Anatomy, Shoulder and Upper Limb, Arm Structure and Function
Anatomy, Shoulder and Upper Limb, Arm Structure and Function
Introduction
The upper extremity or arm is a functional unit of the upper body. It consists of three sections: the upper arm, forearm, and hand. It extends from the shoulder joint to the fingers and contains 30 bones. It also consists of many nerves, blood vessels (arteries and veins), and muscles. The nerves of the arm are supplied by one of the two major nerve plexus of the human body, the brachial plexus.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The upper extremity begins at the shoulder joint. This joint is commonly referred to as a ball-and-socket joint, although it is more correctly described as a ball-and-saucer joint. In contrast to the hip, the other ball-and-socket joint of the body, the socket is much shallower. This allows for less restriction of movement at the joint but compromises stability in the process. The elbow joint is referred to by many as a hinge joint. This is partially true but does not explain the ability to pronate and supinate the forearm at the elbow joint. The articulation of the radial head and the radial notch on the ulna allows for this motion. This creates what is called a "pivot" joint, allowing the movement of one bone on another. The wrist joint can be classified as an ellipsoidal or condyloid joint. There are also joints of the carpal bones, which are referred to as intercarpal joints. Even though they are synovial joints, they do not allow much movement. The interphalangeal joints are basic hinge joints.[1][2][3]
Embryology
During the third week of development, the trilaminar embryonic disc is formed. Three layers, the endoderm, mesoderm, and ectoderm, are differentiated. The notochord is formed from mesoderm, and the overlying ectoderm becomes the neural plate. During the fourth week, the upper and lower limb buds begin to form. Muscle, bone, blood vessels, and lymphatics are all formed from the mesoderm, while the peripheral nerves are differentiated neural crest cells.
Thirty bones in total make up the structure of the upper extremity. They act as a framework for the muscles, blood vessels, nerves, and lymphatics. There is one bone in the upper arm region, the humerus. The forearm contains two bones, the radius and the ulna. When picturing the upper extremity in a standard anatomical position with the palm of the hand facing forward, the radius is located laterally and the ulna medially. However, because the forearm allows rotation around a central axis, the terms radial and ulnar provide a better description when describing the direction or location of the forearm, wrist, and hand. The wrist and hand contain 27 bones. There are eight carpal bones organized into a proximal and distal row. The proximal bones, from radial (thumb side) to ulnar are the scaphoid (navicular), lunate, triquetrum, and pisiform. From radial to ulnar, the distal row consists of the trapezium, trapezoid, capitate, and hamate. There are five metacarpal bones, each associated with a group of phalanges. There are also 14 phalanx bones. Fingers two to five have a proximal, intermediate, and distal phalanx, while the thumb has only a proximal and distal phalanx. Although many bony injuries can result, the most clinically significant are injuries to the humerus and scaphoid bones. Injuries at the neck of the humerus can result in axillary nerve injury. Midshaft fractures will damage the radial nerve, and supracondylar fractures can damage the median nerve (a common mnemonic is "ARM"). Another common clinical pathology is an injury to the scaphoid. Not only is it the most commonly injured carpal bone, but it also is a common site of avascular necrosis due to its retrograde blood supply. This commonly occurs in fall on an outstretched hand (FOOSH) injuries.
Blood Supply and Lymphatics
The arterial supply of the upper extremity starts with the subclavian artery. The subclavian has a complicated course through the axilla, changing names twice before it gets to the upper arm. As it passes the one rib, it becomes the axillary artery. In the axilla, it passes deep to the pectoralis minor muscle toward the humerus. It gives off the anterior and posterior circumflex humeral arteries before coursing posteriorly around the humeral head, giving rise to its largest branch, the subscapular artery. As it passes the teres minor, it becomes the brachial artery. At this point, it gives off the profundal brachii, which supplies the deep structures of the arm. It then travels along the humerus in the radial groove, along with the radial nerve. As it passes into the elbow, near the median nerve, it courses deep to the brachialis and splits into 2 branches, the radial (lateral branch) and ulnar (medial branch). The radial artery courses down the arm and supplies the deep palmar arch, while the ulnar artery supplies the superficial palmar arch. Due to its many anastomosing arteries, there are not many clinical correlates to the arterial injury of the upper extremity.
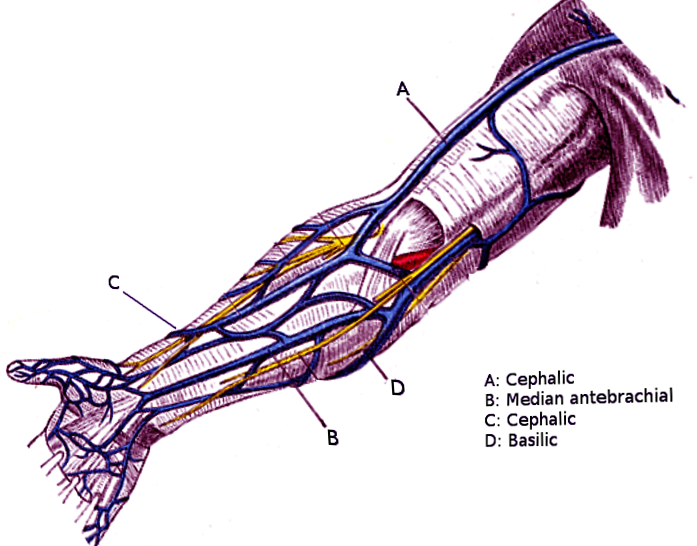
The venous drainage of the upper extremity is accomplished via two large veins. The first, the basilic vein, is formed by the radial and ulnar veins. It courses along the medial side of the arm, where it meets with the brachial veins, forming the axillary vein. The cephalic vein arises around the hand and transverses the anterior-lateral area of the upper limb. It eventually courses between the pectoral and deltoid muscles, dumping into the axillary vein. The median cubital vein is a vein that is commonly used as a venipuncture site. It is a branch connecting the cephalic and basilic veins.
Nerves
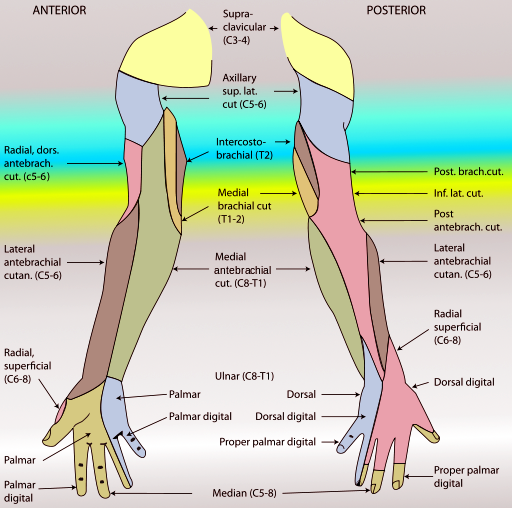
The brachial plexus supplies all the nerves in the upper extremity. It is formed by the anterior rami of spinal nerve levels C5 through T1. The brachial plexus is divided into five subdivisions: the roots, trunks, divisions, cords, and branches. The roots, as stated earlier, are C5 through T1. There are three trunks: the superior (C5 and C6), middle (C7), and inferior (C8 and T1). Each cord divides anteriorly or posteriorly, thus creating the anterior and posterior division of each. These combine to form the cords. The posterior divisions of the three trunks combine to form the posterior cord. The anterior divisions of the superior and middle trunk combine to form the lateral cord, and the anterior division of the inferior trunk continues as the medial cord. The five major branches of the plexus are the musculocutaneous, axillary, median, radial, and ulnar nerve. The lateral cord splits to give half of the median nerve and continues as the musculocutaneous nerve. The medial cord also splits, giving off the other half of the median nerve, as it continues as the ulnar nerve. The posterior cord splits to form the axillary and radial nerve. The brachial plexus also supplies other nerves besides the five major branches. The dorsal scapular nerve arises from the C5 nerve root, and the long thoracic nerve is made up of the C5 to C7 roots. The superior trunk gives off the suprascapular nerve and nerve to subclavius. The lateral pectoral nerve branches from the lateral cord, while the medial pectoral nerve, as well as the medial cutaneous nerve of the arm and forearm, come from the medial cord. The posterior cord also has 3 nerves that originate from it: the upper and lower subscapular and the thoracodorsal nerve. Clinical issues with the brachial plexus sometimes are seen in childbirth. Erb palsy is caused by traction/tear of the upper trunk, resulting in damage to the C5 and C6 nerve roots, and is commonly associated with infant neck traction during delivery. Klumpke palsy occurs when traction on the upper extremity results in tearing of the C8 and T1 roots, usually with an upward pull of the infant's arm on the way out of the birth canal.[4][5][6]
Nerve roots C5 to C7 supply the musculocutaneous nerve. As it moves distally down the upper arm, it pierces the coracobrachialis from deep to superior. It courses between the biceps brachii and brachialis muscle, eventually turning into the lateral cutaneous nerve as it passes lateral to the biceps tendon. In total, it provides motor innervation to the three muscles of the anterior arm, the biceps brachii, brachialis, and coracobrachialis, as well as sensory innervation to the radial side of the forearm. Although lesions of this nerve are rare in clinical practice, they would they would theoretically result in weakened flexion and supination at the elbow joint, although it would not be absent due to the actions of the brachioradialis and supinator muscles. There would also be a sensory loss over the radial side of the forearm.
Nerve roots of C5 and C6 supply the axillary nerve. As it courses through the axilla, it transverses between the axillary artery posteriorly and the subscapularis muscles anteriorly. It then exits posteriorly through the quadrangular space, accompanied by the posterior circumflex humeral artery. The axillary nerve supplies the deltoid muscle, as well as one of the four rotator cuff muscles, the teres minor. It also provides sensory innervation via the upper lateral cutaneous nerve of the arm. The axillary nerve is commonly damaged via trauma to the shoulder or dislocation of the humerus. Injury results in failure of abduction of the arm as well as atrophy of the deltoid and loss of sensation in the upper lateral arm.
The median nerve is derived from nerve roots C6 through TI. It innervates the flexor muscles of the anterior forearm. A major exception to this rule is the flexor digitorum profundus, which is the only muscle in the anterior compartment innervated by the ulnar nerve. The median nerve courses from the axilla down the anterior arm, lateral to the brachial artery. Midway down the arm, it crosses the artery anteriorly, entering the anterior forearm through the cubital fossa. In the forearm, the nerve course between the flexor digitorum superficialis and profundus muscles, giving rise to two branches: the anterior interosseous nerve, which supplies the deep compartment of the anterior forearm, and the palmar cutaneous nerve, which innervates the skin over the radial surface of the palm. It then continues distally through the carpal tunnel, where it splits into two more branches: the recurrent branch, which supplies the thenar muscles, and the palmar digital branch, which supplies sensory innervation to the radial 3.5 digits and the palmar surface as well as motor innervation to the two radial lumbricals. Compression of the median nerve at the site of the carpal tunnel by the flexor retinaculum causes carpal tunnel syndrome. This pathology results in tingling, pain, and numbness in the distribution of the median nerve distally to the wrist. This can be treated conservatively in most cases, with splinting of the wrist. Corticosteroid injections can also manage it. Refractory cases may need to be managed by surgical decompression via flexor retinaculum release by an experienced orthopedic surgeon. The nerve is also commonly damaged via trauma to the elbow and lacerations at the wrist.
The radial nerve has supply from every root of the brachial plexus, C5 through TI. It arises from the axillary region and courses with the axillary artery, exiting posteriorly. It travels down the posterior surface of the humerus in the radial groove. It then wraps laterally around the arm, where it meets and courses near the brachial artery. It then courses over the lateral epicondyle, where it splits into the deep and superficial branches. The deep branch supplies motor innervation to most of the muscles in the posterior compartment of the forearm, while the superficial branch supplies sensory innervation to the posterior surface of the hand and fingers. In the course of the radial nerve down the arm, it also supplies cutaneous innervation via the lower lateral cutaneous nerve of the arm, the posterior cutaneous nerve of the arm, and the posterior cutaneous nerve of the forearm, besides the superficial branch. The radial nerve is commonly injured in midshaft fractures of the humerus, which results in motor deficits to the triceps and extensor muscles of the forearm and wrist drop.
The ulnar nerve contains fibers from spinal roots C8 and T1. It courses down the humerus and over the medial epicondyle. It then pierces the flexor carpi ulnaris and gives way to three branches in the forearm: the muscular branch and the palmar and dorsal cutaneous branches. As it courses down the forearm, it innervates the ulnar half of the flexor digitorum profundus muscle and the flexor carpi ulnaris. As it transverses the wrist, it travels superficial to the flexor retinaculum, into the hand, where it innervates the hypothenar muscles, the ulnar two lumbricals, and the interossei muscle. The cutaneous branches given off also supply the sensation to the ulnar 1/5 fingers. The ulnar nerve is most commonly damaged at the elbow, although damage can also result from lacerations to the wrist. It is also a common nerve palsy seen in bike riders because the ulnar nerve is compressed as it travels through the Guyon canal. There are various presentations of ulnar nerve injury, depending on the location of the injury.
Muscles
The musculature of the upper limb is quite vast, much more so than the lower extremity. The upper arm contains three muscles in the anterior compartment. The long and short heads of the biceps brachii are located superiorly, while the coracobrachialis and brachialis are deep to the biceps. The posterior compartment contains only one muscle, the triceps brachii. The forearm consists of 20 muscles, separated into five compartments. Biceps brachii tendon rupture is a common pathology seen with flexion at the elbow. Patients typically present with a bulge in the anterior arm, sometimes referred to as the "Popeye sign," after hearing a loud pop during the injury.
The anterior forearm consists of four muscles in the superficial group: flexor carpi radialis, flexor carpi ulnaris, palmaris longus, and pronator teres. The lone muscle in the intermediate/middle compartment is the flexor digitorum superficialis. The deep layer of the anterior compartment contains three muscles: flexor digitorum profundus, flexor pollicus longus, and pronator quadratus. These muscles consist mainly of flexor and pronator muscles, and most of the superficial muscles arise from a common flexor tendon on the medial epicondyle of the humerus. Overuse of the superficial flexor muscles can lead to a syndrome known as medial epicondylitis, which is sometimes referred to as "golfer's elbow." Repetitive pronation/flexion leads to pain near the medial epicondyle, which worsens with use.
The posterior forearm is separated into two compartments, superficial and deep, with seven and five muscles, respectively. The superficial compartment consists of anconeus, brachioradialis, extensor carpi radialis longus and brevis, extensor carpi ulnaris, extensor digitorum, and extensor digiti minimi. The deep compartment contains abductor pollicis longus, extensor indicis, extensor pollicis longus and brevis, and supinator. As with the anterior superficial compartment, the majority of the superficial muscles of the posterior compartment arise from a common extensor tendon, this time arising from the lateral epicondyle. The main actions of the muscles in the posterior forearm are extension and supination. Like the flexors in the anterior department, the superficial extensor also can suffer from an overuse injury. This syndrome is referred to as tennis elbow or lateral epicondylitis.
The muscles of the hand can be subdivided into three groups which are muscles of the palm, thenar muscles, and hypothenar muscles. The thenar muscles are located at the thumb and consist of abductor pollicis brevis, flexor pollicis brevis, and opponens pollicis. The median nerve innervates all three of these muscles. The hypothenar muscles are located at the ulnar side of the hand, near the fifth digit or pinky finger. They are the abductor digiti minimi, flexor digiti minimi brevis, and opponens digiti minimi. The ulnar nerve innervates them all. The third group of muscles consists of two single muscles and three groups of muscles. The single muscles are palmaris brevis and adductor pollicis. The first group is the dorsal interossei, which consists of four muscles attaching to the metacarpals, which are responsible for the abduction of the fingers. The second group, the palmar interossei, are three (some anatomy texts report four) muscles located on the anterior surface of the metacarpals. They are responsible for adduction of the fingers. The ulnar nerve innervates both the palmar and dorsal interossei. There are also four lumbrical muscles in the hand. Each of these muscles originates from the tendon of the flexor digitorum profundus and is responsible for the flexion of the finger at the metacarpal-phalangeal joint and extension of the interphalangeal joints. The radial two lumbricals are innervated by the median nerve, while the ulnar nerve innervates the two on the ulnar side. There are no lumbricals associated with the thumb.
Surgical Considerations
Understanding the anatomy of the upper extremity is the most important thing in a surgical setting. Operating safely, with the knowledge of what plane you are in and the neurovascular structures you are working near, will minimize complications during the operation and ultimately improve patient satisfaction and survival. Also, in regards to muscle and tendon repair, knowing the origins and insertions of various muscles allows the surgeon to identify the area in which one is working. Regarding anesthesia in the surgical setting, the knowledge of nerves and the structures they surround allows for better success in peripheral nerve blocks during surgery.[7][8][9]
Clinical Significance
Understanding the anatomy of the arm and the human body as a whole assists physicians in identifying the location of pathology during patient encounters. Identifying weakness or atrophy with anatomical knowledge in mind can assist in locating where and, more importantly, why the problem is occurring. Also, knowing what normal anatomy looks like allows physicians to determine abnormalities in structure. Whether it be emergency room physicians reviewing an x-ray or orthopedic surgeons using intraoperative imaging to determine the proper realignment of a fracture, knowledge of anatomy is of the utmost importance in medicine.
Media
(Click Image to Enlarge)
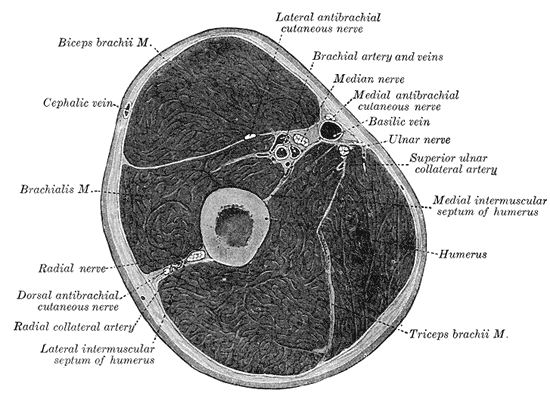
Fascial Compartments of the Arm, Biceps Brachii, Cephalic vein, Brachialis, Radial Nerve, Radial Nerve, Dorsal antebrachial cutaneous nerve, Radial Collateral artery, Lateral intermuscular septum of humerus, Triceps Brachii, Humerus, Medial intermuscular septum of humerus, Superior ulnar collateral artery, Ulnar nerve, Basilic vein, Medial antebrachial cutaneous nerve, Brachial artery and vein, Lateral antebrachial cutaneous nerve.
Henry Vandyke Carter, Public domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Anderson BW, Ekblad J, Black AC, Bordoni B. Anatomy, Appendicular Skeleton. StatPearls. 2024 Jan:(): [PubMed PMID: 30571018]
McCausland C, Sawyer E, Eovaldi BJ, Varacallo M. Anatomy, Shoulder and Upper Limb, Shoulder Muscles. StatPearls. 2024 Jan:(): [PubMed PMID: 30521257]
McGhee DE, Coltman KA, Riddiford-Harland DL, Steele JR. Upper torso pain and musculoskeletal structure and function in women with and without large breasts: A cross sectional study. Clinical biomechanics (Bristol, Avon). 2018 Jan:51():99-104. doi: 10.1016/j.clinbiomech.2017.12.009. Epub 2017 Dec 21 [PubMed PMID: 29287172]
Peterson SL, Rayan GM. Shoulder and upper arm muscle architecture. The Journal of hand surgery. 2011 May:36(5):881-9. doi: 10.1016/j.jhsa.2011.01.008. Epub [PubMed PMID: 21527142]
Ibáñez-Gimeno P, De Esteban-Trivigno S, Jordana X, Manyosa J, Malgosa A, Galtés I. Functional plasticity of the human humerus: shape, rigidity, and muscular entheses. American journal of physical anthropology. 2013 Apr:150(4):609-17. doi: 10.1002/ajpa.22234. Epub 2013 Feb 26 [PubMed PMID: 23440606]
Garner BA, Pandy MG. Musculoskeletal model of the upper limb based on the visible human male dataset. Computer methods in biomechanics and biomedical engineering. 2001 Feb:4(2):93-126 [PubMed PMID: 11264863]
Chauhan M, Anand P, Das JM. Cubital Tunnel Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 30855847]
Lleva JMC, Munakomi S, Chang KV. Ulnar Neuropathy. StatPearls. 2023 Jan:(): [PubMed PMID: 30480959]
DeCastro A, Keefe P. Wrist Drop. StatPearls. 2024 Jan:(): [PubMed PMID: 30422586]