Introduction
The esophagus is a portion of the digestive system connecting the pharynx to the stomach, allowing the passage of food for digestion (see Figure. Digestive and Respiratory Anatomical Structures Connected to the Esophagus). The esophagus measures approximately 25 cm long in a mature adult and begins at the inferior border of the cricoid cartilage (C6 level), descending in the posterior mediastinum through the esophageal hiatus of the diaphragm and terminating at the stomach (T11 level). During its course, the esophagus encounters three anatomic constrictions: (1) at the level of the cricopharyngeus muscle, (2) as it travels posterior to the aortic arch/left mainstem bronchus, and (3) at the level of esophageal hiatus of the diaphragm. These areas of constriction are considered the most frequent sites for a foreign body or food impaction to occur.[1]
The esophagus has two functional sphincters, the upper and lower esophageal sphincters. The upper esophageal sphincter (UES) is a high-pressure zone at the transition of the pharynx and the cervical esophagus. The lower esophageal sphincter (LES) is a high-pressure zone located where the esophagus meets the stomach and protects the esophagus from the reflux of gastric contents. The LES is composed of intrinsic and extrinsic components. The intrinsic component of the LES consists of esophageal muscle fibers and is under neurohormonal control. The extrinsic component consists of the diaphragmatic crura and the phrenoesophageal ligament, which provide anatomical support to the LES and further protection against gastric reflux.[2]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
As previously discussed, the LES is comprised of an intrinsic and an extrinsic component. Any malfunction in either of these components can lead to pathologies such as gastroesophageal reflux disease (GERD) with its associated symptoms and mucosal changes. Additionally, a structurally defective LES and a hiatal hernia are important factors in the pathogenesis of reflux disease.[3] In an individual with a hiatal hernia, the new position of the LES may prevent complete closure, allowing for increased backflow of digestive juices, heartburn, and esophageal damage.[4]
Cellular Level
The intrinsic component of the LES consists of smooth muscle that keeps the sphincter tightly contracted. Direct inhibitory signals allow the smooth muscles in the LES to relax, opening the sphincter and enabling the passage of a food bolus. As the LES does not possess dilator muscles, its opening relies solely on the relaxation of the smooth muscles.[7]
At the intracellular level, LES relaxation occurs due to suppression of a resting chloride conductance by nitric oxide (NO) or activation of a potassium conductance resulting in smooth muscle hyperpolarization. Suppression of calcium influx occurs, leading to the cessation of myosin phosphorylation and muscle relaxation. Studies have shown that cyclic adenosine monophosphate (cAMP) and cyclic guanine monophosphate (cGMP) mediate LES relaxation by activating protein kinases A and G, respectively. These signaling molecules can cause smooth muscle relaxation without causing membrane hyperpolarization. Protein kinases A and G can lower free intracellular calcium by sequestering it in the endoplasmic reticulum. Both vasoactive intestinal polypeptide (VIP) and NO increase intracellular cAMP and cGMP levels. The LES relaxation induced by various physiologic stimuli is associated with an increase in the intracellular cGMP rather than the cAMP, which suggests that NO is the major nonadrenergic noncholinergic (NANC) inhibitory neurotransmitter of the LES smooth muscle.
The pressure in the LES depends on three factors: (1) the myogenic tone of the smooth muscles, (2) inhibitory nitrergic nerves, and (3) excitatory cholinergic nerves. The myogenic tone of smooth muscle is an intrinsic property of the cells in the LES and is responsible for its tonic contraction. The LES smooth muscle cells have more depolarized resting membrane potentials, resulting in spontaneous spike-like action potentials and the generation of a basal tone. Excitatory cholinergic nerves release ACh to promote smooth muscle contraction, which enhances the tonic, myogenic property of the LES and favors contraction. In contrast, the nitrergic pathway releases NO and favors inhibition, opposing the contractile properties of the LES. Overall, the combination of these forces favors contraction over relaxation. Thus, the LES remains contracted even when entirely denervated owing to its myogenic property.[23]
Development
The LES and the smooth muscle of the lower esophagus are derived from the mesodermal tissue of the somites surrounding the foregut. The embryologic origin of the gastroesophageal junction (GEJ) is still under investigation, but at this time, it is believed its function derives from gastric rotation together with augmentation of the fundus of the stomach.[5]
Function
The primary function of the LES is the protection of the esophagus from highly acidic stomach secretions. Except in the lower one-eighth of the esophagus, the esophageal mucosa cannot resist the digestive action of gastric secretions for a prolonged period. Under normal conditions, the LES remains tonically contracted with an intraluminal pressure of about 30 mmHg. When swallowing causes a peristaltic wave to pass down the esophagus, receptive relaxation of the LES occurs ahead of the peristasis, allowing for easy propulsion of the swallowed bolus into the stomach.
Intrinsic Component of LES
- Clasp Fibers
- Semicircular "C-shaped" smooth muscle fibers on the ride side of the LES
- Maintain stronger myogenic tone than sling fibers
- Not responsive to cholinergic stimulation
- Predominantly innervated by inhibitory neurons located in the body of the esophagus
- Utilize L-type calcium channels[6]
- Sling Fibers
- Oblique gastric muscle fibers found on the left side of the LES
- Weaker resting tone
- Contract vigorously to cholinergic agonists
- Predominantly innervated by excitatory neurons located in the stomach
- Responsible for the asymmetry of LES pressure
- Responsible for the maintenance of the angle of HIS and flap valve function - both of which are important in the prevention of reflux[6]
Extrinsic Component of LES
- Crural Diaphragm
- Considered the "external sphincter" of the LES
- Functions to increase pressure at the distal esophagus
- Crucial during inspiration when intrathoracic pressure decreases or during periods of increased intraabdominal pressure - both situations predispose to gastric reflux[7]
- Right Crus
- Thicker and more extensive
- Arises from lumbar vertebrae L1-L3 and divides into superficial and deep components
- Superficial component: lies to the right of the esophageal hiatus
- Deep component: lies to the left of the esophageal hiatus, lateral to the left crus
- Left Crus
- Smaller - arises from L1-L2
- Lies to the left of the esophageal hiatus
- Phrenoesophageal Ligament
- Continuation of the inferior diaphragmatic fascia
- Acts as a protective sleeve over the intraabdominal esophagus
- Upper limb: connects the distal esophagus to the superior aspect of the diaphragm
- Lower limb: connects the cardia of the stomach to the inferior aspect of the diaphragm
- Allows independent movement of the esophagus and diaphragm - protecting against gastric reflux and hiatal hernia[7]
The proper function of the LES occurs through two main mechanisms - myogenic and neural control. Myogenic control is the intrinsic rhythm of gastrointestinal smooth muscle contraction and relaxation. Neural control is achieved through the autonomic and enteric nervous systems.
The LES tonically contracts to an average pressure of 15 to 30 mmHg. After swallowing, inhibitory signals generated by peristalsis cause a reflex relaxation of the LES for approximately 5 seconds, allowing transit of the bolus into the stomach. During this time, the diaphragmatic crura also relax. After the bolus passage, the LES and crura return to their baseline contracted state. Transient LES relaxation (TLESR) is another physiologic relaxation of the LES that occurs outside of the swallowing mechanism. It is believed to be triggered by gastric distention and causes both the LES and the diaphragmatic crura to relax, allowing the release of excess gas. This process is followed by primary peristaltic waves distally to return any refluxed liquid into the stomach.[8]
Mechanism
There are four mechanisms of LES relaxation: vagus nerve stimulation-induced, swallow-induced, esophageal distention-induced, and spontaneous transient LES relaxation (TLESR).
Both sympathetic (primarily splanchnic) and parasympathetic (vagus) fibers innervate the LES, with the vagal pathway essential for the reflexive relaxation of the LES. Vagal sensory afferents from the LES and distal esophagus synapse in the nucleus tractus solitarius (NTS) of the hindbrain. Vagal efferents arise in the dorsal motor nucleus (DMN) and synapse with the myenteric plexus of the enteric nervous system. The parasympathetic system contributes to inhibitory and excitatory neurons, with excitatory nerves arising from the rostral portion of the DMN and inhibitory nerves arising from the caudal portion of the DMN. The DMN and the NTS form a dorsal vagal complex in the hindbrain that coordinates reflex control of the sphincter.
As previously discussed, excitatory impulses are primarily cholinergic-mediated via ACh, with minor contributions by tachykinins (substance P, neurokinin A/B). Inhibitory impulses are primarily nitrergic-mediated (nitric oxide) with smaller contributions by other compounds, including vasoactive inhibitory peptide (VIP), purine structures (particularly ATP), and carbon monoxide. Due to this dual innervation by the vagus nerve, a bilateral vagotomy or tetrodotoxin (pufferfish toxin which blocks neural transmission via sodium-channel blockade) administration elicits no change in baseline LES tone. Conversely, blockade of the inhibitory neurons (with NO inhibitors) or excitatory neurons (with atropine, an anti-cholinergic) leads to unopposed action of the opposite system. While the vagus elicits dual effects, there have been suggestions that the inhibitory effect is more significant, as studies have demonstrated that vagal stimulation leads to net LES relaxation.[9]
For proper transport of ingested contents into the stomach, relaxation of the LES and diaphragmatic sphincter must occur. The action of swallowing and distention of the esophagus are the two major stimuli that induce EGJ relaxation. Swallowing-induced LES relaxation occurs through the release of VIP and NO, begins within 2 seconds of the onset of swallowing, and lasts approximately 6 to 10 seconds.[10] LES relaxation is terminated by the arrival of the peristaltic esophageal contraction at the LES and is subsequently followed by an after-contraction that can last up to 10 seconds. An after-contraction is seen only in the upper portion of the LES, while the pressure within the lower LES returns to its resting pressure level (15 to 30 mmHg). While in the upright position, the swallowed bolus may reach the LES quickly, owing to gravity. In this situation, the bolus may be briefly held at the LES before passage into the stomach. The LES typically relaxes to a pressure close to the intragastric pressure (approximately 3.0 mmHg).[11]
The LES must not only relax but open enough to allow passage of the bolus into the stomach. It is necessary to understand the difference between opening and relaxation, as manometry measures the relaxation of the LES and not the opening function. As long as the LES intraluminal diameter is greater than the size of the manometry catheter, the catheter records complete relaxation. However, for the bolus to pass through the LES, it must open to the diameter of the bolus. LES relaxation is an active process mediated by neurotransmitters, but opening is related to the passive properties of the LES. Under normal circumstances, an opening of 13 mm is required for a bolus to pass freely into the stomach.[12]
Transient Lower Esophageal Sphincter Relaxation (TLESR)
TLESR is the spontaneous relaxation of the LES in the absence of swallowing. While swallow-induced LES relaxation is a physiologic mechanism for the antegrade flow of food, gastric distention-induced TLESR is a physiologic mechanism allowing for the retrograde flow of stomach contents into the esophagus. Vomiting, belching, and physiologic reflux in normal subjects occur through the mechanism of TLESR. While TLESR is a physiologic mechanism seen in both normal individuals and patients with GERD, TLESR is widely considered the primary mechanism of GERD.
Typically, TLESR is of longer duration than swallow-induced LES relaxation, lasting approximately 10 to 45 seconds. The criteria for the definition of TLESR are:
- Absent pharyngeal swallow signal 4 seconds before to 2 seconds after the onset of LES relaxation
- LES pressure fall of 1 mmHg/sec
- A time of 10 seconds from the onset of relaxation to complete relaxation
- A nadir pressure of 2 mmHg
Gastric distention (air or food contents) triggers TLESR. Stomach distention triggers a vasovagal reflex that results in TLESR, which acts as a protective mechanism by preventing the accumulation of excess gas in the stomach from entering the duodenum.[13]
Motilin, a neurohumoral agent released into the circulation by specialized cells in the wall of the intestines, is responsible for phasic LES contraction. Phasic contraction of the proximal portion of the LES also occurs following swallow-induced or esophageal distention-induced LES relaxation. Contraction occurring post relaxation is coordinated with esophageal peristalsis and is atropine sensitive. For example, an atropine dose of 15 g/kg reduces LES pressure by 50 to 70% in humans.
Related Testing
Barium Esophagography - This is often the first study obtained in the workup of dysphagia, dyspepsia, or regurgitation. It is non-invasive and used primarily to assess the structural integrity of the esophagus, identifying hiatal hernias, leaks, diverticula, obstructions, and other structural malformations. This study can grossly assess esophageal motility, but a modified barium swallow performed with a speech pathologist more accurately assesses functional swallowing. While barium provides better contrast than water-soluble solutions, in cases of suspected esophageal perforation, the use of barium increases the risk of inflammatory mediastinitis. A barium esophagogram should not be obtained in cases of acute chemical injury.[14]
Esophagogastroduodenoscopy (EGD) - Upper endoscopy allows for the direct visualization of the pathology in question. It is particularly useful in assessing reflux esophagitis, Barrett metaplasia, strictures, masses, suspected upper GI bleeds, varices, and hiatal hernias. Endoscopy allows for select interventions, including biopsy, foreign body removal, stricture dilation, ligation of bleeding vessels, and pharmacologic injections. The most serious risk of this procedure is esophageal perforation, which occurs in < 1% of cases.[15]
Esophageal pH Monitoring - This is the gold standard for the diagnosis of gastroesophageal reflux disease. This test allows for 24-hr pH monitoring of the lower esophagus, measuring 6 data points to determine the Demeester score (DMS). The DMS is a composite score of acid exposure during prolonged pH monitoring, with a score of >14.72 indicating reflux.[16] The criteria are:
- Percentage of total time pH<4
- Percentage of upright time pH<4
- Percentage of supine time pH<4
- Number of reflux episodes
- Number of reflux episodes lasting > 5 minutes
- Longest reflux episode
The calculation can usually be performed via phone app or website; however, for completeness, the scoring value equation is SVn = (X-A)/SD+1
X= detection value, A = mean value, SD = standard deviation
A composite DMS score is then obtained by adding the six values, such that DMS = SV1 + SV2 + SV3 + SV4 + SV5 + SV6
Score interpretation:
- DMS < 14.72 GERD negative
- DMS 14.72 - 50 mild GERD
- DMS 51 - 100 moderate GERD
- DMS > 100 severe GERD
Esophageal Manometry (EM) - This is a direct measurement of the intraluminal pressure at multiple levels within the esophagus. EM assesses UES function, LES function, and motility within the esophageal body. Manometry is most useful in the workup of suspected achalasia, esophageal spasm, and GERD.[17]
Pathophysiology
Gastroesophageal Reflux Disease (GERD) - A common digestive disorder in the western world, the characteristic presentation of GERD shows the retrograde movement of gastric contents across the LES into the esophagus. Predisposing factors for GERD include an incompetent LES, hiatal hernia, a short intraabdominal esophagus, diaphragmatic crura or phrenoesophageal ligament weakness, and elevated intraabdominal pressure. The most common symptoms reported by patients are heartburn and regurgitation. Less common symptoms include cough, hoarseness, and chest pain.
Esophageal pH monitoring is the gold standard for diagnosing GERD, but barium studies and endoscopy can also play a role in evaluating for hiatal hernia and Barrett metaplasia. Medical treatment is often preferable as behavioral modification and acid-reducing medications (PPIs, H2-antagonists) are effective in many cases. Surgery is an option for patients who fail conservative management to restore length to the intraabdominal esophagus, close the crura of the diaphragm, and reinforce the LES via fundoplication.
Complications of GERD include stricture formation and Barrett metaplasia. Intestinal metaplasia can predispose patients to dysplasia and adenocarcinoma of the esophagus.[18] It might be assumed that a weakness of the LES or the diaphragmatic sphincter is the cause of GERD, but this is not precisely the case. While it is true that some patients with reflux disease have a weak LES, in the majority of patients, especially those with mild to moderate reflux disease, the LES pressure is normal.
Achalasia - A rare esophageal disorder caused by denervation of the myenteric (Auerbach) plexus, leading to failure of LES relaxation and loss of esophageal peristalsis. Patients typically complain of dysphagia progressing from solids to liquids, regurgitation, and possibly a foreign body sensation of the lower esophagus. Barium swallow reveals narrowing of the LES and proximal dilation of the esophagus ('bird beak' appearance). Esophageal manometry reveals a failure of LES relaxation and the absence of normal esophageal peristalsis. Endoscopy is necessary to rule out distal obstruction (pseudoachalasia). While conservative treatment with oral nitrates and calcium-channel blockers has been attempted, they are minimally effective.
Endoscopic treatment options include balloon dilation of the LES, botox injections, and peroral endoscopic myotomy (POEM). Balloon dilations and botox injections are effective in the short-term but require repeat treatments. Repetitive dilations increase the risk of esophageal perforation. POEM involves submucosal tunneling with circular myotomy of the LES and increases the risk for GERD as the LES is rendered incompetent. Surgical management with Heller myotomy is possible via open or laparoscopic techniques and includes fundoplication to prevent reflux.[19]
Hiatal hernia - Herniation of the esophagus, stomach, or other structures through the esophageal hiatus of the diaphragm. There are four types:
- Type I - also known as sliding hiatal hernias, involves the gastroesophageal junction (GEJ) and LES retracting superiorly above the diaphragm. This is the most common type and frequently occurs with laxity of the phrenoesophageal ligament. Intermittent loss of tension from the diaphragmatic crura predisposes these patients to GERD.
Types II-IV are all forms of paraesophageal hernias, which involves herniation of the stomach through the esophageal hiatus.
- Type II - purely paraesophageal, with the GEJ remaining in place
- Type III - mixed sliding-paraesophageal hernia
- Type IV - paraesophageal hernia with herniation of another GI organ (commonly the colon or spleen) through the hiatus
Paraesophageal hernias increase the risk of stomach entrapment, with subsequent ischemia and infarction. Diagnosis can be suggested by an abdominal X-ray, with the finding of an air-fluid level above the diaphragm, but it is confirmed with a contrast upper GI study.
Treatment of asymptomatic sliding hernias often consists of conservative management, while symptomatic cases are treated surgically similarly to GERD. Asymptomatic paraesophageal hernias are controversial, with some advocating for surgical repair to remove the risk of incarceration. In contrast, others argue that this complication is rare and watchful waiting can be appropriate. Symptomatic paraesophageal hernias require surgical repair.[20]
Esophageal Foreign Body - Foreign body ingestion is most common in pediatric patients and patients with cognitive disabilities. Three likely locations for esophageal entrapment are the areas of anatomic constriction, the UES/cricopharyngeus, the crossover of the aorta/left main-stem bronchus, and the esophageal hiatus. Approximately 75% of foreign bodies ingested in pediatric patients are trapped at the UES, while a distal esophageal stricture traps 67% of foreign bodies in adults.
Patients often present complaining of a foreign body sensation, chest pain, or inability to swallow. Drooling, or the inability to swallow secretions is a concerning feature indicative of an emergent obstruction. High-risk objects include batteries, magnets, and sharp objects. Batteries lodged in the esophagus can cause thermal injury to the mucosa, increasing the risk of bleeding and perforation. Sharp objects also increase the risk of perforation. Multiple magnets become a concern in the lower GI tract, where they can become separated and reattach across the bowel wall, increasing the risk for infarction and perforation of the bowel.
Diagnosis can often be made on chest X-ray, with anterior-posterior and lateral films to localize the object. Cervical or mediastinal emphysema are clues to esophageal perforation. Treatment is frequently endoscopic removal, but surgical removal can be performed with failure of endoscopic removal or in cases of esophageal perforation.[21]
Hypertensive LES - A hypertensive LES is a poorly characterized motility disorder associated with symptoms of chest pain and dysphagia. A hypertensive LES is classified as an LES with a mean pressure > 45 mmHg, relaxation greater than 75%, and normal peristalsis. Studies have determined hypertensive LES to be a heterogeneous disorder, with such causes as GERD, anxiety, and somatization. Despite abnormal LES parameters, most patients have normal esophageal function and frequent psychological abnormalities.[22]
Clinical Significance
The physiologic factors controlling LES function are interrelated in a complex fashion. They include the autonomic nerve supply, gastrointestinal hormones, and specific characteristics of the circular smooth muscle at the EGJ. A defect in any of these three controlling mechanisms would result in a clinically recognizable symptom complex. Abnormalities with either high or low LES pressure have been shown to relate to these specific aspects. Studies of the effects of various foods and other agents that decrease or increase LES pressure are of therapeutic interest in patients with reflux symptoms. Decreases in LES pressure after fat ingestion may explain a mechanism for many cases of fatty food intolerance. Pressure decreases after chocolate ingestion, after smoking, and after alcohol; all have strong therapeutic implications in patients with chronic heartburn.[23]
With GERD being a chronic and highly prevalent disorder worldwide, it is a diagnosis that a healthcare provider will undoubtedly see. Understanding the myogenic factors, neural circuitry, and neurotransmitters involved in maintaining the basal tone, sphincter relaxation, and induction of TLESR is of significant clinical importance in the clinical and pharmacologic approaches to anti-reflux therapy.
While it is well known that the LES must relax for vomiting to occur, it is also clinically important to understand at which age this is a normal process. Esophageal peristalsis has been observed by ultrasound examination in the 2nd trimester of pregnancy, but the LES is found to be immature at term. Reflux of breast milk from the stomach into the esophagus through the immature LES is quite common. Approximately 75% of newborns suffer from regurgitation within the first two weeks of their life. The pressure of the LES becomes equal to that of adult pressure at approximately the 3rd to 6th week of life, with regurgitation almost entirely resolved without intervention by the end of the first year of life.[24]
As the LES plays an essential role in swallowing, detailed knowledge of its physiology and pathophysiology can assist in the understanding and diagnosis of esophageal pathology, dysphagia, and related disorders. Normal LES function allows food transit from the esophagus into the stomach and prevents the reflux of gastric contents back into the esophagus. Improper relaxation of the LES can lead to food entrapment in the esophagus, achalasia, and an increased risk of esophageal squamous cell carcinoma. An incompetent LES can lead to GERD, increasing the risk for metaplasia and esophageal adenocarcinoma. Rapid identification of esophageal disorders is of utmost clinical importance and can impact a patient's quality of life and long-term morbidity and mortality.
Media
(Click Image to Enlarge)
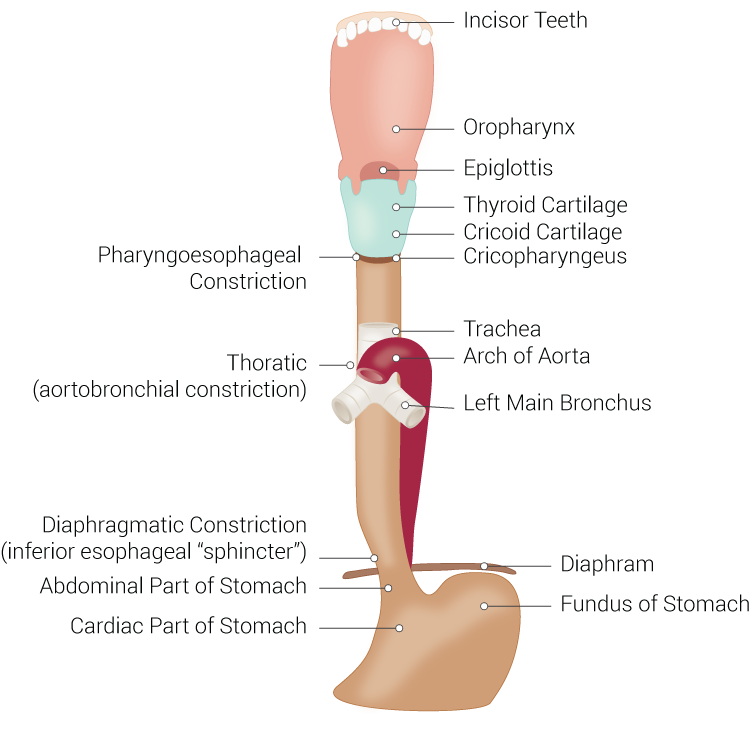
Digestive and Respiratory Anatomical Structures Connected to the Esophagus. Structures include the esophagus, incisor teeth, oropharynx, epiglottis, thyroid cartilage, cricoid cartilage, cricopharyngeus, trachea, arch of aorta, left main bronchus, diaphragm, fundus of stomach, cardiac part of stomach, abdominal part of stomach, diaphragmatic constriction, inferior esophageal sphincter, thoracic, aortobronchial constriction, and pharyngoesophageal constriction.
Illustration by B Palmer
References
Chaudhry SR, Bordoni B. Anatomy, Thorax, Esophagus. StatPearls. 2024 Jan:(): [PubMed PMID: 29494119]
Bajwa SA, Toro F, Kasi A. Physiology, Esophagus. StatPearls. 2024 Jan:(): [PubMed PMID: 30085553]
Fein M, Ritter MP, DeMeester TR, Oberg S, Peters JH, Hagen JA, Bremner CG. Role of the lower esophageal sphincter and hiatal hernia in the pathogenesis of gastroesophageal reflux disease. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 1999 Jul-Aug:3(4):405-10 [PubMed PMID: 10482693]
Hyun JJ, Bak YT. Clinical significance of hiatal hernia. Gut and liver. 2011 Sep:5(3):267-77. doi: 10.5009/gnl.2011.5.3.267. Epub 2011 Aug 18 [PubMed PMID: 21927653]
Rishniw M, Rodriguez P, Que J, Burke ZD, Tosh D, Chen H, Chen X. Molecular aspects of esophageal development. Annals of the New York Academy of Sciences. 2011 Sep:1232():309-15. doi: 10.1111/j.1749-6632.2011.06071.x. Epub [PubMed PMID: 21950820]
Level 3 (low-level) evidenceLiebermann-Meffert D, Allgöwer M, Schmid P, Blum AL. Muscular equivalent of the lower esophageal sphincter. Gastroenterology. 1979 Jan:76(1):31-8 [PubMed PMID: 81791]
Brasseur JG, Ulerich R, Dai Q, Patel DK, Soliman AM, Miller LS. Pharmacological dissection of the human gastro-oesophageal segment into three sphincteric components. The Journal of physiology. 2007 May 1:580(Pt.3):961-75 [PubMed PMID: 17289789]
Kim HI, Hong SJ, Han JP, Seo JY, Hwang KH, Maeng HJ, Lee TH, Lee JS. Specific movement of esophagus during transient lower esophageal sphincter relaxation in gastroesophageal reflux disease. Journal of neurogastroenterology and motility. 2013 Jul:19(3):332-7. doi: 10.5056/jnm.2013.19.3.332. Epub 2013 Jul 8 [PubMed PMID: 23875100]
Tobias A, Sadiq NM. Physiology, Gastrointestinal Nervous Control. StatPearls. 2024 Jan:(): [PubMed PMID: 31424852]
Pouderoux P, Verdier E, Kahrilas PJ. Patterns of esophageal inhibition during swallowing, pharyngeal stimulation, and transient LES relaxation. Lower esophageal sphincter. American journal of physiology. Gastrointestinal and liver physiology. 2003 Feb:284(2):G242-7 [PubMed PMID: 12388187]
El-Serag HB, Tran T, Richardson P, Ergun G. Anthropometric correlates of intragastric pressure. Scandinavian journal of gastroenterology. 2006 Aug:41(8):887-91 [PubMed PMID: 16803686]
Pettersson GB, Bombeck CT, Nyhus LM. The lower esophageal sphincter: mechanisms of opening and closure. Surgery. 1980 Aug:88(2):307-14 [PubMed PMID: 7394711]
Level 3 (low-level) evidenceBanovcin P Jr, Halicka J, Halickova M, Duricek M, Hyrdel R, Tatar M, Kollarik M. Studies on the regulation of transient lower esophageal sphincter relaxations (TLESRs) by acid in the esophagus and stomach. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus. 2016 Jul:29(5):484-9. doi: 10.1111/dote.12357. Epub 2015 Apr 15 [PubMed PMID: 25873206]
Chen A, Tafti D, Tuma F. Barium Swallow. StatPearls. 2024 Jan:(): [PubMed PMID: 29630228]
Ahlawat R, Hoilat GJ, Ross AB. Esophagogastroduodenoscopy. StatPearls. 2024 Jan:(): [PubMed PMID: 30335301]
Butt I, Kasmin F. Esophageal pH Monitoring. StatPearls. 2024 Jan:(): [PubMed PMID: 31971729]
Baldwin D, Puckett Y. Esophageal Manometry. StatPearls. 2024 Jan:(): [PubMed PMID: 32644663]
Antunes C, Aleem A, Curtis SA. Gastroesophageal Reflux Disease. StatPearls. 2024 Jan:(): [PubMed PMID: 28722967]
Momodu II, Wallen JM. Achalasia. StatPearls. 2024 Jan:(): [PubMed PMID: 30137800]
Smith RE, Sharma S, Shahjehan RD. Hiatal Hernia. StatPearls. 2025 Jan:(): [PubMed PMID: 32965871]
Schaefer TJ, Trocinski D. Esophageal Foreign Body. StatPearls. 2024 Jan:(): [PubMed PMID: 29489297]
Waterman DC, Dalton CB, Ott DJ, Castell JA, Bradley LA, Castell DO, Richter JE. Hypertensive lower esophageal sphincter: what does it mean? Journal of clinical gastroenterology. 1989 Apr:11(2):139-46 [PubMed PMID: 2661657]
Level 3 (low-level) evidenceCastell DO. Physiology and pathophysiology of the lower esophageal sphincter. The Annals of otology, rhinology, and laryngology. 1975 Sep-Oct:84(5 Pt 1):569-75 [PubMed PMID: 1190666]
Czinn SJ, Blanchard S. Gastroesophageal reflux disease in neonates and infants : when and how to treat. Paediatric drugs. 2013 Feb:15(1):19-27. doi: 10.1007/s40272-012-0004-2. Epub [PubMed PMID: 23322552]