Introduction
The term "anophthalmic socket" refers to an orbit lacking an eyeball but with orbital soft tissues and eyelid structures. Anophthalmia can arise from congenital diseases, evisceration, or enucleation. Patients with an anophthalmic socket suffer from extreme deformity and mental and social suffering. The most prevalent cause of an anophthalmic socket is globe enucleation or evisceration.[1][2][3] True or primary anophthalmos is extremely uncommon and can only be diagnosed when the ocular tissue within the orbit is completely absent. Extreme microphthalmos occur more often, where a very small globe is present inside the orbital soft tissue and is not evident on initial examination (see Image. Post-Enucleation Anophthalmia).
The anophthalmic socket, a condition resulting from the surgical removal of an eye, poses significant challenges both aesthetically and functionally for patients. Enucleation or evisceration surgeries, which create an anophthalmic socket, are performed for various reasons, including trauma, severe infection, malignancy, and intractable pain in a blind eye. Managing an anophthalmic socket involves an interprofessional approach aimed at restoring the patient's appearance, enhancing functionality, and ensuring psychological well-being.[4]
The practice of enucleation dates back centuries, with its initial use primarily driven by the need to treat painful, blind eyes and severe ocular infections. However, surgical techniques and postoperative management strategies have evolved significantly. The primary focus in the early days was removing the diseased eye with little regard for the aesthetic outcome. However, advances in medical science and an increased understanding of the psychosocial impact of eye loss have shifted the focus toward more holistic management approaches.[5]
The introduction of orbital implants in the late 19th and early 20th centuries marked a significant milestone in managing the anophthalmic socket. These implants aimed to provide volume replacement and support for the prosthetic eye, improving both aesthetic and functional outcomes. Materials and designs for orbital implants have continually improved, with modern implants offering better biocompatibility and integration and reducing complication rates.
The orbit, a complex anatomical structure, houses the eye and its associated structures, including its muscles, nerves, and blood vessels. Eye removal disrupts this delicate balance, often leading to significant orbital anatomy changes. Over time, these changes result in socket contraction, inadequate prosthesis motility, and difficulty fitting an ocular prosthesis. Understanding these anatomical and physiological changes is crucial for developing effective management strategies.
The primary post-enucleation goals include maintaining orbital volume, ensuring good prosthetic motility, and achieving a cosmetically acceptable appearance. Placing an orbital implant helps maintain the socket's shape and supports the prosthetic eye. Various materials, including hydroxyapatite, porous polyethylene, and bioceramics, have been used for orbital implants, each with its own set of advantages and limitations. Managing an anophthalmic socket involves a combination of surgical interventions, prosthetic fittings, and long-term follow-up care. Immediate postoperative care minimizes inflammation, prevents infection, and ensures proper healing (see Image. Post-Evisceration Anophthalmia with Orbital Implant).
The choice of orbital implant and surgical technique is pivotal in long-term patient outcomes. Secondary procedures, such as socket reconstruction and dermis-fat grafts, are often necessary to address complications like socket contracture or implant exposure. Advances in surgical techniques, including the use of dermis-fat grafts and conjunctiva-sparing techniques, have improved the success rates of these secondary interventions. Additionally, using tissue expanders and custom-made implants has enhanced the ability to tailor the management to individual patient needs.[6]
Losing an eye can have profound psychological and social impacts on patients. Depression, anxiety, and social withdrawal are common among individuals with anophthalmic sockets. Therefore, addressing the psychological aspects of eye loss is an integral part of the management plan. Counseling and support groups can help patients cope with their condition and improve their quality of life.
Research and innovation continue to drive improvements in the management of anophthalmic sockets. Advances in biomaterials, 3-dimensional printing technology, and tissue engineering hold promise for developing more effective and personalized treatment options. Integrating these technologies into clinical practice can revolutionize the field, offering better patient outcomes.[7]
Furthermore, an interprofessional approach involving ophthalmologists, maxillofacial surgeons, prosthetists, and psychologists is essential for comprehensive care. Collaborative efforts and continued research are crucial to addressing the complex needs of patients with anophthalmic sockets and enhancing their overall well-being. Managing an anophthalmic socket requires a thorough understanding of the anatomical, physiological, and psychological aspects of eye loss. Advances in surgical techniques, prosthetic technology, and supportive care have significantly improved patient outcomes. Ongoing research and an interprofessional approach are essential for enhancing the quality of life for individuals with this condition.[8]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Anophthalmia and microphthalmia result when eye development is halted at different stages of optic vesicle formation. Anophthalmia occurs due to the failure of ocular structural development, which may stem from issues in neural tube induction, the formation of the optic vesicle or cup, or the subsequent degeneration of already formed optic tissues.[9]
Identifying microphthalmia is crucial, as the development of the orbital area, eyelids, and fornices relies on a normal-sized eye in utero. In children, anophthalmia can lead to significant complications, including the loss of vision and secondary deformities of the orbit, lids, and eye sockets. Causes of anophthalmia include idiopathic or sporadic changes, inherited patterns (dominant, recessive, or sex-linked), and specific chromosomal deletions, such as a deletion in band 14q22-23 associated with polydactyly, and a deletion in 7p15.1-21.1 linked to cryptophthalmos and anophthalmos.[10][11][12]
An anophthalmic socket may develop from various conditions and events that necessitate the surgical removal of the eye, leading to significant changes in orbital anatomy and function. The primary causes are broadly categorized into trauma, infections, neoplasms, and other ocular conditions.
Trauma
Trauma can result from mechanical injury or chemical burns. Severe ocular trauma, often caused by accidents, sports injuries, or occupational hazards, is a leading cause of enucleation, particularly in younger and middle-aged populations. Blunt or penetrating injuries can cause irreparable eye damage, necessitating removal to prevent further complications. Exposure to harmful chemicals can also cause extensive damage to the eye and surrounding structures, sometimes requiring enucleation to manage the injury and prevent systemic toxicity. Please see StatPearls' companion resource, "Blunt Eye Trauma," for more information.
Infections
Uncontrolled, severe ocular infections, such as endophthalmitis or panophthalmitis, can lead to significant inflammation and destruction of ocular tissues. Enucleation is performed when medical therapy fails to control the infection and preserve the overall health of the remaining orbital structures.
Severe keratitis, particularly when caused by resistant bacterial or fungal pathogens, can progress despite aggressive treatment, warranting eye removal. Infections, such as cytomegalovirus, rubella, parvovirus B19, and toxoplasmosis, deficiencies of nutrients such as vitamin A, and in utero exposure to toxins such as alcohol, thalidomide, and warfarin are also possible contributory environmental variables. Please see StatPearls' companion resource, "Bacterial Endophthalmitis," for more information.
Neoplasms
Malignant intraocular tumors, such as retinoblastoma in children and uveal melanoma in adults, are common indications for enucleation. Early detection and removal of the eye are vital to prevent metastasis and improve survival rates. Tumors originating in or spreading to the orbit, including lymphomas and metastatic lesions, often require enucleation to control the disease and alleviate symptoms.[13]
Other Ocular Conditions
Intractable glaucoma causing severe pain and blindness may necessitate enucleation when other treatments fail to control intraocular pressure and alleviate pain. Severe congenital malformations that impair vision and create cosmetic concerns may also require enucleation, especially when associated with other ocular or systemic anomalies.[14]
Phthisis bulbi is a shrunken, nonfunctional eye, often resulting from severe chronic diseases, trauma, or surgery. Enucleation is performed in such cases to improve cosmetic appearance and alleviate discomfort.
Iatrogenic Causes
Surgical complications resulting from intraocular procedures, such as retinal detachment repair and cataract surgery, can sometimes lead to severe outcomes requiring enucleation to manage pain or infection.[15]
Epidemiology
True anophthalmia is a relatively uncommon congenital condition, with reported incidences of 0.18 per 10,000 births in Italy and 0.33 per 10,000 births in California.[16][17] According to a source, depending on the underlying cause of the deformity, 53% to 71% of cases are bilateral, whether isolated, syndromic, or chromosomal.[18] Clinical anophthalmic socket syndrome affects 53% of patients with acquired anophthalmia, often presenting with newly identified issues such as impaired levator muscle function and lagophthalmia. Despite these conditions, patients' quality of life remains unaffected. The overall high quality of life associated with wearing an ocular prosthesis aligns with earlier research, which reported a satisfaction rate of 78% among prosthesis users.[19]
Pathophysiology
Embryonic eye formation results from an orderly series of processes involving the development of ocular tissues from the neuroectoderm, neural crest, mesoderm, and surface ectoderm.[20] The closure of the neural tube's rostral neuropore during the 4th week of development typically marks the beginning of optic tissue development.
The forebrain's neuroectoderm generates the optic vesicles, which prompt the surface ectoderm to differentiate into lens tissue in response to the optic vesicles, which then invaginate to form optic cups. As the optic cups expand around the growing lens, they develop into the retina, iris, and ciliary body of the adult eye. The optic nerve arises from the optic stalk, which connects the optic cup to the forebrain. Surrounding mesenchyme is stimulated to form the sclera, cornea, and choroid structures.[21]
Anophthalmia and other ocular abnormalities arise from disruptions during these developmental stages. True anophthalmia, characterized by the complete absence of eye tissues, can be classified into primary, secondary, or sequential types based on the timing of developmental failure or degeneration. Primary anophthalmia occurs when the optic vesicles fail to separate from the cerebral vesicle. Secondary anophthalmia, a rare and often fatal condition, results from severe anterior neural tube abnormalities. Sequential anophthalmia arises from secondary degeneration of the optic vesicles.
In acquired anophthalmia resulting from enucleation or evisceration, the anophthalmic socket undergoes a series of anatomical and physiological changes post-eye removal. Understanding the pathophysiology of the anophthalmic socket involves examining changes in orbital tissue and ocular adnexa function, as well as the body's compensatory mechanisms.
Tissue Changes
- Orbital fat atrophy: The surrounding orbital fat often undergoes atrophy following eye removal. This volume loss can lead to a sunken appearance of the socket, known as enophthalmos.
- Scarring and fibrosis: Surgical eye removal triggers a wound-healing response, resulting in orbital tissue scarring and fibrosis. These changes can restrict the movement of the remaining structures within the socket.
- Muscle dysfunction: The extraocular muscles responsible for eye movement may lose function or become misaligned post-eye removal. These changes may impair the movement of the ocular prosthesis and result in a less natural appearance.[22]
Ocular Adnexal Changes
- Eyelid malposition: Eye removal can disrupt normal eyelid function, resulting in conditions such as ptosis (drooping of the upper eyelid) or ectropion (outward turning of the eyelid). These changes can reduce socket protection and lubrication.
- Lagophthalmos: In some cases, patients may develop lagophthalmos, an inability to close the eyelids completely, due to scarring, muscle dysfunction, or improper fitting of the ocular prosthesis.
- Conjunctival changes: The conjunctiva, which lines the eyelids and covers the white part of the eye, can become inflamed or scarred, leading to discomfort and discharge.[23]
Compensatory Mechanisms
- Socket contraction: The body may attempt to heal the surgical site by contracting the tissues, which can lead to a contracted socket. This condition can make fitting and retaining an ocular prosthesis challenging.
- Inflammatory responses: Chronic inflammation in the anophthalmic socket can result from irritation caused by the prosthesis or exposure to environmental factors, potentially exacerbating scarring and fibrosis. Please see StatPearls' companion resource, "Contracted Socket," for more information.
Clinical Implications
Changes in the anophthalmic socket necessitate precise fitting and regular maintenance of the ocular prosthesis to ensure both comfort and a natural appearance. An ill-fitting prosthesis can worsen tissue changes and lead to complications.
Effective management of complications, such as socket contraction, eyelid malposition, and chronic inflammation, is essential for preserving the health of the anophthalmic socket and enhancing the patient's quality of life. This management may include therapeutic interventions such as surgery and the use of lubricants.[24]
History and Physical
The absence or loss of an eye due to a congenital malformation, tumor, trauma, or end-stage ocular disease can be extremely challenging for patients. Managing the anophthalmic socket has long been a complex task for ophthalmologists and ocularists. The loss of binocular vision, along with impaired peripheral vision and depth perception, can interfere with daily activities and restrict career opportunities.[25][26]
Perinatal Assessment of Congenital Anophthalmia
Ultrasound can be used to detect anophthalmia in utero, with ocular abnormalities potentially visible as early as the end of the first trimester using 2D and 3D ultrasonography. The diagnosis can be confirmed with fetal magnetic resonance imaging (MRI).[27][28] Given the potential for a syndromic origin, the absence of an eye on ultrasound should prompt further genetic evaluation through amniocentesis or chorionic villus sampling. Notably, it is also important to investigate environmental factors, such as illness, toxin exposure, and vitamin A deficiency.[29]
Neonatal symptoms of anophthalmia may include small conjunctival sacs, compressed lid structures, and a shorter lid fissure. In cases of unilateral anophthalmia, ophthalmic findings in the single eye may reveal coloboma, cataracts, retinal abnormalities, or optic nerve hypoplasia.[30][31]
Assessment of Acquired Anophthalmia
Acquired anophthalmia is more common than congenital anophthalmia and typically results from surgical enucleation, although it can also occur due to trauma. Indications for enucleation include malignant intraorbital tumors, painful blind eyes, and phthisical or buphthalmic eyes that do not respond to other treatment modalities.
Acquired anophthalmos may be complicated by post-enucleation socket syndrome (PESS). Socket changes that may lead to this complication include:[32][33]
- Progressive intraorbital volume loss, leading to rotatory displacement of orbital contents from superior to posterior and posterior to inferior.
- Retraction of the superior rectus and levator muscle complex.
- Downward and forward displacement of orbital fat.
- Upward movement of the distal end of the inferior rectus, resulting in a shallow inferior fornix and probable prosthesis tilt.
- Superior sulcus deepening and upper lid ptosis
- Progressive lower lid laxity aggravated by the weight of the prosthesis
Another less common but significant complication of acquired anophthalmos is a contracted socket. Therefore, the evaluation of anophthalmia and the anophthalmic socket should include a thorough assessment of these complications (discussed in detail in the Evaluation section). Patients with anophthalmic sockets may report symptoms such as discharge, lid malposition, socket discomfort, lesions, cysts, lagophthalmos, and enophthalmos, which may indicate socket dryness, infection, inflammation, or an unsuitable prosthesis.[34][35][36][37]
Evaluation
Congenital Anophthalmia
Congenital eye and orbit deformities, including anophthalmos and microphthalmos, exhibit varying degrees of severity. These conditions may be unilateral or bilateral, with over 50% associated with other systemic disorders.[38][39] Clinically, anophthalmos and microphthalmos often present similarly. Deficient palpebral and bulbar conjunctiva, along with an underdeveloped orbital bone structure, result in reduced eyelid size.[40] The absence of a globe hinders the growth of the socket, eyelids, and the entire hemiface, including the maxilla, maxillary sinus, and jaw.[41][42] The eyelids are often short vertically and horizontally (phimosis).
Blepharoptosis may result from the absence of the levator muscle, while shorter conjunctival fornices can make prosthesis implantation and use challenging. Without treatment, patients may experience a significant reduction in orbital entry size and a loss of up to 60% of orbital volume. Proper replenishment of orbital soft tissue volume is essential for maintaining orbital bone development and adjacent facial growth.[43][44][45]
An ultrasound should be conducted if an eye abnormality is suspected to determine the existence of optic structures. Electrodiagnostic tests, such as flash visual evoked potentials, may be used to detect functional retinal tissue. Computed tomography (CT) and MRI can help define the globe's contents, assess the extent of central optic nerve involvement, and screen for coexisting central nervous system disorders. Additionally, renal ultrasonography is recommended in individuals with anophthalmia due to the frequent coexistence of ocular and renal conditions.
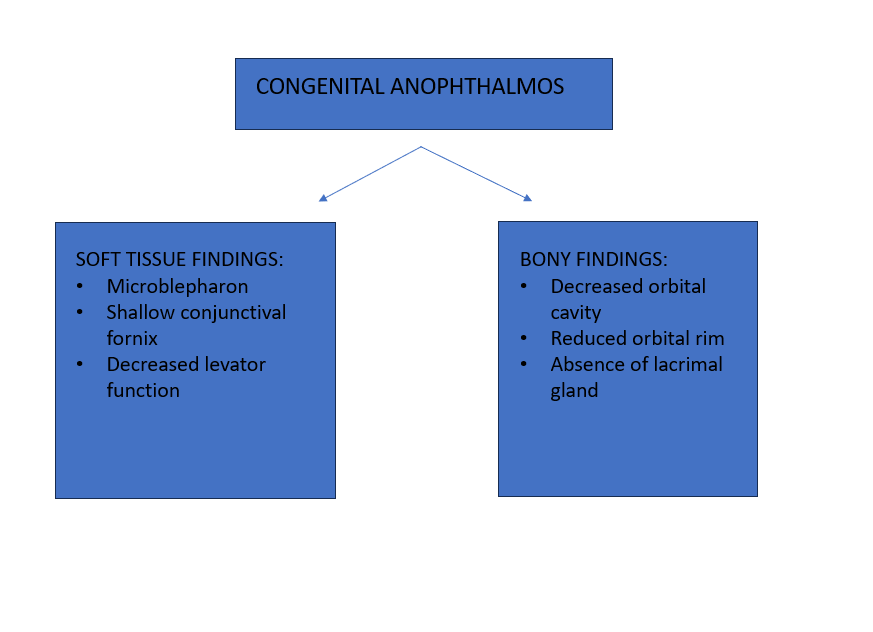
Parents should be informed about the condition and the available therapeutic options after confirming a diagnosis of anophthalmos or microphthalmos (with or without a cyst). A pediatrician will evaluate any systemic abnormalities, while a pediatric ophthalmologist will assess ocular defects and visual potential. An oculoplastic or orbital specialist will address eyelid and socket issues (see Image. Summary of Congenital Anophthalmia).
Acquired Anophthalmic Socket
The clinical assessment of an acquired anophthalmic socket should focus on identifying any complications following enucleation or evisceration surgery. Certain ideal characteristics of the anophthalmic socket are also being evaluated (see Table 1. Ideal Anophthalmic Socket Characteristics).
Table 1. Ideal Anophthalmic Socket Characteristics
| Characteristics | Description |
| Implant | A bioinert implant with enough volume, positioned centrally and well-covered, transmits motility to the overlying prosthesis. |
| Socket lining | A socket lined with healthy conjunctiva and deep fornices accommodates a prosthesis and allows for horizontal and vertical movement. |
| Eyelid position | Normal eyelid and eyelash position, appearance, and eyelid tone. |
| Eyelid fold | The supratarsal eyelid fold is symmetrical to the contralateral eyelid. |
| Prosthesis | A well-fitting ocular prosthesis that closely resembles the sighted contralateral globe and aligns with the same horizontal and anteroposterior planes. |
During follow-ups with anophthalmic patients, a thorough history must be obtained, and the general appearance of the prosthesis in the socket should be assessed. History-taking should cover the fit of the prosthesis, the presence of pain or discharge, outcomes from regular visits to the ocularist, patient satisfaction, and the use of protective glasses for the remaining eye. The socket must then be systematically evaluated, noting the presence or absence of the below-mentioned assessments.
General appearance assessments
- Well-centered
- Symmetry of the horizontal plane
- Prominence of the prosthesis
- Superior sulcus deepening
- Lower lid sagging, laxity, or ectropion
- Upper lid ptosis or entropion
- Lagophthalmos
- Synchronous eye movement
Prosthesis and socket assessments
- Shine, borders, and scratches on the prosthesis
- Unusual socket characteristics after prosthesis removal
- Conjunctival erythema or inflammation, including giant papillary conjunctivitis (GPC), characterized by an everted upper lid, pyogenic granuloma, discharge, or bleeding
- Implant displacement (whether present and well-centered), migration, and exposure or extrusion
- Fornix depth and symblepharon formation [46][47][48]
Treatment / Management
Anophthalmic surgery has evolved beyond merely replacing a diseased eye with an orbital implant. Enucleation and evisceration, such as other microsurgical ophthalmic procedures, must be performed with precision to achieve optimal functional and cosmetic outcomes while preventing complications that can exacerbate the patient's condition. Effective treatment and management of anophthalmia require prompt and early surgical intervention for congenital cases and meticulous management of complications associated with the anophthalmic socket.
Congenital Anophthalmia or Microphthalmia
The management of suspected anophthalmia or microphthalmia typically involves a multidisciplinary team, including a pediatric ophthalmologist, pediatrician, social worker, oculoplastic/orbital specialist, geneticist, and ocularist.[49][50] Treatment planning should be tailored to the systemic abnormalities identified. Referral to a genetic counseling specialist is appropriate once the family has adjusted to the situation and begun eye socket management. Explaining the complexity and guarded prognosis of the condition is crucial while maintaining positivity and encouragement. Parents should understand that early socket expansion using progressively larger conformers can enhance aesthetics in cases of anophthalmos or microphthalmos. Subsequent steps involve fitting an ocular prosthesis and, if necessary, an orbital implant, which can yield satisfactory results.[51](B3)
Patients with phimotic lids and short conjunctival fornices may require early tissue expansion or, in severe cases, the removal of a vestigial eye followed by placement of an orbital implant (expandable or nonexpandable). The eye and orbit grow rapidly in the first year of life, with 70% of globe volume increase occurring by age 4 and 90% by age 7, completing by early adolescence around age 14.[52][53] Reconstruction in cases of anophthalmia or microphthalmia involves expanding affected tissues both horizontally and vertically in the eyelids, enlarging the conjunctival space and forniceal depth, and increasing orbital bone volume.[54][55](B2)
Acquired Anophthalmia
Enucleation and evisceration, such as other microsurgical ophthalmic therapies, must be performed with care to achieve optimal functional and cosmetic outcomes while minimizing complications that could exacerbate the patient's challenging condition. After enucleation or evisceration, an orbital implant is used to replace the lost volume. Orbital implants come in 2 types—porous and nonporous (see Table 2. Types of Orbital Implants).[56][57][58][59](B2)
Table 2. Types of Orbital Implants
|
Porous, Bio-integrated Orbital Implants |
Nonporous, Inert Orbital Implants |
| Allow for anchoring of the extraocular muscles with a proliferation of fibrovascular tissue into the implant itself. |
Nonintegrating and easier to insert or remove. |
| Less migration and better motility but higher exposure rates. |
Worse motility and a higher risk of migration. The sphere is wrapped in a sclera/polygalactin mesh/autogenous material (dermis/fascia) to provide substrate for attachment of extraocular muscles. |
|
Hydroxyapatite (complex calcium phosphate mineral), porous polyethylene, Medpor®, and aluminum oxide. |
Polymethyl methacrylate, acrylic, glass, silicone. |
After enucleation, most patients use 20- to 22-mm spherical implants, while evisceration typically requires 18- to 20-mm implants. Smaller implants (16-18 mm) may be more suitable for young patients due to their age and ongoing orbital bone growth. Individualizing the implant size is crucial for optimizing orbital volume replacement and achieving the best functional and cosmetic results.[60][61](B2)
Postoperative Care Following Enucleation, Evisceration, and Secondary Orbital Implant Surgery
Pain is often treated with mild analgesics such as acetaminophen, codeine, hydrocodone, and morphine. If severe pain persists despite moderate analgesics, stronger oral or intramuscular pain medications may be necessary. Nausea is prevalent following socket surgery due to general anesthesia, pain, and vasovagal reactions, similar to what is observed in strabismus surgery. If intraoperative and recovery area antiemetic therapy is insufficient, sublingual, oral, or suppository antiemetic drugs may be administered before discharge to manage postoperative nausea.
Eye patches can typically be removed after 3 to 5 days without requiring special cleaning. Showering and light face cleansing are permissible. A 1- to 3-week course of topical antibiotic-steroid eye drops or ointment, such as tobramycin-dexamethasone, is usually initiated 2 to 4 times daily after removing the patch. Cool compresses may be used 4 times a day for 10 to 15 minutes each for a few days after removing the patch to aid with swelling and socket soreness. The temporary acrylic conformer is retained in the socket until the ocularist evaluates the patient for an "impression-fitted" bespoke prosthesis when the conjunctival chemosis resolves, which is usually 6 weeks after surgery. Please see StatPearls' companion resource, "Enucleation," for more information.[62][63](A1)
Differential Diagnosis
Congenital anophthalmia with or without a cyst is a close differential diagnosis of microphthalmia with or without a cyst. Both conditions may present with a clinically invisible globe. As the management depends on the presence or absence of the ocular tissue and its viability, the presence of any ocular elements must be identified using appropriate investigations, as discussed above. Unlike microphthalmia-associated cysts, congenital cystic eye-related cysts have a predilection for the orbit's upper and central parts. Histopathology typically reveals rudimentary ocular structures in microphthalmia, whereas anophthalmia shows the absence of such structures.
A history of sudden-onset and rapidly progressive orbital swelling may raise suspicion of an underlying malignancy. Conditions such as dermoid cysts, epidermoid cysts, cryptophthalmos, arachnoid cysts, meningocele, orbital teratomas, primary optic nerve sheath cysts, and encephalocele can mimic an intraorbital cyst, with or without anophthalmia. A meticulous evaluation is crucial in these cases to ensure accurate diagnosis and appropriate management.[64][65]
The differential diagnosis of an anophthalmic socket involves conditions with similar clinical presentations, which include:
- Congenital anophthalmia and microphthalmia: These conditions are characterized by the absence of an eye (anophthalmia) or the presence of a very small eye (microphthalmia) from birth. An anophthalmic socket appearance from birth may be associated with craniofacial anomalies.
- Phthisis bulbi: This condition is characterized by a shrunken, nonfunctional eye, often resulting from severe ocular trauma, inflammation, or end-stage eye disease. A small, disorganized eye within the orbit is often associated with pain, inflammation, and a history of previous eye disease or injury.[66]
- Severe orbital trauma: Significant trauma to the orbit can result in severe damage or dislocation of the eye. Clinicians may observe a history of trauma, potential orbital fractures, and damaged ocular structures that can mimic the appearance of an anophthalmic socket.[67]
- Orbital cellulitis or abscess: Severe infection of the tissues surrounding the eye can lead to significant inflammation and swelling. Symptoms may include pain, redness, swelling, fever, and impaired ocular movement. In severe cases, the infection may cause proptosis or cause the eye to be pushed back or become nonfunctional, potentially simulating the appearance of an anophthalmic socket. Please see StatPearls' companion resource, "Orbital Cellulitis," for more information.
- Chronic orbital inflammation: Conditions such as idiopathic orbital inflammation (orbital pseudotumor) can cause chronic inflammation of the orbit. Symptoms may include proptosis, pain, swelling, and decreased vision. In chronic cases, tissue changes may develop that resemble those seen in an anophthalmic socket.[68]
- Orbital tumors: Benign benign and malignant tumors in the orbit, including rhabdomyosarcoma, lymphoma, and metastatic lesions, can alter the orbital structures. Symptoms may include proptosis, pain, vision changes, and the presence of a palpable mass. Advanced cases can lead to secondary orbital changes that mimic the appearance of an anophthalmic socket.[69]
- Postsurgical changes: Certain ocular surgeries, such as orbital decompression or extensive eyelid procedures, can modify the appearance of the orbit. History of surgery, eyelid position changes, and orbital volume alterations should be assessed.[70]
- Enucleation or evisceration: Removal of the eye, often due to trauma, tumors, or severe disease, results in an absent eye. The patient's surgical history and any postoperative changes are usually reported.
A thorough clinical assessment and careful selection of diagnostic tests are essential for distinguishing each condition and guiding appropriate management.
Treatment Planning
Treatment planning for an anophthalmic socket involves a comprehensive approach aimed at restoring function, aesthetics, and comfort. The treatment plan is tailored to individual patient's needs and may include surgical interventions, prosthetic fitting, and ongoing care.
Key Components of Treatment Planning for an Anophthalmic Socket
The critical components of treatment planning for an anophthalmic socket are listed below.
Initial assessment and consultation: The initial assessment and consultation for managing an anophthalmic socket involves thoroughly assessing anatomical structures and the patient's history.
- Comprehensive evaluation: A detailed clinical assessment is conducted to evaluate the condition of the socket, eyelids, and surrounding structures.
- Patient history: The patient's medical history is reviewed, focusing on the cause of anophthalmia, previous surgeries, and any associated conditions.[71]
Surgical reconstruction: Surgical reconstruction for an anophthalmic socket focuses on socket reconstruction and eyelid surgery.
- Socket reconstruction: Surgical procedures may be necessary to create or enhance the socket to support a prosthetic eye. Socket reconstruction may involve the below-mentioned grafts and implants.
- Dermis-fat grafts: These are used to provide volume and improve the contour of the socket.
- Orbital implants: These are used to maintain orbital volume and support the prosthesis.
- Mucous membrane grafts: These are used to line the socket when conjunctival tissue is insufficient.
- Eyelid surgery: Correction of eyelid malpositions, such as ptosis, entropion, or ectropion, is essential to ensure proper coverage and aesthetics.[72]
Prosthetic fitting: Prosthetic fitting is crucial in achieving a natural appearance and restoring confidence for patients with an anophthalmic socket.
- Custom ocular prosthesis: A custom-made ocular prosthesis is fitted to match the patient's other eye in color and appearance. The process includes the below-mentioned steps.
- Impression molding: An impression of the socket is taken to create a well-fitting prosthesis.
- Prosthetic fabrication: The prosthesis is crafted to match the patient's eye color, shape, and size.
- Fitting and adjustment: The prosthesis is fitted comfortably and securely, with adjustments made as necessary.[73]
Postoperative care: Effective postoperative care is essential to ensure successful outcomes and address any potential complications following anophthalmic socket surgery.
- Regular follow-up: The healing process should be closely monitored to ensure that the socket and prosthesis remain healthy and functional.
- Management of complications: Any complications, such as socket contracture, implant extrusion, or infection, should be promptly addressed.[74]
Long-term maintenance: Long-term maintenance is essential for ensuring the continued comfort, appearance, and functionality of the ocular prosthesis.
- Regular cleaning and polishing: Routine care is necessary to maintain the prosthesis's appearance and function.
- Periodic adjustments: Regular assessments are required to ensure the prosthesis continues to fit well as the socket and surrounding tissues change over time.
- Replacement of prosthesis: The prosthesis should be replaced every few years or as needed due to wear or changes in the socket.[75]
Psychosocial support: Psychosocial support is essential for helping patients navigate the emotional and psychological challenges associated with anophthalmia and the use of an ocular prosthesis.
- Counseling services: Psychological support and counseling are provided to assist the patient in adjusting to the loss of an eye and the use of a prosthetic.
- Support groups: Patients are connected with support groups and resources for individuals with anophthalmia or similar conditions.[76]
Patient education: Patient education is crucial in ensuring that individuals with an ocular prosthesis understand how to maintain their device and recognize potential issues.
- Instruction on prosthesis care: Patients should be guided on the proper care of their prosthesis, including cleaning techniques and the appropriate times to seek professional care.
- Signs of complications: Patients should be informed regarding the signs and symptoms that may indicate complications, such as redness, discharge, or discomfort, that necessitate medical attention.[77]
Treatment planning for an anophthalmic socket is an interprofessional effort that involves ophthalmologists, oculoplastic surgeons, prosthetists, and mental healthcare professionals. The aim is to restore both appearance and function while delivering comprehensive care and support. Each patient's plan is customized to achieve the best possible outcomes in aesthetics, comfort, and quality of life.
Staging
Staging an anophthalmic socket involves evaluating the condition of the socket and surrounding structures to guide treatment planning and interventions. Various classification systems and criteria can be used to stage the socket based on factors such as volume, tissue health, and the presence of complications.
Staging of Anophthalmic Socket
A commonly used staging approach for an anophthalmic socket is mentioned below.
Stage 0: Normal anophthalmic socket
- Volume: Adequate volume without the need for augmentation.
- Tissue health: Healthy conjunctival lining and fornices.
- Complications: No significant complications; well-fitting prosthesis.
Stage 1: Mild socket deficiency
- Volume: Slight volume deficiency that may require minimal augmentation (eg, a small orbital implant).
- Tissue health: Mild conjunctival shrinkage or scarring.
- Complications: Minor complications such as mild discharge or discomfort.
Stage 2: Moderate socket deficiency
- Volume: Moderate volume deficiency requiring a larger orbital implant or dermis-fat graft.
- Tissue health: Moderate conjunctival shrinkage, scarring, or inflammation.
- Complications: More significant issues such as recurrent infections, moderate discharge, or mild ptosis.
Stage 3: Severe socket deficiency
- Volume: Severe volume loss requiring complex reconstructive surgery (eg, large dermis-fat graft and multiple implants).
- Tissue health: Severe conjunctival shrinkage or extensive scarring.
- Complications: Severe complications such as persistent infection, severe discharge, or major ptosis.
Stage 4: Complex anophthalmic socket
- Volume: Extensive volume loss with severe structural deficiencies requiring advanced reconstructive techniques.
- Tissue health: Severely compromised tissue with significant conjunctival and orbital scarring.
- Complications: Includes socket contracture, implant extrusion, severe ptosis, or ectropion.
Factors Considered in Staging
- Socket volume: Assessment through clinical examination and imaging studies (eg, CT and MRI) to determine the extent of volume loss.
- Conjunctival health: Evaluation of the conjunctival tissue for signs of shrinkage, scarring, or inflammation.
- Orbital rim and eyelid position: Assessment of the bony orbital rim and eyelid positions to identify ptosis, entropion, or ectropion.
- Prosthesis fit and function: Evaluation of how well the prosthesis fits and functions within the socket, including aspects of patient comfort and aesthetic outcomes.
- Presence of complications: Identification of any complications such as infection, discharge, socket contracture, and implant issues.
Treatment Implications Based on Staging
- Stages 0 and 1: Conservative management, including fitting and adjusting the prosthesis, minor surgical corrections, and regular follow-up visits.
- Stage 2: Intermediate interventions such as moderate surgical reconstruction, implant placement, and more frequent follow-up and adjustments.
- Stages 3 and 4: Advanced surgical reconstruction, potentially involving multiple stages of surgery, complex grafting procedures, and comprehensive postoperative care and rehabilitation.
Staging an anophthalmic socket is crucial for developing an effective treatment plan. Staging helps determine the severity of the condition and tailor interventions to restore function, aesthetics, and patient comfort. An interprofessional approach, involving ophthalmologists, oculoplastic surgeons, prosthetists, and other healthcare professionals, is essential for the optimal management of the anophthalmic socket.
Prognosis
True anophthalmos is classified as a pediatric ocular emergency. The growth of the bony orbit depends on the development of the globe, and an absent or severely microphthalmic eye hinders this process, resulting in a small bony cavity. This condition is not merely a cosmetic issue but also complicates the fitting of a prosthesis. Despite early and appropriate treatment, outcomes for anophthalmos can be challenging.[78][79] Recent neuroimaging research indicates that individuals with early-life blindness, including those with anophthalmia, undergo extensive brain remodeling. In these cases, the superior colliculus is utilized to process auditory information.
Bilateral anophthalmia or severe microphthalmia without light sensitivity may reverse the natural sleep-wake cycle. In such cases, melatonin supplementation at night can effectively establish a regular nocturnal sleep pattern. Growth evaluation is crucial, as there may be associated pituitary disorders. A developmental assessment by a pediatrician experienced in screening children with vision issues can identify early challenges, offering valuable insights and reassurance to parents, as visually impaired children develop differently from their sighted peers.
The prognosis of an anophthalmic socket is influenced by several factors, including the underlying cause of eye loss, the health of the remaining orbital structures, the presence of complications, and the adequateness of rehabilitation efforts. Below is a detailed overview of the factors influencing the prognosis and the expected outcomes for patients with an anophthalmic socket.
Factors Influencing Prognosis
Cause of eye loss
- Trauma: Eye loss due to trauma can lead to complex orbital injuries and significant scar tissue formation, potentially complicating socket rehabilitation.
- Tumors: Patients who have undergone surgery for malignant tumors may have a more challenging rehabilitation process due to extensive tissue removal and the potential need for additional treatments such as radiation therapy.
- Infections: Severe infections leading to eye loss may result in significant scarring and inflammation, thereby affecting the overall prognosis.[80]
Orbital health
- Volume and tissue health: Adequate orbital volume and healthy conjunctival tissue are essential for a favorable prognosis. Loss of volume or unhealthy tissue can complicate prosthesis fitting and overall comfort.
- Implant stability: The type and stability of the orbital implant are critical factors. Implants that are well-integrated with surrounding tissues typically yield better outcomes.
- Eyelid position: Proper eyelid function and positioning are important for maintaining prosthesis retention and achieving desirable aesthetics.
Complications
- Infections: Recurrent infections can lead to chronic inflammation and scarring, adversely affecting the socket's health and functionality.
- Implant extrusion: Implant extrusion necessitates additional surgical interventions and complicates the rehabilitation process.
- Contracture: Socket contracture can lead to discomfort and difficulties with prosthesis retention, often requiring surgical correction.[81]
Rehabilitation efforts
- Prosthesis fitting: A well-fitting ocular prosthesis significantly enhances cosmetic and functional outcomes.
- Regular follow-up: Regular follow-up with an ophthalmologist and an ocularist is essential for addressing and managing any emerging issues.[82]
Expected Outcomes
Cosmetic appearance
- Advances in prosthesis design and technology have significantly enhanced aesthetic results for many patients.[83]
- A well-fitted prosthesis, particularly in a socket with adequate volume and healthy tissue, often leads to satisfactory cosmetic outcomes.
Functional outcomes
- Most patients adapt well to wearing an ocular prosthesis and experience minimal discomfort.
- Properly managed sockets generally do not impact daily activities significantly.[84]
Quality of life
- Studies show that patients with an anophthalmic socket can achieve a high quality of life, especially with effective prosthetic rehabilitation.
- Psychological support and counseling can further enhance patient adaptation and overall satisfaction.[85]
Long-term stability
- With proper care and regular monitoring, many patients maintain stable socket conditions and adequate prosthesis function over the long term.
- Surgical interventions, when necessary, can address complications and improve outcomes.[86]
Challenges and Limitations
- Chronic inflammation: Persistent inflammation can lead to discomfort and complications, impacting long-term outcomes.
- Socket contracture: Recurrent or severe contracture may require multiple surgical interventions to address and correct the issue.
- Psychosocial impact: The psychological effects of eye loss can be significant, requiring ongoing support to address issues such as body image and self-esteem.
The prognosis for patients with an anophthalmic socket is generally favorable, especially with the advances in modern surgical techniques and prosthetic technology. Effective management involves a multidisciplinary approach, including regular follow-up, timely intervention for complications, and comprehensive rehabilitation efforts. The ultimate goal is to achieve the best possible cosmetic and functional outcomes, thereby enhancing the patient's overall quality of life.
Complications
Patients with anophthalmia should be monitored closely for potential complications (see Table 3. Complications of Anophthalmia). Significant cosmetic defects are common if the anophthalmic orbit is not corrected promptly. Despite using conformers, expanders, or surgical interventions, outcomes are often visually unsatisfactory. Prostheses are typically immobile, and eyelids may exhibit major abnormalities such as shortening and immobility. Phantom eye syndrome, which may include phantom pain, phantom sensation, and phantom vision, refers to any sensation experienced by a patient with anophthalmia or enucleation.[87] Individuals with prosthetic eyes should avoid focusing on their prostheses, as excessive self-consciousness can cause persistent anxiety.[88][89]
Table 3. Complications of Anophthalmia
| Intraoperative Complications | Postoperative Complications |
|
Removal of the wrong eye |
Wound-related:
|
| Extraocular muscle damage |
Conjunctiva-related:
|
| Levator damage |
Implant-related:
|
| Orbital hemorrhage |
Lid-related:
|
Management of Anophthalmic Socket Problems
Managing anophthalmic socket issues is crucial in ophthalmic and reconstructive surgery, addressing both functional and cosmetic concerns. Effective management can significantly enhance the quality of life for patients with anophthalmic sockets.
Socket dryness: Using artificial tears or gel should be used throughout the day to alleviate dryness. If tear supplements do not alleviate dry eye problems, applying a drop of light mineral oil to the surface of the artificial eye can facilitate the eyelid to move smoothly over the prosthesis.
Discharge and irritation: The use of a prosthetic eye can lead to mucoid discharge, which negatively impacts the quality of life for those who have lost an eye. Frequent handling of the prosthesis may retard the development of the normal prosthesis socket microenvironment and damage the highly polished prosthetic surface, which may increase the discharge.[90] Recurrent and chronic socket discharge is a defining symptom of GPC. Treatment often involves using a mild corticosteroid drop, such as fluorometholone, or a combination antibiotic/steroid drop, such as tobramycin-dexamethasone, once or twice daily. This approach frequently reduces the discharge and should be guided by an ophthalmologist and ocularist based on the specific condition.
Reports of intermittent bleeding are common, and these vascular lesions usually occur around an implant peg, at the conjunctival closure site, or in frictional areas. Treatment typically involves using a moderate corticosteroid drop, such as fluorometholone, or a combination antibiotic/steroid drop, such as tobramycin-dexamethasone, applied once or twice daily. This treatment usually reduces discharge and helps resolve small lesions.
A conjunctival bacterial or viral infection should be considered when the discharge is purulent or copious. Acute or chronic conjunctivitis usually presents with additional symptoms.[91] Another possible reason for persistent or recurring socket discharge is a pyogenic granuloma. Many individuals who develop large pyogenic granulomas may eventually require surgical granuloma excision and removal of the triggering chemical or irritant. An excision biopsy can provide histological confirmation if the diagnosis remains uncertain.[92]
Lagophthalmos and prosthesis surface exposure: Individuals with nocturnal lagophthalmos may experience dryness on the prosthesis's anterior surface, leading to eyelid or lash adhesion. To clean the prosthetic eye, it should be removed from the socket, and the surface should be washed with a moist paper towel and cool tap water. To prevent debris buildup and eyelid adhesion, a light mineral oil or lubricating eye ointment (such as Lacri-lube) should be applied to the anterior surface of the prosthesis before bedtime.
Socket pain: Although rare, pain and discomfort in the anophthalmic socket can vary in severity and impact daily activities.[91] Socket pain and discomfort may arise from several issues, which can be identified through a comprehensive evaluation of the prosthesis and eye socket.
The socket implant should be assessed for signs of migration and the conjunctiva for indications of infection, inflammation, or implant exposure. Implant migration can cause pressure between the prosthesis and implant, affecting the prosthetic fitting. Triamcinolone injection (0.3–0.4 mL of 40 mg/mL vial) into the peritrochlear area may effectively relieve this discomfort. For persistent socket pain, neuroimaging (eg, CT and MRI) of the orbit, paranasal sinuses, and brainstem are essential to rule out amputation neuromas, sinus infections or masses, and intraorbital or central nervous system anomalies.[93]
Anterior orbital cysts: A subconjunctival or anterior orbital cyst may cause socket pain, including aching and pressure sensations, as well as issues with prosthetic eye fit.[94] These cysts form from trapped conjunctival epithelium after wound closure. Management options include surgical excision, marsupialization, 100% alcohol injection, and trichloroacetic acid injection.[95]
Eyelid malpositions: Lower eyelid laxity, prevalent in patients with artificial eyes, results from aging eyelids supporting the prosthesis and changes in soft tissue support following eye removal (anophthalmic socket syndrome). Lower eyelid laxity may be addressed with a tarsal strip operation.[96] Horizontal lid tightening helps preserve the natural shape of the lower eyelid and lateral canthus, thereby improving support for the prosthesis while preserving conjunctival tissue and inferior fornix volume.
Lower eyelid ectropion, often a result of significant lid laxity, may initially appear as a cosmetic issue but may eventually lead to prosthesis retention. A tarsal strip-type operation with a posterior lamellar spacer graft (eg, auricular cartilage) may be necessary.[97] Upper eyelid ptosis can result from laxity in the fibrous connective tissue framework of the superior orbit (including the Whitnall ligament), leading to posterior and inferior rotation of orbital tissues (PESS). The condition may also be caused by trauma from injury or surgery or senile dehiscence of the levator aponeurosis.[98]
Deep superior sulcus and enophthalmos: Enucleation or evisceration surgery can cause soft tissue and volume changes in the socket, leading to upper eyelid ptosis, lower eyelid malposition, and a deepened superior sulcus. Factors such as inadequate volume replacement (eg, too small an implant or lack of an implant) at the time of the enucleation or evisceration procedure and postsurgical orbital fat atrophy are other important factors in the development of a deep superior sulcus.[99][100][101] Conservative therapy for superior sulcus deformity may include using lightly tinted glasses or a weak plus lens (+1 to +2) to provide magnification (see Image. Superior Sulcus Deformity).
Surgical options include:
- Correcting bone defects from previous orbital fractures.
- Restoring socket volume with implants (eg, orbital floor wedge implant).
- Superior sulcus tissue grafting using dermis fat grafts or acellular human dermis grafts (eg, AlloDerm by Lifecell Inc., Woodlands, TX, USA or DermaMatrix by Synthes, West Chester, PA, USA).[102][103]
Soft tissue fillers, such as hyaluronic acid-derived products, offer a novel approach to restoring superior sulcus volume loss in the anophthalmic socket.[104] Patients with anophthalmia and deep superior sulci, enophthalmos, or eyelid malpositions may require multiple surgical interventions to achieve satisfactory symmetry. Enucleation or evisceration-related alterations, inadequate implant volume replacement, and implant extrusion can contribute to enophthalmos. A subsequent intraconal orbital implant can address superior sulcus depression and enophthalmos. Secondary orbital implantation may also be indicated to improve prosthesis motility or resolve issues such as implant exposure or migration affecting prosthetic fitting.[105][106]
Implant migration: Long-term orbital implants may be subjected to implant migration due to gradual changes in the orbital soft tissue within the anophthalmic socket. This migration can lead to improper alignment of the prosthesis, resulting in discomfort, cosmetic deformities, and potential complications such as socket inflammation or infection. Regular follow-up and adjustments are essential to monitor the implant's position and address any issues promptly. In some cases, surgical intervention may be required to reposition or replace the implant to maintain optimal functionality and aesthetic appearance.
Implant infection: Factors that predispose to infection include early conjunctival dehiscence with implant exposure, poor or delayed vascular ingrowth due to chronic illness (eg, diabetes, immunosuppression, and vasculopathy), chemotherapy, radiation therapy, prior socket reconstruction, and delayed fibrovascular ingrowth within a host scleral shell with no portals for vascular growth.
Implant exposure and extrusion: Implant exposure may be caused by tension wound closure, poor surgical technique, infection, mechanical or inflammatory irritation from the porous implant surface, and delayed fibrovascular tissue ingrowth, leading to tissue collapse.[107]
Acquired socket contracture: Acquired socket contracture occurs when the orbital tissues in an anophthalmic socket shrink and shorten, resulting in inadequate conjunctival fornices for prosthesis retention.[108] Effective treatment aims to identify and address the underlying cause when possible. Preventive measures include preserving tissues (such as the conjunctiva), reducing dissection into the fornices, restricting cauterization, restoring tissues to their anatomical position, and using a conformer during the healing phase after orbital trauma surgeries (see Table 4. Stages and Management of Acquired Socket Contracture).[109][110][111][112]
Table 4. Stages and Management of Acquired Socket Contracture
| Socket Contracture Stages | Characteristics | Treatment Options |
|
Mild socket contracture |
Shortening of the posterior lamella (tarsus and conjunctiva) of the upper or lower eyelids. |
Marginal lid rotation (tarsotomy) may be combined with horizontal lid shortening. |
|
Moderate socket contracture |
Significant contracture and tissue loss of conjunctival surface area, especially in the inferior or superior conjunctival fornix. |
Tissue grafting procedures (amniotic membrane transplantation, mucous membrane grafting, skin grafting, or forearm-free flaps). |
|
Severe socket contracture |
Nearly absent or obliterated conjunctival fornices, making prosthetic eye retention difficult. |
Advanced procedures, including the previously mentioned techniques with or without a temporal flap. |
Postoperative and Rehabilitation Care
Follow-up examinations are typically scheduled at 1 week, 3 to 4 weeks, and a few weeks after fitting the prosthetic eye. Patients are then reevaluated every 6 to 12 months, with annual assessments thereafter. Frequent evaluations are important to address any concerns related to socket or eyelid malposition. The temporary acrylic conformer is retained in the socket until the ocularist evaluates the patient for a custom "impression-fitted" prosthesis, typically around 6 weeks after surgery, once conjunctival chemosis has resolved. If the conformer dislodges prematurely, it can be reinserted by the patient or surgeon using lubricating or antimicrobial eye ointment on its edges and interior. Should conjunctival chemosis prolapse from the lid fissure, applying lubricating ophthalmic ointment every 1 to 2 hours while awake is recommended.
Consultations
An interprofessional team approach is essential to provide comprehensive care and address the wide range of needs of patients with anophthalmia. The involvement of various specialties ensures that all aspects of the condition, from diagnosis to long-term management, are covered. Here are key specialties that should be consulted:
- Ophthalmology: An ophthalmologist, particularly one with experience in pediatric or neuroophthalmology, is crucial for the initial diagnosis, ongoing assessment of any residual vision, and management of associated ocular conditions.
- Oculoplastic surgery: Oculoplastic surgeons specialize in treating the eye socket, eyelids, tear ducts, and face. These professionals are essential for performing anophthalmia-related surgeries, such as socket expansion procedures and the insertion of orbital implants.
- Pediatrics or pediatric genetics: For congenital anophthalmia, a pediatrician or a geneticist can offer insights into the genetic aspects of the condition and guide the management of any related systemic issues. Genetic counseling may also be recommended for the family.
- Prosthesis specialist (ocularist): Ocularists are technicians who design, fabricate, and fit custom ocular prostheses. These specialists play a critical role in providing cosmetic solutions for patients with anophthalmia and work closely with patients to ensure the best possible aesthetic and functional outcomes.
- Radiology: Radiologists may be involved in the initial assessment and ongoing monitoring of anophthalmia, particularly with imaging studies such as MRI or CT scans, to evaluate the orbit and any associated craniofacial abnormalities.
- Neurology: In cases where anophthalmia is part of a broader syndrome or is associated with neurological conditions, a neurologist's expertise is invaluable for comprehensive care and management of neurological issues.[113]
- Psychology or psychiatry: The psychological impact of anophthalmia, particularly on self-image and social interactions, can be significant. Psychologists or psychiatrists may provide support and therapy to help patients and families cope with these challenges.
- Social work and patient advocacy: Social workers and patient advocates can help patients and families navigate healthcare systems, access resources, and connect with support groups. These professionals play a vital role in the overall well-being of patients and families.
- Occupational and physical therapy: These specialists may help address developmental challenges in children with anophthalmia and ensure that patients achieve their maximum functional potential.
- Special education services: Early intervention and special education services may be necessary for children to address developmental delays and provide support for learning and adaptation.
Collaboration among these specialties ensures that patients with anophthalmia receive a holistic care plan tailored to their individual needs, spanning medical, surgical, cosmetic, and psychosocial aspects.[114]
Deterrence and Patient Education
Educating patients about the importance of maintaining proper hygiene and attending regular follow-up visits is paramount. This education should include instructions on cleaning the socket and the prosthesis, recognizing signs of infection or irritation, and understanding the importance of moisture management to prevent dryness and discomfort. Patients should also be informed about the potential for socket changes over time, which may necessitate adjustments to or replacement of the ocular prosthesis to ensure a comfortable and secure fit.
Furthermore, education should address psychological aspects by providing support and resources to help individuals adjust to the loss of an eye and the use of a prosthesis. This includes discussions about social concerns, potential impacts on self-esteem, and strategies for handling questions or reactions from others. By providing comprehensive information and support, healthcare providers can help prevent complications, promote positive outcomes, and enhance the overall well-being of individuals living with an anophthalmic socket.[115]
Pearls and Other Issues
Pearls
-
Comprehensive initial evaluation: A thorough assessment of the anophthalmic socket, including orbital volume, eyelid position, and health of the conjunctival tissue, is critical for planning effective treatment and prosthesis fitting.
-
Custom ocular prosthesis: Personalized prosthetic eyes made by skilled ocularists provide the best cosmetic and functional outcomes. Prostheses must match the patient's other eye in color, size, and movement.
-
Interprofessional approach: Collaboration among ophthalmologists, ocularists, and plastic surgeons (when necessary) ensures comprehensive care. In addition, psychosocial support from counselors or support groups can aid in the emotional and mental adjustment of patients.
-
Regular follow-up: Routine check-ups with an ophthalmologist and ocularist are crucial for identifying and managing complications such as socket contracture, implant extrusion, and infections.[116]
Disposition
-
Postsurgical care: After enucleation or evisceration, patients require close monitoring for signs of infection, inflammation, or implant exposure. Early intervention is crucial to prevent complications. Emphasize the importance of adhering to follow-up appointments and postoperative care instructions to maintain socket health.
-
Long-term management: This part of management should include regular cleaning of the prosthesis and socket, periodic adjustments or replacements of the prosthesis, and prompt attention to any issues that arise to ensure ongoing functionality and comfort.
-
Psychological support: The loss of an eye can significantly affect a patient's mental health. Access to counseling services and support groups can aid in managing body image concerns and emotional distress, fostering better overall well-being.
Pitfalls
-
Delayed diagnosis of complications: Failure to recognize early signs of complications, such as implant extrusion, infection, or socket contracture, can lead to more severe problems requiring extensive surgical intervention.
-
Improper prosthesis fit: An ill-fitting prosthesis can cause discomfort, irritation, and poor cosmetic appearance. Regular adjustments by an ocularist are essential for maintaining a good fit.
-
Inadequate patient education: Patients should be educated about caring for their prostheses and sockets, attending regular follow-up visits, and recognizing signs of complications. Lack of proper education can lead to neglect and subsequent issues.[117]
Prevention
-
Meticulous surgical technique: The use of proper surgical techniques during enucleation or evisceration and implant placement helps minimize the risk of postoperative complications.
-
Prophylactic measures: The administration of antibiotics after surgery can prevent infections, while anti-inflammatory medications can help reduce postoperative inflammation.
-
Early intervention for complications: Prompt treatment of complications such as infections, implant exposure, or socket contracture can prevent more severe issues. Regular monitoring and early intervention are crucial for maintaining optimal outcomes.
-
Proper socket and prosthesis care: Patients should be educated on the importance of regularly cleaning and maintaining their ocular prostheses and sockets. Guidelines should be provided to ensure they perform these tasks effectively.[118]
Additional Information
-
Implant technology advances: Recent advancements in implant materials and designs have enhanced integration with surrounding tissues, leading to reduced complication rates and improved cosmetic results.
-
Socket expansion techniques: For contracted sockets, techniques such as mucous membrane grafting, dermis-fat grafting, and the use of expanders can facilitate better prosthetic fit and increased comfort.
-
Prosthetic eye innovations: Advances in materials and techniques have led to more realistic and comfortable prosthetic eyes. Innovations such as digital imaging and 3D printing are being explored to enhance the customization and fit of prostheses.
-
Long-term outcomes: Studies indicate that patients with anophthalmic sockets can achieve high satisfaction with their appearance and functionality and lead normal lives with proper management.
By incorporating these key insights, addressing potential pitfalls, and implementing effective prevention strategies, healthcare providers can optimize the management of anophthalmia, improving clinical outcomes and enhancing the quality of life for patients.[119]
Enhancing Healthcare Team Outcomes
Enhancing healthcare outcomes for patients with anophthalmic sockets involves an interprofessional approach that addresses the physical, emotional, and psychological aspects of care. Key strategies to consider are listed below.
- Custom ocular prostheses: Creating custom-made ocular prostheses can significantly improve cosmetic appearance and patient satisfaction. These prostheses are designed to match the patient's other eye in size, color, and orientation. Advances in materials and technology can also enhance comfort and wearability.
- Surgical interventions: For some patients, surgical interventions may be necessary to prepare the anophthalmic socket for prosthetic fitting. These interventions can include procedures to improve socket depth, correct eyelid abnormalities, and address socket volume deficiencies. Surgical options may also involve implants to enhance cosmesis and provide additional support for the prosthetic eye.
- Long-term follow-up care: Regular follow-up with a multidisciplinary healthcare team, including an oculoplastic surgeon, an ocularist, and, potentially, a psychologist, is crucial. These appointments are essential for ensuring the health of the anophthalmic socket and the integrity of the prosthetic eye and addressing any psychological impacts.
- Psychological support: The loss of an eye can profoundly affect a patient's emotional and psychological well-being. Providing access to psychological support or counseling can help patients manage the emotional challenges associated with anophthalmic sockets. Additionally, support groups and peer counseling may offer valuable assistance and encouragement.
- Education and training: Educating patients on the care and maintenance of their ocular prosthesis is essential. This includes providing clear instructions on how to clean the prosthesis and socket, recognize signs of infection or irritation, and understand when to seek medical attention.
- Innovations and research: Staying abreast of the latest research and innovations is vital to providing patients access to new treatments and technologies. Advancements may include improvements in prosthetic materials, surgical techniques, or nonsurgical treatments that enhance socket health and prosthetic fit.
- Interprofessional team approach: A coordinated approach involving ophthalmologists, ocularists, oculoplastic surgeons, psychologists, and other healthcare professionals is crucial for comprehensive care. This interprofessional approach addresses the diverse needs of patients with anophthalmic sockets.
Implementing these strategies requires a patient-centered approach, considering the unique needs and circumstances of each patient. Enhancing healthcare outcomes for patients with anophthalmic sockets is an ongoing process that benefits from continuous communication, support, and access to the latest advancements in care.[120]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Fitzpatrick DR, van Heyningen V. Developmental eye disorders. Current opinion in genetics & development. 2005 Jun:15(3):348-53 [PubMed PMID: 15917212]
Level 3 (low-level) evidenceHandler LF, Heher KL, Katowitz JA. Congenital and acquired anophthalmia. Current opinion in ophthalmology. 1994 Oct:5(5):84-90 [PubMed PMID: 10172408]
Level 3 (low-level) evidenceSaxby E, Davies R, Kerr J. Living with an artificial eye-the emotional and psychosocial impact. Eye (London, England). 2019 Aug:33(8):1349-1351. doi: 10.1038/s41433-019-0398-y. Epub 2019 Mar 19 [PubMed PMID: 30890777]
Quaranta-Leoni FM, Fiorino MG, Quaranta-Leoni F, Di Marino M. Anophthalmic Socket Syndrome: Prevalence, Impact and Management Strategies. Clinical ophthalmology (Auckland, N.Z.). 2021:15():3267-3281. doi: 10.2147/OPTH.S325652. Epub 2021 Aug 6 [PubMed PMID: 34393477]
Kord Valeshabad A, Naseripour M, Asghari R, Parhizgar SH, Parhizgar SE, Taghvaei M, Miri S. Enucleation and evisceration: indications, complications and clinicopathological correlations. International journal of ophthalmology. 2014:7(4):677-80. doi: 10.3980/j.issn.2222-3959.2014.04.17. Epub 2014 Aug 18 [PubMed PMID: 25161942]
Chen XY, Yang X, Fan XL. The Evolution of Orbital Implants and Current Breakthroughs in Material Design, Selection, Characterization, and Clinical Use. Frontiers in bioengineering and biotechnology. 2021:9():800998. doi: 10.3389/fbioe.2021.800998. Epub 2022 Feb 17 [PubMed PMID: 35252161]
Demmin DL, Silverstein SM. Visual Impairment and Mental Health: Unmet Needs and Treatment Options. Clinical ophthalmology (Auckland, N.Z.). 2020:14():4229-4251. doi: 10.2147/OPTH.S258783. Epub 2020 Dec 3 [PubMed PMID: 33299297]
Roccia F, Boffano P, Guglielmi V, Forni P, Cassarino E, Nadalin J, Fea A, Gerbino G. Role of the maxillofacial surgeon in the management of severe ocular injuries after maxillofacial fractures. Journal of emergencies, trauma, and shock. 2011 Apr:4(2):188-93. doi: 10.4103/0974-2700.82204. Epub [PubMed PMID: 21769204]
Verma AS, Fitzpatrick DR. Anophthalmia and microphthalmia. Orphanet journal of rare diseases. 2007 Nov 26:2():47 [PubMed PMID: 18039390]
Ahmad ME, Dada R, Dada T, Kucheria K. 14q(22) deletion in a familial case of anophthalmia with polydactyly. American journal of medical genetics. Part A. 2003 Jul 1:120A(1):117-22 [PubMed PMID: 12794703]
Level 3 (low-level) evidenceHoover-Fong JE, Cai J, Cargile CB, Thomas GH, Patel A, Griffin CA, Jabs EW, Hamosh A. Facial dysgenesis: a novel facial syndrome with chromosome 7 deletion p15.1-21.1. American journal of medical genetics. Part A. 2003 Feb 15:117A(1):47-56 [PubMed PMID: 12548740]
Arce-Estrada GE, Gómez-Toscano V, Cedillo-Peláez C, Sesman-Bernal AL, Bosch-Canto V, Mayorga-Butrón JL, Vargas-Villavicencio JA, Correa D. Report of an unsual case of anophthalmia and craniofacial cleft in a newborn with Toxoplasma gondii congenital infection. BMC infectious diseases. 2017 Jul 3:17(1):459. doi: 10.1186/s12879-017-2565-8. Epub 2017 Jul 3 [PubMed PMID: 28673238]
Level 3 (low-level) evidenceCui Y, Yin S, Qin X, Jiao W, Ren A, Wang F, Zhao B. Advances in the treatment of intraocular malignancies: A literature review. Frontiers in medicine. 2022:9():975565. doi: 10.3389/fmed.2022.975565. Epub 2022 Oct 18 [PubMed PMID: 36330064]
Level 2 (mid-level) evidenceParra-Tanoux D, Dussan-Vargas MP, Escandon MG. Painful-blind eye: A forgotten palliative care. Indian journal of ophthalmology. 2023 Jun:71(6):2399-2408. doi: 10.4103/IJO.IJO_3063_22. Epub [PubMed PMID: 37322649]
Wang T, Moinuddin O, Abuzaitoun R, Hwang M, Besirli C, Wubben TJ, Zacks DN. Retinal Detachment After Endophthalmitis: Risk Factors and Outcomes. Clinical ophthalmology (Auckland, N.Z.). 2021:15():1529-1537. doi: 10.2147/OPTH.S302757. Epub 2021 Apr 13 [PubMed PMID: 33880012]
Shaw GM, Carmichael SL, Yang W, Harris JA, Finnell RH, Lammer EJ. Epidemiologic characteristics of anophthalmia and bilateral microphthalmia among 2.5 million births in California, 1989-1997. American journal of medical genetics. Part A. 2005 Aug 15:137(1):36-40 [PubMed PMID: 16007635]
Clementi M, Tenconi R, Bianchi F, Botto L, Calabro A, Calzolari E, Cianciulli D, Mammi I, Mastroiacovo P, Meli P, Spagnolo A, Turolla L, Volpato S. Congenital eye malformations: a descriptive epidemiologic study in about one million newborns in Italy. Birth defects original article series. 1996:30(1):413-24 [PubMed PMID: 9125347]
Källén B, Robert E, Harris J. The descriptive epidemiology of anophthalmia and microphthalmia. International journal of epidemiology. 1996 Oct:25(5):1009-16 [PubMed PMID: 8921488]
Ruiters S, Mombaerts I. The prevalence of anophthalmic socket syndrome and its relation to patient quality of life. Eye (London, England). 2021 Jul:35(7):1909-1914. doi: 10.1038/s41433-020-01178-2. Epub 2020 Sep 14 [PubMed PMID: 32929179]
Level 2 (mid-level) evidenceFuhrmann S. Eye morphogenesis and patterning of the optic vesicle. Current topics in developmental biology. 2010:93():61-84. doi: 10.1016/B978-0-12-385044-7.00003-5. Epub [PubMed PMID: 20959163]
Morrison D, FitzPatrick D, Hanson I, Williamson K, van Heyningen V, Fleck B, Jones I, Chalmers J, Campbell H. National study of microphthalmia, anophthalmia, and coloboma (MAC) in Scotland: investigation of genetic aetiology. Journal of medical genetics. 2002 Jan:39(1):16-22 [PubMed PMID: 11826019]
Cohen LM, Habib LA, Yoon MK. Post-traumatic enophthalmos secondary to orbital fat atrophy: a volumetric analysis. Orbit (Amsterdam, Netherlands). 2020 Oct:39(5):319-324. doi: 10.1080/01676830.2019.1691607. Epub 2019 Nov 14 [PubMed PMID: 31726012]
Borrelli M, Geerling G. Current concepts of ocular adnexal surgery. GMS Interdisciplinary plastic and reconstructive surgery DGPW. 2013:2():Doc06. doi: 10.3205/iprs000026. Epub 2013 Feb 27 [PubMed PMID: 26504698]
Schmitzer S, Simionescu C, Alexandrescu C, Burcea M. The Anophthalmic Socket - Reconstruction Options. Journal of medicine and life. 2014:7 Spec No. 4(Spec Iss 4):23-9 [PubMed PMID: 27478515]
Coday MP, Warner MA, Jahrling KV, Rubin PA. Acquired monocular vision: functional consequences from the patient's perspective. Ophthalmic plastic and reconstructive surgery. 2002 Jan:18(1):56-63 [PubMed PMID: 11910326]
McBain HB, Ezra DG, Rose GE, Newman SP, Appearance Research Collaboration (ARC). The psychosocial impact of living with an ocular prosthesis. Orbit (Amsterdam, Netherlands). 2014 Feb:33(1):39-44. doi: 10.3109/01676830.2013.851251. Epub 2013 Nov 8 [PubMed PMID: 24205995]
Mashiach R, Vardimon D, Kaplan B, Shalev J, Meizner I. Early sonographic detection of recurrent fetal eye anomalies. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2004 Nov:24(6):640-3 [PubMed PMID: 15517557]
Searle A, Shetty P, Melov SJ, Alahakoon TI. Prenatal diagnosis and implications of microphthalmia and anophthalmia with a review of current ultrasound guidelines: two case reports. Journal of medical case reports. 2018 Aug 29:12(1):250. doi: 10.1186/s13256-018-1746-4. Epub 2018 Aug 29 [PubMed PMID: 30153864]
Level 3 (low-level) evidenceSociety for Maternal-Fetal Medicine, Benacerraf BR, Bromley B, Jelin AC. Anophthalmia and Microphthalmia. American journal of obstetrics and gynecology. 2019 Nov:221(5):B20-B21. doi: 10.1016/j.ajog.2019.08.054. Epub [PubMed PMID: 31679591]
Schittkowski MP, Weiss N. [Ocular prosthetics in children-Possibilities and challenges]. Die Ophthalmologie. 2023 Feb:120(2):139-149. doi: 10.1007/s00347-022-01794-1. Epub 2023 Jan 20 [PubMed PMID: 36662298]
Ragge NK, Subak-Sharpe ID, Collin JR. A practical guide to the management of anophthalmia and microphthalmia. Eye (London, England). 2007 Oct:21(10):1290-300 [PubMed PMID: 17914432]
Soll DB. Anophthalmic socket surgery. International ophthalmology clinics. 1978 Fall:18(3):169-93 [PubMed PMID: 711390]
Thaller VT. Enucleation volume measurement. Ophthalmic plastic and reconstructive surgery. 1997 Mar:13(1):18-20 [PubMed PMID: 9076778]
Rose GE. The giant fornix syndrome: an unrecognized cause of chronic, relapsing, grossly purulent conjunctivitis. Ophthalmology. 2004 Aug:111(8):1539-45 [PubMed PMID: 15288985]
Jordan DR, Brownstein S, Lee-Wing M, Ashenhurst M. Pyogenic granuloma following oculoplastic procedures: an imbalance in angiogenesis regulation? Canadian journal of ophthalmology. Journal canadien d'ophtalmologie. 2001 Aug:36(5):260-8 [PubMed PMID: 11548142]
Srinivasan BD, Jakobiec FA, Iwamoto T, DeVoe AG. Giant papillary conjunctivitis with ocular prostheses. Archives of ophthalmology (Chicago, Ill. : 1960). 1979 May:97(5):892-5 [PubMed PMID: 444123]
Remulla HD, Rubin PA, Shore JW, Sutula FC, Townsend DJ, Woog JJ, Jahrling KV. Complications of porous spherical orbital implants. Ophthalmology. 1995 Apr:102(4):586-93 [PubMed PMID: 7536909]
Stoll C, Alembik Y, Dott B, Roth MP. Epidemiology of congenital eye malformations in 131,760 consecutive births. Ophthalmic paediatrics and genetics. 1992 Sep:13(3):179-86 [PubMed PMID: 1484696]
Warburg M. Classification of microphthalmos and coloboma. Journal of medical genetics. 1993 Aug:30(8):664-9 [PubMed PMID: 8411053]
Weiss AH, Kousseff BG, Ross EA, Longbottom J. Simple microphthalmos. Archives of ophthalmology (Chicago, Ill. : 1960). 1989 Nov:107(11):1625-30 [PubMed PMID: 2818284]
HOWARD GM, KINDER RS, MACMILLAN AS Jr. ORBITAL GROWTH AFTER UNILATERAL ENUCLEATION IN CHILDHOOD. Archives of ophthalmology (Chicago, Ill. : 1960). 1965 Jan:73():80-3 [PubMed PMID: 14220611]
Kennedy RE. Growth retardation and volume determinations of the anophthalmic orbit. Transactions of the American Ophthalmological Society. 1972:70():278-97 [PubMed PMID: 4663670]
Yago K, Furuta M. Orbital growth after unilateral enucleation in infancy without an orbital implant. Japanese journal of ophthalmology. 2001 Nov-Dec:45(6):648-52 [PubMed PMID: 11754910]
Bentley RP, Sgouros S, Natarajan K, Dover MS, Hockley AD. Normal changes in orbital volume during childhood. Journal of neurosurgery. 2002 Apr:96(4):742-6 [PubMed PMID: 11990816]
Fountain TR, Goldberger S, Murphree AL. Orbital development after enucleation in early childhood. Ophthalmic plastic and reconstructive surgery. 1999 Jan:15(1):32-6 [PubMed PMID: 9949427]
Vasquez RJ, Linberg JV. The anophthalmic socket and the prosthetic eye. A clinical and bacteriologic study. Ophthalmic plastic and reconstructive surgery. 1989:5(4):277-80 [PubMed PMID: 2487236]
Pine KR, Sloan B, Jacobs RJ. The development of measurement tools for prosthetic eye research. Clinical & experimental optometry. 2013 Jan:96(1):32-8. doi: 10.1111/j.1444-0938.2012.00754.x. Epub 2012 Jun 6 [PubMed PMID: 22672062]
Pine KR, Sloan BH, Jacobs RJ. A proposed model of the response of the anophthalmic socket to prosthetic eye wear and its application to the management of mucoid discharge. Medical hypotheses. 2013 Aug:81(2):300-5. doi: 10.1016/j.mehy.2013.04.024. Epub 2013 May 6 [PubMed PMID: 23660132]
Plaisancie J, Calvas P, Chassaing N. Genetic Advances in Microphthalmia. Journal of pediatric genetics. 2016 Dec:5(4):184-188 [PubMed PMID: 27895970]
Level 3 (low-level) evidenceGregory-Evans CY, Williams MJ, Halford S, Gregory-Evans K. Ocular coloboma: a reassessment in the age of molecular neuroscience. Journal of medical genetics. 2004 Dec:41(12):881-91 [PubMed PMID: 15591273]
Gundlach KK, Guthoff RF, Hingst VH, Schittkowski MP, Bier UC. Expansion of the socket and orbit for congenital clinical anophthalmia. Plastic and reconstructive surgery. 2005 Oct:116(5):1214-22 [PubMed PMID: 16217460]
Furuta M. Measurement of orbital volume by computed tomography: especially on the growth of the orbit. Japanese journal of ophthalmology. 2001 Nov-Dec:45(6):600-6 [PubMed PMID: 11754901]
Farkas LG, Posnick JC, Hreczko TM, Pron GE. Growth patterns in the orbital region: a morphometric study. The Cleft palate-craniofacial journal : official publication of the American Cleft Palate-Craniofacial Association. 1992 Jul:29(4):315-8 [PubMed PMID: 1643059]
Hou Z, Xian J, Chang Q, Wei W, Li D. Digital evaluation of orbital development after self-inflating hydrogel expansion in Chinese children with congenital microphthalmia. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2016 May:69(5):706-14. doi: 10.1016/j.bjps.2016.01.011. Epub 2016 Jan 19 [PubMed PMID: 26923661]
McLean CJ, Ragge NK, Jones RB, Collin JR. The management of orbital cysts associated with congenital microphthalmos and anophthalmos. The British journal of ophthalmology. 2003 Jul:87(7):860-3 [PubMed PMID: 12812886]
Dutton JJ. Coralline hydroxyapatite as an ocular implant. Ophthalmology. 1991 Mar:98(3):370-7 [PubMed PMID: 1850825]
Blaydon SM, Shepler TR, Neuhaus RW, White WL, Shore JW. The porous polyethylene (Medpor) spherical orbital implant: a retrospective study of 136 cases. Ophthalmic plastic and reconstructive surgery. 2003 Sep:19(5):364-71 [PubMed PMID: 14506421]
Level 2 (mid-level) evidenceMa X, Schou KR, Maloney-Schou M, Harwin FM, Ng JD. The porous polyethylene/bioglass spherical orbital implant: a retrospective study of 170 cases. Ophthalmic plastic and reconstructive surgery. 2011 Jan-Feb:27(1):21-7. doi: 10.1097/IOP.0b013e3181de01a7. Epub [PubMed PMID: 20700071]
Level 2 (mid-level) evidenceMawn LA, Jordan DR, Gilberg S. Proliferation of human fibroblasts in vitro after exposure to orbital implants. Canadian journal of ophthalmology. Journal canadien d'ophtalmologie. 2001 Aug:36(5):245-51 [PubMed PMID: 11548140]
Kaltreider SA. The ideal ocular prosthesis: analysis of prosthetic volume. Ophthalmic plastic and reconstructive surgery. 2000 Sep:16(5):388-92 [PubMed PMID: 11021389]
Kaltreider SA, Lucarelli MJ. A simple algorithm for selection of implant size for enucleation and evisceration: a prospective study. Ophthalmic plastic and reconstructive surgery. 2002 Sep:18(5):336-41 [PubMed PMID: 12352819]
Kowanz DH, Wawer Matos PA, Gordon E, Doulis A, Simon M, Rokohl AC, Heindl LM. [Evisceration, enucleation and exenteration-Indications, techniques, and postoperative care]. Die Ophthalmologie. 2023 Feb:120(2):126-138. doi: 10.1007/s00347-022-01791-4. Epub 2023 Jan 12 [PubMed PMID: 36635593]
Hogeboom CSE, Mourits DL, Ket JCF, Tan HS, Hartong DT, Moll AC. Persistent socket pain postenucleation and post evisceration: a systematic review. Acta ophthalmologica. 2018 Nov:96(7):661-672. doi: 10.1111/aos.13688. Epub 2018 Apr 6 [PubMed PMID: 29633581]
Level 1 (high-level) evidenceCelebi AR, Sasani H. Differentiation of true anophthalmia from clinical anophthalmia using neuroradiological imaging. World journal of radiology. 2014 Jul 28:6(7):515-8. doi: 10.4329/wjr.v6.i7.515. Epub [PubMed PMID: 25071894]
Guthoff R, Klein R, Lieb WE. Congenital cystic eye. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2004 Mar:242(3):268-71 [PubMed PMID: 14676958]
Tripathy K, Chawla R, Temkar S, Sagar P, Kashyap S, Pushker N, Sharma YR. Phthisis Bulbi-a Clinicopathological Perspective. Seminars in ophthalmology. 2018:33(6):788-803. doi: 10.1080/08820538.2018.1477966. Epub 2018 Jun 14 [PubMed PMID: 29902388]
Level 3 (low-level) evidenceRoth FS, Koshy JC, Goldberg JS, Soparkar CN. Pearls of orbital trauma management. Seminars in plastic surgery. 2010 Nov:24(4):398-410. doi: 10.1055/s-0030-1269769. Epub [PubMed PMID: 22550464]
Chaudhry IA, Shamsi FA, Arat YO, Riley FC. Orbital pseudotumor: distinct diagnostic features and management. Middle East African journal of ophthalmology. 2008 Jan:15(1):17-27. doi: 10.4103/0974-9233.53370. Epub [PubMed PMID: 20379424]
Vogele D, Sollmann N, Beck A, Haggenmüller B, Schmidt SA, Schmitz B, Kapapa T, Ozpeynirci Y, Beer M, Kloth C. Orbital Tumors-Clinical, Radiologic and Histopathologic Correlation. Diagnostics (Basel, Switzerland). 2022 Sep 30:12(10):. doi: 10.3390/diagnostics12102376. Epub 2022 Sep 30 [PubMed PMID: 36292065]
Baeg J, Choi HS, Kim C, Kim H, Jang SY. Update on the surgical management of Graves' orbitopathy. Frontiers in endocrinology. 2022:13():1080204. doi: 10.3389/fendo.2022.1080204. Epub 2023 Feb 6 [PubMed PMID: 36824601]
Quaranta-Leoni FM. Treatment of the anophthalmic socket. Current opinion in ophthalmology. 2008 Sep:19(5):422-7. doi: 10.1097/ICU.0b013e32830b1551. Epub [PubMed PMID: 18772676]
Level 3 (low-level) evidenceAlkhairy S, Baig MM, Pasha UA. Unilateral Anophthalmic Socket Reconstruction With Dermis Fat Graft. Cureus. 2021 Oct:13(10):e18834. doi: 10.7759/cureus.18834. Epub 2021 Oct 17 [PubMed PMID: 34804689]
Sethi T, Kheur M, Haylock C, Harianawala H. Fabrication of a custom ocular prosthesis. Middle East African journal of ophthalmology. 2014 Jul-Sep:21(3):271-4. doi: 10.4103/0974-9233.134694. Epub [PubMed PMID: 25100916]
Level 3 (low-level) evidencePippi R. Post-Surgical Clinical Monitoring of Soft Tissue Wound Healing in Periodontal and Implant Surgery. International journal of medical sciences. 2017:14(8):721-728. doi: 10.7150/ijms.19727. Epub 2017 Jul 18 [PubMed PMID: 28824306]
Goiato MC, Zucolotti BC, Mancuso DN, dos Santos DM, Pellizzer EP, Verri FR. Care and cleaning of maxillofacial prostheses. The Journal of craniofacial surgery. 2010 Jul:21(4):1270-3. doi: 10.1097/SCS.0b013e3181e1b431. Epub [PubMed PMID: 20613613]
Chotprasert N, Shrestha B, Thanasapburachot P, Kanpiputana R, Sipiyaruk K. Psychosocial distress and psychological adjustment in patients with ocular loss: a framework analysis. BMC oral health. 2022 Nov 24:22(1):533. doi: 10.1186/s12903-022-02597-1. Epub 2022 Nov 24 [PubMed PMID: 36424616]
O'Keeffe B, Rout S. Prosthetic Rehabilitation in the Lower Limb. Indian journal of plastic surgery : official publication of the Association of Plastic Surgeons of India. 2019 Jan:52(1):134-143. doi: 10.1055/s-0039-1687919. Epub 2019 Apr 29 [PubMed PMID: 31456622]
Clauser L, Sarti E, Dallera V, Galiè M. Integrated reconstructive strategies for treating the anophthalmic orbit. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2004 Oct:32(5):279-90 [PubMed PMID: 15458669]
Coullon GS, Jiang F, Fine I, Watkins KE, Bridge H. Subcortical functional reorganization due to early blindness. Journal of neurophysiology. 2015 Apr 1:113(7):2889-99. doi: 10.1152/jn.01031.2014. Epub 2015 Feb 11 [PubMed PMID: 25673746]
Atkins EJ, Newman NJ, Biousse V. Post-traumatic visual loss. Reviews in neurological diseases. 2008 Spring:5(2):73-81 [PubMed PMID: 18660739]
Galindo-Ferreiro A, AlGhafri L, Elkhamary SM, Maktabi A, Gálvez-Ruiz A, Galindo-Alonso J, Schellini Proff S. Chronic Inflammation in an Anophthalmic Socket due to a Room Temperature Vulcanized Silicone Implant. Case reports in ophthalmology. 2016 Jan-Apr:7(1):216-22. doi: 10.1159/000445496. Epub 2016 Apr 29 [PubMed PMID: 27462246]
Level 3 (low-level) evidenceKumar Ch S, Sajjan CS. Prosthetic management of an ocular defect. Contemporary clinical dentistry. 2010 Jul:1(3):201-3. doi: 10.4103/0976-237X.72795. Epub [PubMed PMID: 22114418]
Bates TJ, Fergason JR, Pierrie SN. Technological Advances in Prosthesis Design and Rehabilitation Following Upper Extremity Limb Loss. Current reviews in musculoskeletal medicine. 2020 Aug:13(4):485-493. doi: 10.1007/s12178-020-09656-6. Epub [PubMed PMID: 32488625]
Level 3 (low-level) evidenceShapira Y, Worrell E, Litwin AS, Malhotra R. The UK National Artificial Eye Questionnaire study: predictors of artificial eye wearers' experience part 1-comfort and satisfaction. Eye (London, England). 2021 Aug:35(8):2233-2240. doi: 10.1038/s41433-020-01236-9. Epub 2020 Oct 26 [PubMed PMID: 33106611]
Rokohl AC, Wall K, Trester M, Wawer Matos PA, Guo Y, Adler W, Pine KR, Heindl LM. Novel point-of-care biomarkers of the dry anophthalmic socket syndrome: tear film osmolarity and matrix metalloproteinase 9 immunoassay. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2023 Mar:261(3):821-831. doi: 10.1007/s00417-022-05895-0. Epub 2022 Nov 11 [PubMed PMID: 36357674]
Anderst W, Fiedler G, Onishi K, McKernan G, Gale T, Paulus P. Within-subject effects of standardized prosthetic socket modifications on physical function and patient-reported outcomes. Trials. 2022 Apr 12:23(1):299. doi: 10.1186/s13063-022-06205-z. Epub 2022 Apr 12 [PubMed PMID: 35413866]
Andreotti AM, Goiato MC, Pellizzer EP, Pesqueira AA, Guiotti AM, Gennari-Filho H, dos Santos DM. Phantom eye syndrome: a review of the literature. TheScientificWorldJournal. 2014:2014():686493. doi: 10.1155/2014/686493. Epub 2014 Dec 7 [PubMed PMID: 25548790]
Rasmussen ML, Ekholm O, Prause JU, Toft PB. Quality of life of eye amputated patients. Acta ophthalmologica. 2012 Aug:90(5):435-40. doi: 10.1111/j.1755-3768.2010.02092.x. Epub 2011 Feb 10 [PubMed PMID: 21310012]
Level 2 (mid-level) evidenceAhn JM, Lee SY, Yoon JS. Health-related quality of life and emotional status of anophthalmic patients in Korea. American journal of ophthalmology. 2010 Jun:149(6):1005-1011.e1. doi: 10.1016/j.ajo.2009.12.036. Epub 2010 Mar 15 [PubMed PMID: 20231012]
Level 2 (mid-level) evidencePine KR, Sloan B, Stewart J, Jacobs RJ. The response of the anophthalmic socket to prosthetic eye wear. Clinical & experimental optometry. 2013 Jul:96(4):388-93. doi: 10.1111/cxo.12004. Epub 2013 Jan 21 [PubMed PMID: 23336714]
Kim JH, Lee MJ, Choung HK, Kim NJ, Hwang SW, Sung MS, Khwarg SI. Conjunctival cytologic features in anophthalmic patients wearing an ocular prosthesis. Ophthalmic plastic and reconstructive surgery. 2008 Jul-Aug:24(4):290-5. doi: 10.1097/IOP.0b013e3181788dff. Epub [PubMed PMID: 18645434]
Jordan DR, Brownstein S, Faraji H. Clinicopathologic analysis of 15 explanted hydroxyapatite implants. Ophthalmic plastic and reconstructive surgery. 2004 Jul:20(4):285-90 [PubMed PMID: 15266142]
Bohman E, Roed Rassmusen ML, Kopp ED. Pain and discomfort in the anophthalmic socket. Current opinion in ophthalmology. 2014 Sep:25(5):455-60. doi: 10.1097/ICU.0000000000000069. Epub [PubMed PMID: 24878963]
Level 3 (low-level) evidenceOwji N, Aslani A. Conjunctival cysts of the orbit after enucleation: the use of trichloroacetic acid. Ophthalmic plastic and reconstructive surgery. 2005 Jul:21(4):264-6 [PubMed PMID: 16052137]
Sánchez EM, Formento NA, Pérez-López M, Jiménez AA. Role of trichloroacetic acid in treating posterior conjunctival cyst in an anopthalmic socket. Orbit (Amsterdam, Netherlands). 2009:28(2-3):101-3 [PubMed PMID: 19839892]
Anderson RL. Tarsal strip procedure for correction of eyelid laxity and canthal malposition in the anophthalmic socket. Ophthalmology. 1981 Sep:88(9):895-903 [PubMed PMID: 7301306]
Smith RJ, Malet T. Auricular cartilage grafting to correct lower conjunctival fornix retraction and eyelid malposition in anophthalmic patients. Ophthalmic plastic and reconstructive surgery. 2008 Jan-Feb:24(1):13-8. doi: 10.1097/IOP.0b013e31815efe35. Epub [PubMed PMID: 18209634]
Kaltreider SA, Shields MD, Hippeard SC, Patrie J. Anophthalmic ptosis: investigation of the mechanisms and statistical analysis. Ophthalmic plastic and reconstructive surgery. 2003 Nov:19(6):421-8 [PubMed PMID: 14625487]
Smit TJ, Koornneef L, Zonneveld FW, Groet E, Otto AJ. Primary and secondary implants in the anophthalmic orbit. Preoperative and postoperative computed tomographic appearance. Ophthalmology. 1991 Jan:98(1):106-10 [PubMed PMID: 2023724]
Custer PL, Maamari RN, Huecker JB, Gordon MO. Eyebrow Position Before and After Enucleation. Ophthalmic plastic and reconstructive surgery. 2022 Sep-Oct 01:38(5):438-443. doi: 10.1097/IOP.0000000000002145. Epub 2022 Mar 21 [PubMed PMID: 36084340]
Custer PL, Maamari RN, Huecker JB, Gordon MO. Volumetric Versus Empirical Determination of Enucleation Implant Size. Ophthalmic plastic and reconstructive surgery. 2021 Sep-Oct 01:37(5):414-419. doi: 10.1097/IOP.0000000000001884. Epub [PubMed PMID: 33237669]
Lee EW, Berbos Z, Zaldivar RA, Lee MS, Harrison AR. Use of DermaMatrix graft in oculoplastic surgery. Ophthalmic plastic and reconstructive surgery. 2010 May-Jun:26(3):153-4. doi: 10.1097/IOP.0b013e3181b8e788. Epub [PubMed PMID: 20489536]
Shorr N, Perry JD, Goldberg RA, Hoenig J, Shorr J. The safety and applications of acellular human dermal allograft in ophthalmic plastic and reconstructive surgery: a preliminary report. Ophthalmic plastic and reconstructive surgery. 2000 May:16(3):223-30 [PubMed PMID: 10826764]
Larned DC. Lacrimal mechanics in the enucleated state. Ophthalmic plastic and reconstructive surgery. 1992:8(3):202-7 [PubMed PMID: 1390428]
Smit TJ, Koornneef L, Mourits MP, Groet E, Otto AJ. Primary versus secondary intraorbital implants. Ophthalmic plastic and reconstructive surgery. 1990:6(2):115-8 [PubMed PMID: 2285660]
Jordan DR. Localization of extraocular muscles during secondary orbital implantation surgery: the tunnel technique: experience in 100 patients. Ophthalmology. 2004 May:111(5):1048-54 [PubMed PMID: 15121387]
Jordan DR, Klapper SR, Gilberg SM, Dutton JJ, Wong A, Mawn L. The bioceramic implant: evaluation of implant exposures in 419 implants. Ophthalmic plastic and reconstructive surgery. 2010 Mar-Apr:26(2):80-2. doi: 10.1097/IOP.0b013e3181b80c30. Epub [PubMed PMID: 20305504]
Cheng MS, Liao SL, Lin LL. Late porous polyethylene implant exposure after motility coupling post placement. American journal of ophthalmology. 2004 Sep:138(3):420-4 [PubMed PMID: 15364224]
Li D, Jie Y, Liu H, Liu J, Zhu Z, Mao C. Reconstruction of anophthalmic orbits and contracted eye sockets with microvascular radial forearm free flaps. Ophthalmic plastic and reconstructive surgery. 2008 Mar-Apr:24(2):94-7. doi: 10.1097/IOP.0b013e318166dad1. Epub [PubMed PMID: 18356711]
Bajaj MS, Pushker N, Singh KK, Chandra M, Ghose S. Evaluation of amniotic membrane grafting in the reconstruction of contracted socket. Ophthalmic plastic and reconstructive surgery. 2006 Mar-Apr:22(2):116-20 [PubMed PMID: 16550056]
El-Khatib HA. Prefabricated temporalis fascia pedicled flap for previously skin-grafted contracted eye socket. Plastic and reconstructive surgery. 2000 Sep:106(3):571-5 [PubMed PMID: 10987462]
Sterker I, Frerich B. [Secondary reconstruction of the eye socket with a free radial forearm flap]. Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2007 Nov:104(11):978-82 [PubMed PMID: 17468873]
Changal N, AlRasheed W, Khandekar R. Ocularists the less known mid eye care professionals and their contribution in eye health care. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2020 Jul-Sep:34(3):195-197. doi: 10.4103/1319-4534.310403. Epub 2021 Feb 27 [PubMed PMID: 34085013]
Wahass SH. The role of psychologists in health care delivery. Journal of family & community medicine. 2005 May:12(2):63-70 [PubMed PMID: 23012077]
Paterick TE, Patel N, Tajik AJ, Chandrasekaran K. Improving health outcomes through patient education and partnerships with patients. Proceedings (Baylor University. Medical Center). 2017 Jan:30(1):112-113 [PubMed PMID: 28152110]
Vardizer Y, Sobeh T, Prat DL, Ben Simon GJ, Tomkins-Netzer O. Assessing the results of anophthalmic prostheses. Indian journal of ophthalmology. 2021 Jul:69(7):1876-1881. doi: 10.4103/ijo.IJO_2682_20. Epub [PubMed PMID: 34146048]
Gupta S, Gupta H, Tandan A. Technical complications of implant-causes and management: A comprehensive review. National journal of maxillofacial surgery. 2015 Jan-Jun:6(1):3-8. doi: 10.4103/0975-5950.168233. Epub [PubMed PMID: 26668445]
Fay A, Nallasamy N, Pemberton JD, Callahan A, Wladis EJ, Nguyen J, Durand ML, New England Oculoplastics Society Study Group. Prophylactic postoperative antibiotics for enucleation and evisceration. Ophthalmic plastic and reconstructive surgery. 2013 Jul-Aug:29(4):281-5. doi: 10.1097/IOP.0b013e3182916674. Epub [PubMed PMID: 23645357]
Mastrangelo F. New Implant Materials. Materials (Basel, Switzerland). 2023 Jun 22:16(13):. doi: 10.3390/ma16134525. Epub 2023 Jun 22 [PubMed PMID: 37444838]
Rokohl AC, Mor JM, Trester M, Koch KR, Heindl LM. [Rehabilitation of Anophthalmic Patients with Prosthetic Eyes in Germany Today - Supply Possibilities, Daily Use, Complications and Psychological Aspects]. Klinische Monatsblatter fur Augenheilkunde. 2019 Jan:236(1):54-62. doi: 10.1055/a-0764-4974. Epub 2018 Dec 19 [PubMed PMID: 30567009]