-Mode).[17] Ultrasound can help identify patients who may require needle decompression, document evidence of pneumothorax, and confirm lung reinflation.[18] As portable ultrasound devices become more common in EMS, providers should be familiar with basic lung assessment using POCUS.
Technique or Treatment
If a pneumothorax is suspected, the airway, breathing, and circulation should be secured according to standard EMS protocol. High-flow oxygen must be administered to symptomatic patients to create a nitrogen gas pressure gradient that will help reabsorb some of the intrapleural air.[19][20][21][22] Patients with minimal symptoms likely do not need high-flow oxygen therapy. Open chest wounds should be covered with a sealable dressing with a one-way air valve to prevent buildup. This one-way valve may be created by applying an occlusive dressing and taping on 3 sides.[23] This 'vented' chest seal is superior to nonvented models because it prevents tension physiology.[24]
Providers should initiate further management if the patient shows signs of hypoperfusion or is at risk for decompensation. Needle decompression should be performed with an anterior or lateral approach. The anterior approach enters the midclavicular line in the 2nd or 3rd intercostal space. However, this location may have more soft tissue than the lateral region or be unavailable for needle insertion. A lateral approach is recommended as an alternative, performed at the anterior axillary line along the 4th or 5th intercostal space.
Inserting a 14-gauge or 10-gauge catheter above the rib is preferable to placement at the inferior edge, where neurovascular structures are situated and thus more likely to get injured.
The needle and catheter should be placed for 5 to 10 seconds before removal and subsequent disposal. Successful decompression is signified by a hiss of escaping air, improved respiratory status, and vital signs improvement. The catheter should remain in place during transport. Some facilities recommend the placement of a one-way valve over the catheter, similar to an open chest wound.
Decompression may also be performed on children. A 22-gauge catheter is appropriate for very young children, while an 18-gauge catheter is recommended for older children. Most pediatric patients can be managed with a standard 3.175 cm intravenous catheter.[25]
Complications
Lung auscultation must be performed after needle decompression to reassess the patient. Needle decompression is only a temporizing measure. Chest tube placement is still necessary upon arrival at the emergency department. Possible treatment complications include worsening pneumothorax, bleeding, infection, and lung parenchymal damage.
Most prehospital providers are confident in their ability to perform needle decompression. However, a study found that only approximately one-third of prehospital decompression catheters are correctly placed within the pleural cavity, and up to 20% of procedures are not medically indicated. Incorrectly placed needles may damage surrounding vasculature or solid organs, including the heart.
Individuals with a simple, spontaneous pneumothorax who were simply provided oxygen treatment must be observed for 3 to 6 hours. Longer observation periods are warranted for patients with more complex pneumothoraces. Recurrence may occur after pneumothorax treatment, especially at high altitudes or deep sea. Therefore, patients must be advised to avoid air travel or diving for 7 to 14 days after treatment.[26]
Clinical Significance
Pneumothorax is air accumulation in the pleural space. Signs and symptoms of simple pneumothorax include acute-onset chest pain, dyspnea, hypoxia, tachycardia, decreased unilateral breath sounds, and hyperresonance of the affected side to percussion. This condition can evolve into tension pneumothorax, manifesting with similar symptoms, but may also present with hypotension, hypoperfusion, jugular venous distention, and contralateral tracheal deviation.
Needle decompression may be performed in the prehospital setting if tension pneumothorax is suspected. The treatment can maintain cardiac output initially but is only a temporizing measure. The definitive treatment for pneumothorax is chest tube placement performed in the emergency department.
Enhancing Healthcare Team Outcomes
Pneumothorax management is best approached interprofessionally. The members of this team include the following:
- EMS personnel: providers who are often the first responders, crucial in recognizing potential pneumothorax in the prehospital setting and providing initial treatment.
- Emergency physicians: responsible for confirming the diagnosis of pneumothorax, often using ancillary imaging modalities such as chest x-rays or CT. Emergency physicians may perform chest tube insertion and initiate referrals to surgeons and pulmonologists for co-management.
- Radiologists: interpret imaging studies, provide detailed assessments of pneumothorax severity, and offer insights into potential complications.
- Pulmonologists: provide treatment for the underlying medical causes of pneumothorax.
- Respiratory therapists: assist in managing patients' respiratory status, ensuring adequate oxygenation, and collaborating with the team in implementing appropriate ventilatory support if necessary.
- General or thoracic surgeons: may provide expertise in surgical repair of persistent or recurrent pneumothoraces.
- Nurses: play a critical role in continuous patient monitoring, administering medications, and providing supportive care.
- Pharmacists: ensure appropriate medication management and address potential drug interactions or contraindications in the context of pneumothorax management.
- Rehabilitation specialists: physical and occupational therapists help patients optimize their functional capacity after pneumothorax resolution.
Effective communication, collaboration, and a clear delineation of roles within the interprofessional team are essential for providing optimal care to patients with pneumothorax.[27][28]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
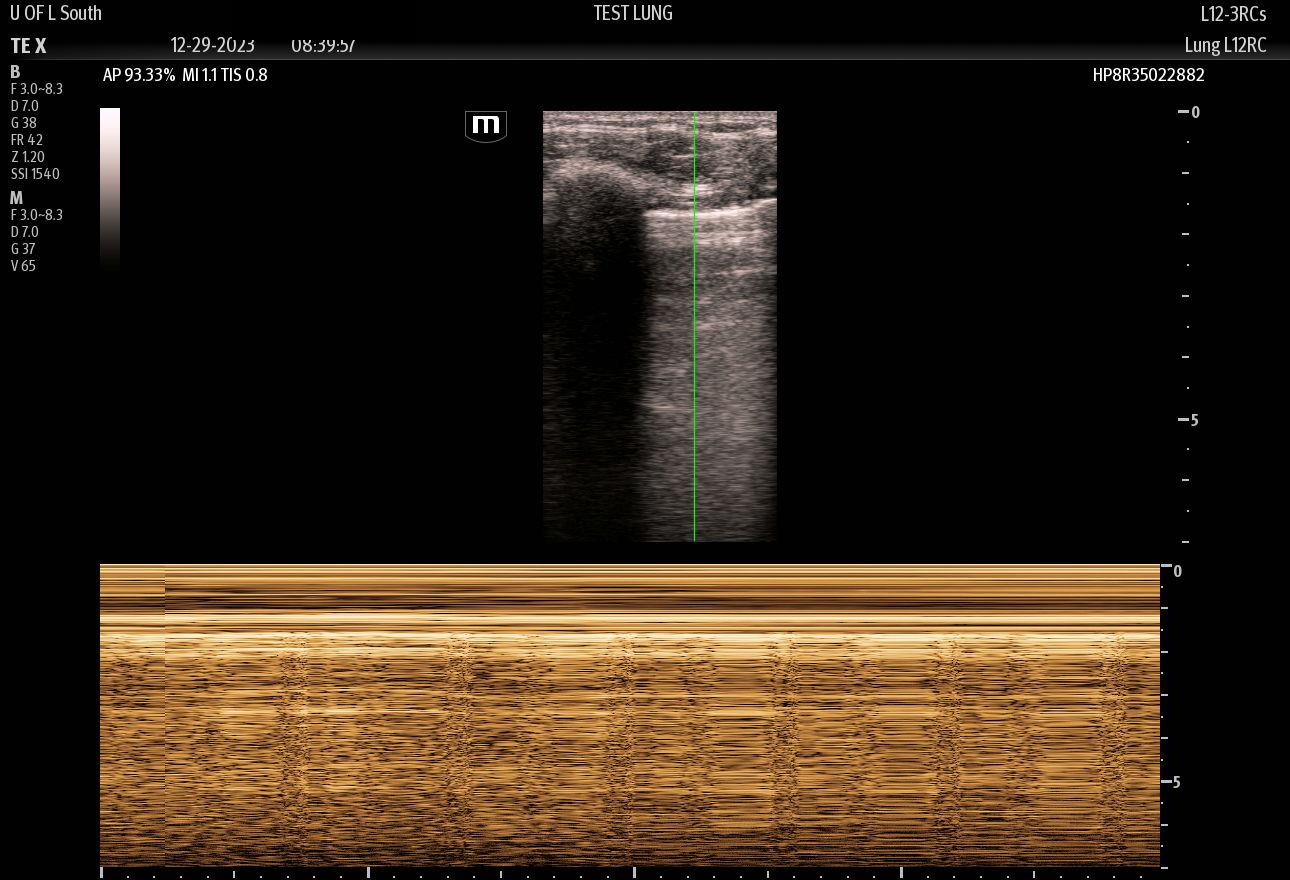
Lung Ultrasound M-Mode. This ultrasound shows the use of motion mode (M-mode), which helps identify pneumothorax. The yellow portion shows the flat, unmoving chest wall, while the grainy portion shows pleural movement. This is called the "Sandy Shore" and is present in normal examinations.
Contributed by Evan Kuhl, MD
(Click Video to Play)
Normal Lung Ultrasound. This video shows a normal lung ultrasound with lung sliding. The hyperechoic pleura is seen moving along the chest wall between 2 rib shadows. This indicates normal functioning and the absence of a pneumothorax.
Contributed by Evan Kuhl, MD
References
Wernick B, Hon HH, Mubang RN, Cipriano A, Hughes R, Rankin DD, Evans DC, Burfeind WR Jr, Hoey BA, Cipolla J, Galwankar SC, Papadimos TJ, Stawicki SP, Firstenberg MS. Complications of needle thoracostomy: A comprehensive clinical review. International journal of critical illness and injury science. 2015 Jul-Sep:5(3):160-9. doi: 10.4103/2229-5151.164939. Epub [PubMed PMID: 26557486]
Abdelrahman H, Atique S, Kloub AG, Hakim SY, Laughton J, Abdulrahman YS, El-Menyar A, Al-Thani H. Needle Decompression Causing Pericardial and Pulmonary Artery Injuries in Patients With Blunt Trauma: Two Case Reports and Literature Review. Journal of investigative medicine high impact case reports. 2023 Jan-Dec:11():23247096231211063. doi: 10.1177/23247096231211063. Epub [PubMed PMID: 37950344]
Level 3 (low-level) evidenceBaumann MH, Noppen M. Pneumothorax. Respirology (Carlton, Vic.). 2004 Jun:9(2):157-64 [PubMed PMID: 15182264]
Abolnik IZ, Lossos IS, Zlotogora J, Brauer R. On the inheritance of primary spontaneous pneumothorax. American journal of medical genetics. 1991 Aug 1:40(2):155-8 [PubMed PMID: 1897568]
Level 2 (mid-level) evidenceMinhas MS, Khan KM, Effendi J, Bhatti A, Jamali S. Improvised explosive device bombing police bus: Pattern of injuries, patho-physiology and early management. JPMA. The Journal of the Pakistan Medical Association. 2014 Dec:64(12 Suppl 2):S49-53 [PubMed PMID: 25989781]
Rodriguez RM, Canseco K, Baumann BM, Mower WR, Langdorf MI, Medak AJ, Anglin DR, Hendey GW, Addo N, Nishijima D, Raja AS. Pneumothorax and Hemothorax in the Era of Frequent Chest Computed Tomography for the Evaluation of Adult Patients With Blunt Trauma. Annals of emergency medicine. 2019 Jan:73(1):58-65. doi: 10.1016/j.annemergmed.2018.08.423. Epub 2018 Oct 2 [PubMed PMID: 30287121]
Neeki MM, Cheung C, Dong F, Pham N, Shafer D, Neeki A, Hajjafar K, Borger R, Woodward B, Tran L. Emergent needle thoracostomy in prehospital trauma patients: a review of procedural execution through computed tomography scans. Trauma surgery & acute care open. 2021:6(1):e000752. doi: 10.1136/tsaco-2021-000752. Epub 2021 Aug 27 [PubMed PMID: 34527813]
Osterman J, Kay AB, Morris DS, Evertson S, Brunt T, Majercik S. Prehospital decompression of tension pneumothorax: Have we moved the needle? American journal of surgery. 2022 Dec:224(6):1460-1463. doi: 10.1016/j.amjsurg.2022.09.014. Epub 2022 Sep 24 [PubMed PMID: 36210204]
Muchnok D, Vargo A, Deeb AP, Guyette FX, Brown JB. Association of Prehospital Needle Decompression With Mortality Among Injured Patients Requiring Emergency Chest Decompression. JAMA surgery. 2022 Oct 1:157(10):934-940. doi: 10.1001/jamasurg.2022.3552. Epub [PubMed PMID: 35976642]
Butler FK Jr, Holcomb JB, Shackelford SA, Montgomery HR, Anderson S, Cain JS, Champion HR, Cunningham CW, Dorlac WC, Drew B, Edwards K, Gandy JV, Glassberg E, Gurney JM, Harcke T, Jenkins DA, Johannigman J, Kheirabadi BS, Kotwal RS, Littlejohn LF, Martin MJ, Mazuchowski EL, Otten EJ, Polk T, Rhee P, Seery JM, Stockinger Z, Torrisi J, Yitzak A, Zafren K, Zietlow SP. Management of Suspected Tension Pneumothorax in Tactical Combat Casualty Care: TCCC Guidelines Change 17-02. Journal of special operations medicine : a peer reviewed journal for SOF medical professionals. 2018 Summer:18(2):19-35. doi: 10.55460/XB1Z-3BJU. Epub [PubMed PMID: 29889952]
Zengerink I, Brink PR, Laupland KB, Raber EL, Zygun D, Kortbeek JB. Needle thoracostomy in the treatment of a tension pneumothorax in trauma patients: what size needle? The Journal of trauma. 2008 Jan:64(1):111-4. doi: 10.1097/01.ta.0000239241.59283.03. Epub [PubMed PMID: 18188107]
Zietlow J, Hernandez M, Bestland A, Musa J, Ferrara M, Berns K, Anderson J, Zielinski M, Aho J. "Decompression of tension pneumothorax in a trauma patient -first use of a novel decompression colorimetric capnography device in human patient". General thoracic and cardiovascular surgery. 2021 Feb:69(2):391-393. doi: 10.1007/s11748-020-01471-7. Epub 2020 Sep 3 [PubMed PMID: 32885324]
Bøtker MT, Jacobsen L, Rudolph SS, Knudsen L. The role of point of care ultrasound in prehospital critical care: a systematic review. Scandinavian journal of trauma, resuscitation and emergency medicine. 2018 Jun 26:26(1):51. doi: 10.1186/s13049-018-0518-x. Epub 2018 Jun 26 [PubMed PMID: 29940990]
Level 1 (high-level) evidenceEimer C, Lorenzen U, Reifferscheid F, Passau N, Helzel K, Schmuck A, Seewald S, Köser A, Weiler N, Gässler H, Hossfeld B, Gruenewald M, Feth M. [Ultrasound diagnostics in prehospital emergency care-do we need a standardized educational approach?]. Medizinische Klinik, Intensivmedizin und Notfallmedizin. 2023 Aug 14:():. doi: 10.1007/s00063-023-01045-4. Epub 2023 Aug 14 [PubMed PMID: 37656173]
Meadley B, Olaussen A, Delorenzo A, Roder N, Martin C, St Clair T, Burns A, Stam E, Williams B. Educational standards for training paramedics in ultrasound: a scoping review. BMC emergency medicine. 2017 Jun 17:17(1):18. doi: 10.1186/s12873-017-0131-8. Epub 2017 Jun 17 [PubMed PMID: 28623905]
Level 2 (mid-level) evidenceBhoil R, Ahluwalia A, Chopra R, Surya M, Bhoil S. Signs and lines in lung ultrasound. Journal of ultrasonography. 2021 Aug 16:21(86):e225-e233. doi: 10.15557/JoU.2021.0036. Epub 2021 Sep 9 [PubMed PMID: 34540277]
Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonographic diagnosis of pneumothorax. Journal of emergencies, trauma, and shock. 2012 Jan:5(1):76-81. doi: 10.4103/0974-2700.93116. Epub [PubMed PMID: 22416161]
Taylor A, Anjum F, O'Rourke MC. Thoracic and Lung Ultrasound. StatPearls. 2024 Jan:(): [PubMed PMID: 29763189]
Park CB, Moon MH, Jeon HW, Cho DG, Song SW, Won YD, Kim YH, Kim YD, Jeong SC, Kim KS, Choi SY. Does oxygen therapy increase the resolution rate of primary spontaneous pneumothorax? Journal of thoracic disease. 2017 Dec:9(12):5239-5243. doi: 10.21037/jtd.2017.10.149. Epub [PubMed PMID: 29312731]
Marquette CH, Marx A, Leroy S, Vaniet F, Ramon P, Caussade S, Smaiti N, Bonfils C, Pneumothorax Study Group. Simplified stepwise management of primary spontaneous pneumothorax: a pilot study. The European respiratory journal. 2006 Mar:27(3):470-6 [PubMed PMID: 16507845]
Level 3 (low-level) evidenceBaumann MH. Management of spontaneous pneumothorax. Clinics in chest medicine. 2006 Jun:27(2):369-81 [PubMed PMID: 16716824]
Currie GP, Alluri R, Christie GL, Legge JS. Pneumothorax: an update. Postgraduate medical journal. 2007 Jul:83(981):461-5 [PubMed PMID: 17621614]
Kuhlwilm V. The Use of Chest Seals in Treating Sucking Chest Wounds: A Comparison of Existing Evidence and Guideline Recommendations. Journal of special operations medicine : a peer reviewed journal for SOF medical professionals. 2021 Spring:21(1):94-101. doi: 10.55460/3G6H-14FD. Epub [PubMed PMID: 33721314]
Kheirabadi BS, Terrazas IB, Koller A, Allen PB, Klemcke HG, Convertino VA, Dubick MA, Gerhardt RT, Blackbourne LH. Vented versus unvented chest seals for treatment of pneumothorax and prevention of tension pneumothorax in a swine model. The journal of trauma and acute care surgery. 2013 Jul:75(1):150-6 [PubMed PMID: 23940861]
Hossain R, Qadri U, Dembowski N, Garcia A, Chen L, Cicero MX, Riera A. Sound and Air: Ultrasonographic Measurements of Pediatric Chest Wall Thickness and Implications for Needle Decompression of Tension Pneumothorax. Pediatric emergency care. 2021 Dec 1:37(12):e1544-e1548. doi: 10.1097/PEC.0000000000002112. Epub [PubMed PMID: 32925707]
Henry M, Arnold T, Harvey J, Pleural Diseases Group, Standards of Care Committee, British Thoracic Society. BTS guidelines for the management of spontaneous pneumothorax. Thorax. 2003 May:58 Suppl 2(Suppl 2):ii39-52 [PubMed PMID: 12728149]
Level 1 (high-level) evidenceKepka S, Dalphin JC, Pretalli JB, Parmentier AL, Lauque D, Trebes G, EXPPI study group, Mauny F, Desmettre T. How spontaneous pneumothorax is managed in emergency departments: a French multicentre descriptive study. BMC emergency medicine. 2019 Jan 11:19(1):4. doi: 10.1186/s12873-018-0213-2. Epub 2019 Jan 11 [PubMed PMID: 30634911]
Bou Zein Eddine S, Boyle KA, Dodgion CM, Davis CS, Webb TP, Juern JS, Milia DJ, Carver TW, Beckman MA, Codner PA, Trevino C, de Moya MA. Observing pneumothoraces: The 35-millimeter rule is safe for both blunt and penetrating chest trauma. The journal of trauma and acute care surgery. 2019 Apr:86(4):557-564. doi: 10.1097/TA.0000000000002192. Epub [PubMed PMID: 30629009]