Introduction
Esophagitis refers to inflammation or injury to the esophageal mucosa. There are many causes of esophagitis and essentially the presentation is similar which include retrosternal chest, heartburn, dysphagia or odynophagia.[1][2]
One of the most common causes is gastroesophageal reflux, which can lead to erosive esophagitis. Other etiologies include radiation, infections, local injury caused by medications, pill esophagitis, and eosinophilic esophagitis (EoE). The most common symptoms in patients with esophagitis are chest pain, odynophagia, and dysphagia. Patients with EoE may present with food impaction. If the esophagitis is severe and leads to strictures, fistulization, and perforation, patients may present with symptoms related to those entities.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Multiple etiologies for esophagitis have been identified such as reflux esophagitis, Medication (Pills) induced esophagitis, infectious , eosinophilic and radiation esophagitis.[3]
- Reflux or erosive esophagitis that occurs because of the reflux of gastric contents into the stomach leading to mucosal injury is one of the most common causes of esophagitis.
- Infection esophagitis can be caused by bacteria, viruses, fungal and parasitic microorganisms with the least common being bacteria and the most common being fungal.
- Pill induced esophagitis is most commonly associated with oral bisphosphonates like alendronate, some antibiotics like tetracycline, doxycycline, and clindamycin. NSAIDs, aspirin, ferrous sulfate, potassium chloride, and mexiletine has also been reported as a cause of pill-induced esophagitis.
- Eosinophilic esophagitis (EoE) is now thought to be a chronic immune antigen-related esophageal disease with almost similar symptoms of esophagitis but histologically have squamous mucosal inflammation caused by predominant eosinophilic infiltration.[4]
- Radiation-induced esophagitis is associated with radiotherapy related toxicity and can present as both in acute and chronic forms.
Epidemiology
Epidemiology varies depending on the subset to which one refers.[5][6][7]
- Professionals estimate that 1% of the population suffers from erosive esophagitis.
- Medication-induced esophagitis has an estimated incidence of 3.9 per 100,000 population per year with a mean age at diagnosis of 41.5 years.
- Many studies have tried to identify the most accurate incidence and prevalence of eosinophilic esophagitis. The estimated incidence is 0.35 per 100,000 population with a prevalence of 55 per 100,000 population has been associated with food allergies, asthma, and eczema. It appears to be more common in males who usually present with symptoms in their 2nd or 3rd decade.
- Radiation esophagitis is a relatively frequent complication of radiation therapy. Acute injury invariably occurs at doses of 6000 cGy given in fractions of 1000 cGy per week. Lower doses or longer schedules are associated with lower rates of radiation esophagitis.
- For infectious esophagitis, the numbers are not very easy to define. One thing that is certain is that is way more prevalent in patients who are immunocompromised such as HIV-infected patients and patients with hematological malignancies.
Pathophysiology
The pathophysiology also depends in large part on the subset of esophagitis to which one refers.[8][9][10]
- Reflux esophagitis: Abnormal amount and frequent reflux of gastric content into the esophagus lead to mucosal injury. Several mechanisms take place in the pathophysiology of reflux. See more information in the Gastroesophageal Reflux Disease (GERD) chapter. Briefly, the lower esophageal sphincter (LES) seems to have decreased tone and increased transient relaxations. These factors facilitate the anterograde flow of acid. Also, patients with large Hiatal hernias seem to have a higher incidence of reflux since they contribute to a decreased tone in the LES. In contrast, any conditions that decrease esophageal peristalsis or affects saliva content can affect the protective mechanisms in place to prevent esophageal injury, contributing to the development of reflux esophagitis.
- Medication-induced esophagitis: The pathogenesis of medication-induced esophagitis involves a direct irritant effect and disruption of cytoprotective barriers. Researchers hypothesize that prolonged contact of irritants with the esophageal mucosa can lead to damage. Medications like doxycycline, tetracyclines, and ferrous sulfate can cause local caustic injury as they have a pH of less than three once dissolved in water or saliva. Other medications such as potassium chloride can cause tissue destruction and vascular injury due to its hyperosmolar nature.
- Eosinophilic esophagitis: The pathogenesis of EoE is incompletely defined. Considerable evidence suggests that eosinophilic esophagitis is an allergic disorder induced by antigen sensitization either through foods and/or aeroallergens. Eotaxin, interleukin 5 (IL-5) and STAT6 may play important roles. Some patients have at least partially improved symptoms with acid suppression therapy suggesting that acid reflux may be a contributor.
- Radiation esophagitis: The pathophysiology involves DNA damage and cell death from high-energy electrons leading to the formation of volatile oxygen-free radicals. The radiation injury can be acute or chronic. In the acute phase, radiation destroys epithelial cells and interferes with proliferation. Small doses can lead to villous blunting and minor alterations in mucosal formation, but larger doses can denude extensive regions of the mucosa. The chronic injury seems to involve small vessel ischemic injury. Endothelial inflammation coupled with smooth muscle and fibroblast proliferation compromise blood flow into the small vessels. Excessive fibrosis and the presence of atypical fibroblasts characterizes chronic radiation injury. Progressive injury can lead to strictures, ulceration, fistula formation and even perforation.
- Infectious esophagitis: Infection esophagitis can be caused by bacterial, fungal, parasitic and viral micro-organisms. Bacterial esophagitis is the least common of all. Candida albicans infection is the most common cause of infectious esophagitis. The first step in the pathophysiology involves colonization with mucosal adherence and proliferation. The second step involves impairing the host defense mechanisms. C. Albicans is a normal component of oral flora, but it can become a problem if their number increases (e.g., with the use of antibiotics) or if the patient is immunosuppressed (e.g., by therapy with corticosteroids). Herpes simplex virus (HSV) is the most common cause of viral esophagitis. It infects the squamous epithelium leading to vesicles and then ulcerations. Cytomegalovirus (CMV), Epstein-Barr (EBV) and varicella-zoster (VZV) are other viral causes of viral esophagitis.
Histopathology
Reflux esophagitis histopathology usually not very specific. common findings are dilation of intercellular space and neutrophils and eosinophils infiltration. Eosinophilic infiltration if present in GERD esophagitis can mimic eosinophilic esophagitis however it also responds to treatment with proton pump inhibitors in contrast with eosinophilic esophagitis
Eosinophilic esophagitis histopathology shows intraepithelial eosinophils and usually requires at least 15/HPF eosinophils in at least one biopsy sample to diagnose EoE.
Multinucleated giant cells with ballooning and degeneration of squamous cells with Cowdry type A inclusion is pathognomonic diagnosis finding for HSV esophagitis and Large cells with both intracytoplasmic inclusions and amphophilic intranuclear inclusions are seen in CMV esophagitis.[11][5]
History and Physical
The most common symptoms and signs are retrosternal chest pain, Heartburns, odynophagia or dysphagia. Patients with EoE can present with food impaction and more often seen in young adults or children with some history of asthma, food allergy or atopy. Reflux esophagitis symptoms may include Globus sensation, regurgitation and sometimes wheezing or chronic cough. History should be included regarding commonly known medicine ingestion which can cause pill-induced esophagitis. History of cancer and radiation therapy can provide a clue regarding radiation esophagitis.
Evaluation
Diagnosis of esophagitis can be made based on history and clinical examination however to differentiate subtypes of esophagitis requires endoscopy and biopsy examination. In suspected acid reflux esophagitis if symptoms are mild to moderate then an endoscopy may not be required and can be reserved if poor or failed response to proton pump inhibitors. Similarly, if the history is very suggestive of medication-induced (pill) esophagitis, endoscopy may not be initially required.
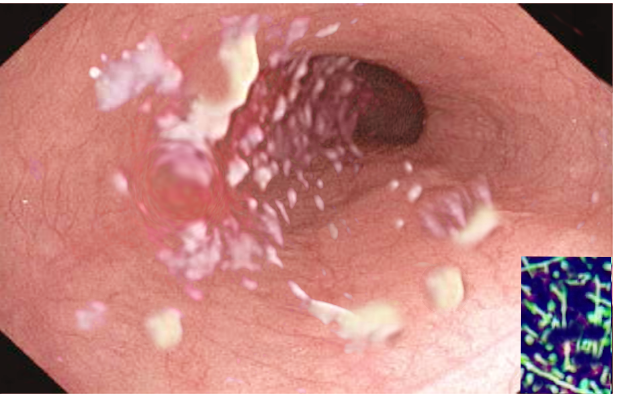
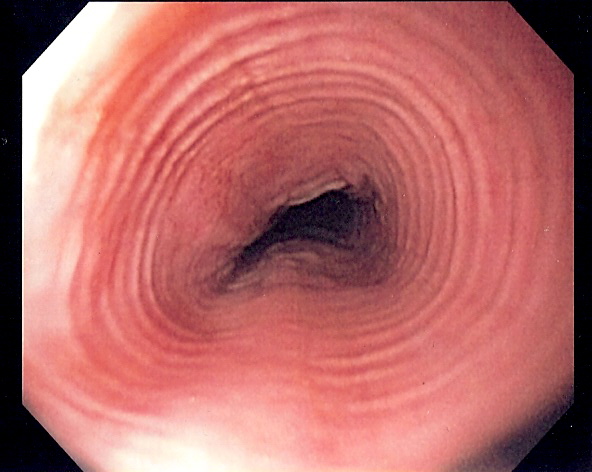
The endoscopic appearance of the mucosal lesions can help with diagnosis. In patients with suspected eosinophilic esophagitis, endoscopy may reveal white exudates or papules, red furrows, corrugated concentric rings, and strictures; but endoscopy may be normal in up to 10% of patients. Endoscopic signs of candidiasis are small, diffuse, linear, yellow-white "cheese-like" plaques adherent to the mucosa. CMV esophagitis is characterized by several large, shallow, superficial ulcerations. HSV esophagitis results in multiple small, deep ulcerations.
Endoscopic biopsy of esophageal lesion histology study can differentiate and confirm different esophagitis etiology. Patients with eosinophilic esophagitis on histology will have a characteristic eosinophilic infiltration (> 15 eosinophils per high-power field). Histology can also be helpful in the diagnosis of infectious etiologies. Multinucleated giant cells with ballooning and degeneration of squamous cells are diagnostic of HSV esophagitis with Cowdry type A inclusions being pathognomonic. Large cells with both intracytoplasmic inclusions and amphophilic intranuclear inclusions are suggestive of CMV esophagitis.[11][5]
Treatment / Management
Treatment depends on the etiology but core principles of treatment in addition to etiology specific treatment include acid suppression with PPI or H2 blockers, lifestyle modification, liquid to soft or puree diet to allow adequate time for healing and dietary modification. If the etiology appears to be acid reflux based on history then the use of H2 blockers twice a day or proton-pump inhibitors daily is indicated initially. Patient should also be advised of lifestyle and dietary modifications which include weight loss, elevating the head end of bed (patient with nocturnal symptoms of cough, hoarseness, sore throat), elimination of some dietary triggers such as fatty food, chocolate, carbonated drinks, spicy food, smoking, and alcohol. If the etiology is medication-induced esophagitis, the medication should be stopped if possible and if necessary then should be switched to any other alternatives. The patient should be instructed to take pills with 4 oz of water and remain upright for 30 min after taking the pills. For eosinophilic esophagitis treatment include acid suppression, topical or systemic steroids either topical budesonide or fluticasone and dietary modification if a food allergy is suspected. If etiology is infectious, target therapy is indicated. For C. Albicans, oral fluconazole is the drug of choice. For HSV esophagitis, treatment is oral or intravenous acyclovir and Foscarnet for those who are non-responders. CMV esophagitis is treated with Gancyclovir or Valganciclovir. Treatment of complications like stenosis or stricture may require endoscopic dilation. Addition of topical anesthesia like topical lidocaine (e.g. GI cocktail) and opioids may help in ulcers related pain. NSAIDs must be avoided as it may exacerbate symptoms.[12][13][14]
Differential Diagnosis
In general, all types of esophagitis can mimic each other as the initial clinical presentation is usually similar and will require further detailed history and further diagnostic test including endoscopy and histopathology examination. Histologically Reflux esophagitis can closely mimic eosinophilic esophagitis. In these cases, usual clinical practice is to prescribe Proton pump inhibitors (PPI) for 8 weeks. Acid reflux esophagitis usually responds well to PPI treatment with a resolution of eosinophilic infiltration but the persistence of clinical symptoms or eosinophilic infiltration on repeat endoscopy confirms EoE. Endoscopy appearance of the esophageal lesion with histology also confirm different types of infectious esophagitis.
Because retrosternal chest pain and dysphagia or odynophagia are common symptoms are shared by many other diseases differential diagnosis is usually broad. Some important differential diagnosis which must be considered is acute coronary syndrome with atypical chest pain, malignancy, peptic ulcer disease, rings and webs, pneumonia, pulmonary embolism, achalasia, and esophageal motility disorder.
Radiation Oncology
Irradiation therapy for treatment of thoracic ,head and neck or abdominopelvic malignancy can cause radiation induced esophageal injury . Treatment
Complications
Complication of chronic and untreated esophagitis includes
- Bleeding
- Stricture
- Barrett esophagus
- Perforation
- Laryngitis
- Aspiration pneumonitis
Consultations
Gastroenterology service is required in the comprehensive management of esophagitis including diagnosis and treatment of esophagitis related complications. Dietary consultation can be useful in-patient education regarding dietary modification
Deterrence and Patient Education
Lifestyle and dietary modifications are important parts of treatment and further prevention of esophagitis. Patient with Acid reflux esophagitis who are overweight should try for weight loss. Common dietary triggers and habits which include fatty and spicy meals, coffee, carbonated drinks, spicy food, chocolate, alcohol, smoking and not keeping enough time between dinner and bedtime should be avoided. The elevating head end of the bed to 30-45 degree can help with nocturnal symptoms of acid reflux include night cough, sore throat and voice hoarseness. Patient diagnosed with EoE should avoid foods they are allergic to. Maintenance of small meals, clear liquid or soft puree diet during treatment can help with symptoms and accelerate healing time.[15]
Enhancing Healthcare Team Outcomes
There are many causes of esophagitis and healthcare workers in many disciplines will encounter these patients. To avoid delay in diagnosis, an interprofessional approach is necessary. The prognosis for most patients is good with prompt treatment, but ultimately the outcomes depend on the underlying cause. When esophagitis is recurrent, it can lead to anxiety and absenteeism from work because of the need to rule out other more serious causes of chest pain. Untreated esophagitis can lead to stricture formation and malnutrition. Both bleeding and perforation are also relatively common complications. Some patients may aspirate and develop pneumonitis or worsening of asthma. In most patients who do not change their lifestyle, recurrences are common, and thus life long therapy is required. In immunocompromised patients, both candida and herpes can lead to severe pain, dysphagia, and weight loss. Patient education is key when a diagnosis of esophagitis is made. The patient should be told to sleep with the head of bed elevated, avoid lying supine after a meal and lose weight. The patient should also avoid caffeinated beverages, alcohol and discontinue smoking. Finally, the patient should be told to avoid NSAIDS.[16][17]
Media
(Click Image to Enlarge)
References
Habbal M, Scaffidi MA, Rumman A, Khan R, Ramaj M, Al-Mazroui A, Abunassar MJ, Jeyalingam T, Shetty A, Kandel GP, Streutker CJ, Grover SC. Clinical, endoscopic, and histologic characteristics of lymphocytic esophagitis: a systematic review. Esophagus : official journal of the Japan Esophageal Society. 2019 Apr:16(2):123-132. doi: 10.1007/s10388-018-0649-1. Epub 2018 Oct 29 [PubMed PMID: 30370453]
Level 1 (high-level) evidenceGomez Torrijos E, Gonzalez-Mendiola R, Alvarado M, Avila R, Prieto-Garcia A, Valbuena T, Borja J, Infante S, Lopez MP, Marchan E, Prieto P, Moro M, Rosado A, Saiz V, Somoza ML, Uriel O, Vazquez A, Mur P, Poza-Guedes P, Bartra J. Eosinophilic Esophagitis: Review and Update. Frontiers in medicine. 2018:5():247. doi: 10.3389/fmed.2018.00247. Epub 2018 Oct 9 [PubMed PMID: 30364207]
Hoversten P, Kamboj AK, Katzka DA. Infections of the esophagus: an update on risk factors, diagnosis, and management. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus. 2018 Dec 1:31(12):. doi: 10.1093/dote/doy094. Epub [PubMed PMID: 30295751]
Liacouras CA, Furuta GT, Hirano I, Atkins D, Attwood SE, Bonis PA, Burks AW, Chehade M, Collins MH, Dellon ES, Dohil R, Falk GW, Gonsalves N, Gupta SK, Katzka DA, Lucendo AJ, Markowitz JE, Noel RJ, Odze RD, Putnam PE, Richter JE, Romero Y, Ruchelli E, Sampson HA, Schoepfer A, Shaheen NJ, Sicherer SH, Spechler S, Spergel JM, Straumann A, Wershil BK, Rothenberg ME, Aceves SS. Eosinophilic esophagitis: updated consensus recommendations for children and adults. The Journal of allergy and clinical immunology. 2011 Jul:128(1):3-20.e6; quiz 21-2. doi: 10.1016/j.jaci.2011.02.040. Epub 2011 Apr 7 [PubMed PMID: 21477849]
Level 1 (high-level) evidenceKim HP, Dellon ES. An Evolving Approach to the Diagnosis of Eosinophilic Esophagitis. Gastroenterology & hepatology. 2018 Jun:14(6):358-366 [PubMed PMID: 30166949]
Wang F, Li G, Ning J, Chen L, Xu H, Kong X, Bu J, Zhao W, Li Z, Wang X, Li X, Ma J. Alcohol accumulation promotes esophagitis via pyroptosis activation. International journal of biological sciences. 2018:14(10):1245-1255. doi: 10.7150/ijbs.24347. Epub 2018 Jul 13 [PubMed PMID: 30123073]
Ansari SA, Iqbal MUN, Khan TA, Kazmi SU. Association of oral Helicobacter pylori with gastric complications. Life sciences. 2018 Jul 15:205():125-130. doi: 10.1016/j.lfs.2018.05.026. Epub 2018 May 12 [PubMed PMID: 29763614]
Nejat Pish-Kenari F, Qujeq D, Maghsoudi H. Some of the effective factors in the pathogenesis of gastro-oesophageal reflux disease. Journal of cellular and molecular medicine. 2018 Dec:22(12):6401-6404. doi: 10.1111/jcmm.13939. Epub 2018 Oct 15 [PubMed PMID: 30320456]
Goyal A. Eosinophilic esophagitis: short and long-term considerations. Current opinion in pediatrics. 2018 Oct:30(5):646-652. doi: 10.1097/MOP.0000000000000662. Epub [PubMed PMID: 30015687]
Level 3 (low-level) evidenceDavis BP. Pathophysiology of Eosinophilic Esophagitis. Clinical reviews in allergy & immunology. 2018 Aug:55(1):19-42. doi: 10.1007/s12016-017-8665-9. Epub [PubMed PMID: 29332138]
DeBoer EM, Kinder S, Duggar A, Prager JD, Soden J, Deterding RR, Ruiz AG, Jensen EL, Weinman J, Wine T, Fortunato JE, Friedlander JA. Evaluating the yield of gastrointestinal testing in pediatric patients in aerodigestive clinic. Pediatric pulmonology. 2018 Nov:53(11):1517-1524. doi: 10.1002/ppul.24170. Epub 2018 Oct 4 [PubMed PMID: 30288952]
Ishimura N, Sumi S, Okada M, Mikami H, Okimoto E, Nagano N, Araki A, Tamagawa Y, Mishiro T, Oshima N, Ishihara S, Maruyama R, Kinoshita Y. Is Asymptomatic Esophageal Eosinophilia the Same Disease Entity as Eosinophilic Esophagitis? Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2019 Jun:17(7):1405-1407. doi: 10.1016/j.cgh.2018.08.048. Epub 2018 Aug 23 [PubMed PMID: 30144524]
Huang KZ, Jensen ET, Chen HX, Landes LE, McConnell KA, Almond MA, Johnston DT, Durban R, Jobe L, Frost C, Donnelly S, Antonio B, Safta AM, Quiros JA, Markowitz JE, Dellon ES. Practice Pattern Variation in Pediatric Eosinophilic Esophagitis in the Carolinas EoE Collaborative: A Research Model in Community and Academic Practices. Southern medical journal. 2018 Jun:111(6):328-332. doi: 10.14423/SMJ.0000000000000817. Epub [PubMed PMID: 29863219]
James C, Assa'ad A. The Global Face of Eosinophilic Esophagitis: Advocacy and Research Groups. Clinical reviews in allergy & immunology. 2018 Aug:55(1):99-105. doi: 10.1007/s12016-018-8683-2. Epub [PubMed PMID: 29730731]
Ness-Jensen E, Hveem K, El-Serag H, Lagergren J. Lifestyle Intervention in Gastroesophageal Reflux Disease. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2016 Feb:14(2):175-82.e1-3. doi: 10.1016/j.cgh.2015.04.176. Epub 2015 May 6 [PubMed PMID: 25956834]
Jensen ET, Gupta SK. Early Life Factors and Eosinophilic Esophagitis: Building the Evidence. Journal of pediatric gastroenterology and nutrition. 2018 Nov:67(5):549-550. doi: 10.1097/MPG.0000000000002136. Epub [PubMed PMID: 30211841]
Pan J, Cen L, Chen W, Yu C, Li Y, Shen Z. Alcohol Consumption and the Risk of Gastroesophageal Reflux Disease: A Systematic Review and Meta-analysis. Alcohol and alcoholism (Oxford, Oxfordshire). 2019 Jan 1:54(1):62-69. doi: 10.1093/alcalc/agy063. Epub [PubMed PMID: 30184159]
Level 1 (high-level) evidence