Introduction
Hallux rigidus (Latin for “stiff toe”) is a condition that refers to degenerative arthritis of the first MTP joint.[1] Nicoladoni first described the condition in 1881, but it was popularized in 1887 by Davies Colley, who coined the term hallux flexus to describe the plantarflexed position of the proximal phalanx relative to the metatarsal head.[2] During the same year, Cotterill described the term hallux rigidus to characterize the painful limitation of motion of the first MTP joint.[3] Finally, the term hallux limitus was only reported in 1931 by Hiss.[2] Today, hallux limitus is widely referred to when there is a limitation at the first MTP range of motion, while hallux rigidus is reserved for joints with nearly no movement.
Various etiologies for the condition have been postulated, and an extensive list of treatment options.[4] This review discusses the evaluation and management of each hallux rigidus stage.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Normally, the first MTP joint carries approximately 119% of body weight during gait with each step.[5] This could be aggravated by certain foot structures and biomechanical imbalances, leading to the exacerbation of degenerative arthritis.
Multiple theories have been proposed to explain the cause of hallux rigidus. Coughlin found a strong association between a history of trauma and unilateral involvement of first MTP arthritis.[1] In contrast, bilateral cases have been reported to be most commonly associated with family history and the female gender.[5]
Additional documented etiologies include a flat or chevron-shaped joint, increased hallux interphalangeal angle, longer proximal phalanx, first metatarsal length, and first ray hypermobility.[6][7][8] Metatarsus adductus, equinus deformity, hallux valgus, and footwear are other proposed etiologies with no supportive evidence.
Systemic metabolic and inflammatory conditions such as gout, rheumatoid arthritis, and seronegative arthropathies may also contribute to early degeneration of the joint and should be considered.[1]
Epidemiology
Hallux rigidus is the second most common condition affecting the first MTP joint, after hallux valgus. It affects 25% of patients who are older than 50 and present with foot disorders and is as high as 73% in a population with end-stage ankle arthritis.[9]
Females are twice as likely as men to have hallux rigidus.[5] The condition can occur in adolescence but is uncommon. The condition is associated with osteochondritic lesions when present in the adolescent patient.[10]
In 2021, a cross-sectional study from Japan revealed that knee osteoarthritis, gout attacks, and hallux abducto valgus deformities are strongly correlated to the degeneration of the first metatarsophalangeal joint. In addition, the frequency of knee osteoarthritis was significantly associated with hallux rigidus.[11]
Pathophysiology
Most cases of hallux rigidus are idiopathic. However, multiple authors have noted an association with the development of arthritis changes through both traumatic and iatrogenic causes.[1] The underlying cause is likely multifactorial. Bilateral involvement is more common and is associated with family history and the female gender. Up to two-thirds of patients have a family history of hallux valgus. Achilles contracture, shoe wear, and an elevated metatarsal head also appear to contribute to developing the first MTP joint arthritis.[5]
Histopathology
Although a history of trauma is not always present, similar histological features are noticeable under the microscope. Common characteristics include a cleavage lesion in the articular cartilage with detached subchondral bone at the center of the metatarsal head. The forced extension and axial compression of the dorsal aspect of the proximal phalanx on the convex metatarsal head can produce an osteochondral defect, whether caused by a traumatic event or repetitive microtrauma. Osteochondral lesions are usually located at the center of the metatarsal head, followed by a horseshoe-shaped collar of bone, responsible for the limitation in joint dorsiflexion.[12]
History and Physical
Presentation
- Presenting symptoms include pain, altered gait, and increased bulk of joints, leading to difficulty with shoe wear.
- The compression of the dorsal medial cutaneous nerve may lead to numbness along the medial border of the great toe.
Physical Exam
- As with all foot examinations, neurovascular status should be confirmed. A positive Tinel sign might be present when the medial dorsal cutaneous nerve impinges on the medial aspect of the hallux.
- The first MTP joint is often swollen and tender and may have palpable dorsal osteophytes. There is a decrease in passive and active range of motion (ROM), most commonly in dorsiflexion. The pain usually occurs at terminal ROM with milder diseases. Pain during midrange motion may indicate a more severe arthritic condition due to more global articular wear to the metatarsal head. The production of pain with forced dorsiflexion and the grind test suggest pathology.[13]
- A pronated foot may be noted accompanied by pes planus, but studies have shown no strong association between hallux rigidus and a pronated foot. In contrast, patients with supinated feet have significantly lower odds of suffering from hallux rigidus.[14]
- Dermatologic manifestations could include redness and skin irritation overlying the dorsal osteophyte of the 1st MTP joint, which is likely secondary to shoe gear.
Evaluation
Radiographic Evaluation
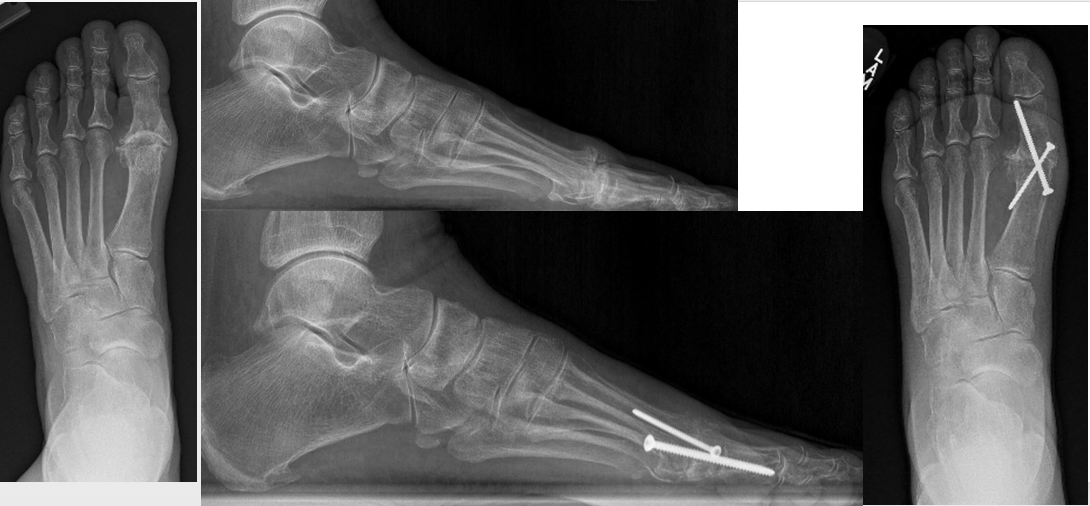
- Weight-bearing plain radiographs in anteroposterior, lateral, and oblique views are indicated (see Image. Mild Hallux Rigidus). The main flaw of plain radiographs is that they do not reveal the site or size of cartilage loss.[13] MRI and CT scans are not required for diagnosis or treatment planning of the disease. An oblique radiograph best determines the extent of joint space narrowing.[5]
Classification
- Coughlin and Shurnas modified Hattrup and Johnson's grading in 2003, offering clinical and radiographic findings of the disease. The Coughlin and Shurnas Clinical Radiographic System for Grading Hallux Rigidus is the most comprehensive grading accepted today.[4] The characteristics of each grade are as follows:
Grade 0
- Dorsiflexion: 40 to 60° or 10% to 20% loss compared to the normal side.
- Radiographic findings: normal
- Clinical Findings: No pain. Stiffness and loss of motion are present on physical examination.
Grade 1
- Dorsiflexion: 30 to 40° or 20% to 50% loss compared to the normal side
- Radiographic findings: Dorsal osteophyte is the main finding. Minimal joint space narrowing, periarticular sclerosis, and flattening of the metatarsal head are present.
- Clinical findings: Mild pain and stiffness, pain at extremes of dorsiflexion or plantar flexion on examination.
Grade 2
- Dorsiflexion: 10 to 30° or 50% to 75% loss compared to the normal side
- Radiographic findings: Dorsal, lateral, and possibly medial osteophytes give a flattened appearance to the metatarsal head. No more than one-fourth of the dorsal joint space is involved on the lateral radiograph. Mild to moderate joint space narrowing and sclerosis are present. The sesamoids are not usually affected.
- Clinical findings: Moderate to severe pain and stiffness that may be constant; pain occurs just before maximum dorsiflexion and maximum plantarflexion on examination
Grade 3
- Dorsiflexion: 10° or less or 75% to 100% loss compared with the normal side. There is a notable loss of metatarsophalangeal plantarflexion as well.
- Radiographic findings: Same as grade 2 but with substantial narrowing, possibly periarticular cystic changes, more than one-fourth of the dorsal joint space involved on the lateral radiograph. The sesamoids are enlarged, cystic, or irregular.
- Clinical findings: Nearly constant pain and substantial stiffness are present at extremes of the range of motion but not at mid-range.
Grade 4
- Dorsiflexion: Same as grade 3
- Radiographic findings: same as grade 3
- Clinical findings: Same criteria as grade 3, but there is definite pain at mid-range of passive motion.[15]
Treatment / Management
Nonoperative
Up to 55% of patients with hallux rigidus have adequate pain relief without surgical intervention.[16] NSAIDs can help reduce swelling and joint pain. Intraarticular steroid injections can provide temporary relief but have not shown long-term benefits. Dexamethasone phosphate should be preferred over triamcinolone due to chondrotoxic effects when intraarticular injections are utilized.[17] Activity modifications such as avoiding running, jumping, and stairs can make a difference in pain and discomfort. This may not be desirable for all patients.
Other conservative treatments include shoe modifications and orthotics, which aim to modify the biomechanics of the first MTP joint, reduce motion, limit irritation from the dorsal osteophytes, and reduce the mechanical stresses on the joint. Carbon fiber or spring steel are common materials used in prefabricated devices or are combined with custom orthotics to limit motion.[16] Morton's extension, made of a firm or rigid orthotic material that extends under the great toe, can help reduce dorsiflexion. Navicular pads have been used to alter the loading patterns of the joint. Rocker bottom soles can help diminish painful dorsiflexion during the gait cycle. Shoes with a high-toe box can take the pressure off prominent osteophytes. However, many of these modifications are not well tolerated by patients.[18]
Operative
Cheilectomy: This procedure has a good outcome for grade 1 and 2 hallux rigidus, with up to 97% of patients reporting excellent results and 92% having pain relief and function improvement in a 10-year follow-up period. However, less satisfactory results are seen with higher stages of hallux rigidus, where conversion to arthrodesis is 25% to 56%.[19] This procedure uses a dorsal approach. The capsule is opened, followed by a complete synovectomy. Approximately 30% of the dorsal aspect of the metatarsal head is removed. Removal of more than 40% can lead to a painful overload of the remaining articular surface or dorsal subluxation of the phalanx. If present, lateral osteophytes are removed as well. The dorsal bone is removed until 60 to 70° of dorsiflexion at the MTP joint is achieved. The average increase in dorsiflexion is approximately 25°. The main benefit is the relief of dorsal impingement, the primary source of pain.[20]
Cheilectomy may also be performed by a medial approach. Care is necessary to identify and protect the sensory nerve branches on the medial aspect of the toe. The medial approach allows for the inspection of the metatarsal sesamoid complex, which is not accessible by a dorsal approach. Occasionally, marginal osteophytes or adhesions may be present, requiring removal. Care is necessary to repair the medial capsule at closure to prevent hallux valgus. A minimally invasive approach can also be performed. Minimally Invasive Dorsal Cheilectomies (MIDC) have shown promising clinical outcomes.[21] However, Glenn and colleagues emphasized the importance of combining the procedure with arthroscopy due to bone debris, synovitis, loose bodies, and large cartilage flaps left within the joint.[22] Cheilectomies have a survival rate of 70% in an approximately 7-year period.[19](B2)
Moberg procedure: This procedure is a dorsal closing wedge osteotomy of the proximal phalanx. It can be used during cheilectomy if it fails to achieve adequate dorsiflexion.[23]
Arthrodesis: This procedure is the gold standard for treating more severe (grade 3 to 4) hallux rigidus.[24] Successful clinical outcomes are based on the correct positioning of the fusion (see Images. Hallux Rigidus Plate & Hallux Rigidus Screws). The recommended positioning of the hallux relative to the floor is between 10 and 15° of dorsiflexion and 10 to 15° of valgus.[20](A1)
Keller resection arthroplasty: This surgery involves the removal of the base of the proximal phalanx. It is indicated in low-demand patients older than 70.[25](B2)
First MTP implant arthroplasty: Silicone implants were the first hemi implants created in the 1960s. Since then, they have been through many modifications, including dracon jackets to aid fibrous tissue ingrowth and metal grommets to prevent detritic synovitis.[26] Newer studies have shown promising results of the double-stemmed hinge silicone implant following modifications, with pain relief in 95% of patients in up to 9 years of follow-up.[27][28](B2)
Total joint implants are controversial. Generally not recommended in young or active persons due to the risk of implant loosening, subsidence, plantar subluxation, and component malalignment.[20] Results have shown to be less superior to arthrodesis regarding clinical outcomes, reduction in pain, complications, and revisions.[25](B2)
Polyvinyl alcohol hydrogel hemiarthroplasty received FDA approval for implantation in July 2016 in the United States. It has similar material properties to human articular cartilage regarding water content, tensile strength, and compressive modulus. Early data showed similar outcomes to arthrodesis; newer studies concluded that the frequency of conflict of interest by authors weakens the strength of evidence of previous studies, and more studies with long-term data are necessary.[29]
Interposition arthroplasty: This technique includes a modification of the Keller arthroplasty with the addition of an autogenous, allogeneic, or synthetic matrix spacer. Emmons and colleagues systematically reviewed 20 studies that utilized this technique with different materials. Out of 539 feet in a mean follow-up of 4.5 years, 90% of patients reported statistically significant improvement, and only 3.8% proceeded to further surgery.[30](A1)
Differential Diagnosis
Differentiating hallux rigidus from other causes of first metatarsophalangeal joint pain, which includes bunions, gout, hallux valgus, infection, and turf toe, is crucial. Restriction in dorsiflexion and the presence of dorsal osteophytes can lead to the diagnosis of hallux rigidus. Turf toe would present more acutely after traumatic injury. While hallux rigidus can have a swollen and painful great toe, laboratory evaluation can differentiate it from other diseases such as septic first MTP joint or gout.
Prognosis
Nonoperative treatment should be the first attempted intervention, as it has been shown to have good outcomes. Grady and colleagues reviewed 772 patients with either operative or nonoperative management; 55% percent of all patients had treatment success with conservative care alone.[16] As per operative treatment, first metatarsophalangeal joint arthrodesis remains the gold standard for end-stage hallux rigidus, with a success rate of approximately 90%.[31]
Complications
Cheilectomy does not prevent disease progression. Conversion rates to arthrodesis have ranged from 7% to 9% within 10 years. If the procedure fails, it does not compromise further revision surgery.[20] A systematic review by Stevens et al demonstrated a nonunion or delayed union rate of about 6.6% associated with arthrodesis. The study also showed that about 20% of patients had asymptomatic nonunion that did not require treatment. Other complications may include hardware removal, joint stiffness, and metatarsalgia. Complications associated with Keller resection arthroplasty include hallux cock-up deformity, toe-off weakness, and transfer metatarsalgia. Arthroplasty-related complications include failure of arthroplasty. It has correlated with implant-related complications of 26%, with the majority due to prosthetic loosening, causing instability and pain while walking.[25]
Postoperative and Rehabilitation Care
Postoperative protocol for cheilectomies, osteotomies, and implants usually includes immediate weight bearing in a surgical shoe. At the same time, a first MTP joint fusion requires a non–weight-bearing period varying from 4 to 8 weeks. No current guidelines for physical therapy and rehabilitation protocol following surgery exist; however, a study from the Department of Kinesiology of VA recently showed that intrinsic muscles of the foot significantly decreased in cross-sectional area and muscle thickness following a first MTP fusion. The results suggest that patients may benefit from an appropriate rehabilitation protocol that includes intrinsic foot muscle training.[32]
Deterrence and Patient Education
Hallux rigidus (stiff toe) is arthritis in the big toe joint. Even though its etiology is not fully understood, this condition has been mainly associated with trauma in unilateral cases and family history, as well as female gender in bilateral involvement. Shoe wear does not cause hallux rigidus. Appropriate support through shoe modifications or orthotic devices may improve foot function and decrease the progression of the deformity. Other conservative treatment options include oral nonsteroidal anti-inflammatory drugs, steroid injections, and physical therapy. Over 50% of patients have satisfactory pain relief with nonoperative treatment, while more severe stages of the disease may require surgery.
Enhancing Healthcare Team Outcomes
Hallux rigidus is a common condition encountered by primary care providers. Referral to foot and ankle surgeons and podiatrists may be needed. Surgical treatment should only be an option after the failure of nonoperative treatment. Nonoperative treatments are successful for about half of all patients. Cheilectomy has demonstrated promising outcomes for the early stages of hallux rigidus. Arthrodesis of the first MTP joint remains the gold standard of treatment for advanced arthritis. Other treatments, such as MTP joint implants and interposition arthroplasty, may be an option if preservation of motion in that joint is desired. However, these require additional long-term studies.[5] Foot and nail care nurses are an integral part of the interprofessional team.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Massimi S, Caravelli S, Fuiano M, Pungetti C, Mosca M, Zaffagnini S. Management of high-grade hallux rigidus: a narrative review of the literature. Musculoskeletal surgery. 2020 Dec:104(3):237-243. doi: 10.1007/s12306-020-00646-y. Epub 2020 Feb 6 [PubMed PMID: 32030657]
Level 3 (low-level) evidenceRoukis TS. Metatarsus primus elevatus in hallux rigidus: fact or fiction? Journal of the American Podiatric Medical Association. 2005 May-Jun:95(3):221-8 [PubMed PMID: 15901807]
Cotterill JM. THE PATHOLOGY OF HALLUX RIGIDUS. British medical journal. 1903 Nov 28:2(2239):1400 [PubMed PMID: 20761209]
Galois L, Hemmer J, Ray V, Sirveaux F. Surgical options for hallux rigidus: state of the art and review of the literature. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2020 Jan:30(1):57-65. doi: 10.1007/s00590-019-02528-x. Epub 2019 Aug 7 [PubMed PMID: 31392522]
Lam A, Chan JJ, Surace MF, Vulcano E. Hallux rigidus: How do I approach it? World journal of orthopedics. 2017 May 18:8(5):364-371. doi: 10.5312/wjo.v8.i5.364. Epub 2017 May 18 [PubMed PMID: 28567339]
Beeson P, Phillips C, Corr S, Ribbans WJ. Cross-sectional study to evaluate radiological parameters in hallux rigidus. Foot (Edinburgh, Scotland). 2009 Mar:19(1):7-21. doi: 10.1016/j.foot.2008.07.002. Epub 2008 Oct 10 [PubMed PMID: 20307444]
Level 2 (mid-level) evidenceCalvo A, Viladot R, Giné J, Alvarez F. The importance of the length of the first metatarsal and the proximal phalanx of hallux in the etiopathogeny of the hallux rigidus. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2009:15(2):69-74. doi: 10.1016/j.fas.2008.08.001. Epub 2008 Oct 1 [PubMed PMID: 19410172]
Level 2 (mid-level) evidenceLee HY, Lalevee M, Mansur NSB, Vandelune CA, Dibbern KN, Barg A, Femino JE, de Cesar Netto C. Multiplanar instability of the first tarsometatarsal joint in hallux valgus and hallux rigidus patients: a case-control study. International orthopaedics. 2022 Feb:46(2):255-263. doi: 10.1007/s00264-021-05198-9. Epub 2021 Sep 1 [PubMed PMID: 34468786]
Level 2 (mid-level) evidenceBejarano-Pineda L, Cody EA, Nunley JA 2nd. Prevalence of Hallux Rigidus in Patients With End-Stage Ankle Arthritis. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2021 Jan-Feb:60(1):21-24. doi: 10.1053/j.jfas.2020.04.004. Epub 2020 Nov 5 [PubMed PMID: 33160837]
Air ME, Rietveld AB. Freiberg's disease as a rare cause of limited and painful relevé in dancers. Journal of dance medicine & science : official publication of the International Association for Dance Medicine & Science. 2010:14(1):32-6 [PubMed PMID: 20214853]
Level 3 (low-level) evidenceSenga Y, Nishimura A, Ito N, Kitaura Y, Sudo A. Prevalence of and risk factors for hallux rigidus: a cross-sectional study in Japan. BMC musculoskeletal disorders. 2021 Sep 13:22(1):786. doi: 10.1186/s12891-021-04666-y. Epub 2021 Sep 13 [PubMed PMID: 34517874]
Level 2 (mid-level) evidenceBotek G, Anderson MA. Etiology, pathophysiology, and staging of hallux rigidus. Clinics in podiatric medicine and surgery. 2011 Apr:28(2):229-43, vii. doi: 10.1016/j.cpm.2011.02.004. Epub [PubMed PMID: 21669337]
Walter R, Perera A. Open, Arthroscopic, and Percutaneous Cheilectomy for Hallux Rigidus. Foot and ankle clinics. 2015 Sep:20(3):421-31. doi: 10.1016/j.fcl.2015.04.005. Epub [PubMed PMID: 26320557]
Hagedorn TJ, Dufour AB, Riskowski JL, Hillstrom HJ, Menz HB, Casey VA, Hannan MT. Foot disorders, foot posture, and foot function: the Framingham foot study. PloS one. 2013:8(9):e74364. doi: 10.1371/journal.pone.0074364. Epub 2013 Sep 5 [PubMed PMID: 24040231]
Level 3 (low-level) evidenceCoughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. The Journal of bone and joint surgery. American volume. 2003 Nov:85(11):2072-88 [PubMed PMID: 14630834]
Colò G, Fusini F, Samaila EM, Rava A, Felli L, Alessio-Mazzola M, Magnan B. The efficacy of shoe modifications and foot orthoses in treating patients with hallux rigidus: a comprehensive review of literature. Acta bio-medica : Atenei Parmensis. 2020 Dec 30:91(14-S):e2020016. doi: 10.23750/abm.v91i14-S.10969. Epub 2020 Dec 30 [PubMed PMID: 33559617]
Braun HJ, Wilcox-Fogel N, Kim HJ, Pouliot MA, Harris AH, Dragoo JL. The effect of local anesthetic and corticosteroid combinations on chondrocyte viability. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2012 Sep:20(9):1689-95. doi: 10.1007/s00167-011-1728-1. Epub 2011 Oct 29 [PubMed PMID: 22037813]
Kunnasegaran R, Thevendran G. Hallux Rigidus: Nonoperative Treatment and Orthotics. Foot and ankle clinics. 2015 Sep:20(3):401-12. doi: 10.1016/j.fcl.2015.04.003. Epub 2015 Jun 9 [PubMed PMID: 26320555]
Sidon E, Rogero R, Bell T, McDonald E, Shakked RJ, Fuchs D, Daniel JN, Pedowitz DI, Raikin SM. Long-term Follow-up of Cheilectomy for Treatment of Hallux Rigidus. Foot & ankle international. 2019 Oct:40(10):1114-1121. doi: 10.1177/1071100719859236. Epub 2019 Jul 16 [PubMed PMID: 31307212]
Deland JT, Williams BR. Surgical management of hallux rigidus. The Journal of the American Academy of Orthopaedic Surgeons. 2012 Jun:20(6):347-58. doi: 10.5435/JAAOS-20-06-347. Epub [PubMed PMID: 22661564]
Teoh KH, Tan WT, Atiyah Z, Ahmad A, Tanaka H, Hariharan K. Clinical Outcomes Following Minimally Invasive Dorsal Cheilectomy for Hallux Rigidus. Foot & ankle international. 2019 Feb:40(2):195-201. doi: 10.1177/1071100718803131. Epub 2018 Oct 4 [PubMed PMID: 30282465]
Level 2 (mid-level) evidenceGlenn RL, Gonzalez TA, Peterson AB, Kaplan J. Minimally Invasive Dorsal Cheilectomy and Hallux Metatarsal Phalangeal Joint Arthroscopy for the Treatment of Hallux Rigidus. Foot & ankle orthopaedics. 2021 Jan:6(1):2473011421993103. doi: 10.1177/2473011421993103. Epub 2021 Mar 4 [PubMed PMID: 35097431]
Yee G, Lau J. Current concepts review: hallux rigidus. Foot & ankle international. 2008 Jun:29(6):637-46. doi: 10.3113/FAI.2008.0637. Epub [PubMed PMID: 18549766]
de Bot RTAL, Veldman HD, Eurlings R, Stevens J, Hermus JPS, Witlox AM. Metallic hemiarthroplasty or arthrodesis of the first metatarsophalangeal joint as treatment for hallux rigidus: A systematic review and meta-analysis. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2022 Feb:28(2):139-152. doi: 10.1016/j.fas.2021.03.004. Epub 2021 Mar 11 [PubMed PMID: 33812802]
Level 1 (high-level) evidenceStevens J, de Bot RTAL, Hermus JPS, van Rhijn LW, Witlox AM. Clinical Outcome Following Total Joint Replacement and Arthrodesis for Hallux Rigidus: A Systematic Review. JBJS reviews. 2017 Nov:5(11):e2. doi: 10.2106/JBJS.RVW.17.00032. Epub [PubMed PMID: 29135720]
Level 2 (mid-level) evidenceButterworth ML, Ugrinich M. First Metatarsophalangeal Joint Implant Options. Clinics in podiatric medicine and surgery. 2019 Oct:36(4):577-596. doi: 10.1016/j.cpm.2019.07.003. Epub [PubMed PMID: 31466569]
Ter Keurs EW, Wassink S, Burger BJ, Hubach PC. First metatarsophalangeal joint replacement: long-term results of a double stemmed flexible silicone prosthesis. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2011 Dec:17(4):224-7. doi: 10.1016/j.fas.2010.08.001. Epub 2010 Sep 9 [PubMed PMID: 22017891]
Level 2 (mid-level) evidenceKanzaki N, Nishiyama T, Fujishiro T, Hayash S, Hashimoto S, Kuroda R, Kurosaka M. Flexible hinge silicone implant with or without titanium grommets for arthroplasty of the first metatarsophalangeal joint. Journal of orthopaedic surgery (Hong Kong). 2014 Apr:22(1):42-5 [PubMed PMID: 24781612]
Level 2 (mid-level) evidenceBernasconi A, De Franco C, Iorio P, Smeraglia F, Rizzo M, Balato G. Use of synthetic cartilage implant (Cartiva®) for degeneration of the first and second metatarsophalangeal joint: what is the current evidence? Journal of biological regulators and homeostatic agents. 2020 May-Jun:34(3 Suppl. 2):15-21. ADVANCES IN MUSCULOSKELETAL DISEASES AND INFECTIONS - SOTIMI 2019 [PubMed PMID: 32856435]
Emmons BR, Carreira DS. Outcomes Following Interposition Arthroplasty of the First Metatarsophalangeal Joint for the Treatment of Hallux Rigidus: A Systematic Review. Foot & ankle orthopaedics. 2019 Apr:4(2):2473011418814427. doi: 10.1177/2473011418814427. Epub 2019 Apr 2 [PubMed PMID: 35097316]
Level 1 (high-level) evidenceRammelt S, Panzner I, Mittlmeier T. Metatarsophalangeal Joint Fusion: Why and How? Foot and ankle clinics. 2015 Sep:20(3):465-77. doi: 10.1016/j.fcl.2015.04.008. Epub 2015 Jun 10 [PubMed PMID: 26320560]
Jaffri AH, Hertel J, Saliba S. Ultrasound examination of intrinsic foot muscles in patients with 1st metatarsophalangeal joint arthrodesis. Foot (Edinburgh, Scotland). 2019 Dec:41():79-84. doi: 10.1016/j.foot.2019.08.009. Epub 2019 Sep 3 [PubMed PMID: 31739244]