Introduction
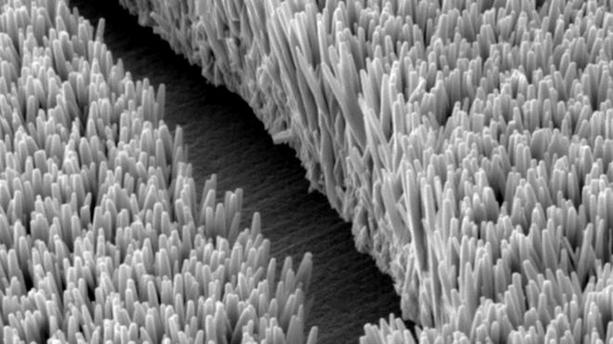
Enteroglucagon is a molecule discovered in the human intestine. The historical belief was that it was an extra-pancreatic isoform of glucagon. Glucagon-like substances in the intestine were first described by Sutherland and De Duve, who identified them in preparations from the intestinal mucosa.[1] These substances became known as peptides with glucagon-like immunoreactivity (GLI) due to patterns of immunoreactivity shared with glucagon.[2] Subsequent sequencing studies revealed that enteroglucagons consisted of several different molecules derived within the L-cells (enteroendocrine cells) of the intestine by post-translational modification of the preproglucagon polypeptide (see Image. Intestinal Epithelium With L Cells Present).[3] L-cells or enteroendocrine cells have been localized most specifically to the ileum and the colon, although they occur sporadically in other parts of the intestine.[4]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
The preproglucagon polypeptides play key roles in intestinal and systemic metabolism:
- Glicentin
- Glucagon-like peptide 1 (GLP-1)
- Glucagon-like peptide 2 (GLP-2)
- Oxyntomodulin
Cellular Level
The preproglucagon gene is the precursor to glucagon and is shared between the A-cells of the pancreatic islets of Langerhans and the L-cells of the intestine. Within the L-cells, the processing of preproglucagon polypeptide forms glicentin, glucagon-like peptides 1 and 2 (GLP-1 and GLP-2), and glicentin is then further cleaved to produce oxyntomodulin, with a leftover fragment called glicentin-related polypeptide (GRPP).[5] GLP-1 undergoes further processing, with the removal of amino acids from the N-terminus, to form the molecule GLP-1 (7-36), which significantly promotes insulin release from the pancreatic islets. This insulinotropic effect is active even at lower blood glucose levels. It is much more potent than the glucose-dependent insulinotropic peptide (GIP, previously known as a gastric-inhibitory peptide). Exenatide, a synthetic GLP-1 receptor agonist, was developed after the discovery of Exendin-4, a molecule of the glucagon superfamily of hormones, in the saliva of the Gila monster, which showed potent pancreatic insulinotropic effects in studies on animals, thus motivating the development of a new class of anti-diabetic medication.[6] The gene that codes for glicentin is on chromosome 2 (6 exons, 5 introns) and is found in the alpha cells of the pancreas and the intestinal or intestinal L cells.
Development
In a 1991 study, researchers highlighted the presence of enteroglucagon/glicentin in a 10-week-old human fetus in pancreatic cells.
Organ Systems Involved
Organ systems involved with enteroglucagon include:
- Glicentin (69 amino acids) is present in alpha cells of the pancreas, intestinal L cells (duodenum, rectum, distal ileum, proximal colon, caecum, proximal jejunum). Researchers have also found the glicentin gene in the central nervous system.
- GLP-1 (30 amino acids) is also in the alpha cells of the pancreas, L cells of the intestine (proximal small intestine, colon, and distal ileum), and in the central nervous system (nucleus tractus solitaries of the brain stem).
- GLP-2 (33 amino acids) is in the L cells of the intestine (colon and distal small intestine).
- Oxyntomodulin (37 amino acids) is likewise present in the L cells of the intestine.
Function
GLP-1 belongs to a class of molecules known as “incretins,” molecules that stimulate a decrease in blood glucose levels. The release of these molecules depends on the oral intake of glucose and other nutrients. This contributes to the “incretin effect,” a phenomenon by which oral glucose ingestion induces a greater increase in insulin release than an intravenous glucose load.[7] GLP-1 also participates in the “ileal-brake” effect, a mechanism by which the small intestine, in the presence of unabsorbed nutrients, exerts negative feedback on gastric emptying and gut motility to allow better digestion and absorption of these nutrients.[8] GLP-2 is involved in proliferative effects on small intestine mucosa.[9] These include hypertrophy of the epithelium and villi accompanied by increased mucosal blood flow at the cellular level, with evidence of hypertrophy also evident in gross anatomy in the form of increased mucosal folds and an increase in the caliber of the bowel. Glicentin shows some glucagon-like activity, while the roles of oxyntomodulin and GRPP in humans are currently unclear.[10][11] However, studies are ongoing to determine their effects on diabetes and obesity. According to some authors, oxyntomodulin reduces the sense of appetite, increases metabolism, and helps maintain systemic glucose homeostasis.
Mechanism
GLP-1 acts on the GLP-1 receptor (GLP-1R), which belongs to the class of G-protein coupled receptors (GPCRs).[12] The GLP-1R has a Gs subunit responsible for activating the intracellular enzyme adenylyl cyclase, which is the catalyst for converting ATP to cAMP. This molecule is the second messenger for GLP-1 and GLP-2 and mediates further downstream effects of these peptides. After release, GLP-1 is degraded by the enzyme dipeptidyl peptidase-4 (DPP-4) to GLP-1 (9–36) amide.[13] DPP-4 is widely expressed by endothelial cells on their surface, especially those neighboring GLP-1 secretion sites, and degrades other bioactive peptides such as GIP. DPP-4 is also present in high levels of hepatocytes, and the liver degrades much of the remaining GLP-1. Thus, very little GLP-1 leaves the intestine intact, and even less makes it to the systemic circulation.[12] Neutral endopeptidase 24.11 (NEP 24.11) is another enzyme that catabolizes GLP-1. It is a zinc metallopeptidase expressed in several locations, particularly in the kidneys. However, its contribution to GLP-1 degradation only becomes clear following inhibition of DPP-4, as otherwise, most of the GLP-1 reaching the kidneys is already degraded by DPP-4.[14] Proteolysis by DPP-4 limits the half-life of endogenous GLP-1 to 1-5 minutes. Analogs of GLP-1 in clinical use are thus chemically modified to be resistant to the effects of this enzyme and, therefore, have much longer half-lives than endogenous GLP-1 (eg, liraglutide, exenatide). Another mechanism of prolonging the actions of GLP-1, apart from degradation-resistant synthetic analogs, is the inhibition of their degradation by the action of the class of drugs called DPP-4 inhibitors (eg, sitagliptin, saxagliptin, vildagliptin).
Related Testing
The role of preproglucagon is still under study, and it has probable different clinical applications, but currently, no routine test is performed in the clinical setting.
Pathophysiology
Enteroglucagon was once implicated in the pathogenesis of diabetes after pancreatectomy. These have also been described in a rare functional pancreatic neuroendocrine tumor, which may be located in the pancreas itself or in the small intestine, where they correlate with slight intestinal hypertrophy. A case report exists describing the trophic effects of enteroglucagon (now known to be due to GLP-2) in a patient with an endocrine tumor in the kidney.[15]
Clinical Significance
GLP-1 analogs are now used in the management of diabetes.[16] These agents can potentiate endogenous insulin release in response to oral glucose loads with only a minor risk of hypoglycemia compared to sulfonylureas. Examples include long-acting GLP-1 agonists such as liraglutide, which are resistant to degradation by the enzyme dipeptidyl-peptidase-4 (DPP-4), and short-acting agonists like lixisenatide. Exenatide, another GLP-1 agonist, is available as both an immediate-release and an extended-release formulation. DPP-4 inhibitors inhibit the degradation of endogenous GLP-1 by DPP-4 and thus increase the half-life of the endogenous product. Examples include sitagliptin, saxagliptin, and linagliptin, among others. The efficacy of linagliptin may be adversely affected by CYP3A4 or P-glycoprotein inducers such as rifampin or St. John’s wort, thus requiring the use of alternative agents that are not pharmacodynamically affected by changes in CYP-450 drug metabolism.[17] GLP-2 analogs are currently emerging as a treatment for short-bowel syndrome due to their trophic effects on the small intestine.[18] Currently, teduglutide, a novel GLP-2 analog, is being tested for use in this condition, seen in patients who have undergone extensive small bowel resection and subsequently lack sufficient small bowel absorptive area to keep up with the production of digestive juices and intake of foods and fluids.[19]
Media
(Click Image to Enlarge)
References
SUTHERLAND EW, DE DUVE C. Origin and distribution of the hyperglycemic-glycogenolytic factor of the pancreas. The Journal of biological chemistry. 1948 Sep:175(2):663-74 [PubMed PMID: 18880761]
Unger RH, Ketterer H, Eisentraut AM. Distribution of immunoassayable glucagon in gastrointestinal tissues. Metabolism: clinical and experimental. 1966 Oct:15(10):865-7 [PubMed PMID: 5923522]
Level 3 (low-level) evidenceLund PK, Goodman RH, Dee PC, Habener JF. Pancreatic preproglucagon cDNA contains two glucagon-related coding sequences arranged in tandem. Proceedings of the National Academy of Sciences of the United States of America. 1982 Jan:79(2):345-9 [PubMed PMID: 7043459]
Level 3 (low-level) evidenceGunawardene AR,Corfe BM,Staton CA, Classification and functions of enteroendocrine cells of the lower gastrointestinal tract. International journal of experimental pathology. 2011 Aug; [PubMed PMID: 21518048]
Holst JJ. Enteroglucagon. Annual review of physiology. 1997:59():257-71 [PubMed PMID: 9074764]
Level 3 (low-level) evidenceEng J, Kleinman WA, Singh L, Singh G, Raufman JP. Isolation and characterization of exendin-4, an exendin-3 analogue, from Heloderma suspectum venom. Further evidence for an exendin receptor on dispersed acini from guinea pig pancreas. The Journal of biological chemistry. 1992 Apr 15:267(11):7402-5 [PubMed PMID: 1313797]
Level 3 (low-level) evidenceTian L, Jin T. The incretin hormone GLP-1 and mechanisms underlying its secretion. Journal of diabetes. 2016 Nov:8(6):753-765. doi: 10.1111/1753-0407.12439. Epub 2016 Aug 31 [PubMed PMID: 27287542]
Nauck MA,Meier JJ, Incretin hormones: Their role in health and disease. Diabetes, obesity [PubMed PMID: 29364588]
Drucker DJ. Mechanisms of Action and Therapeutic Application of Glucagon-like Peptide-1. Cell metabolism. 2018 Apr 3:27(4):740-756. doi: 10.1016/j.cmet.2018.03.001. Epub [PubMed PMID: 29617641]
Pocai A. Unraveling oxyntomodulin, GLP1's enigmatic brother. The Journal of endocrinology. 2012 Dec:215(3):335-46. doi: 10.1530/JOE-12-0368. Epub 2012 Sep 27 [PubMed PMID: 23019069]
Level 3 (low-level) evidenceHolst JJ, Albrechtsen NJW, Gabe MBN, Rosenkilde MM. Oxyntomodulin: Actions and role in diabetes. Peptides. 2018 Feb:100():48-53. doi: 10.1016/j.peptides.2017.09.018. Epub [PubMed PMID: 29412831]
Lee S, Lee DY. Glucagon-like peptide-1 and glucagon-like peptide-1 receptor agonists in the treatment of type 2 diabetes. Annals of pediatric endocrinology & metabolism. 2017 Mar:22(1):15-26. doi: 10.6065/apem.2017.22.1.15. Epub 2017 Mar 31 [PubMed PMID: 28443255]
Mentlein R, Gallwitz B, Schmidt WE. Dipeptidyl-peptidase IV hydrolyses gastric inhibitory polypeptide, glucagon-like peptide-1(7-36)amide, peptide histidine methionine and is responsible for their degradation in human serum. European journal of biochemistry. 1993 Jun 15:214(3):829-35 [PubMed PMID: 8100523]
Plamboeck A, Holst JJ, Carr RD, Deacon CF. Neutral endopeptidase 24.11 and dipeptidyl peptidase IV are both mediators of the degradation of glucagon-like peptide 1 in the anaesthetised pig. Diabetologia. 2005 Sep:48(9):1882-90 [PubMed PMID: 16025254]
Level 3 (low-level) evidenceGleeson MH, Bloom SR, Polak JM, Henry K, Dowling RH. Endocrine tumour in kidney affecting small bowel structure, motility, and absorptive function. Gut. 1971 Oct:12(10):773-82 [PubMed PMID: 4941684]
Sharma D, Verma S, Vaidya S, Kalia K, Tiwari V. Recent updates on GLP-1 agonists: Current advancements & challenges. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. 2018 Dec:108():952-962. doi: 10.1016/j.biopha.2018.08.088. Epub 2018 Sep 27 [PubMed PMID: 30372907]
Graefe-Mody U, Retlich S, Friedrich C. Clinical pharmacokinetics and pharmacodynamics of linagliptin. Clinical pharmacokinetics. 2012 Jul 1:51(7):411-27. doi: 10.2165/11630900-000000000-00000. Epub [PubMed PMID: 22568694]
Level 3 (low-level) evidenceJeppesen PB. Teduglutide, a novel glucagon-like peptide 2 analog, in the treatment of patients with short bowel syndrome. Therapeutic advances in gastroenterology. 2012 May:5(3):159-71. doi: 10.1177/1756283X11436318. Epub [PubMed PMID: 22570676]
Level 3 (low-level) evidenceWallis K, Walters JR, Gabe S. Short bowel syndrome: the role of GLP-2 on improving outcome. Current opinion in clinical nutrition and metabolic care. 2009 Sep:12(5):526-32. doi: 10.1097/MCO.0b013e32832d23cd. Epub [PubMed PMID: 19474717]
Level 3 (low-level) evidence