Introduction
Ackermann first described basilar invagination (BI) in cretins. Schuller gave the first radioimaging diagnosis, which Chamberlain and other radiologists later refined.
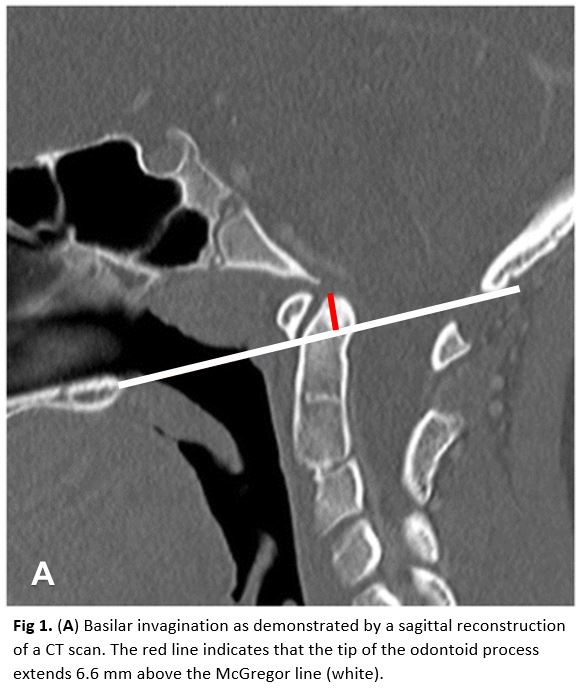
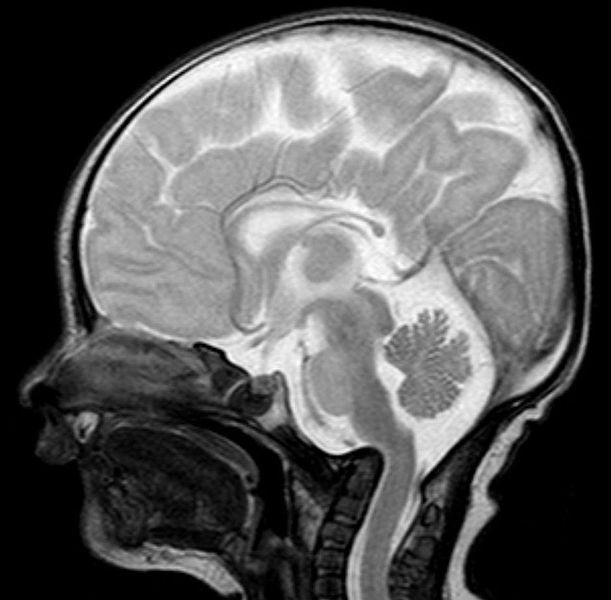
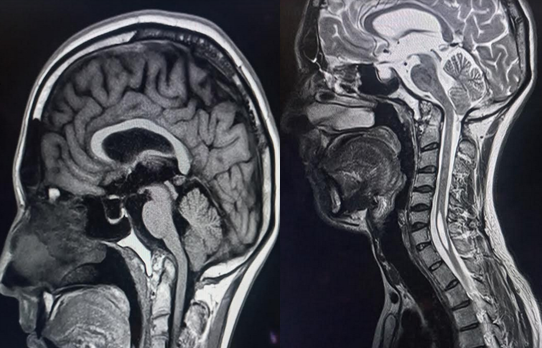
Basilar invagination is an abnormality at the craniovertebral junction, either congenital or degenerative, resulting in the odontoid prolapsing into the already limited space of the foramen magnum. It is commonly associated with conditions such as Chiari malformation, syringomyelia, and Klippel-Feil syndrome. Clinical presentations can range from chronic headaches, limited neck motion, and acute neurologic deterioration. CT and MRI are critical to diagnosing and managing this condition, including operative planning when needed.
Determining the need for operative intervention is controversial in asymptomatic patients, but those at risk of neurologic compromise could require preoperative cervical traction and algorithmic surgical strategies.[1][2][3][4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Compared to the skeletal development of other regions of the spine, the cervical spine has more pronounced changes from birth to skeletal maturity. While some defects may appear static, changes in the cervical spine are more likely to become symptomatic and even life-threatening.[5][6][7]
The most common adult craniocervical junction malformations include Chiari malformations and basilar invagination. Basilar invagination is a condition where the floor of the skull at the foramen magnum has developed in such a way that the superior aspect of the cervical spine is more cephalad (and often posterior) and, in effect, has created a narrowing at the foramen magnum opening. This area is at risk of odontoid prolapse along with the decrease in surface area that places the patient at an increased risk for neurologic injury or disruption of cerebrospinal fluid flow. This condition can result from C1-C2 facet instability, congenital osseous defect, or secondary to degenerative processes, as seen in 20% of patients with rheumatoid arthritis.
Epidemiology
BI is the most common form of craniovertebral junction malformation (CVJM).[8][9] A study examining craniovertebral junction (CVJ) anomalies in young adults observed BI to be the most common anomaly (52.3%), followed by atlanto-occipital assimilation (33.3%).[10]
One notable study looking at surgically treated BI patients indicated that a Chiari malformation might correlate to the age at presentation and symptoms. Those with a Chiari malformation usually presented later in the second (20%), third (44%), and fourth (24%) decades of life compared to those without the malformation, usually presenting earlier in the first (15%) and second (58%) decade of life. Furthermore, those with a Chiari malformation had slower progressing symptoms occurring over a longer time, most commonly weakness (94%), paresthesia (79%), posterior column, and spinothalamic tract disturbance (56%), and ataxia (47%). Those without the Chiari malformation mainly presented with weakness (100%), neck pain (59%), solely posterior column dysfunction (39%), bowel and bladder disturbance (28%), and paresthesia (25%). Furthermore, while none of the patients with the Chiari malformation had a history of trauma just before symptomatology, 48% of those without the malformation noted trauma precipitating the symptoms.
Pathophysiology
The most recent theory behind Group A BI is the atlantoaxial facet joint instability, thereby predisposing to upward migration of the odontoid peg through the foramen magnum resulting in brainstem compression.[11] BI is the result of the listhesis of C1-C2 facets.[12] “Craniovertebral realignment” through manipulation, distraction, reduction, and fixation of the atlantoaxial facet joint is, therefore, the principal mandate of surgery in these cohorts.
A developmental anomaly of the bone, as suggested by Virchow and Grawitz, is the pathogenesis for Group B BI. The congenital osseous dysgenesis leads to crowding of the posterior fossa and compression at the foramen magnum.[12]
Secondary natural protective mechanisms after that progress to minimize the stretching of the cord over the indenting odontoid peg by allowing a relatively stretch-free traversal.
History and Physical
There is a wide array of presentations for BI, with many of them directly resulting from the syndrome it may be associated with, such as a Chiari malformation, which is suboccipital at a rate of 33% to 38%. The degree of cephalad migration of the dens-atlas-clivus weightlifting determines the neurologic sequelae, as this creates significant crowding at the foramen magnum as well as at the medulla oblongata. Also, this crowding could obstruct cerebrospinal fluid (CSF) flow leading to syringomyelia. In the event of medullary dysfunction, a patient may exhibit ataxia, dysmetria, nystagmus, dysphagia, or cranial nerve palsies.
Interestingly there have been well-documented associations between exertional cough headaches (almost exclusively at the occipital or suboccipital, not migraine in a pattern) and BI. In a study of 97 patients evaluated for a cough, exertional, or sexual headaches, advanced imaging noted an intracranial defect in 45% of cases, and up to 80% of the secondary cough headaches were associated with Chiari I. The authors recommended that every patient with a cough headache have a craniocervical MRI. In addition to coughing, these headaches can be brought on by laughing, weight lifting, or head postural changes. Other sometimes more apparent findings, while not exclusive to basilar invagination, is a short neck (reported in 78% of cases) and asymmetric face/skull or torticollis (reported in 68% of cases).
One of the frequent causes of the secondary-type basilar impression is rheumatoid arthritis. The basilar impression resulting from rheumatoid arthritis was originally termed “cranial settling” when Mathews and others interpreted odontoid migration to result from cranial descent due to eroded lateral atlantal masses. Approximately 8% of rheumatoid patients demonstrate these changes. These changes may lead to sudden death as a result of instability and require surgical fixation.
The predominant signs and symptoms in patients with BI can be broadly categorized as follows:
- Pyramidal symptoms
- Altered Kinesthetic sensations
- Spinothalamic dysfunction[12]
Constellation of presenting signs and symptoms include:
- Weakness
- Numbness
- Paresthesia
- Neck pain
- Gait instability
- Spasticity
- Dysphagia
- Dysarthria[13]
Neck pain is the most common (approximately 80%) presenting symptom. Torticollis is observed in around 40% of them.[12] The presentation is comparatively acute in Group A, whereas slowly progressive in Group B patients.[12] Almost 60% of patients with Type A BI have a history of head injury prior to the onset of their symptoms.[12] Short neck and torticollis are common in Group A basilar invagination. They also have neurological symptoms due to direct compression of the brainstem by the odontoid process. Dysfunctioning medullary structures such as olivary nucleus and nucleus prepositus hypoglossi lead to transsynaptic degeneration, causing disproportionate atrophy of the cerebellar vermis with preserved tonsillar volume.[14] Group B patients have clinical features relating to Central cord syndrome and syringomyelia secondary to crowding of the posterior fossa.[12]
BI can be associated with other concurrent anomalies like:
- Atlantoaxial dislocation
- Chiari malformation
- Atlas occipitalization, and
- Klippel-Feil syndrome.
- Atlanto-occipital hypoplasia
- Clival hypoplasia
- Os odontoideum
- Platybasia[13][15]
Telescoping of the spinal segments, in the event of chronic atlantoaxial instability, try to confer natural protection, thereby leading to:
- Short neck
- Torticollis
- Dorsal kyphoscoliosis
- Klippel-Feil alteration
- C2–3 fusion
- Assimilation of atlas
- Bifid arches of atlas and axis
- Platybasia
- Chiari formation
- Syringomyelia
These natural protective sequelae are most often reversible following atlantoaxial stabilization in group A BI and foramen magnum decompression in group B BI.[16]
Evaluation
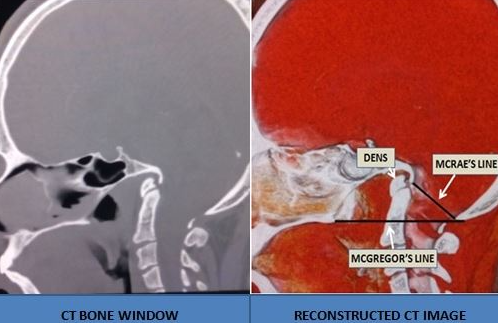
BI is most often diagnosed pertaining to the following midsagittal craniovertebral parameters:
- Chamberlain's line-running from the posterior aspect of the hard palate and the posterior margin of the foramen magnum
- McGregor's line-running from the posterior margin of the hard palate to the lowest aspect of the squama occipitalis (as the posterior edge of the foramen magnum could not always be visualized)
- McRae's line – connotes the anteroposterior line at the foramen magnum[15][17]
The criteria for diagnosis are the tip of the dens lying >5 mm above Chamberlain's Line, >7 mm above McGregor's Line, or McRae's line.
Based on Atlantodens interval (ADI):
- Type 1- when ADI > 3 mm in adults or ADI > 5 mm in children or
- Type 2- when ADI ≤ 3 mm in adults or ADI ≤ 5 mm in children.[18]
Recently, BI has been divided into:
- Group A BI- the tip of the odontoid process is above the Chamberlain line, McRae line, and Wackenheim's clival line.
- Group B BI- the odontoid process and clivus remained anatomically aligned, and the tip of the odontoid process is above Chamberlain's line but below McRae's and Wackenheim's lines.[12]
A few of the essential radiological parameters utilized during the management of patients with BI include:
- Clivus length and basal angle play a role in the pathophysiology of BI and CM.[19]
- The odontoid tip either intersects the minimum perpendicular distance from the odontoid tip to the palate-internal occipital protuberance (P-IOP) line or is < 9 mm below the P-IOP line (in Goel group A and B BI, respectively).[20]
- Clivus slope (CS) is the angle between the Wackenheim line and the horizontal line. A reduction in the CS affects the postoperative PRO-JOA score of BI patients.[15]
- The foramen magnum angle (FMA) between Chamberlain's line and McGregor's line, which characterizes the tilt of the FM, is almost 22 degrees in BI (versus six degrees in normal cohorts) due to clivus hypogenesis.[17]
- Clivus line violation (CLV) is the most widely used indicator in the diagnosis of BI, with a value of CLV ≥ 3 mm currently defining BI.[15]
- Basilar invagination usually shows a decrease in clivus axis angle (CAA), which could give rise to progressive neural compression.[21]
- The clivopalatal angle (CPA) is the angle between the Wackenheim line and the tangent line of the hard palate plane and can be applied intraoperatively for correcting sagittal alignment.[15] CPA showed higher interobserver agreement than clivoaxial angle (CXA).[22]
- The distance of the odontoid apex to Chamberlain's line (DOCL) and Boogaard's angle (BOA) ≥ 136 degrees has been observed to have the highest diagnostic accuracy for type B BI.[23]
- The minimum perpendicular distance from the odontoid tip to the palate-internal occipital protuberance (P-IOP) has the advantage of diagnosing both types of BI while comparing to Boogards's angle. This is not affected by the position of the head.[24]
- Postoperative Boogaard's angle (BoA) was the most important predictor of BI prognosis.[25]
- Cervicomedullary angle (CMA) in normal patients ranges from 139.0 to 175.5 degrees, with an average of 158.5 degrees. The CMA is considered an effective index to assess the grade of anterior spinal cord compression.[9]
- The clivus axial angle (CXA) was divided by the Chamberlain line into clivus tilt (CT) and axial tilt (AT). The difference between actual AT and its ideal value (about 94 degrees) is the optimal target of CXA correction to decompress neural elements ventrally and recover better subaxial cervical lordosis.[26] The clivus axis angle (CAA)< 150° cause medullary compression. This can also be used to evaluate decompression postoperatively.[27]
Dynamic CT imaging help assess CVJ instability.[10] Computed tomography (CT) scan also details patterns of bony abnormalities, pertinent osseous anatomy, facet angle, and degree of boy destruction. This also helps determine the need for C1–2 osteotomy.[28] The C2 pedicle in the BI is thinner than the control group.[29] The occipital bone in BI patients is thinner (11 +/- 2.84 mm in the BI group and 17.56 +/- 3.03 mm in the control group).[30] The upper cervical spine is also relatively stiffer in BI patients.[29][31]
Preoperative CT angiography (CTA) is highly recommended to identify any anomalous variations such as "kissing" carotids, high riding vertebral, and an anomalous right vertebral artery (VA) to minimize the risk of intraoperative injury.[32][33][34][35] The separating, fusing, opacifying, and false-coloring-volume rendering (SFOF-VR) technique has been used to identify the course of the VA.[36]
Multi-positional MRI is reliable imaging to evaluate the level of cord compression, T2 signal changes, Chiari malformation, and syringomyelia.[37][28]
Treatment / Management
Evolution of Surgical Strategies
In 1939, Chamberlain first described suboccipital craniectomy, cervical laminectomy, and dural opening to manage BI. However, significant morbidity and mortality were reported following the procedure, especially by Barucha Dastur and Sinh, including the risk of intramedullary hemorrhages.
Sekir advocated the use of traction. For the few patients without any neurological disturbances, clinical and radiological preoperative traction for the progression of the disease has been described as a reasonable alternative to operative stabilization.[38][39] The determination of the approach is usually a result of the reducibility of the BI. Given the importance of reducibility in the surgical approach, preoperative traction is a valuable tool in determining the degree of reducibility and assessment of neurological status. In a case series of surgically treated patients with BI performed by Goel et al., 82 patients without any associated Chiari malformation were placed in cervical traction, and 82% of these patients noted rapid clinical improvement after the application of traction. Traction can be a useful tool in evaluating the reducibility and predicting intraoperative neurological worsening by surgical position. Headframe reduction technique can be applied in patients with reducible atlantoaxial dislocation (AAD) and BI.[40] Irreducibility is defined as nonalignment of C1–2 during neck extension (determined on lateral x-ray) or after cervical traction.[28]Simple posterior fixation and fusion are adequate for reducible CVJ deformity.(B2)
In 1980, Menezes et al. divided craniocervical abnormalities into reducible and irreducible groups. Posterior fixation was recommended for reducible variants. Transoral decompression was followed by posterior occipitocervical fixation for stable ventral lesions, whereas dorsal decompression with or without stabilization was carried out for dorsal pathologies. Transoral surgery, first used by Kanavel, was popularized by Crockard et al.with the application of retractor systems and a microscope for managing the BI. BI is the most common indication for Occipitocervical fixation (OCF).[41] OCF, however, has implant and wound-related complications and significantly restricts head movements as well.[41](B2)
The surgical strategies have slowly evolved from only bone overlay to sublaminar wire fixation and, subsequently, screw plate/rod fixation. From midline fixation strategies, now the notion has shifted to facet fixation, as described by Goel and Laheri.
A reduction via anterior transoral or posterior C1–2 facet distraction is necessary for irreducible deformity.[28]Posterior intra-articular distraction followed by cage implantation and cantilever correction can achieve a complete reduction in most cases.[42] One-stage release, reduction, and fixation through a posterior approach are safe and efficient.[43] A single-stage posterior stand-alone approach is accepted as the first-line treatment.[9] Posterior atlantoaxial facet reduction, fixation, and fusion (AFRF) are also recommended for patients with failed suboccipital bony decompression.[36] If C1–2 facets are fixed, osteotomy may be required.[28] Anterior release reduction and posterior fixation for irreducible BI with AAD, especially in patients with severely deformed bony mass anteriorly compressing the cervicomedullary junction.[28](B2)
Ultimately, the approach should be made on a case-by-case basis after a thorough evaluation of clinical findings and radio-imagings. There has been a paradigm shift from anterior and combined anterior-posterior approaches to a stand-alone posterior surgical strategy whenever feasible.
The aims of surgical interventions include:
- Foramen magnum decompression,
- Restoring and stabilizing the alignment at the CVJ, and
- Restoring normal cerebrospinal fluid flow dynamics.[9][28]
Traditionally, basilar invagination can be treated with cervical traction and posterior stabilization. However, anterior decompression via a transoral or endonasal approach may be necessary in irreducible cases.[44] Transoral atlantoaxial reduction plate (TARP) fixation, the performance of reduction and decompression, and earlier bone fusion rates of TARP procedure are superior to those of OF.[45] Transoral odontoidectomy as a salvage surgery is safe and effective for inadequate decompression from posterior distraction and fixation.[9][46]
Recently Endoscopic endonasal approach (EAA) has been postulated.[13][47] Compared to the traditional transoral or transpalatal approaches, the EEA approach has the following benefits:
- Minimal stay in ventilator/earlier extubation
- Minimized need for tracheotomy
- EEA, negating prolonged tongue retraction and splitting of the soft or hard palates, reduces the risk of postoperative upper airway edema, velopalatal insufficiency, and dysphagia.
- Earlier postoperative oral feeds, and
- Reduced hospital stays.[13][48][49]
Following EEA for BI, almost 90% of patients have shown neurologic improvement.[13] Image-guided navigation and intraoperative CT can facilitate localization and complete resection of the odontoid process and decompression of the spinal cord.[9]
There is, however, a steep learning curve.[13] Moreover, intraoperative and postoperative CSF leaks have been reported up to 30% and 5%, respectively.[13] A multilayered closure or a mucoperichondrial vascularized flap is preferred to prevent CSF leaks.[13][48]
Limitations of EEA include:
- Limited surgical window
- A narrow surgical corridor hinders the manipulation of the surgical instruments
- Suturing, especially during primary closure following a cerebrospinal fluid leak, is very challenging[9]
A recent study has validated the role of atlanto-axial facet distraction with fusion posterior only for the group A variant, whereas only suboccipital and foramen magnum decompression without need for duroplasty in the group B variant, even in the presence of syringomyelia.[50]
Posterior C1-C2 distraction and fixation is a safe and effective technique for the treatment of basilar invagination.[21] Restoring the height of the atlantoaxial lateral mass by using an individualized cage and adjusting the posterior occipitocervical angle (ΔPOCA) using cantilever technology is possible.[27] An attempt at C2 nerve root preservation is preferred. [51]The accuracy of freehand pedicle screw placement, measured by the Gertzbein-Robbins scale in BI, has sometimes been reported to be below 25%.[32] Navigation is preferred for complex congenital CVJ malformation to improve the accuracy of instrumentation.[9][52](B2)
The inter-articular cage causes a “folding chair” effect to reduce the dislocation.[27] This cage can also be used as a fulcrum to adjust the occipitocervical angle through the cantilever technique.[27] Appropriate selection of the occipitocervical angle by adjusting the POCA by shaping the rod can be undertaken.[27] CVJ alignment measured by Clivus-canal angle and cervicomedullary angle can help plan the surgical strategy.[28] Head extension maneuver through the occipital screws and rod system for the craniocervical realignment.[28]
Posterior decompression alone, without duroplasty, in type 2 BI releases local compression, alleviates posterior crowding, and promotes ventricular flows.[14]
A geometric model of the atlantoaxial dislocation and basilar invagination reduction is also developed.[53]
Differential Diagnosis
"Platybasia" - an abnormal flattening of the base of the skull was coined by Virchow.
"Basilar impression," also referred to as atlantoaxial impaction or vertical cranial settling, results from softening of the bone at the skull base secondary to:
- Rheumatoid arthritis
- Paget's disease
- Osteomalacia
- Hyperparathyroidism
- Osteogenesis imperfecta
- Hurler syndrome
- Rickets, and
- Skull base infection.[28]
It is speculated that the basilar impression is due to recurrent microfractures from repetitive axial loads. Supporting this theory are intraoperative findings of proliferative callus at the base of the skull in patients with osteogenesis imperfect (OI). One study showed that about 25% of such patients had this defect. Even if treated secondary, basilar invagination potentially has devastating sequelae in osteogenesis imperfect patients and other osteochondrodysplasias such as Hajdu-Cheney syndrome.
Prognosis
While surgery can improve some neurological symptoms, complete recovery is not always possible. Residual neurological deficits are common and, in some cases, may be disabling.
Complications
Possible reasons for insufficient decompression include:
- Complex regional osseous anatomy
- Severe obliquity of C1-C2 facets
- Abnormal osseous fusion[9]
The presence of oilisthesis, extreme facet arthropathy, and the contraction of the tissues can hinder the realignment process.[54]
The main limiting variables in reducing AAD in BI are:
- Anterior atlantoaxial tension band and
- Lateral articular process deformity noose.[27]
Complications of the transoral approach:
- Damage to the eustachian tube and hypoglossal nerve.
- Bleeding
- Severe tongue swelling
- Palatal and pharyngeal dehiscence
- Retropharyngeal abscess
- Neurological worsening
- Aspiration
- CSF leak
- Meningitis
- Delayed pharyngeal bleeding, and
- Craniovertebral junction instability.
Complications of craniovertebral junction fusion surgery:
- Neurological worsening
- Vertebral artery injury
- Bleeding from vertebral venous plexus
- Craniovertebral junction instability
- Cord edema
- CSF leak
- Meningitis
- Nonunion
- Hardware failure, and
- Sudden death.
A few of the common complications of posterior fusion surgery can be:
- Mechanical failure includes nonunion, instrument failure, and adjacent segment degeneration. The C1–2 facet joint is the most critical area for assuring good fusion and undertaking kyphotic correction.
- Subaxial kyphotic deformity has been observed following laminoplasty and wider detachment of deep extensor muscle. Therefore, it is imperative to avoid occipital fixation to minimize such risk and to ensure the preservation of C0–1 motion.
- Occipital neuralgia can occur following C2 root resection but has not been observed to affect patient-reported outcomes and quality of life significantly.
- Neurological worsening is most commonly observed during vertical reduction. The risk increases among patients with T2 signal changes in MRI and reduced canal diameter. This can be prevented with the adjunct use of intraoperative neuromonitoring (IONM).
- Dysphagia – especially following the “military tuck” positioning that can lead to glossoptosis. This is also increased among patients with OC fixation in retraction posture.[28]
Pearls and Other Issues
Basilar invagination is infrequently found in isolation and poses significant treatment challenges. Before any treatments specific to the condition, practitioners should screen for other associated anomalies. Advancements in diagnostic techniques have facilitated the management of this condition. Patients with reducible invaginations potentially can avoid a combined anterior and posterior approach, requiring only posterior decompression and stabilization. The most appropriate surgical approach and fixation choices will likely remain controversial until high-level randomized trials can elucidate the most effective treatment course.
Enhancing Healthcare Team Outcomes
Basilar invagination is a rare neurological disorder that may be found in isolation and poses significant treatment challenges. Because of the complexity of management, it is best managed by an interprofessional team that includes a neurologist, neurosurgeon, ICU nurses, therapists, and a radiologist. Before any treatments specific to the invagination, practitioners should screen for other associated conditions and try to avoid compromising potential surgical treatment for the invagination. Advancements in diagnostic techniques have assisted with the management of this condition. Patients with reducible invaginations potentially can avoid a combined anterior and posterior approach, requiring only posterior decompression and stabilization. The most appropriate surgical approach and fixation choices will likely remain controversial until high-level randomized trials can elucidate the most effective treatment course.
Irrespective of the type of surgery, some rehabilitation is required in most patients. Besides the physical therapist, the speech and occupational therapist are necessary to regain the function of the muscles. The social worker should be involved to ensure that the patient's home environment is safe and support systems are available. A neurology nurse should follow the patient to ensure that the patient is not worsening. Open communication between interprofessional team members is vital to improving outcomes.
Media
(Click Image to Enlarge)
References
Kahilogullari G,Eroglu U,Yakar F,Beton S,Meco C,Caglar YS, Endoscopic Endonasal Approaches to Craniovertebral Junction Pathologies: A Single-Center Experience. Turkish neurosurgery. 2018 Aug 27; [PubMed PMID: 30649807]
Chibbaro S,Ganau M,Cebula H,Nannavecchia B,Todeschi J,Romano A,Debry C,Proust F,Olivi A,Gaillard S,Visocchi M, The Endonasal Endoscopic Approach to Pathologies of the Anterior Craniocervical Junction: Analytical Review of Cases Treated at Four European Neurosurgical Centres. Acta neurochirurgica. Supplement. 2019; [PubMed PMID: 30610322]
Level 3 (low-level) evidenceLiao C,Visocchi M,Zhang W,Li S,Yang M,Zhong W,Liu P, The Relationship Between Basilar Invagination and Chiari Malformation Type I: A Narrative Review. Acta neurochirurgica. Supplement. 2019; [PubMed PMID: 30610310]
Level 3 (low-level) evidenceDonnally CJ 3rd,Butler AJ,Rush AJ 3rd,Bondar KJ,Wang MY,Eismont FJ, The most influential publications in cervical myelopathy. Journal of spine surgery (Hong Kong). 2018 Dec; [PubMed PMID: 30714009]
Ferrante A,Ciccia F,Giammalva GR,Iacopino DG,Visocchi M,Macaluso F,Maugeri R, The Craniovertebral Junction in Rheumatoid Arthritis: State of the Art. Acta neurochirurgica. Supplement. 2019; [PubMed PMID: 30610306]
Goel A, Cervical Fusion as a Protective Response to Craniovertebral Junction Instability: A Novel Concept. Neurospine. 2018 Dec; [PubMed PMID: 30562886]
Rusbridge C,Stringer F,Knowler SP, Clinical Application of Diagnostic Imaging of Chiari-Like Malformation and Syringomyelia. Frontiers in veterinary science. 2018; [PubMed PMID: 30547039]
Botelho RV,Botelho PB,Hernandez B,Sales MB,Rotta JM, Association between Brachycephaly, Chiari Malformation, and Basilar Invagination. Journal of neurological surgery. Part A, Central European neurosurgery. 2021 Dec 20 [PubMed PMID: 34929749]
Wang X,Ma L,Liu Z,Chen Z,Wu H,Jian F, Reconsideration of the transoral odontoidectomy in complex craniovertebral junction patients with irreducible anterior compression. Chinese neurosurgical journal. 2020 [PubMed PMID: 32944290]
Ravikanth R,Majumdar P, Embryological considerations and evaluation of congenital anomalies of craniovertebral junction: A single-center experience. Tzu chi medical journal. 2021 Apr-Jun [PubMed PMID: 33912416]
Goel A, Basilar invagination, syringomyelia and Chiari formation and their relationship with atlantoaxial instability. Neurology India. 2018 Jul-Aug; [PubMed PMID: 30038072]
Goel A, Basilar invagination, Chiari malformation, syringomyelia: a review. Neurology India. 2009 May-Jun; [PubMed PMID: 19587461]
Halderman AA,Barnett SL, Endoscopic endonasal approach to the craniovertebral junction. World journal of otorhinolaryngology - head and neck surgery. 2022 Mar [PubMed PMID: 35619929]
Lee J,Guk HS,Kim M,Lee EJ, Successful Treatment of Basilar Invagination and Platybasia Associated With Cerebellar Atrophy by Decompression Surgery. Journal of clinical neurology (Seoul, Korea). 2022 Mar [PubMed PMID: 35274843]
Peng L,Zuo W,Cheng C,Yang F,Wang P,Mao Z,Zhang J,Li W, Association Between the Clivus Slope and Patient-Reported Japanese Orthopaedic Association (PRO-JOA) Scores in Patients with Basilar Invagination: A Retrospective Study. Turkish neurosurgery. 2021 Nov 26; [PubMed PMID: 35713252]
Level 2 (mid-level) evidenceGoel A, Basilar invagination, spinal "degeneration," and "lumbosacral" spondylolisthesis: Instability is the cause and stabilization is the treatment. Journal of craniovertebral junction & spine. 2021 Oct-Dec [PubMed PMID: 35068814]
Jian Q,Zhang B,Jian F,Bo X,Chen Z, Corrigendum to "Basilar Invagination: A Tilt of the Foramen Magnum" [World Neurosurgery 164 (2022) e629-e635]. World neurosurgery. 2022 Aug 30 [PubMed PMID: 36058831]
Jian Q,Zhang B,Jian F,Bo X,Chen Z, Basilar Invagination: A Tilt of the Foramen Magnum. World neurosurgery. 2022 Aug [PubMed PMID: 35577208]
Diniz JM,Botelho RV, The role of clivus length and cranial base flexion angle in basilar invagination and Chiari malformation pathophysiology. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2020 Jul; [PubMed PMID: 32002740]
Sardhara J,Behari S,Singh S,Srivastava AK,Chauhan G,Lal H,Das KK,Bhaisora KS,Mehrotra A,Mishra P,Jaiswal AK, A Universal Craniometric Index for Establishing the Diagnosis of Basilar Invagination. Neurospine. 2021 Mar [PubMed PMID: 33494552]
Feng SP,Wang HW,Qiao GY,Yu XG, Indirect Ventral Brainstem Decompression by Posterior C1-C2 Distraction and Fixation for Basilar Invagination. World neurosurgery. 2022 Jul [PubMed PMID: 35314410]
Level 2 (mid-level) evidenceMa L,Guo L,Li X,Qin J,He W,Xiao X,Lu L,Xu Y,Wu Y, Clivopalate angle: a new diagnostic method for basilar invagination at magnetic resonance imaging. European radiology. 2019 Jul [PubMed PMID: 30820721]
Level 2 (mid-level) evidenceNascimento JJC,Neto EJS,Mello-Junior CF,Valença MM,Araújo-Neto SA,Diniz PRB, Diagnostic accuracy of classical radiological measurements for basilar invagination of type B at MRI. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2019 Feb; [PubMed PMID: 30498960]
Sardhara J,Behari S, Reply to Commentary on "A Universal Craniometric Index for Establishing the Diagnosis of Basilar Invagination". Neurospine. 2021 Sep [PubMed PMID: 34610697]
Level 3 (low-level) evidencePeng L,Peng C,Yang F,Zuo W,Cheng C,Wang P,Zhang J,Li W, Comparative Analysis Between Machine Learning Algorithms and Conventional Regression in Predicting the Prognosis of Patients with Basilar Invagination: A Retrospective Cohort Study. Turkish neurosurgery. 2021 Nov 10; [PubMed PMID: 35416266]
Level 2 (mid-level) evidenceLiu Z,Zhao X,Guan J,Duan W,Goel A,Xia Z,Jian F,Chen Z, Quantitative Reduction of Basilar Invagination: Correction Target of Clivo-Axial Angle. Clinical spine surgery. 2020 Oct [PubMed PMID: 32187082]
Guan J,Jian F,Yao Q,Yuan C,Zhang C,Ma L,Liu Z,Duan W,Wang X,Bo X,Chen Z, Quantitative Reduction of Basilar Invagination With Atlantoaxial Dislocation by a Posterior Approach. Neurospine. 2020 Sep [PubMed PMID: 33022162]
Hong JT,Kim IS,Lee HJ,Park JH,Hur JW,Lee JB,Lee JJ,Lee SH, Evaluation and Surgical Planning for Craniovertebral Junction Deformity. Neurospine. 2020 Sep [PubMed PMID: 33022160]
Xiao R,Hou J,Zhou Y,Zheng J,Zou X,Zhu Y,Yao L,Ma X,Chen J,Yang J, Anatomical analysis of the C2 pedicle in patients with basilar invagination. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2022 Oct [PubMed PMID: 35604456]
Ji W,Lin S,Bao M,Zou X,Ge S,Ma X,Chen J,Yang J, Anatomical analysis of the occipital bone in patients with basilar invagination: a computed tomography-based study. The spine journal : official journal of the North American Spine Society. 2020 Jun [PubMed PMID: 31972304]
Lin JY,Bao MG,Lin SY,Liu JH,Liu Q,Li RY,Huang ZC,Zhu QA,Zhang ZM,Ji W, Cervical Alignment of Patients with Basilar Invagination: A Radiological Study. Orthopaedic surgery. 2022 Mar [PubMed PMID: 35156312]
Zhou LP,Zhang RJ,Zhang HQ,Jiang ZF,Shang J,Shen CL, Effect of High-Riding Vertebral Artery on the Accuracy and Safety of C2 Pedicle Screw Placement in Basilar Invagination and Related Risk Factors. Global spine journal. 2022 Jun 18 [PubMed PMID: 35719094]
Das KK,Pattankar S,Srivastava AK, Arterial Fencing: A Challenge During Complex Craniovertebral Junction Surgery. World neurosurgery. 2022 May [PubMed PMID: 35248774]
Su C,Chen Z,Wu H,Jian F, Computed tomographic angiography to analyze dangerous vertebral artery anomalies at the craniovertebral junction in patients with basilar invagination. Clinical neurology and neurosurgery. 2021 Jan [PubMed PMID: 33109467]
Zhou LP,Zhang RJ,Jiang ZF,Tao EX,Shang J,Shen CL, Ideal entry point and trajectory for C2 pedicle screw placement in basilar invagination patients with high-riding vertebral artery based on 3D computed tomography. The spine journal : official journal of the North American Spine Society. 2022 Aug [PubMed PMID: 35508287]
Du YQ,Qiao GY,Yin YH,Li T,Yu XG, Posterior atlantoaxial facet joint reduction, fixation and fusion as revision surgery for failed suboccipital decompression in patients with basilar invagination and atlantoaxial dislocation: Operative nuances, challenges and outcomes. Clinical neurology and neurosurgery. 2020 Jul [PubMed PMID: 32283470]
Level 2 (mid-level) evidenceChamnan R,Chantarasirirat K,Paholpak P,Wiley K,Buser Z,Wang JC, Occipitocervical measurements: correlation and consistency between multi-positional magnetic resonance imaging and dynamic radiographs. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2020 Nov; [PubMed PMID: 32318836]
Al Jishi A, Commentary: Comprehensive Drilling of C1-2 Facets in Congenital Atlanto-Axial Dislocation and Basilar Invagination: Critical Review. Operative neurosurgery (Hagerstown, Md.). 2019 Feb 1; [PubMed PMID: 30059986]
Level 3 (low-level) evidenceJoaquim AF,Tedeschi H,Chandra PS, Controversies in the surgical management of congenital craniocervical junction disorders - A critical review. Neurology India. 2018 Jul-Aug; [PubMed PMID: 30038084]
Li T,Du YQ,Yin YH,Xing SL,Qiao GY, Treatment of Reducible Atlantoaxial Dislocation and Basilar Invagination Using the Head Frame Reduction Technique and Atlantoaxial Arthrodesis. Global spine journal. 2022 Jun [PubMed PMID: 33138641]
Level 2 (mid-level) evidenceZileli M, Akıntürk N. Complications of occipitocervical fixation: retrospective review of 128 patients with 5-year mean follow-up. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2022 Feb:31(2):311-326. doi: 10.1007/s00586-021-07037-2. Epub 2021 Nov 2 [PubMed PMID: 34725722]
Level 2 (mid-level) evidenceChen Z,Duan W,Chou D,Guan J,Liu Z,Jian Q,Zhang B,Bo X,Jian F, A Safe and Effective Posterior Intra-Articular Distraction Technique to Treat Congenital Atlantoaxial Dislocation Associated With Basilar Invagination: Case Series and Technical Nuances. Operative neurosurgery (Hagerstown, Md.). 2021 Mar 15; [PubMed PMID: 33372978]
Level 2 (mid-level) evidenceWang J,Xu T,Pu L,Mai E,Guo H,Sheng J,Deng Q,Liao Y,Sheng W, Release, reduction, and fixation of one-stage posterior approach for basilar invagination with irreducible atlantoaxial dislocation. British journal of neurosurgery. 2020 Dec 21 [PubMed PMID: 33345635]
Liu JK,Dodson VN,Zhao K,Eloy JA, Endoscopic Endonasal Transclival Odontoidectomy for Basilar Invagination: Operative Video and Technical Nuances. Journal of neurological surgery. Part B, Skull base. 2021 Feb; [PubMed PMID: 33717805]
Zou X,Ouyang B,Yang H,Wang B,Ge S,Chen Y,Ni L,Zhang S,Xia H,Yang J,Ma X, Surgical treatment for basilar invagination with irreducible atlantoaxial dislocation: transoral atlantoaxial reduction plate fixation vs occipitocervical fixation. BMC musculoskeletal disorders. 2020 Dec 8 [PubMed PMID: 33292209]
Duan W,Chou D,Jian F,Chen Z, Navigated transoral odontoidectomy to treat congenital basilar invagination after failed posterior reduction and fusion. Neurosurgical focus: Video. 2020 Jul [PubMed PMID: 36285122]
Ruiz-Garcia H,Gassie K,Marenco-Hillembrand L,Donaldson AM,Chaichana KL, Endoscopic endonasal odontoidectomy for the treatment of basilar invagination. Neurosurgical focus: Video. 2020 Jul; [PubMed PMID: 36285120]
Simal-Julián JA,Miranda-Lloret P,Sanchis-Martín MR,Quiroz A,Botella-Asunción C,Kassam AB, Endonasal Odontoidectomy in Basilar Invagination. Journal of neurological surgery. Part B, Skull base. 2021 Feb [PubMed PMID: 33717804]
Bassiouni H, Basilar Invagination: Transoral Microsurgical Endoscopically-Controlled Odontoidectomy without Palatotomy in Extreme form of Basilar Invagination. Journal of neurological surgery. Part B, Skull base. 2021 Feb [PubMed PMID: 33717799]
Joaquim AF,Ghizoni E,Giacomini LA,Tedeschi H,Patel AA, Basilar invagination: Surgical results. Journal of craniovertebral junction [PubMed PMID: 25210337]
Puneeth S,Karthigeyan M,Salunke P,Panchal C,Kataria MS, C2 Nerve Root Preservation During Posterior Fixation for Instability Secondary to Congenital Craniovertebral Junction Anomalies: Feasibility Factors and Related Outcomes. World neurosurgery. 2022 Jan [PubMed PMID: 34610446]
Level 2 (mid-level) evidenceVilleneuve LM,Voronovich Z,Evans A,El Rassi ET,Dunn IF,Smith ZA, A combined approach for stabilization and endoscopic/ endonasal odontoid and clivus resection for treatment of basilar invagination. Surgical neurology international. 2021; [PubMed PMID: 34754561]
Hu XJ,Wang SX,Li Y,Xia YZ,Liao ZB,Yan Y, [Geometric model of reduction in basilar invagination with atlantoaxial dislocation and its clinical application]. Zhonghua wai ke za zhi [Chinese journal of surgery]. 2021 Mar 1 [PubMed PMID: 33685056]
Duan W,Chou D,Jian F,Chen Z, Posterior intra-articular distraction with cage placement to treat congenital atlantoaxial dislocation associated with basilar invagination. Neurosurgical focus: Video. 2020 Jul [PubMed PMID: 36285121]