Introduction
Bile, a digestive fluid produced and secreted by the liver, is transported by a series of branching bile ducts known collectively as the biliary tree. At the cellular level, several narrow tubular channels called canaliculi collect the bile generated by each hepatocyte. These canaliculi drain into an intralobular bile duct which collects all the bile from each lobule, the functional unit of the liver. Intralobular ducts then drain into the interlobular ducts, which are located between lobules. The interlobular ducts merge to form the two main bile ducts of the liver: the right hepatic duct (RHD) and the left hepatic duct (LHD). Extrahepatically, the RHD and LHD coalesce to form the common hepatic duct (CHD), which travels within the hepatoduodenal ligament until coming into contact with the cystic duct, the bile duct, which connects to the gallbladder. The CHD and cystic duct merge to form the common bile duct (CBD). The hepatopancreatic ampulla, also called the hepatopancreatic duct or ampulla of Vater, is a spherical structure located at the site of the confluence of the common bile duct and pancreatic duct, marking the entry point of bile into the second portion of the duodenum. This is controlled by the smooth muscle fibers of the sphincter of Oddi, which opens at the duodenal papilla, allowing bile to flow into the small intestine. Alternatively, bile can travel into the gallbladder for storage via the cystic duct.[1][2][3]
Intrahepatic Ducts
- Canaliculi: Contain microvilli for increased surface area
- Intralobular ducts: These ducts are located alongside the hepatic artery and the portal vein. Together, these three structures are referred to as portal triads and are ensheathed by a layer of connective tissue known as Glisson’s capsule
- Interlobular ducts
- Right hepatic duct: Drains right lobe of the liver (segments V, VI, VII, and VIII)
- Left hepatic duct: Drains the left lobe of the liver (segments II, III, IV).
The caudate lobe of the liver (segment I) is drained by small ducts from both the right and left lobes.
Extrahepatic Ducts
- Extrahepatic segments of the right hepatic and the left hepatic ducts
- Common hepatic duct. Approximately 4 cm in length
- Cystic duct: Outflow tract of the gallbladder. Approximately 7 mm in diameter. Contains valves of Heister
- Common bile duct: Normal width should be less than approximately 6 mm. Approximately 6.0 cm to 8.0 cm in length.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The primary function of the biliary tract is to transport and release the bile. The gallbladder stores and concentrates bile. Bile assists with the absorption and digestion of fats and fat-soluble vitamins in addition to the removal of lipid-soluble waste products. The main components of bile are cholesterol, bile salts, and bilirubin. Bilirubin, responsible for the signature yellow-green color of bile, is also excreted in bile and is responsible for the pigmentation of feces.[4]
Embryology
The biliary ducts originate embryologically from the foregut. Early in the fourth week of development, the hepatic diverticulum arises from the endodermal epithelium of the ventral foregut. The hepatic diverticulum serves as the anlage for the liver, extrahepatic ducts, gallbladder, and ventral pancreas. The hepatic diverticulum is divided into two buds, the cranial bud and the caudal bud. The intrahepatic bile ducts develop from the cranial bud, whereas the extrahepatic biliary tree develops from the caudal bud. Notably, the hepatic diverticulum must recanalize to form the ducts. Hepatoblasts differentiate into the cholangiocytes that line the intrahepatic bile ducts.
Blood Supply and Lymphatics
Arterial
The blood supply of the biliary system originates from the celiac trunk, which branches off of the abdominal aorta at the T12 level, giving rise to the splenic artery, common hepatic artery, and left gastric artery. Arterial supply to the biliary tract is well documented due to its clinical relevance in the liver transplant procedure. In general, the common hepatic artery plays a crucial role in providing oxygenated blood to the liver. Supplies to the biliary tree rely on an intricate network of plexuses from subsidiary branches of larger vessels, including hepatic proper, cystic, gastroduodenal, and posterior superior pancreaticoduodenal arteries. Paracholedocal plexus, as the name implies, supplies the medial and lateral sides of the biliary duct, while epicholedocal plexus trails on the top of the duct. However, not all portions of the biliary tree receive equal blood supply from the nearby arteries. For example, the supraduodenal CBD (immediately inferior to the confluence between the cystic duct and the CHD) receives the least amount of blood supply, thus predisposing it to ischemic attack; the implication is especially strong in liver transplantation where the arterial supply is often disrupted.[5][6]
Venous Drainage
The venous network that drains the biliary tree is parallel to that of its arterial counterpart. The main difference is that the epicholedocal venous plexus drains into epicholedocal plexus. Epicholedocal plexus has a superior and an inferior outlet; the former joins the portal vein near the hilar of the liver, whereas the latter drains into the superior mesenteric vein before merging with the portal vein.[7][8]
Lymphatics
The lymphatic drainage of the gallbladder is more commonly described than that of the biliary ducts. From the gallbladder, lymph flows through the cystic nodes, hepatic nodes, and finally, the celiac chains.
Nerves
The biliary tree is innervated by both sympathetic and parasympathetic fibers from the celiac plexus. The splanchnic nerves carry sympathetic fibers, while the vagus nerve carries parasympathetic fibers. Stimulation of splanchnic nerve visceral efferent fibers causes gallbladder relaxation, allowing bile to flow into the gallbladder through the cystic duct for storage.
Conversely, gallbladder contraction with bile secretion is primarily mediated by the hormone cholecystokinin (CCK), which the duodenum secretes in response to the arrival of food in the small intestine. Parasympathetic fibers from the vagus nerve assist CCK in this process.
Physiologic Variants
Different biliary tree configurations have been identified through the study of cadavers, MRCP, and intraoperative cholangiogram. Most commonly, the unity of a horizontally traversed right posterior duct (RPD) and a vertically traversed right anterior duct (RAD) forms the RHD. The RHD then joins with the LHD to create a CHD. The second variant describes a trifurcated configuration where the RPD, RAD, and LHD join at a single confluence to form a CHD. Rarely one can see the presence of an accessory duct (Duct of Luschka) that extends from the liver and enters the gallbladder. Configurations such as abnormal emptying of the RPD or direct drainage from the RHD into the cystic duct exist but are less frequently seen.[9][10][11]
The cystic duct typically originated from the gallbladder, joining with the CHD to form the CBD. The confluence is found in the middle third of the extrahepatic duct in the majority of the population. However, anatomical variants exist, and one must recognize them during biliary procedures. For example, a low fusion of a long cystic duct and CHD is seen in approximately 8.6% of study subjects. In contrast, 2.1% of cystic duct fuses with proximal CHD near the liver edge. Other variants, such as the absence of cystic duct or duplicated ducts, have all been reported. [10][12]
Surgical Considerations
Bile duct injury is a potential complication of cholecystectomy. Misidentification of critical anatomical structures is a common cause, mainly due to the proximity of the cystic duct, the CHD, and the CBD. The incidence is higher in a laparoscopic than in an open procedure.[13][14] During the operation, it is crucial to identify Calot's triangle - an anatomical space defined superiorly by the inferior border of the liver, medially by the common hepatic duct, and laterally by the cystic duct. Calot's triangle contains structures such as the cystic artery and Mascagni's node (Lund's node). Rarely, an accessory hepatic duct or right hepatic artery can also be found traversing through this space. To avoid arterial or unwanted biliary injury, surgeons need to establish a "critical view of safety." The critical view of safety comprises three components: identifying Calot's triangle, exposing the inferior portion (infundibulum) of the gallbladder, and revealing only the cystic duct and cystic artery for ligation.[15]
Cholecystectomy, the surgical removal of the gallbladder, is usually performed laparoscopically. Indications for cholecystectomy include symptomatic cholelithiasis, cholecystitis, porcelain gallbladder, and gallbladder polyps greater than 0.5 cm. Cholecystectomy is recommended for patients with asymptomatic cholelithiasis if there is an increased risk of gallbladder carcinoma or other complications.[16][17]
Clinical Significance
The biliary tract provides an outlet to transport bile into the gastrointestinal tract, which facilitates the absorption of fat-soluble nutrients. In general, acute obstruction of the biliary tract can lead to steatorrhea, while chronic obstruction can cause fat-soluble vitamin deficiency (A, D, E, and K). Proximal to the site of obstruction also harbors an opportunity for bacterial infection, as in the case of ascending cholangitis.[18] If left untreated, a chronic biliary obstruction can cause portal hypertension and its associated complications.
Congenital anomalies associated with the biliary tract include biliary atresia, choledochal cysts, and congenital biliary ectasia. Biliary atresia is the most common cause of conjugated hyperbilirubinemia in young infants. [19] The etiology of the disease is not well understood; however, both genetic and environmental factors have been implicated.[20][21][22][23] Several mechanisms have been proposed, including failure to recanalize during the bile duct formation and repeated structural insult leading to extensive luminal fibrosis. Patients usually have normal growth but gradually develop jaundice and acholic stools within two months after birth. The initial evaluation with ultrasound is aimed at excluding other causes of cholestasis, such as a choledochal cyst. Hepatobiliary scintigraphy can delineate the patency of the biliary tree. The liver function test often confers to cholestasis pattern. If surgical intervention is warranted, a definitive diagnosis can be confirmed by an intraoperative cholangiogram. Early surgical intervention with Kasai portoenterostomy procedure improves the disease prognosis. Ultimately, patients will require a liver transplant.
Cholelithiasis, commonly known as gallstones, is a common disease in Western populations.[24][25][26] While the majority of people with gallstones are asymptomatic, biliary pathology is often associated with gallstones. For example, acute cholecystitis is most commonly caused by gallstone obstruction of the cystic duct. This obstruction leads to inflammation of the gallbladder. Classically, the patient will present with right upper quadrant abdominal pain, fever, nausea, vomiting, and an elevated white blood cell count. If the subdiaphragmatic parietal peritoneum is irritated by the inflamed gallbladder, patients may also experience pain in the right shoulder - a phenomenon called "referred pain." Rarely, an obstruction in the cystic duct is severe, so the enlarged duct compresses on the nearby common hepatic duct, as seen in Mirrizi syndrome. Patients with Mirrizi syndrome show signs of jaundice in addition to the classic symptoms of cholecystitis.[27]
Clinical Vocabulary
- Biliary colic is the intermittent, dull RUQ pain due to transient blockage of bile flow
- Cholelithiasis means gallstones present within the gallbladder
- Choledocholithiasis means gallstones situate within the common bile duct
- Gallstone pancreatitis is pancreatic inflammation from gallstone blockage of the pancreatic duct
- Cholecystitis is inflammation of the gallbladder due to prolonged obstruction of the cystic duct
- Cholecystectomy is the surgical removal of the gallbladder
- Cholangitis is an infection of the bile ducts
- Cholangiocarcinoma is an aggressive cancer of the bile ducts
Media
(Click Image to Enlarge)
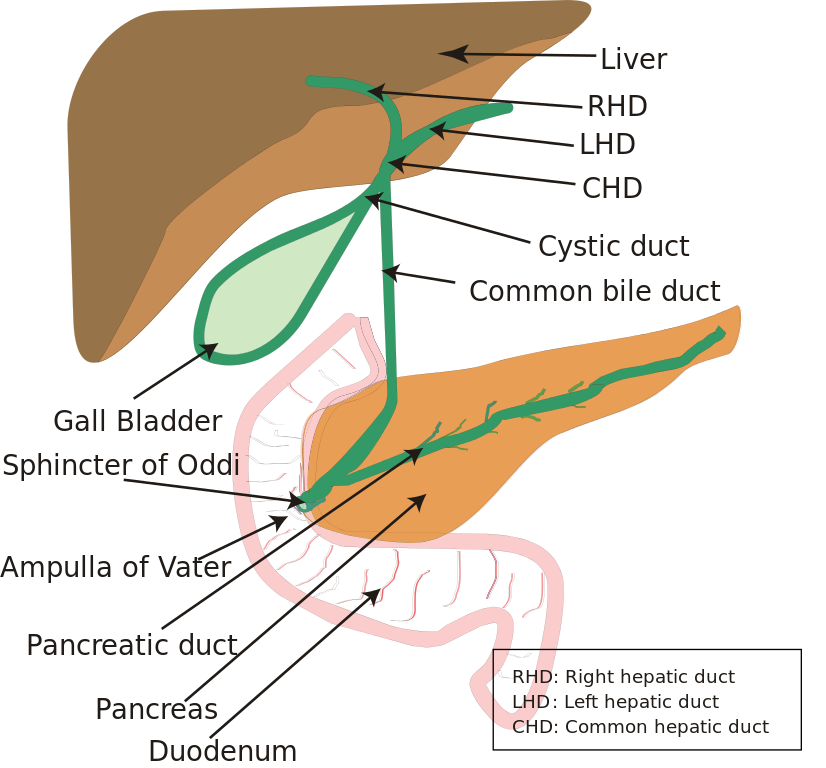
Diagram of the Biliary System. Note that the ampulla of Vater is behind the major duodenal papilla—sphincter of Oddi.
Vishnu2011, Public Domain, via Wikimedia Commons
References
Garg S, Kumar H, Sahni D, Yadav TD, Aggarwal A, Gupta T. Rare anatomic variations of the right hepatic biliary system. Surgical and radiologic anatomy : SRA. 2019 Sep:41(9):1087-1092. doi: 10.1007/s00276-019-02260-5. Epub 2019 May 21 [PubMed PMID: 31115596]
Kafle A, Adhikari B, Shrestha R, Ranjit N. Anatomic Variations of the Right Hepatic Duct: Results and Surgical Implications From a Cadaveric Study. Journal of Nepal Health Research Council. 2019 Apr 28:17(1):90-93. doi: 10.33314/jnhrc.2012. Epub 2019 Apr 28 [PubMed PMID: 31110384]
Chehade M, Kakala B, Sinclair JL, Pang T, Al Asady R, Richardson A, Pleass H, Lam V, Johnston E, Yuen L, Hollands M. Intraoperative detection of aberrant biliary anatomy via intraoperative cholangiography during laparoscopic cholecystectomy. ANZ journal of surgery. 2019 Jul:89(7-8):889-894. doi: 10.1111/ans.15267. Epub 2019 May 13 [PubMed PMID: 31083792]
Vosshenrich J, Boll DT, Zech CJ. [Passive and active magnetic resonance cholangiopancreatography : Technique, indications, and typical anatomy]. Der Radiologe. 2019 Apr:59(4):306-314. doi: 10.1007/s00117-019-0507-8. Epub [PubMed PMID: 30859236]
Ramesh Babu CS, Sharma M. Biliary tract anatomy and its relationship with venous drainage. Journal of clinical and experimental hepatology. 2014 Feb:4(Suppl 1):S18-26. doi: 10.1016/j.jceh.2013.05.002. Epub 2013 May 25 [PubMed PMID: 25755590]
Vellar ID. The blood supply of the biliary ductal system and its relevance to vasculobiliary injuries following cholecystectomy. The Australian and New Zealand journal of surgery. 1999 Nov:69(11):816-20 [PubMed PMID: 10553973]
Couinaud C. The parabiliary venous system. Surgical and radiologic anatomy : SRA. 1988:10(4):311-6 [PubMed PMID: 3145573]
Vellar ID. Preliminary study of the anatomy of the venous drainage of the intrahepatic and extrahepatic bile ducts and its relevance to the practice of hepatobiliary surgery. ANZ journal of surgery. 2001 Jul:71(7):418-22 [PubMed PMID: 11450918]
Choi JW, Kim TK, Kim KW, Kim AY, Kim PN, Ha HK, Lee MG. Anatomic variation in intrahepatic bile ducts: an analysis of intraoperative cholangiograms in 300 consecutive donors for living donor liver transplantation. Korean journal of radiology. 2003 Apr-Jun:4(2):85-90 [PubMed PMID: 12845303]
Hyodo T, Kumano S, Kushihata F, Okada M, Hirata M, Tsuda T, Takada Y, Mochizuki T, Murakami T. CT and MR cholangiography: advantages and pitfalls in perioperative evaluation of biliary tree. The British journal of radiology. 2012 Jul:85(1015):887-96. doi: 10.1259/bjr/21209407. Epub 2012 Mar 14 [PubMed PMID: 22422383]
Mortelé KJ, Ros PR. Anatomic variants of the biliary tree: MR cholangiographic findings and clinical applications. AJR. American journal of roentgenology. 2001 Aug:177(2):389-94 [PubMed PMID: 11461869]
Benson EA, Page RE. A practical reappraisal of the anatomy of the extrahepatic bile ducts and arteries. The British journal of surgery. 1976 Nov:63(11):853-60 [PubMed PMID: 1000180]
Pucher PH, Brunt LM, Davies N, Linsk A, Munshi A, Rodriguez HA, Fingerhut A, Fanelli RD, Asbun H, Aggarwal R, SAGES Safe Cholecystectomy Task Force. Outcome trends and safety measures after 30 years of laparoscopic cholecystectomy: a systematic review and pooled data analysis. Surgical endoscopy. 2018 May:32(5):2175-2183. doi: 10.1007/s00464-017-5974-2. Epub 2018 Mar 19 [PubMed PMID: 29556977]
Level 1 (high-level) evidenceSouthern Surgeons Club. A prospective analysis of 1518 laparoscopic cholecystectomies. The New England journal of medicine. 1991 Apr 18:324(16):1073-8 [PubMed PMID: 1826143]
Zarin M, Khan MA, Khan MA, Shah SAM. Critical view of safety faster and safer technique during laparoscopic cholecystectomy? Pakistan journal of medical sciences. 2018 May-Jun:34(3):574-577. doi: 10.12669/pjms.343.14309. Epub [PubMed PMID: 30034418]
Cohen JT, Charpentier KP, Beard RE. An Update on Iatrogenic Biliary Injuries: Identification, Classification, and Management. The Surgical clinics of North America. 2019 Apr:99(2):283-299. doi: 10.1016/j.suc.2018.11.006. Epub 2019 Feb 10 [PubMed PMID: 30846035]
Bauschke A. [Biliary system : What does the surgeon want to know from the radiologist?]. Der Radiologe. 2019 Apr:59(4):300-305. doi: 10.1007/s00117-019-0502-0. Epub [PubMed PMID: 30820620]
Kimura Y, Takada T, Kawarada Y, Nimura Y, Hirata K, Sekimoto M, Yoshida M, Mayumi T, Wada K, Miura F, Yasuda H, Yamashita Y, Nagino M, Hirota M, Tanaka A, Tsuyuguchi T, Strasberg SM, Gadacz TR. Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. Journal of hepato-biliary-pancreatic surgery. 2007:14(1):15-26 [PubMed PMID: 17252293]
Gottesman LE, Del Vecchio MT, Aronoff SC. Etiologies of conjugated hyperbilirubinemia in infancy: a systematic review of 1692 subjects. BMC pediatrics. 2015 Nov 20:15():192. doi: 10.1186/s12887-015-0506-5. Epub 2015 Nov 20 [PubMed PMID: 26589959]
Level 1 (high-level) evidenceCaton AR, Druschel CM, McNutt LA. The epidemiology of extrahepatic biliary atresia in New York State, 1983-98. Paediatric and perinatal epidemiology. 2004 Mar:18(2):97-105 [PubMed PMID: 14996248]
Hart MH, Kaufman SS, Vanderhoof JA, Erdman S, Linder J, Markin RS, Kruger R, Antonson DL. Neonatal hepatitis and extrahepatic biliary atresia associated with cytomegalovirus infection in twins. American journal of diseases of children (1960). 1991 Mar:145(3):302-5 [PubMed PMID: 1848391]
Level 3 (low-level) evidenceHarper P, Plant JW, Unger DB. Congenital biliary atresia and jaundice in lambs and calves. Australian veterinary journal. 1990 Jan:67(1):18-22 [PubMed PMID: 2334368]
Level 3 (low-level) evidenceLorent K, Gong W, Koo KA, Waisbourd-Zinman O, Karjoo S, Zhao X, Sealy I, Kettleborough RN, Stemple DL, Windsor PA, Whittaker SJ, Porter JR, Wells RG, Pack M. Identification of a plant isoflavonoid that causes biliary atresia. Science translational medicine. 2015 May 6:7(286):286ra67. doi: 10.1126/scitranslmed.aaa1652. Epub [PubMed PMID: 25947162]
Cannella R, Giambelluca D, Diamarco M, Caruana G, Cutaia G, Midiri M, Salvaggio G. Congenital Cystic Lesions of the Bile Ducts: Imaging-Based Diagnosis. Current problems in diagnostic radiology. 2020 Jul-Aug:49(4):285-293. doi: 10.1067/j.cpradiol.2019.04.005. Epub 2019 Apr 6 [PubMed PMID: 31027922]
Snyder E,Lopez PP, Hepatobiliary Iminodiacetic Acid (HIDA) Scan 2019 Jan; [PubMed PMID: 30969603]
Coucke EM, Akbar H, Kahloon A, Lopez PP. Biliary Obstruction. StatPearls. 2023 Jan:(): [PubMed PMID: 30969520]
Clemente G, Tringali A, De Rose AM, Panettieri E, Murazio M, Nuzzo G, Giuliante F. Mirizzi Syndrome: Diagnosis and Management of a Challenging Biliary Disease. Canadian journal of gastroenterology & hepatology. 2018:2018():6962090. doi: 10.1155/2018/6962090. Epub 2018 Aug 12 [PubMed PMID: 30159303]