Introduction
Laryngeal and tracheal stenosis are a relatively rare but potentially catastrophic cause of acute airway compromise.[1] Laryngeal stenosis may be due to narrowing of the supraglottis, glottis, or subglottis; the subglottis is defined as the airway situated 10mm below the apex of the laryngeal ventricle and 5mm below the posterior inferior surface of the true vocal folds.[2] Tracheal stenosis occurs from the inferior margin of the subglottis to the carina, and bronchial stenosis affects the mainstem bronchi and distal airways.[3]
It is imperative to differentiate between laryngeal and tracheal stenosis despite some shared presentation, etiology, and management aspects. The long-term management and prognosis of these two processes can significantly diverge. However, stenting is a potential treatment avenue for both conditions, be they congenital anomalies or those acquired later in life.
Laryngeal stenosis is predominately congenital; it is the third-most common congenital laryngeal anomaly after laryngomalacia and congenital vocal fold palsy.[4] However, laryngeal stenosis is often acquired and is frequently subglottic and idiopathic. Acquired idiopathic subglottic laryngeal stenosis disproportionately affects adult women for reasons unknown.[5] Airway stenosis following endotracheal intubation poses a substantial healthcare burden, manifesting as either subglottic laryngeal stenosis, tracheal stenosis, or a combination of both.[6] Additional causes for acquired laryngeal and tracheal stenosis include caustic injury, infection, tumor, or granulomatous disease.[7]
Laryngotracheal stenosis lacks a universally standardized management protocol or algorithm; cause- and location-specific treatment must be personalized for each patient. Airway stenosis may be managed with endoscopic dilatation, laryngeal microsurgery, laser-assisted excision, open airway surgery, or endoscopic stent placement.[8]
Laryngeal and tracheal stents, crafted from solid or hollow materials, prevent the collapse of the airway lumen. Stents stabilize surgical reconstructions of the larynx or trachea and mechanically expand areas affected by scar tissue or tumor encroachment.[9] Stents may be absorbable or nonabsorbable and are available in diverse sizes and shapes tailored to the underlying condition. Recent advancements have explored the use of extraluminal tracheal suspension devices.[10][11]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Larynx
The larynx is positioned above the trachea and beneath the hyoid bone. The larynx is a complex cartilaginous structure comprising 9 framework cartilages. This framework includes the thyroid cartilage, cricoid cartilage, epiglottis, and pairs of arytenoid, cuneiform, and corniculate cartilage.[12] The larynx regulates air flow in and out of the lungs, safeguarding against the entry of food and water into the lungs, and provides a controlled vibratory locus for speech centered around the true vocal folds. Balancing these functions, the dynamic nature of the larynx allows the essential processes of respiration and phonation while preventing the aspiration of liquids and solids through controlled mechanical obstruction.[13] However, the use of stenting, an adynamic splinting of the airway, in the larynx, while potentially aiding respiratory function by expanding the airway lumen, may pose a significant compromise to its protective function by impeding the closure of the glottis or movement of the larynx.[14]
Trachea
The trachea is a fibrocartilaginous structure in the lower respiratory tract below the larynx that consists of 16 to 20 incomplete anterior cartilaginous rings and the trachealis muscle posteriorly, forming the shared wall with the anterior esophagus. Bounded superiorly by the laryngeal subglottis and inferiorly by the carina and mainstem bronchi, the trachea plays a crucial role in transporting air to and from the lungs while maintaining the structural integrity of the airway to prevent collapse during respiration.[15] Narrowing of the tracheal lumen can result from mucosal, cartilaginous, or external factors. As the tracheal lumen narrows, according to the law of Poiseuille, the velocity of airflow through the constricted space and the pressure required to maintain flow increases by the fourth power of the radius of the lumen.[16]
Stenosis Grading
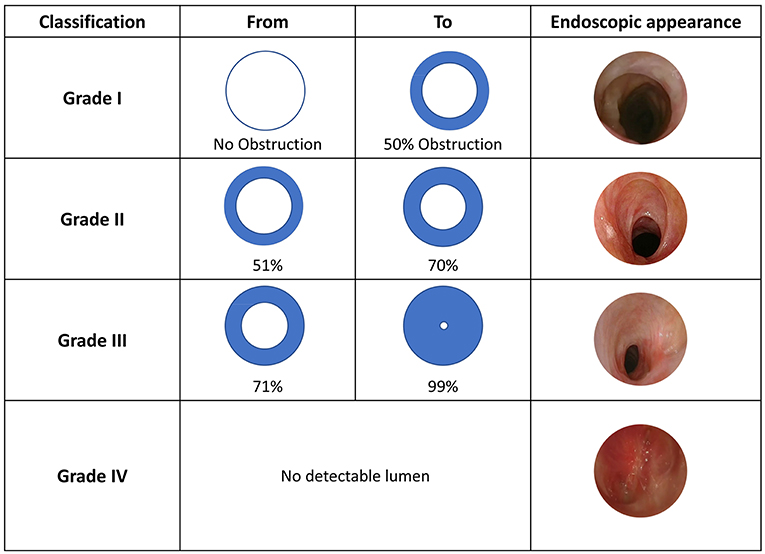
Laryngotracheal stenosis can be graded based on the percent of obstruction of the diameter of the tracheal lumen using the Cotton-Myer subglottic stenosis grading scale (see Image. Myer-Cotton Grading Scale). The luminal obstruction grading in this scale is as follows: grade I is 0%-50%, grade II is 51%-70%, grade III is 71%-99%, and grade IV is a complete obstruction.[17]
In 1992, McCaffrey proposed a classification to describe the extension of the stenosis among the most commonly involved subsites: glottis, subglottis, and trachea (see Image. McCaffrey Classification). This classification was conceived after both univariate and multivariate analyses demonstrated that the involved site had the most consistent significant predictive value for determining the time to decannulation. Stage I is located in the subglottis or trachea in this classification system, with a craniocaudal extension of less than 1 cm. Stage II stenosis is limited to the subglottis and has a craniocaudal extension of more than 1 cm. Stage III stenosis involves both the subglottis and trachea and stage IV stenosis extends to the glottis with fixation or paralysis of at least 1 vocal cord.
Indications
There are many congenital and acquired conditions in which laryngeal and tracheal stents may be required. These conditions include but are not limited to:
- Reconstruction of laryngotracheal stenosis
- Trauma
- Congenital laryngeal or tracheal stenosis
- Malignancy invading the tracheal or bronchial lumen
- Laryngeal atresia
- Tracheomalacia or bronchomalacia.[18]
Contraindications
Absolute contraindications to laryngeal and tracheal stents include patients who are poor candidates for general anesthesia, those with an allergy to stent material, and those with no expandable lung distal to the obstruction.[19]
Equipment
Laryngotracheal stents are typically categorized as either suprastomal or substomal/intratracheal. Suprastomal stents are designed to treat diseases in the suprastomal trachea, subglottic, and glottic larynx; these diseases are typically associated with laryngeal pathology. Substomal/intratracheal stents are placed below the stoma or when the disease is confined to the trachea. Depending on the disease being treated, laryngotracheal stents may be placed by either an endoscopic or open approach. Several stent materials are currently available; depending on the material and underlying indications, the stent may be designed for short-term use of less than 6 weeks or longer-term use.[20][21] The versatility in stent types and placement approaches allows tailored solutions aligned with specific patient needs and the nature of the pathology being addressed.
Suprastomal Stents
Montgomery T-tube
The Montgomery T-tube, a vintage airway stent introduced in the 1960s, is a cylindrical soft silicone stent featuring an accessory tube branching off at a 75- to 90-degree angle, creating an overall T-shaped structure.[22] This accessory tube is inserted through a tracheostoma, offering respiratory and suction access to the lower airway via the neck while the stent is in position. While the soft silicone minimizes irritation to the underlying mucosa, it does impede mucociliary clearance, necessitating meticulous T-tube care. Available in adult and pediatric sizes, T-tubes with a lumen smaller than 5 mm are susceptible to crusting and obstruction, leading to reduced favor in many centers.[23] In laryngotracheal reconstruction, the cephalad end of the T-tube is positioned above the vocal cords, instructing patients to utilize a supraglottic swallow to minimize aspiration; removal is typically scheduled after 2 weeks.[9]
Aboulker stent
The Aboulker stent, once a predominant choice after laryngotracheal reconstruction, gained popularity in the late 1980s. Comprising a rigid Teflon structure with bilaterally tapered ends, this cigar-shaped stent differs from a Montgomery T-tube by lacking an accessory lumen. However, the potential life-threatening migration of the solid rigid Aboulker stent over the tracheostoma posed a significant concern. The most common mitigating approach involved suturing the Aboulker stent to a Jackson metallic tracheostomy tube to ensure fixed positioning and minimize mucosal irritation at the stent ends.[24] The Aboulker stent is no longer available in the United States. The Rutter and Monnier stents and the continued use of the Montgomery T-tube have almost entirely supplanted the use of the Aboulker stent.
Rutter stent
The Rutter stent is a soft, silastic, cylindrical device featuring a tapered distal end, designed for placement through both open and endoscopic approaches without impeding tracheostomy insertion. The distal taper reduces mucosal irritation and granulation tissue formation. The proximal end is precisely trimmed to rest at the level of the false vocal cords, accompanied by a soft, rounded cap to minimize the risk of supraglottic stenosis.[25] Given its typical capped configuration, occluding the proximal end of the stent, a tracheostomy is required.[26]
Monnier stent
The Monnier stent, crafted from soft silicone and molded based on cadaver larynges, is produced in 10 sizes for tailored applications.[27] Designed to replicate the glottic airway with fully abducted vocal cords, the Monnier stent proves particularly effective in addressing posterior glottic stenosis and subglottic stenosis. The soft silicone construction prioritizes patient comfort by minimizing mucosal trauma and reducing granulation at pressure points around the arytenoids.[28]
Silastic sheet
Introduced in the 1970s, silastic sheets initially served as soft stents when rolled and were later found to be applied as small sheets or keels in cases of anterior glottic stenosis. However, the sharper edges of silastic sheets led to substantial irritation and granulation tissue formation, prompting their replacement by softer, less traumatic stents like the Rutter or Monnier.[29] Despite this, silastic sheets have experienced a resurgence in the era of endoscopic laryngotracheal reconstruction, where they can be strategically placed as an anterior keel using an endoscopic approach.[30]
Tracheal Stents
Silicone stents
Silicone stents, such as the Dumon and Hood varieties, which have been widely available since the 1990s, have been recognized for their soft material, which does not induce significant mucosal granulation tissue formation compared to silastic or metal alternatives. However, a notable risk of stent migration is associated with silicone materials.[31] Efforts have been made to enhance stent fixation, yielding varying degrees of success.[32][33] Additionally, silicone stents are susceptible to forming intraluminal biofilms, which may lead to stent narrowing or obstruction.[34]
Endotracheal tubes
Endotracheal tubes have long been used as temporary, short-term airway stents after tracheal resection or laryngotracheal reconstruction, notably after an anterior cricoid split operation pioneered by Cotton.[35] While the use of endotracheal tubes for longer-term stenting has been reported, this is most often related to emergent situations where a more suitable stent was unavailable for supply-chain reasons.[36][37]
Metallic stents
The original expandable wire mesh stents were made of bare metal wire, similar in appearance to angioplasty stents.[38] The wire mesh design was thought to facilitate mucociliary activity. However, significant granulation tissue often develops within these spaces and at the end of the stents.[39] These wire stents frequently become fully integrated into the trachea and are considered by some authors to be permanent stents.[40]
Metallic stents should only be used temporarily and cautiously in the pediatric population, as the rate and severity of complications may be similar to or worse than the underlying airway pathology.[41] For this reason, there is a United States Food and Drug Administration (FDA) black box warning on such stents for use in benign airway pathology in children. Metallic stents coated with silicone have been developed to alleviate some of these complications. However, the ends of the stent are left as bare wire to anchor the stent within the trachea.[11] As a result, tumor ingrowth within the stent has been reduced, but granulation tissue at the ends remains problematic. These coated stents are more easily removed than the bare wire stents.[42]
Preparation
A comprehensive airway assessment relies on laryngoscopy and bronchoscopy, complemented by imaging studies such as computed tomography (CT) or magnetic resonance imaging (MRI) if a complete understanding of the lesion is not achievable through endoscopy alone. Identifying the precise location of the stenosis or lesion is essential, differentiating between laryngeal regions (supraglottic, glottic, subglottic, or trans-glottic) and tracheal or bronchial sites. Additionally, the distance from relevant landmarks, typically measured from the glottis, should be documented. Grading systems like the Cotton-Myer or estimating the percentage of luminal obstruction while recording the length of the stenotic segment are viable options for evaluating the degree of stenosis.
In cases where severe or tortuous stenosis hinders accurate endoscopic measurement, CT images provide a valuable alternative for estimating stenosis length.[43] Based on the severity, length, and location within the trachea or larynx, the choice of stent type and the decision between open and endoscopic surgical approaches are determined. At this stage, a multidisciplinary team, including pulmonologists and cardiothoracic surgeons, can offer valuable insights and contribute to the surgical plan.[44]
Technique or Treatment
Both laryngeal and tracheal stents can be placed via endoscopic, open, or combined approaches, depending on the patient, underlying pathology, and the preference and experience of the operating surgeon.
Laryngeal Stents
Laryngeal stents are not commonly used as a primary treatment for laryngeal stenosis but are usually placed temporarily after a surgical intervention, either by endoscopy or open surgery, to keep the airway open and maintain the position of any reconstructive devices. This differs from the trachea, where stents are used more frequently as a primary treatment.
Endoscopic approach
The endoscopic approach to laryngeal stent placement is frequently employed in adults to insert anterior glottic keels following the treatment of anterior glottic stenosis.[45] This approach is also utilized to place temporary stents, such as silicone stents, after addressing subglottic stenosis.[46] In pediatric cases of laryngeal stenosis, the endoscopic approach plays a role in either a combined endoscopic-open procedure, incorporating various stent types, or as the primary method for placing a Rutter or other type of stent, especially in cases of posterior subglottic stenosis.[47]
Patient positioning for laryngeal stent placement is crucial; supine positioning with a shoulder roll facilitates neck extension. The anterior neck is prepped as a separate sterile surgical field or made easily accessible for emergencies. A preoperative anesthetic plan, tailored in consultation with the anesthesiologist, may include tracheostomy, jet ventilation, total intravenous anesthesia, or transnasal humidified rapid-insufflation ventilatory exchange.[48] The choice depends on the planned operation and patient considerations.
The use of suspension microlaryngoscopy instruments and the selection of the largest bore laryngoscope for optimal visualization of laryngeal pathology are emphasized. Larger scopes like Lindholm or Dedo are preferred to allow the greatest possible working space. Rigid video telescopes and traditional microscopes can be used, with the latter offering the advantage of bimanual instrumentation. A rigid bronchoscopy setup should be available for emergent airway situations.
The planned procedure is then performed to address the laryngeal stenosis, and the stent can be placed endoscopically. The keel or silastic/silicone sheet is positioned in the neo-anterior commissure under endoscopic guidance for anterior glottic stenosis. Transcutaneous securing involves nylon or prolene sutures through the neck skin and into the airway under endoscopic visualization. The suture is passed through the stent, returned to the skin surface, and tied subcutaneously or over a bolster.
In the case of subglottic stenosis, the dilatation procedure is performed via various endoscopic approaches, and the silicone or other temporary stent is then selected. A Montgomery T-tube may be trimmed and sculpted to serve as a temporary stent, allowing custom sizing for each patient.[49] The stent is placed under endoscopic visualization and then secured via a transtracheal anterior neck incision with 2-0 nylon or prolene suture. This combined endoscopic-open approach ensures the suture secures the stent in place.[50]
Alternatively, particularly in endoscopic pediatric laryngotracheal reconstruction, the procedure and graft placement occur while carefully intubating the patient transorally with the endoscope. The tube is left in place as a de facto stent for a week, with subsequent extubation and repeat laryngoscopy performed in the operating room to verify graft positions are maintained.[51]
Open approach
With the numerous advances in endoscopic techniques and technology, an ever-expanding number of conditions can be managed without open laryngeal surgery. Nevertheless, laryngofissure is still a viable treatment approach for severe glottic stenosis, and open approaches are routinely used for laryngotracheal reconstruction when both anterior and posterior grafting are required.[52][53] In an open approach, the stent is placed after the extirpative or reconstructive procedure, and the larynx is closed over the stent. As previously discussed, combined endoscopic-open approaches are also employed.
Tracheal Stents
Tracheal stents can be used for short—or long-term applications and are placed using a bronchoscopic or open approach; the latter is becoming increasingly rare.
Bronchoscopic approach
The nuances of stent deployment are contingent on the specific stent type and its construction material. Adherence to the manufacturers' instructions is imperative to ensure safety and efficacy. Although variations exist among stents, the general procedure is outlined here.
Typically performed under general anesthesia, the process begins with a flexible bronchoscopy to examine the airway, confirm the lesion's location, and assess its severity.[54] Following this, the narrowed airway is dilated using a balloon, or tumor debulking is conducted in cases of tumor encroachment. A guidewire is threaded through the stenotic segment, with fluoroscopy used for confirmation if the distal tip of the guidewire is not directly visible. Subsequently, the selected stent delivery device is advanced over the guidewire per the stent manufacturer's guidelines.[55] Once the position is confirmed, the stent is deployed. A chest radiograph is routinely obtained to ensure proper placement, although fluoroscopy and intraoperative CT scans have also been employed.[56] Following deployment, it takes 24 to 48 hours for the stent to enlarge and reach its final dimensions fully.[57][58]
Traditionally, tracheal stents were inserted via rigid bronchoscopy using a similar technique; however, advances in imaging and flexible bronchoscopy instrument capabilities have considerably diminished the elective use of rigid bronchoscopy for stent placement.[59]]
Open approach
While tracheal stents can be inserted through open techniques, such practices are exceedingly rare, primarily due to the prominence of endoscopic methods that emerged in the 1970s.[60] In contemporary practice, isolated tracheal stenoses are typically addressed using either endoscopic methods or open resections, effectively avoiding the considerable morbidity associated with sternotomy. Nevertheless, there is a resurgence of interest in open approaches, particularly in exploring external tracheal scaffolding, tracheal transplantation, and other open techniques for tracheobronchial replacement or reconstruction.[60][61][62]
Complications
Potential complications of laryngeal stents include:
- Granulation tissue formation at stent edges (up to 80%) [63]
- Stent dislodgement and potential aspiration
- Stent occlusion by secretions
- Stent-associated infection (most often Staphylococcus aureus or Pseudomonas aeruginosa) [64]
- Stent migration (7%-30%) [65]
- Recurrence of stenosis after stent removal (40%-80%) [66]
- Dysphagia
- Aspiration
The complications that can arise from tracheal stents are similar to those of laryngeal stents. The most common issues are migration and granulation tissue formation, which can lead to restenosis at the end of the stent.[67][68] Potential complications of tracheal stents include:
- Granulation tissue formation
- Stent migration (17%-50%) [69]
- Stent dislodgement and potential aspiration
- Stent occlusion by secretions
- Tracheoinnominate fistula (rare; 0.1%-1% rate) [70]
- Tracheoesophageal fistula (up to 39% recurrence rate if the stent was placed to treat a fistula initially) [71]
- Recurrence of stenosis formation (67%-90%) [68]
- Stent fracture (~10%) [67]
Clinical Significance
Laryngeal and tracheal stents serve distinct purposes, yet both are frequently employed to support the airway during the postoperative phase following reconstructive surgery. Tracheal stents, commonly utilized in palliative care, prove beneficial for patients grappling with end-stage airway disease or malignancies encroaching upon the airway lumen. Interventional pulmonologists or cardiothoracic surgeons typically undertake the insertion of these stents in such patient populations.
Currently, no standardized recommendations dictate the optimal stent characteristics for these scenarios. The determination of stent type and material remains a nuanced decision guided by the unique circumstances of each patient. Ongoing research endeavors are concentrated on developing an ideal stent capable of ensuring a patent airway, offering a range of sizes, expanding effectively, minimizing complications, and eliciting minimal tissue reaction.
Enhancing Healthcare Team Outcomes
In the management of laryngeal and tracheal stents, it is crucial to have a collaborative and interprofessional approach to ensure optimum patient-centered care, favorable outcomes, patient safety, and effective team performance. Physicians play a critical role in the initial diagnosis, treatment planning, and decision-making regarding the type and placement of stents based on the patient's condition. Advanced practitioners, including nurse practitioners or physician assistants, contribute to the care continuum by assisting in patient assessments, monitoring stent-related complications, and ensuring adherence to treatment plans. Nurses are pivotal in patient education, postoperative care, and ongoing monitoring, bridging patients and the broader healthcare team. Pharmacists are integral in managing medications, ensuring appropriate drug interactions, and promoting medication safety.
Interprofessional communication is paramount, facilitating the exchange of critical information among team members, which enhances care coordination. Regular team meetings and case discussions enable shared decision-making and the alignment of treatment goals. This collaborative approach helps address any emerging issues promptly, improving patient safety and overall outcomes. Additionally, a coordinated effort ensures that patient care is seamless and consistent across various healthcare settings, from initial diagnosis to postoperative follow-up, enhancing the overall quality of care for individuals with laryngeal and tracheal stents.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
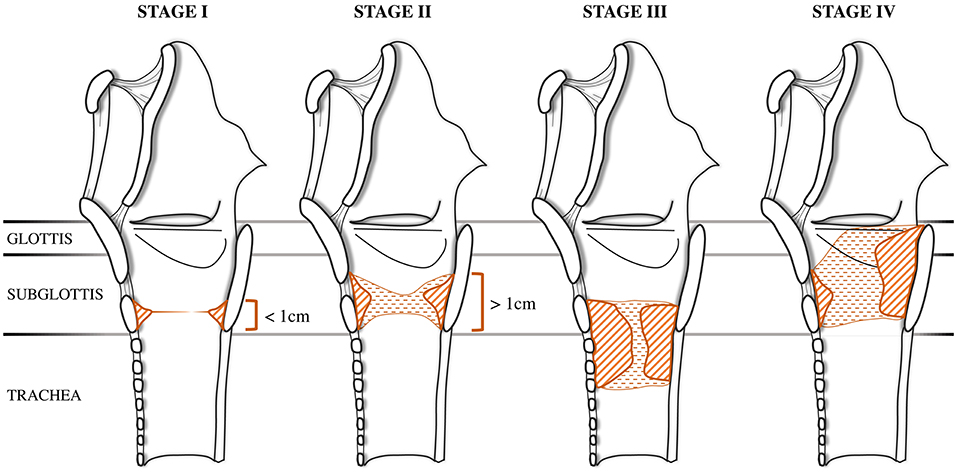
McCaffrey Classification. The McCaffrey classification is used to describe the extension of the stenosis among the most commonly involved subsites: the glottis, the subglottis, and the trachea.
Filauro M, Mazzola F, Missale F, Canevari FR, Peretti G. Endoscopic preoperative assessment, classification of stenosis, decision-making. Front Pediatr. 2020;7:532. doi: 10.3389/fped.2019.00532.
References
Courey MS. Airway obstruction. The problem and its causes. Otolaryngologic clinics of North America. 1995 Aug:28(4):673-84 [PubMed PMID: 7478630]
McCullagh KL, Shah RN, Huang BY. Anatomy of the Larynx and Cervical Trachea. Neuroimaging clinics of North America. 2022 Nov:32(4):809-829. doi: 10.1016/j.nic.2022.07.011. Epub [PubMed PMID: 36244725]
Bacchin D, Aprile V, Lenzini A, Korasidis S, Mastromarino MG, Picchi A, Fanucchi O, Ribechini A, Ambrogi MC, Lucchi M. Surgical treatment of tracheal stenosis during Covid-19 era: a single-center experience and lessons learnt on the field. Updates in surgery. 2023 Sep:75(6):1681-1690. doi: 10.1007/s13304-023-01577-6. Epub 2023 Jul 17 [PubMed PMID: 37458903]
Pandya A, Sreevidya SR, Chaudhari N, Prajapati BJ, Gupta N. Laryngotracheal Stenosis: Our Experience in a Tertiary Care Hospital. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 2023 Mar:75(1):39-44. doi: 10.1007/s12070-022-03445-y. Epub 2022 Dec 31 [PubMed PMID: 37007876]
Talatala ERR, Clark E, Ye W, Davis RJ, Hillel AT, Collins SL, Ramirez-Solano M, Sheng Q, Gelbard A. Localizing Hormone Receptor Expression to Cellular Compartments in Idiopathic Subglottic Stenosis. The Laryngoscope. 2023 Dec:133(12):3506-3511. doi: 10.1002/lary.30856. Epub 2023 Jun 29 [PubMed PMID: 37382162]
Krishnan A, Guenthart BA, Choi A, Trope W, Berry GJ, Pinezich MR, Vunjak-Novakovic G, Shaller B, Sung CK, Liou DZ, Damrose EJ, Lui NS. Tracheal stenosis and airway complications in the Coronavirus Disease-19 era. Annals of thoracic surgery short reports. 2023 Jun 7:():. doi: 10.1016/j.atssr.2023.05.013. Epub 2023 Jun 7 [PubMed PMID: 37360840]
Thawley SE, Ogura JH. Panel discussion: the management of advanced laryngotracheal stenosis. Use of the hyoid graft for treatment of laryngotracheal stenosis. The Laryngoscope. 1981 Feb:91(2):226-32 [PubMed PMID: 7464385]
Simpson GT, Strong MS, Healy GB, Shapshay SM, Vaughan CW. Predictive factors of success or failure in the endoscopic management of laryngeal and tracheal stenosis. The Annals of otology, rhinology, and laryngology. 1982 Jul-Aug:91(4 Pt 1):384-8 [PubMed PMID: 7114718]
Prasanna Kumar S, Ravikumar A, Senthil K, Somu L, Nazrin MI. Role of Montgomery T-tube stent for laryngotracheal stenosis. Auris, nasus, larynx. 2014 Apr:41(2):195-200. doi: 10.1016/j.anl.2013.10.008. Epub 2013 Oct 27 [PubMed PMID: 24172854]
Level 2 (mid-level) evidenceTinga S, Thieman Mankin KM, Peycke LE, Cohen ND. Comparison of Outcome After Use of Extra-Luminal Rings and Intra-Luminal Stents for Treatment of Tracheal Collapse in Dogs. Veterinary surgery : VS. 2015 Oct:44(7):858-65. doi: 10.1111/vsu.12365. Epub 2015 Aug 6 [PubMed PMID: 26249528]
Folch E, Keyes C. Airway stents. Annals of cardiothoracic surgery. 2018 Mar:7(2):273-283. doi: 10.21037/acs.2018.03.08. Epub [PubMed PMID: 29707506]
Sung YN, Kim Y, Cho KJ, Sim J. Assessment of thyroid cartilage ossification pattern in cancer patients: A suggestion of active ossification by tumor progression. Head & neck. 2023 Aug:45(8):2040-2046. doi: 10.1002/hed.27430. Epub 2023 Jun 23 [PubMed PMID: 37353470]
Paniello RC, Brookes S, Zhang H, Halum S. Enhanced Abductor Function in Bilateral Vocal Fold Paralysis with Muscle Stem Cells. The Laryngoscope. 2024 Jan:134(1):324-328. doi: 10.1002/lary.30885. Epub 2023 Jul 18 [PubMed PMID: 37462328]
Coviello CM, Sheehan C, Hernandez DJ, Liou NE, Sandulache VC, Haskins AD, Sturgis EM, Huang AT. Outcome Comparison of Functional Laryngectomy for the Dysfunctional Larynx to Salvage Laryngectomy. The Laryngoscope. 2024 Jan:134(1):222-227. doi: 10.1002/lary.30844. Epub 2023 Jun 22 [PubMed PMID: 37345670]
Suzuki K, Yambe N, Hojo K, Komatsu Y, Serikawa M, Usami A. Anatomical morphometry for Cricothyrotomy puncture and incision. BMC surgery. 2023 Jul 12:23(1):198. doi: 10.1186/s12893-023-02100-9. Epub 2023 Jul 12 [PubMed PMID: 37438728]
Voets PJ, van Helvoort HA. The role of equal pressure points in understanding pulmonary diseases. Advances in physiology education. 2013 Sep:37(3):266-7. doi: 10.1152/advan.00014.2013. Epub [PubMed PMID: 24022774]
Level 3 (low-level) evidenceMyer CM 3rd, O'Connor DM, Cotton RT. Proposed grading system for subglottic stenosis based on endotracheal tube sizes. The Annals of otology, rhinology, and laryngology. 1994 Apr:103(4 Pt 1):319-23 [PubMed PMID: 8154776]
Li Y, Zhu M, Chen J, Ren K, Wan L, Lu H, Ren J, Han X. Single Y-shaped tracheal self-expandable metallic stent for emergent carinal stenosis combined with stenosis of the right main and intermediate bronchi. Medicine. 2020 May 29:99(22):e20498. doi: 10.1097/MD.0000000000020498. Epub [PubMed PMID: 32481466]
Tsakiridis K, Darwiche K, Visouli AN, Zarogoulidis P, Machairiotis N, Christofis C, Stylianaki A, Katsikogiannis N, Mpakas A, Courcoutsakis N, Zarogoulidis K. Management of complex benign post-tracheostomy tracheal stenosis with bronchoscopic insertion of silicon tracheal stents, in patients with failed or contraindicated surgical reconstruction of trachea. Journal of thoracic disease. 2012 Nov:4 Suppl 1(Suppl 1):32-40. doi: 10.3978/j.issn.2072-1439.2012.s002. Epub [PubMed PMID: 23304439]
Thomas GK, Stevens MH. Stenting in experimental laryngeal injuries. Archives of otolaryngology (Chicago, Ill. : 1960). 1975 Apr:101(4):217-21 [PubMed PMID: 1120009]
Level 3 (low-level) evidenceFroehlich P, Truy E, Stamm D, Floret D, Morgon A. Role of long-term stenting in treatment of pediatric subglottic stenosis. International journal of pediatric otorhinolaryngology. 1993 Oct:27(3):273-80 [PubMed PMID: 8270365]
Level 2 (mid-level) evidenceWahidi MM, Ernst A. The Montgomery T-tube tracheal stent. Clinics in chest medicine. 2003 Sep:24(3):437-43 [PubMed PMID: 14535218]
Hu H,Zhang J,Wu F,Chen E, Application of the Montgomery T-tube in subglottic tracheal benign stenosis. Journal of thoracic disease. 2018 May; [PubMed PMID: 29997975]
Zalzal GH, Grundfast KM. Broken Aboulker stents in the tracheal lumen. International journal of pediatric otorhinolaryngology. 1988 Nov:16(2):125-30 [PubMed PMID: 3209360]
Level 3 (low-level) evidenceWilcox JD, Nassar M. A Modified Laryngeal Stent for Glotto-Subglottic Stenosis: A Novel Stent for Better Outcomes. Ear, nose, & throat journal. 2021 Sep:100(5_suppl):399S-403S. doi: 10.1177/0145561319883074. Epub 2019 Oct 22 [PubMed PMID: 31637951]
Smith DF, de Alarcon A, Jefferson ND, Tabangin ME, Rutter MJ, Cotton RT, Hart CK. Short- versus Long-term Stenting in Children with Subglottic Stenosis Undergoing Laryngotracheal Reconstruction. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2018 Feb:158(2):375-380. doi: 10.1177/0194599817737757. Epub 2017 Oct 24 [PubMed PMID: 29064319]
Monnier P. A new stent for the management of adult and pediatric laryngotracheal stenosis. The Laryngoscope. 2003 Aug:113(8):1418-22 [PubMed PMID: 12897569]
Alshammari J, Monnier P. Airway stenting with the LT-Mold™ for severe glotto-subglottic stenosis or intractable aspiration: experience in 65 cases. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2012 Dec:269(12):2531-8. doi: 10.1007/s00405-012-2080-x. Epub 2012 Jun 22 [PubMed PMID: 22722945]
Level 3 (low-level) evidenceZalzal GH. Stenting for pediatric laryngotracheal stenosis. The Annals of otology, rhinology, and laryngology. 1992 Aug:101(8):651-5 [PubMed PMID: 1497269]
Sweed AH, Mobashir M, Mohamed AES, Elsayed AI, Elmalt A, Elshora ME. Simple Endoscopic Application of Laryngeal Keel Stent. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2022 Feb:166(2):399-402. doi: 10.1177/01945998211002162. Epub 2021 Mar 23 [PubMed PMID: 33752537]
Dalar L, Tural Önür S, Özdemir C, Sökücü SN, Karasulu AL, Altin S. Is silicone stent insertion a clinically useful option for tracheobronchomalacia? Turkish journal of medical sciences. 2016 Feb 17:46(2):437-42. doi: 10.3906/sag-1412-104. Epub 2016 Feb 17 [PubMed PMID: 27511508]
Miwa K, Takamori S, Hayashi A, Fukunaga M, Shirouzu K. Fixation of silicone stents in the subglottic trachea: preventing stent migration using a fixation apparatus. The Annals of thoracic surgery. 2004 Dec:78(6):2188-90 [PubMed PMID: 15561074]
Andreetti C, Menna C, D'Andrilli A, Ibrahim M, Venuta F, Santini M, Rendina EA, Fiorelli A. A modified technique to simplify external fixation of the subglottic silicone stent. Interactive cardiovascular and thoracic surgery. 2018 Dec 1:27(6):878-880. doi: 10.1093/icvts/ivy178. Epub [PubMed PMID: 29868866]
McGinniss JE, Imai I, Simon-Soro A, Brown MC, Knecht VR, Frye L, Ravindran PM, Dothard MI, Wadell DA, Sohn MB, Li H, Christie JD, Diamond JM, Haas AR, Lanfranco AR, DiBardino DM, Bushman FD, Collman RG. Molecular analysis of the endobronchial stent microbial biofilm reveals bacterial communities that associate with stent material and frequent fungal constituents. PloS one. 2019:14(5):e0217306. doi: 10.1371/journal.pone.0217306. Epub 2019 May 29 [PubMed PMID: 31141557]
Cotton RT, Myer CM 3rd, Bratcher GO, Fitton CM. Anterior cricoid split, 1977-1987. Evolution of a technique. Archives of otolaryngology--head & neck surgery. 1988 Nov:114(11):1300-2 [PubMed PMID: 3166763]
Kurien M, Raviraj R, Mathew J, Kaliaperumal I, Ninan S. Modified endotracheal tube: emergency alternative to paediatric tracheostomy tube. The Journal of laryngology and otology. 2011 Jul:125(7):729-31. doi: 10.1017/S0022215111000636. Epub 2011 Apr 13 [PubMed PMID: 21486520]
Level 3 (low-level) evidenceAwasthy N, Arora HS, Radhakrishnan S. Endotracheal tube as tracheal stent in vascular ring. Asian cardiovascular & thoracic annals. 2016 Feb:24(2):195-7. doi: 10.1177/0218492314554238. Epub 2014 Oct 3 [PubMed PMID: 25281764]
Level 3 (low-level) evidencePhillips MJ. Stenting therapy for stenosing airway diseases. Respirology (Carlton, Vic.). 1998 Dec:3(4):215-9 [PubMed PMID: 10201046]
Lim LH, Cotton RT, Azizkhan RG, Wood RE, Cohen AP, Rutter MJ. Complications of metallic stents in the pediatric airway. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2004 Oct:131(4):355-61 [PubMed PMID: 15467599]
Level 3 (low-level) evidenceChin CS, Litle V, Yun J, Weiser T, Swanson SJ. Airway stents. The Annals of thoracic surgery. 2008 Feb:85(2):S792-6. doi: 10.1016/j.athoracsur.2007.11.051. Epub [PubMed PMID: 18222219]
Hramiec JE, Haasler GB. Tracheal wire stent complications in malacia: implications of position and design. The Annals of thoracic surgery. 1997 Jan:63(1):209-12; discussion 213 [PubMed PMID: 8993267]
Level 3 (low-level) evidenceBi Y, Li J, Bai L, Han X, Ren J. Long-term outcomes of tracheal stents removal under fluoroscopy guidance: comparison of tracheal fistulas and tracheal stenosis. BMC pulmonary medicine. 2021 Jan 7:21(1):14. doi: 10.1186/s12890-020-01349-7. Epub 2021 Jan 7 [PubMed PMID: 33413278]
Choi MJ, Kang H. CT Findings of Central Airway Lesions Causing Airway Stenosis-Visualization and Quantification: A Pictorial Essay. Taehan Yongsang Uihakhoe chi. 2021 Nov:82(6):1441-1476. doi: 10.3348/jksr.2020.0212. Epub 2021 Sep 16 [PubMed PMID: 36238875]
Nair S, Mohan S, Mandal G, Nilakantan A. Tracheal stenosis: our experience at a tertiary care centre in India with special regard to cause and management. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 2014 Jan:66(1):51-6. doi: 10.1007/s12070-013-0663-5. Epub 2013 Jun 15 [PubMed PMID: 24605302]
Moore AE, Walker A, Kanotra SP. Endoscopic Versus Open Surgical Intervention for Congenital Laryngeal Webs: A Systematic Review and Meta-Analysis. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2023 Aug:169(2):227-233. doi: 10.1002/ohn.279. Epub 2023 Feb 7 [PubMed PMID: 36939597]
Level 1 (high-level) evidenceLorenz RR. The Evolution and Outcomes of the "Maddern Procedure" for the Treatment of Subglottic Stenosis. The Laryngoscope. 2023 Nov:133(11):3100-3108. doi: 10.1002/lary.30752. Epub 2023 May 17 [PubMed PMID: 37194674]
Rutter MJ, Cotton RT. The use of posterior cricoid grafting in managing isolated posterior glottic stenosis in children. Archives of otolaryngology--head & neck surgery. 2004 Jun:130(6):737-9 [PubMed PMID: 15210555]
Level 2 (mid-level) evidenceWei W, Li X, Feng L, Jiao J, Li W, Cai Y, Fang R, Han Y. The effect of intraoperative transnasal humidified rapid-insufflation ventilatory exchange on emergence from general anesthesia in patients undergoing microlaryngeal surgery: a randomized controlled trial. BMC anesthesiology. 2023 Jun 13:23(1):202. doi: 10.1186/s12871-023-02169-y. Epub 2023 Jun 13 [PubMed PMID: 37312020]
Level 1 (high-level) evidenceDavis RJ, Lina I, Motz K, Gelbard A, Lorenz RR, Sandhu GS, Hillel AT. Endoscopic Resection and Mucosal Reconstitution With Epidermal Grafting: A Pilot Study in Idiopathic Subglottic Stenosis. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2022 May:166(5):917-926. doi: 10.1177/01945998211028163. Epub 2021 Jul 13 [PubMed PMID: 34253069]
Level 3 (low-level) evidenceLiang KY, Nelson RC, Bryson PC, Lorenz RR. High Tracheal Resection With Intralaryngeal Extension as an Alternative to Cricotracheal Resection for Treatment of Subglottic Stenosis. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2023 May:168(5):1139-1145. doi: 10.1002/ohn.180. Epub 2023 Jan 19 [PubMed PMID: 36939535]
Redmann AJ, Moore C, Kou YF, Tabangin ME, Wilcox L, Smith MM, Hart CK, Rutter MJ, de Alarcon A. Revision Endoscopic Posterior Costal Cartilage Grafting: Is It Feasible? Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2023 Aug:169(2):432-434. doi: 10.1002/ohn.275. Epub 2023 Feb 7 [PubMed PMID: 36939543]
Jethwa AR, Hasan W, Palme CE, Mäkitie AA, Espin-Garcia O, Goldstein DP, Gilbert RW, Keshavjee S, Pierre A, Gullane PJ. Cricotracheal resection for adult subglottic stenosis: Factors predicting treatment failure. The Laryngoscope. 2020 Jul:130(7):1634-1639. doi: 10.1002/lary.28273. Epub 2019 Sep 9 [PubMed PMID: 31498456]
Tan LT, Xie Y, Li Q, Chen C. [Outcomes of laryngotracheal reconstruction with anterior and posterior costal cartilage grafts in severe pediatric subglottic stenosis or laryngeal web]. Zhonghua er bi yan hou tou jing wai ke za zhi = Chinese journal of otorhinolaryngology head and neck surgery. 2023 Jul 7:58(7):699-704. doi: 10.3760/cma.j.cn115330-20221124-00708. Epub [PubMed PMID: 37455115]
Ravikumar N, Ho E, Wagh A, Murgu S. The role of bronchoscopy in the multidisciplinary approach to benign tracheal stenosis. Journal of thoracic disease. 2023 Jul 31:15(7):3998-4015. doi: 10.21037/jtd-22-1734. Epub 2023 Jun 28 [PubMed PMID: 37559626]
Hautmann H, Bauer M, Pfeifer KJ, Huber RM. Flexible bronchoscopy: a safe method for metal stent implantation in bronchial disease. The Annals of thoracic surgery. 2000 Feb:69(2):398-401 [PubMed PMID: 10735670]
Li J, Xu K, Li Z, Li Y, Zhou X, Liu J, Yao Y, Liu Z, Jiao DC, Han X. Intraoperative cone beam computed tomography of tracheal stenting for stenosis and fistula diseases: a retrospective cohort study. Quantitative imaging in medicine and surgery. 2022 May:12(5):2709-2720. doi: 10.21037/qims-21-858. Epub [PubMed PMID: 35502374]
Level 2 (mid-level) evidenceMarchese R, Poidomani G, Palumbo VD, Lo Nigro C, Caterino U, Lo Monte AI, Cajozzo M. Secondary Carina and Lobar Bronchi Stenting in Patients with Advanced Lung Cancer: Is It Worth the Effort? A Clinical Experience. Annals of thoracic and cardiovascular surgery : official journal of the Association of Thoracic and Cardiovascular Surgeons of Asia. 2020 Dec 20:26(6):320-326. doi: 10.5761/atcs.oa.19-00040. Epub 2020 May 18 [PubMed PMID: 32418926]
Jung HS, Chae G, Kim JH, Park CY, Lim S, Park SE, Kim HC, Lee YJ, Kang SK, Kim DH, Lee Y, Lee T. The mechanical characteristics and performance evaluation of a newly developed silicone airway stent (GINA stent). Scientific reports. 2021 Apr 12:11(1):7958. doi: 10.1038/s41598-021-87142-w. Epub 2021 Apr 12 [PubMed PMID: 33846477]
Lin J, Frye L. The intersection of bronchoscopy and extracorporeal membrane oxygenation. Journal of thoracic disease. 2021 Aug:13(8):5176-5182. doi: 10.21037/jtd-2019-ipicu-08. Epub [PubMed PMID: 34527357]
Ren J, Xu Y, Zhiyi G, Ren T, Ren J, Wang K, Luo Y, Zhu M, Tan Q. Reconstruction of the trachea and carina: Surgical reconstruction, autologous tissue transplantation, allograft transplantation, and bioengineering. Thoracic cancer. 2022 Feb:13(3):284-295. doi: 10.1111/1759-7714.14315. Epub 2022 Jan 13 [PubMed PMID: 35023311]
Khalid T, Soriano L, Lemoine M, Cryan SA, O'Brien FJ, O'Leary C. Development of tissue-engineered tracheal scaffold with refined mechanical properties and vascularisation for tracheal regeneration. Frontiers in bioengineering and biotechnology. 2023:11():1187500. doi: 10.3389/fbioe.2023.1187500. Epub 2023 Jun 6 [PubMed PMID: 37346796]
Murray P. The trachea transplant scandal and "compassionate use". BMJ (Clinical research ed.). 2023 Aug 10:382():1808. doi: 10.1136/bmj.p1808. Epub 2023 Aug 10 [PubMed PMID: 37562813]
Li ZM, Jiao DC, Han XW, Lu HB, Ren KW, Yang H. Clinical evaluation the success rate and complications of fluoroscopically guided removal of tracheal tube metallic stents. Journal of cardiothoracic surgery. 2021 Mar 25:16(1):54. doi: 10.1186/s13019-021-01444-8. Epub 2021 Mar 25 [PubMed PMID: 33766043]
Nouraei SA, Petrou MA, Randhawa PS, Singh A, Howard DJ, Sandhu GS. Bacterial colonization of airway stents: a promoter of granulation tissue formation following laryngotracheal reconstruction. Archives of otolaryngology--head & neck surgery. 2006 Oct:132(10):1086-90 [PubMed PMID: 17043256]
Rampey AM, Silvestri GA, Gillespie MB. Combined endoscopic and open approach to the removal of expandable metallic tracheal stents. Archives of otolaryngology--head & neck surgery. 2007 Jan:133(1):37-41 [PubMed PMID: 17224520]
Pasick LJ, Anis MM, Rosow DE. An Updated Review of Subglottic Stenosis: Etiology, Evaluation, and Management. Current pulmonology reports. 2022:11(2):29-38. doi: 10.1007/s13665-022-00286-6. Epub 2022 Mar 3 [PubMed PMID: 35261874]
Ho S, Goh SK, Ng AW, Tai DY, Lim AY, Kor AC, Sien Zin NN, Abisheganaden J, Verma A. Long-term tolerance of a fractured self-expanding metal stent in a patient with adenoid cystic carcinoma. Respiratory medicine case reports. 2019:28():100960. doi: 10.1016/j.rmcr.2019.100960. Epub 2019 Oct 25 [PubMed PMID: 31720207]
Level 3 (low-level) evidenceSriram K, Robinson P. Recurrent airway obstructions in a patient with benign tracheal stenosis and a silicone airway stent: a case report. Cases journal. 2008 Oct 7:1(1):226. doi: 10.1186/1757-1626-1-226. Epub 2008 Oct 7 [PubMed PMID: 18840299]
Level 3 (low-level) evidenceBiswas A, Jantz MA, Fernandez-Bussy S, Flanagan M, Mehta HJ. Repositioning of migrated self-expanding metallic tracheobronchial stent: predictors of a successful maneuver and its impact on survival. Journal of thoracic disease. 2020 May:12(5):1866-1876. doi: 10.21037/jtd-20-608. Epub [PubMed PMID: 32642090]
Grant CA, Dempsey G, Harrison J, Jones T. Tracheo-innominate artery fistula after percutaneous tracheostomy: three case reports and a clinical review. British journal of anaesthesia. 2006 Jan:96(1):127-31 [PubMed PMID: 16299043]
Level 3 (low-level) evidenceChaddha U, Hogarth DK, Murgu S. Perspective on airway stenting in inoperable patients with tracheoesophageal fistula after curative-intent treatment for esophageal cancer. Journal of thoracic disease. 2019 May:11(5):2165-2174. doi: 10.21037/jtd.2018.12.128. Epub [PubMed PMID: 31285911]
Level 3 (low-level) evidence