Introduction
An ablative nerve block is a minimally invasive procedure that involves coagulation necrosis of afferent nociceptive signals via high-frequency waves (300 to 500 Hz). In 1975, ablation was initially used to treat chronic back pain and sciatica of unknown etiology as an alternative to the prior treatment of severing the dorsal rami via the intertransverse ligaments. Currently, ablation is most commonly used to destroy the medial branches of the dorsal rami, which are responsible for facet-joint-mediated back pain. Ablative nerve blocks are commonly used to treat chronic low back pain. The patient benefits the most in the short term, within the first 4 weeks following the procedure.[1] However, significant pain relief has been shown to last up to a year.[2]
Many studies do not show superiority over placebo for either pain relief or functional improvement.[3][4] However, recent guidelines provide a moderate degree of evidence to support ablative nerve block use.[5] There is also evidence for ablative nerve block use for chronic discogenic back pain.[6] Recent literature supports the ablation of peripheral nerves that have a primary role in nociception for pain treatment, particularly when symptomatology has been refractory to conservative management but is relieved with targeted blocks using short-acting anesthetic agents.[7]
Other indications for ablative nerve block are the treatment of knee joint osteoarthritis, trigeminal neuralgia, and abdominal and thoracic chronic pain syndromes. Since ablative nerve blocks are frequently used for the treatment of back pain, the discussion will concentrate on this indication and briefly mention other associated conditions.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
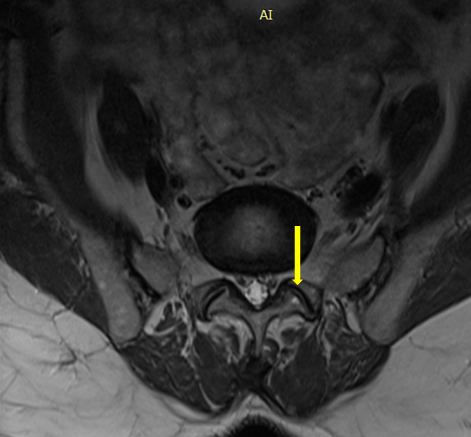
Facet-mediated pain is caused by facet arthropathy or arthritis, which arises during the degenerative process of the spinal column. A single facet joint comprises the inferior articulating process of 1 vertebra and the superior articulating process of the vertebra directly inferior. These joints, also known as zygapophyseal joints, are synovial and are potential generators of pain (see Image. Facet Joint).
Medial branches from the primary dorsal rami of spinal nerve roots at the same level and 1 level above provide sensory innervation to the facet (for example, the L4-L5 facet joint is innervated by the medial branches of L3 and L4, located on L4 and L5 respectively). The medial branches typically course over the bases of the transverse processes at their junctions with the superior articulating processes. The L5 dorsal ramus is usually found inside a groove at the base of the S1 superior articular process. The L5 medial branch originates from this location towards the lower end of the process.
The 2 most typically afflicted lumbar facet joints are L4-L5 and L5-S1, so the nerves that innervate these joints, the L3 and L4 medial branches and the L5 dorsal ramus, are the most frequently chosen for ablation. The L5 dorsal ramus is ablated as it is more accessible than the medial branch.[8]
An insulated electrode with an uninsulated tip is advanced toward the concavity formed between the superior articulating process and the adjacent transverse process, which is in proximity to the nerve suspected of causing the symptoms. This location is where high-frequency or radiofrequency energy is generated to produce a lesion via coagulative necrosis, thereby disrupting afferent pain signals. In pain medicine, radiofrequency ablation most commonly involves targeting the specific medial branches of the dorsal rami that innervate pain-producing facet joints under fluoroscopic guidance. However, further investigations regarding the efficacy of ablation in other common pain syndromes continue to diversify its use.[9][7]
Radioablation blocks nociceptive signals traveling through A-delta and C-fibers from the peripheral to the central nervous system while preserving motor and sensory (A-beta) fibers. The hypothesized mechanism of action is the modulation of pain signals, suppressing the release of immune-mediator cells and pro-inflammatory cytokines (interleukin-1β and interleukin-6) rather than the thermal destruction of the nerve.[10][11]
Indications
Nerve ablation is indicated to treat facet-mediated axial back pain of the cervical and lumbar spine that has failed conservative therapy. Ablation has other uses, such as relief of chronic neck pain after whiplash and chronic headache syndromes due to occipital and trigeminal neuralgia. Ablation is performed after successful analgesia of the suspected trouble-causing nerve with a local anesthetic.
Studies continue to investigate the role of ablation in peripheral nerve-mediated pain outside of the spinal column, particularly in knee osteoarthritis and plantar fasciitis.[12][13] Ablative nerve blocks, with cooled radiofrequency ablation of the genicular nerve, are an effective pain reliever for refractory osteoarthritis of the knee. Furthermore, studies show improved knee function up to 6 months following the ablation procedure.[14]
There are no pathognomonic findings on history or physical examination.[15] However, pain from lumbar facet joints tends to be nonradicular, centered in the paraspinal regions and may be referred to the posterior thighs in a nondermatomal pattern. Referred pain below the knee joints is very rare.[8] Medial branch blocks, performed with local anesthesia, help determine the likelihood of success of radiofrequency ablation of dorsal primary rami. Patients who respond to the medial branch block are found to have reduced low back pain and increased function.[16][17]
Contraindications
Absolute contraindications for ablative nerve blocks include active local infection at the needle insertion site, systemic infection, allergy to local anesthetic, and elevated intracranial pressure. Patients taking anticoagulants provide a unique challenge for practitioners. Clinical judgment must be followed along with adherence to accepted guidelines. Current guidelines put forth by the American Society of Regional Anesthesia and Pain Medicine (ASRA) recommend that:
- Aspirin to be stopped 6 days preprocedure
- Clopidogrel to be stopped 7 days preprocedure
- Apixaban to be stopped 3 to 5 days preprocedure
- Rivaroxaban to be stopped 3 days preprocedure
- Warfarin to be stopped 5 days preprocedure
- Intravenous heparin to be stopped 4 hours preprocedure
Other relative contraindications that must considered before the procedure include the following:
- Neurologic abnormalities
- Concerning clinical or imaging findings
- Definitive causes of low back pain (eg, disc herniation, spondylolisthesis, spondylosis, spinal stenosis, malignancy, infection, or trauma)
- Lack of pain relief from prior diagnostic nerve blocks [18]
Technical limitations are as follows:
- Scoliosis
- Severe degenerative changes
- Facet arthropathy
- Bone spurs
Bipolar radiofrequency ablation is of use in patients with implantable devices like cardiac implantable electronic devices or deep brain stimulators. The latter is to be switched off during surgery, and the cautery pads must be kept as far away from these implants as possible.[10]
Equipment
The procedure is routinely performed in a sterile procedure suite, with the patient lying prone on a procedure table.
Key supplies for the procedure include the following (see Image. Standard Nerve Block Tray [PENG Block]):
- C-arm mobile fluoroscopic unit
- Local anesthetic drug
- Continuous high-frequency radiofrequency generator with a built-in thermocouple, impedance, voltage, and amperage monitor
- Introducer Quincke needles (50 to 150 mm in length, 22- or 25-gauge in diameter for branch block)
- Radiofrequency cannulas with corresponding electrodes (18-gauge or larger is advisable to increase the capture rate)
- Active and ground electrodes - The active electrode delivers the high-frequency current, which is dissipated through a ground electrode attached to the patient.
All equipment should be checked for proper working order prior to the procedure.
Personnel
As with other interventional spinal procedures, only physicians trained explicitly in fluoroscopically-guided procedures should perform radiofrequency ablation. Qualified physicians typically undergo residency training in anesthesiology, physiatry, neurology, psychiatry, or neurosurgery. This training is followed by an interventional pain or spine fellowship that allows adequate training under an experienced interventionalist before performing the procedure independently. Support staff for the procedure can include an assistant to draw up necessary medications and operate the radiofrequency generator and a radiology technician to operate the C-arm under the guidance of the performing physician.
A nurse should monitor the patient's vital signs continuously during the procedure and record blood pressure at least every 5 minutes throughout the procedure. Nurses should be prepared to administer IV fluids and conscious sedation if indicated as ordered by the physician. During the ablation, nurses are responsible for checking the grounding pads periodically for full adhesion to the skin and for increasing temperature of the skin and pads to avoid burns.
Preparation
The destruction of tissue via radiofrequency must occur after successful diagnostic anesthetic nerve blocks have located the target nerve. During the procedure, the patient should receive little to no sedation, as they must define what they are experiencing during stimulation and lesioning of the nerve.
Technique or Treatment
The steps of the procedure can be outlined as follows: [8]
The patient is placed in a comfortable position with adequate exposure to the region overlying the target nerve. The skin is cleaned and prepped, and the target is found using fluoroscopy. A small amount of local anesthetic is injected subcutaneously at the point of needle insertion.
Lumbar Medial Branch Block
- The nerves are targeted by advancing the spinal needle under fluoroscopic guidance to the following points as given below:
- L5 dorsal ramus: The junction of the sacral ala and the sacral articular process
- L4 medial branch: The junction of the L5 superior articular and transverse processes
- L3 medial branch: The junction of the L4 superior articular and transverse processes
- Needles are checked for placement into the above junctions and absence of entry into a blood vessel.
- Local anesthetic is injected.
Lumbar Radiofrequency Ablation
- The introducer cannula is then inserted through the skin, subcutaneous tissue, and muscle toward the same targets mentioned above, using fluoroscopy to guide the trajectory.
- This insertion requires a medial and cephalad trajectory to place the cannula almost parallel to the nerve to maximize the coagulation.
- Once the needle tip is placed satisfactorily close to the target, the active electrode is inserted through the needle.
- The target location is found using sensory stimulation, recreating the painful symptoms that the patient experiences.
- This step is followed by motor stimulation to ensure the active tip is not close to the motor nerves.
- Once confirmed, a local anesthetic agent is administered into each cannula. Subsequently, the generator produces a continuous output voltage at the tip of the electrode. The generator should be kept at 70 to 80 °C for approximately 1 minute, creating a zone of thermally induced coagulation.[19]
Complications
Nerve ablation is a minimally invasive, relatively low-risk procedure with a limited adverse event profile.[20] The following is a list of the most commonly associated adverse events.
Complications Associated with the Advancement of the Introducer Needle
- Localized swelling and pain (transient postoperative pain is the premier adverse event)
- Hematoma
- Pneumothorax
- Dural puncture
- Spinal cord trauma
- Subdural injection
- Neural trauma
- Infection (eg, meningitis, abscess)
- Temporary weakness or numbness
- Allergy to materials or anesthetics
Complications Associated with Radiofrequency Ablation [18][21]
- Weakness of lumbar paraspinal muscles
- Dysesthesias
- Transient mild neuritis (may feel like a sunburn)
- Burns (due to errors in ground pad placement)
- Worsened pain
- Sensory loss
- New-onset neuropathic pain
- Atrophy of the multifidus muscle due to denervation
- Flushing
- Hypotension
- Nonpostural headaches
- Allodynia in the paravertebral skin or denervated facets
- Camptocormia [22]
Complications Associated with Intracranial Ablation of the Trigeminal Ganglion
- Facial numbness
- Dysesthesia
- Anesthesia dolorosa
- Corneal anesthesia
- Keratitis
- Trigeminal motor dysfunction
Clinical Significance
One hundred million Americans suffer from some form of chronic pain that results in more than $100 billion in expenses annually. Furthermore, 84% of American adults will suffer from chronic low-back pain at some point in their lifetime. While the causes of low-back pain are often multifactorial and can be due to many causes, the degenerative cascade that affects the spine plays a significant role. Destruction of cartilage that comprises the spinal facet joints results in severe discomfort when placed under stress, typically in extension or rotation of the spine. The sensory nerves responsible are the medial branches of the dorsal rami, the most common target in ablative procedures. Radiofrequency ablation is efficacious in reducing the severity of back pain for extended periods (ranging from 6 to 24 months). Ablative nerve blocks have utility in treating trigeminal and occipital neuralgia, complex regional pain syndrome, hip and knee osteoarthritis, and plantar fasciitis. As with other interventional procedures that provide pain relief, ablation aims to play a significant role in reducing opiates and other habit-forming pain medications.
This review focuses on conventional radiofrequency ablation, which utilizes a continuous energy source causing coagulative thermal necrosis. Other forms of ablation used in pain management include the following:
- Pulsed radiofrequency applies heat in a pulsatile manner (pulse durations of 5 to 50 ms and pulse frequency of 1 to 10 Hz, but the most widely used sequence is a frequency of 2 Hz and a duration of 20 ms) but uses lower temperatures than conventional radiofrequency to avoid neurolysis.
- Cooled radiofrequency utilizes specialized electrodes cooled with water flowing along its shaft but not at the active tip. This technology allows high temperatures (60 °C) and more spherical lesion sizes to be achieved at the target site with less risk of tissue damage superficial to the target. Cooled radiofrequency may be more useful in patients with technical limitations (mentioned under the contraindications above). Cooled radiofrequency is found to be superior in effectiveness compared to facet joint steroid injections.[23]
- Cryoablation destroys axons by disrupting the vasa nervorum. It has increased in popularity due to decreased postprocedural hyperalgesia and neuroma formation compared to conventional radiofrequency.
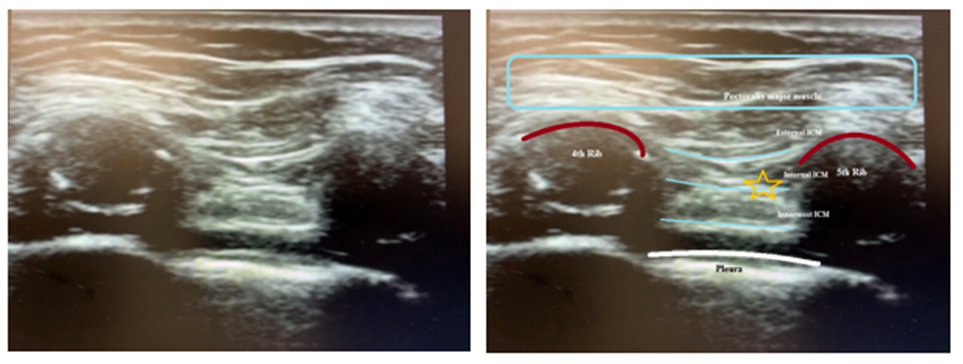
Cases of ablative nerve block use have been successfully used for intercostal neuralgia (see Image. Intercostal Nerve Block Landmark).[24] Ablative nerve blocks of the genicular nerve for chronic new pain have also been shown to be an effective pain reliever for chronic, refractory knee pain.[25] Patients who undergo ablation of the genicular nerve have been shown to have pain for up to 6 months following the procedure.[26] Furthermore, studies have also been done regarding the effectiveness of ablative techniques on cancer pain. Results have shown blocks to be effective for upper abdominal cancers such as gastric or pancreatic cancer.[27] Chronic pericranial headaches have also been studied, and evidence of radiofrequency ablation of the pericranial nerves has been found.[28] One promising 2016 study also looked at radiofrequency ablation in the treatment of vertebral compression fractures. However, more studies need to be done.[29] There is limited effectiveness in using ablative nerve blocks for facet joint osteoarthritis compared to a placebo.[30]
The other conditions in which ablative nerve block is useful in pain management and the corresponding nerves targeted are listed below (see Table. Ablative Nerve Block Indications: Other Conditions).
Table. Ablative Nerve Block Indications: Other Conditions
| Condition | Nerve(s) Blocked | Reference |
| Trigeminal neuralgial |
Peripheral branches of trigeminal nerve Gasserian ganglion |
Huang P et al [31] Wang Z et al [32] |
| Knee joint osteoarthritis |
Superior lateral genicular nerve (SLGN) Superior medial genicular nerve (SMGN) Inferior medial genicular nerve (IMGN) |
Karm MH et al [33] |
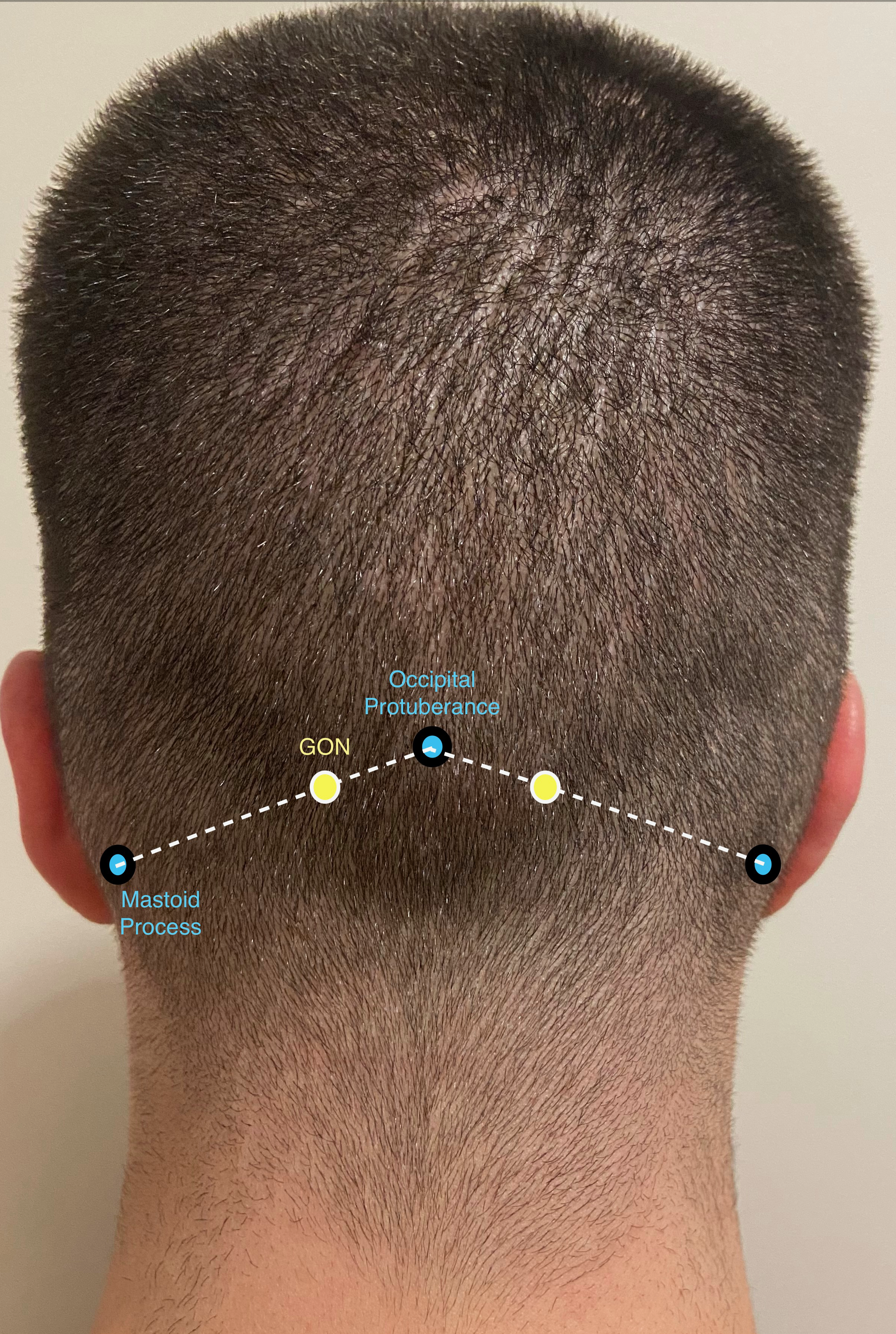
| Craniofacial pain syndromes | Greater occipital nerve | Fabry et al [34] |
| Cervicogenic headache | Cervical medial branch with third occipital nerve | Odonkor CA et al [35] |
| Intercostal neuralgia | Intercostal nerves | Fiala KJ et al [36] |
| Chronic thoracic pain | Thoracic dorsal root ganglia | Reyad RM et al [37] |
| Abdominal cancer pain | Splanchnic nerve | Amr SA et al [27] |
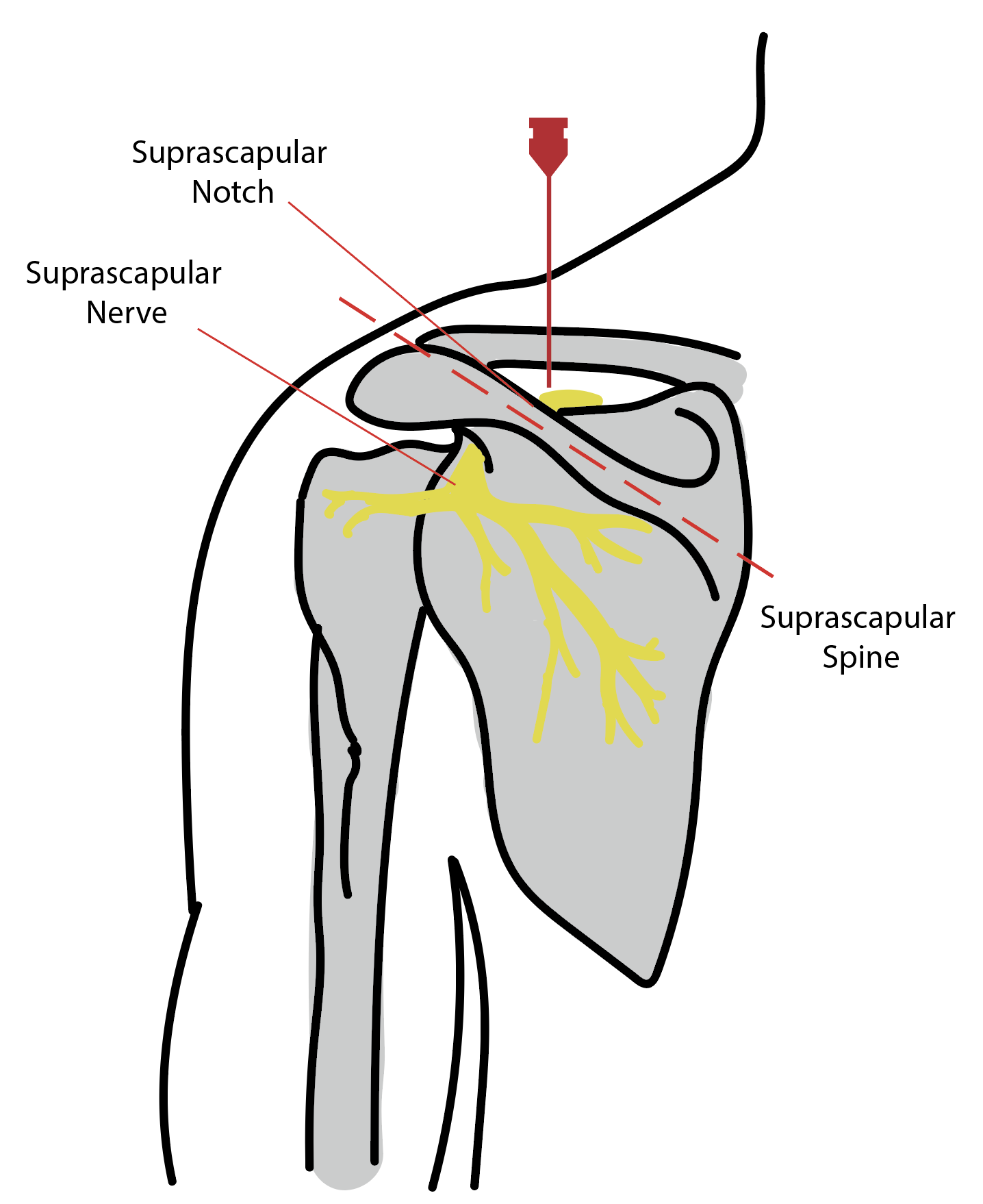
| Chronic shoulder pain | Suprascapular nerve (see Image. Suprascapular Nerve Block) | Alanbay E et al [38] |
| Chronic testicular pain | Spermatic cord | Misra S et al [39] |
| Sacroiliac joint pain | Medial branch of L4, posterior primary rami of L5, and lateral branches S1 and S2 | Vallejo R et al [40] |
| Chronic inguinal herniorrhaphy pain | T12, L1 and L2 nerve root | Rozen D et al [41] |
| Discogenic pain | Intradiscal | Teixeira A et al [42] |
| Plantar fasciitis | Baxter's nerve (inferior calcaneal nerve) | Caicedo Gutiérrez L et al [43] |
| Hip joint osteoarthritis | The obturator and femoral nerve articular sensory branches | Kallas ON et al [44] |
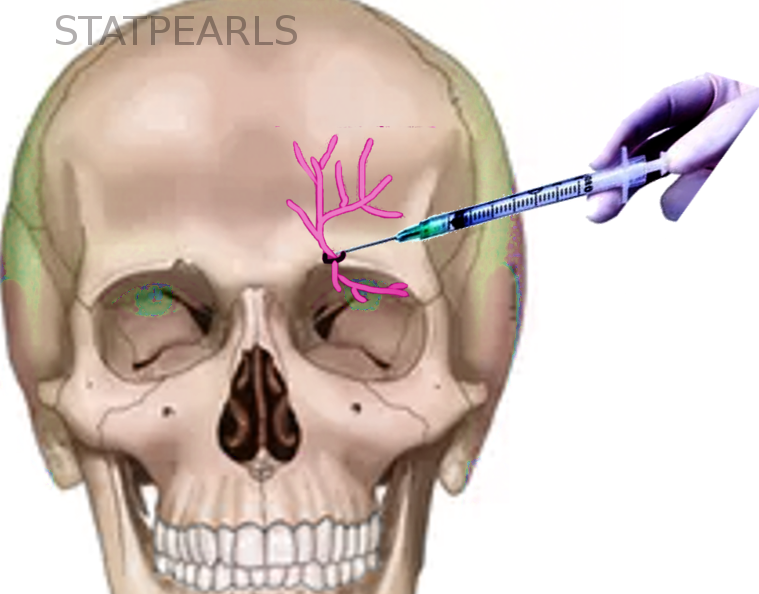
| Pericranial neuralgias associated with chronic daily headache |
Supraorbital nerve (see Image. Supraorbital Nerve Block) Supratrochlear nerve Infratrochlear nerve Infraorbital nerve Greater occipital nerve (most commonly targeted) (see Image. Greater Occipital Nerve Block Anatomy) Lesser occipital nerve External branches of anterior ethmoidal nerve |
Abd-Elsayed A et al [28] |
Enhancing Healthcare Team Outcomes
Patients undergoing ablative nerve blocks for pain management, such as those for back pain, require a coordinated interprofessional approach to ensure safety, minimize risks, and optimize outcomes. Ablative nerve block, commonly performed on an outpatient basis, relies on the collaborative efforts of a dedicated healthcare team to deliver patient-centered care effectively and enhance overall outcomes.
Anesthesiologists, pain management specialists, and surgeons are responsible for performing the actual nerve ablation. To ensure the procedure's success, they must possess the knowledge and skills of ablative techniques, select appropriate candidates, and manage potential complications. Advanced practitioners play a critical role in the preprocedure evaluation, obtaining informed consent, and managing postprocedure care. Patient monitoring is often entrusted to a dedicated nurse or anesthesia provider during the procedure. They are responsible for monitoring the patient's vital signs at regular intervals, managing hypotension, escalating sedation needs, and communicating concerns about the patient's status during the procedure. After the procedure, postanesthesia recovery nurses monitor the patient in the recovery room for several hours. These nurses play a vital role in assessing the patient's recovery from sedation, managing pain, monitoring for complications, and ensuring the patient's readiness for discharge. Before discharge, patients must be thoroughly informed about the possible adverse effects of the procedure, care instructions for the treated area, and clear guidelines on when to seek medical attention postdischarge.[45]
Effective interprofessional communication is key to the success of this collaborative approach. Care coordination is crucial in navigating the patient's journey from assessment through treatment to follow-up, ensuring a seamless transition between different phases of care and enhancing patient safety. By adhering to these principles of skill, strategy, ethics, responsibilities, interprofessional communication, and care coordination, healthcare teams can deliver comprehensive, patient-centered care. This approach improves outcomes for patients undergoing ablative nerve blocks and enhances team performance in managing patients with complex and/or chronic pain.
Media
(Click Image to Enlarge)
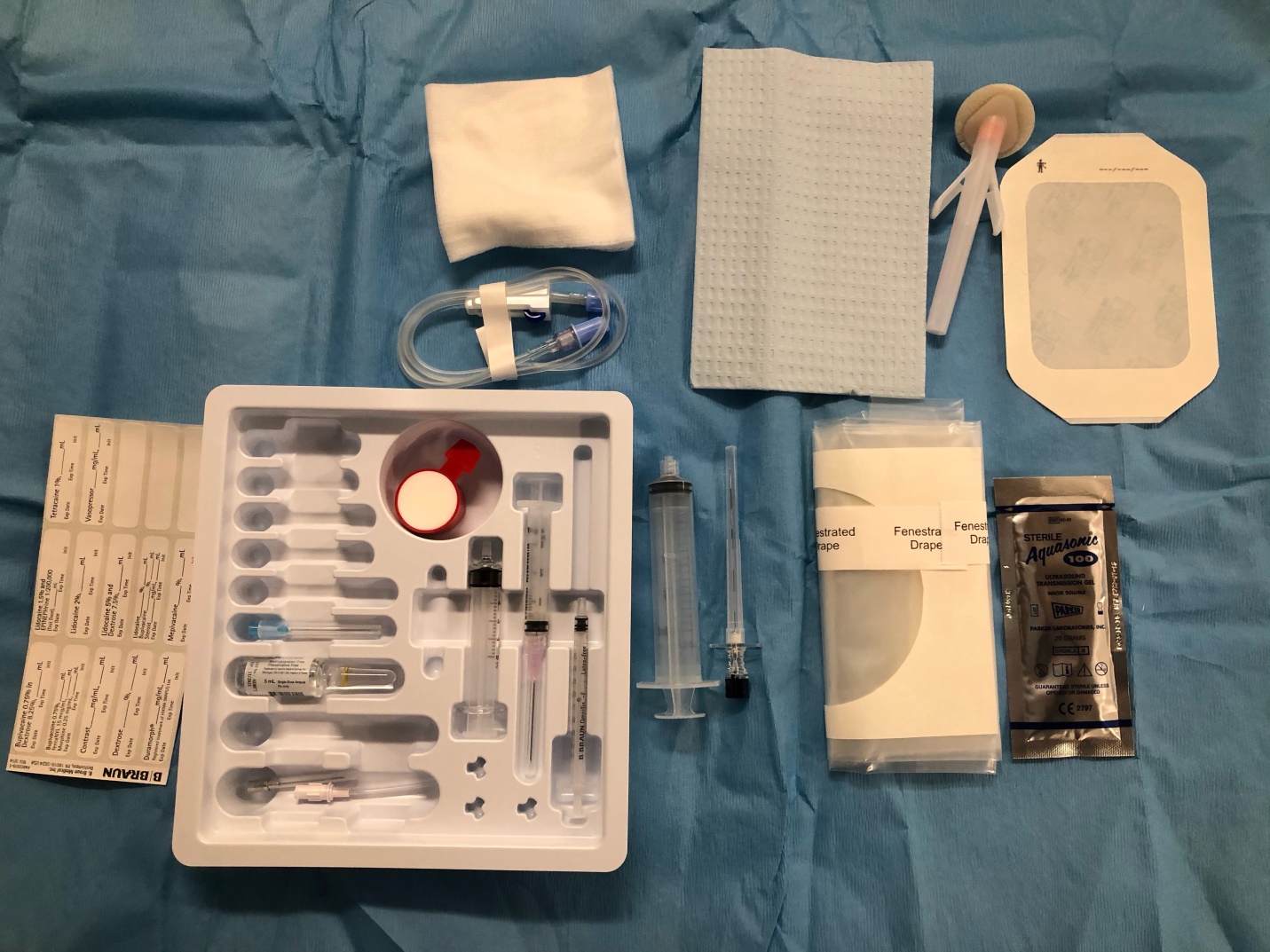
Standard Nerve Block Tray. A standard nerve block tray for performing pericapsular nerve group block includes the following equipment—an ultrasound machine with a low-frequency curvilinear probe, sterile sleeve, and gel; a 23- to 25-gauge needle for skin infiltration; 20 mL of local anesthetic; an 80-mm B-bevel nerve block needle; a pack of 4- × 4-inch gauze; chlorhexidine gluconate solution for skin asepsis; sterile gloves and a marking pen.
Contributed by B Berlioz MD
(Click Image to Enlarge)
References
Leclaire R, Fortin L, Lambert R, Bergeron YM, Rossignol M. Radiofrequency facet joint denervation in the treatment of low back pain: a placebo-controlled clinical trial to assess efficacy. Spine. 2001 Jul 1:26(13):1411-6; discussion 1417 [PubMed PMID: 11458140]
Level 1 (high-level) evidenceCohen SP, Hurley RW, Buckenmaier CC 3rd, Kurihara C, Morlando B, Dragovich A. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008 Aug:109(2):279-88. doi: 10.1097/ALN.0b013e31817f4c7c. Epub [PubMed PMID: 18648237]
Level 1 (high-level) evidencevan Wijk RM, Geurts JW, Wynne HJ, Hammink E, Buskens E, Lousberg R, Knape JT, Groen GJ. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: a randomized, double-blind, sham lesion-controlled trial. The Clinical journal of pain. 2005 Jul-Aug:21(4):335-44 [PubMed PMID: 15951652]
Level 1 (high-level) evidenceMaas ET, Ostelo RW, Niemisto L, Jousimaa J, Hurri H, Malmivaara A, van Tulder MW. Radiofrequency denervation for chronic low back pain. The Cochrane database of systematic reviews. 2015 Oct 23:2015(10):CD008572. doi: 10.1002/14651858.CD008572.pub2. Epub 2015 Oct 23 [PubMed PMID: 26495910]
Level 3 (low-level) evidenceManchikanti L, Kaye AD, Soin A, Albers SL, Beall D, Latchaw R, Sanapati MR, Shah S, Atluri S, Abd-Elsayed A, Abdi S, Aydin S, Bakshi S, Boswell MV, Buenaventura R, Cabaret J, Calodney AK, Candido KD, Christo PJ, Cintron L, Diwan S, Gharibo C, Grider J, Gupta M, Haney B, Harned ME, Helm Ii S, Jameson J, Jha S, Kaye AM, Knezevic NN, Kosanovic R, Manchikanti MV, Navani A, Racz G, Pampati V, Pasupuleti R, Philip C, Rajput K, Sehgal N, Sudarshan G, Vanaparthy R, Wargo BW, Hirsch JA. Comprehensive Evidence-Based Guidelines for Facet Joint Interventions in the Management of Chronic Spinal Pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines Facet Joint Interventions 2020 Guidelines. Pain physician. 2020 May:23(3S):S1-S127 [PubMed PMID: 32503359]
Level 1 (high-level) evidenceOh WS, Shim JC. A randomized controlled trial of radiofrequency denervation of the ramus communicans nerve for chronic discogenic low back pain. The Clinical journal of pain. 2004 Jan-Feb:20(1):55-60 [PubMed PMID: 14668658]
Level 1 (high-level) evidenceChoi EJ, Choi YM, Jang EJ, Kim JY, Kim TK, Kim KH. Neural Ablation and Regeneration in Pain Practice. The Korean journal of pain. 2016 Jan:29(1):3-11. doi: 10.3344/kjp.2016.29.1.3. Epub 2016 Jan 4 [PubMed PMID: 26839664]
Hao D, Yong RJ, Cohen SP, Stojanovic MP. Medial Branch Blocks and Radiofrequency Ablation for Low Back Pain from Facet Joints. The New England journal of medicine. 2023 Dec 21:389(25):e53. doi: 10.1056/NEJMvcm2211108. Epub [PubMed PMID: 38118025]
Senthelal S, Dydyk AM, Mesfin FB. Ablative Nerve Block. StatPearls. 2024 Jan:(): [PubMed PMID: 29763150]
Sowder T, Sayed D, Concannon T, Pew SH, Strand NH, Abd-Elsayed A, Wie CS, Gomez Ramos DE, Raslan AM, Deer TR. The American Society of Pain and Neuroscience (ASPN) Guidelines for Radiofrequency Ablative Procedures in Patients with Implanted Devices. Journal of pain research. 2023:16():3693-3706. doi: 10.2147/JPR.S419594. Epub 2023 Nov 3 [PubMed PMID: 37942223]
Chen B, Yang Y, Wang H, Guo X, Wu Z, Lan Z. Is radiofrequency ablation effective in treating patients with chronic knee osteoarthritis? A meta-analysis of randomized controlled trials. Annals of medicine and surgery (2012). 2024 Jan:86(1):412-420. doi: 10.1097/MS9.0000000000001509. Epub 2023 Nov 17 [PubMed PMID: 38222705]
Level 1 (high-level) evidenceZakrzewska JM, Akram H. Neurosurgical interventions for the treatment of classical trigeminal neuralgia. The Cochrane database of systematic reviews. 2011 Sep 7:2011(9):CD007312. doi: 10.1002/14651858.CD007312.pub2. Epub 2011 Sep 7 [PubMed PMID: 21901707]
Level 1 (high-level) evidenceSaedi N, Hamilton HK, Arndt KA, Dover JS. How to prepare patients for ablative laser procedures. Journal of the American Academy of Dermatology. 2013 Aug:69(2):e49. doi: 10.1016/j.jaad.2013.04.019. Epub [PubMed PMID: 23866890]
McCormick ZL, Reddy R, Korn M, Dayanim D, Syed RH, Bhave M, Zhukalin M, Choxi S, Ebrahimi A, Kendall MC, McCarthy RJ, Khan D, Nagpal G, Bouffard K, Walega DR. A Prospective Randomized Trial of Prognostic Genicular Nerve Blocks to Determine the Predictive Value for the Outcome of Cooled Radiofrequency Ablation for Chronic Knee Pain Due to Osteoarthritis. Pain medicine (Malden, Mass.). 2018 Aug 1:19(8):1628-1638. doi: 10.1093/pm/pnx286. Epub [PubMed PMID: 29300971]
Manchikanti L, Pampati V, Fellows B, Baha AG. The inability of the clinical picture to characterize pain from facet joints. Pain physician. 2000 Apr:3(2):158-66 [PubMed PMID: 16906195]
Cohen SP, Bhaskar A, Bhatia A, Buvanendran A, Deer T, Garg S, Hooten WM, Hurley RW, Kennedy DJ, McLean BC, Moon JY, Narouze S, Pangarkar S, Provenzano DA, Rauck R, Sitzman BT, Smuck M, van Zundert J, Vorenkamp K, Wallace MS, Zhao Z. Consensus practice guidelines on interventions for lumbar facet joint pain from a multispecialty, international working group. Regional anesthesia and pain medicine. 2020 Jun:45(6):424-467. doi: 10.1136/rapm-2019-101243. Epub 2020 Apr 3 [PubMed PMID: 32245841]
Level 1 (high-level) evidenceConger A, Burnham T, Salazar F, Tate Q, Golish M, Petersen R, Cunningham S, Teramoto M, Kendall R, McCormick ZL. The Effectiveness of Radiofrequency Ablation of Medial Branch Nerves for Chronic Lumbar Facet Joint Syndrome in Patients Selected by Guideline-Concordant Dual Comparative Medial Branch Blocks. Pain medicine (Malden, Mass.). 2020 May 1:21(5):902-909. doi: 10.1093/pm/pnz248. Epub [PubMed PMID: 31609391]
Level 2 (mid-level) evidenceDjebbar S, Rossi IM, Adler RS. Ultrasound-Guided Cryoanalgesia of Peripheral Nerve Lesions. Seminars in musculoskeletal radiology. 2016 Nov:20(5):461-471. doi: 10.1055/s-0036-1596063. Epub 2016 Dec 21 [PubMed PMID: 28002868]
Chang KV, Hung CY, Wang TG, Yang RS, Sun WZ, Lin CP. Ultrasound-Guided Proximal Suprascapular Nerve Block With Radiofrequency Lesioning for Patients With Malignancy-Associated Recalcitrant Shoulder Pain. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2015 Nov:34(11):2099-105. doi: 10.7863/ultra.14.12042. Epub 2015 Oct 9 [PubMed PMID: 26453125]
Tekin I, Mirzai H, Ok G, Erbuyun K, Vatansever D. A comparison of conventional and pulsed radiofrequency denervation in the treatment of chronic facet joint pain. The Clinical journal of pain. 2007 Jul-Aug:23(6):524-9 [PubMed PMID: 17575493]
Level 1 (high-level) evidenceToukhy ME, Campkin NT. Severe diarrhea following neurolytic coeliac plexus block: case report and literature review. The American journal of hospice & palliative care. 2011 Nov:28(7):511-4. doi: 10.1177/1049909111402185. Epub 2011 Mar 21 [PubMed PMID: 21422068]
Level 3 (low-level) evidenceDobrogowski J, Wrzosek A, Wordliczek J. Radiofrequency denervation with or without addition of pentoxifylline or methylprednisolone for chronic lumbar zygapophysial joint pain. Pharmacological reports : PR. 2005 Jul-Aug:57(4):475-80 [PubMed PMID: 16129914]
McCormick ZL, Conger A, Kendall R, Wagner G, Henrie AM, Littell M, Sperry BP, Petersen R, Cooper AN, Teramoto M, Burnham TR. A pragmatic randomized prospective trial of cooled radiofrequency ablation of the medial branch nerves versus facet joint injection of corticosteroid for the treatment of lumbar facet syndrome: 12 month outcomes. Pain medicine (Malden, Mass.). 2023 Dec 1:24(12):1318-1331. doi: 10.1093/pm/pnad107. Epub [PubMed PMID: 37578437]
Level 1 (high-level) evidenceAbd-Elsayed A, Lee S, Jackson M. Radiofrequency Ablation for Treating Resistant Intercostal Neuralgia. Ochsner journal. 2018 Spring:18(1):91-93 [PubMed PMID: 29559878]
Jamison DE, Cohen SP. Radiofrequency techniques to treat chronic knee pain: a comprehensive review of anatomy, effectiveness, treatment parameters, and patient selection. Journal of pain research. 2018:11():1879-1888. doi: 10.2147/JPR.S144633. Epub 2018 Sep 18 [PubMed PMID: 30271194]
Iannaccone F, Dixon S, Kaufman A. A Review of Long-Term Pain Relief after Genicular Nerve Radiofrequency Ablation in Chronic Knee Osteoarthritis. Pain physician. 2017 Mar:20(3):E437-E444 [PubMed PMID: 28339444]
Amr SA, Reyad RM, Othman AH, Mohamad MF, Mostafa MM, Alieldin NH, Hamed FA. Comparison between radiofrequency ablation and chemical neurolysis of thoracic splanchnic nerves for the management of abdominal cancer pain, randomized trial. European journal of pain (London, England). 2018 Nov:22(10):1782-1790. doi: 10.1002/ejp.1274. Epub 2018 Jul 11 [PubMed PMID: 29975804]
Abd-Elsayed A, Kreuger L, Wheeler S, Robillard J, Seeger S, Dulli D. Radiofrequency Ablation of Pericranial Nerves for Treating Headache Conditions: A Promising Option for Patients. Ochsner journal. 2018 Spring:18(1):59-62 [PubMed PMID: 29559871]
Solberg J, Copenhaver D, Fishman SM. Medial branch nerve block and ablation as a novel approach to pain related to vertebral compression fracture. Current opinion in anaesthesiology. 2016 Oct:29(5):596-9. doi: 10.1097/ACO.0000000000000375. Epub [PubMed PMID: 27548307]
Cohen SP, Doshi TL, Constantinescu OC, Zhao Z, Kurihara C, Larkin TM, Griffith SR, Jacobs MB, Kroski WJ, Dawson TC, Fowler IM, White RL, Verdun AJ, Jamison DE, Anderson-White M, Shank SE, Pasquina PF. Effectiveness of Lumbar Facet Joint Blocks and Predictive Value before Radiofrequency Denervation: The Facet Treatment Study (FACTS), a Randomized, Controlled Clinical Trial. Anesthesiology. 2018 Sep:129(3):517-535. doi: 10.1097/ALN.0000000000002274. Epub [PubMed PMID: 29847426]
Huang P, Liu H, Huang L, Jin X. The long-term outcome of CT-guided radiofrequency ablation of the peripheral branches of the trigeminal nerve in trigeminal neuralgia. Neurosurgical review. 2024 Jan 6:47(1):33. doi: 10.1007/s10143-023-02269-w. Epub 2024 Jan 6 [PubMed PMID: 38182916]
Wang Z, Wang Z, Li K, Su X, Du C, Tian Y. Radiofrequency thermocoagulation for the treatment of trigeminal neuralgia. Experimental and therapeutic medicine. 2022 Jan:23(1):17. doi: 10.3892/etm.2021.10939. Epub 2021 Oct 30 [PubMed PMID: 34815769]
Karm MH, Kwon HJ, Kim CS, Kim DH, Shin JW, Choi SS. Cooled radiofrequency ablation of genicular nerves for knee osteoarthritis. The Korean journal of pain. 2024 Jan 1:37(1):13-25. doi: 10.3344/kjp.23344. Epub [PubMed PMID: 38155108]
Fabry A, Nedunchelian M, Stacoffe N, Guinebert S, Zipfel J, Krainik A, Maindet C, Kastler B, Grand S, Kastler A. Review of craniofacial pain syndromes involving the greater occipital nerve: relevant anatomy, clinical findings, and interventional management. Neuroradiology. 2024 Feb:66(2):161-178. doi: 10.1007/s00234-023-03273-z. Epub 2023 Dec 30 [PubMed PMID: 38159141]
Odonkor CA, Tang T, Taftian D, Chhatre A. Bilateral Intra-Articular Radiofrequency Ablation for Cervicogenic Headache. Case reports in anesthesiology. 2017:2017():1483279. doi: 10.1155/2017/1483279. Epub 2017 Jan 9 [PubMed PMID: 28149652]
Level 3 (low-level) evidenceFiala KJ, Martens JM, Keith MK, Ghouse A, Abd-Elsayed A. Cooled Radiofrequency Ablation for Intercostal Neuralgia. Ochsner journal. 2023 Summer:23(2):159-163. doi: 10.31486/toj.22.0087. Epub [PubMed PMID: 37323517]
Reyad RM, Ghobrial HZ, Shaker EH, Reyad EM, Shaaban MH, Hashem RH, Darwish WM. Modified technique for thermal radiofrequency ablation of Thoracic dorsal root ganglia under combined fluoroscopy and CT guidance: a randomized clinical trial. BMC anesthesiology. 2019 Dec 18:19(1):234. doi: 10.1186/s12871-019-0906-4. Epub 2019 Dec 18 [PubMed PMID: 31852438]
Level 1 (high-level) evidenceAlanbay E, Aras B, Kesikburun S, Kizilirmak S, Yasar E, Tan AK. Effectiveness of Suprascapular Nerve Pulsed Radiofrequency Treatment for Hemiplegic Shoulder Pain: A Randomized-Controlled Trial. Pain physician. 2020 Jun:23(3):245-252 [PubMed PMID: 32517390]
Level 1 (high-level) evidenceMisra S, Ward S, Coker C. Pulsed radiofrequency for chronic testicular pain-a preliminary report. Pain medicine (Malden, Mass.). 2009 May-Jun:10(4):673-8. doi: 10.1111/j.1526-4637.2009.00581.x. Epub 2009 Mar 19 [PubMed PMID: 19302438]
Vallejo R, Benyamin RM, Kramer J, Stanton G, Joseph NJ. Pulsed radiofrequency denervation for the treatment of sacroiliac joint syndrome. Pain medicine (Malden, Mass.). 2006 Sep-Oct:7(5):429-34 [PubMed PMID: 17014602]
Rozen D, Parvez U. Pulsed radiofrequency of lumbar nerve roots for treatment of chronic inguinal herniorraphy pain. Pain physician. 2006 Apr:9(2):153-6 [PubMed PMID: 16703977]
Teixeira A, Sluijter ME. Intradiscal high-voltage, long-duration pulsed radiofrequency for discogenic pain: a preliminary report. Pain medicine (Malden, Mass.). 2006 Sep-Oct:7(5):424-8 [PubMed PMID: 17014601]
Caicedo Gutiérrez L, Moreno Martínez D. Case report: Baxter's nerve radiofrequency in patient with plantar fasciitis nonresponsive to conventional treatment. Revista espanola de anestesiologia y reanimacion. 2022 May:69(5):306-309. doi: 10.1016/j.redare.2022.05.001. Epub 2022 May 13 [PubMed PMID: 35577703]
Level 3 (low-level) evidenceKallas ON, Nezami N, Singer AD, Wong P, Kokabi N, Bercu ZL, Umpierrez M, Tran A, Reimer NB, Oskouei SV, Gonzalez FM. Cooled Radiofrequency Ablation for Chronic Joint Pain Secondary to Hip and Shoulder Osteoarthritis. Radiographics : a review publication of the Radiological Society of North America, Inc. 2022 Mar-Apr:42(2):594-608. doi: 10.1148/rg.210074. Epub 2022 Feb 11 [PubMed PMID: 35148246]
Zakrzewska JM, Linskey ME. Trigeminal neuralgia. BMJ clinical evidence. 2009 Mar 12:2009():. pii: 1207. Epub 2009 Mar 12 [PubMed PMID: 19445753]
Level 1 (high-level) evidence