Introduction
Airway monitoring, as part of a comprehensive physical examination, evaluates a patient's ventilation and gas exchange capacity. This assessment includes examining the airway's condition and interpreting data from adjunct monitors. Although vital for patient care, caution is necessary while analyzing monitor data due to inherent limitations. This review explores various airway monitoring techniques, their functions, and limitations.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
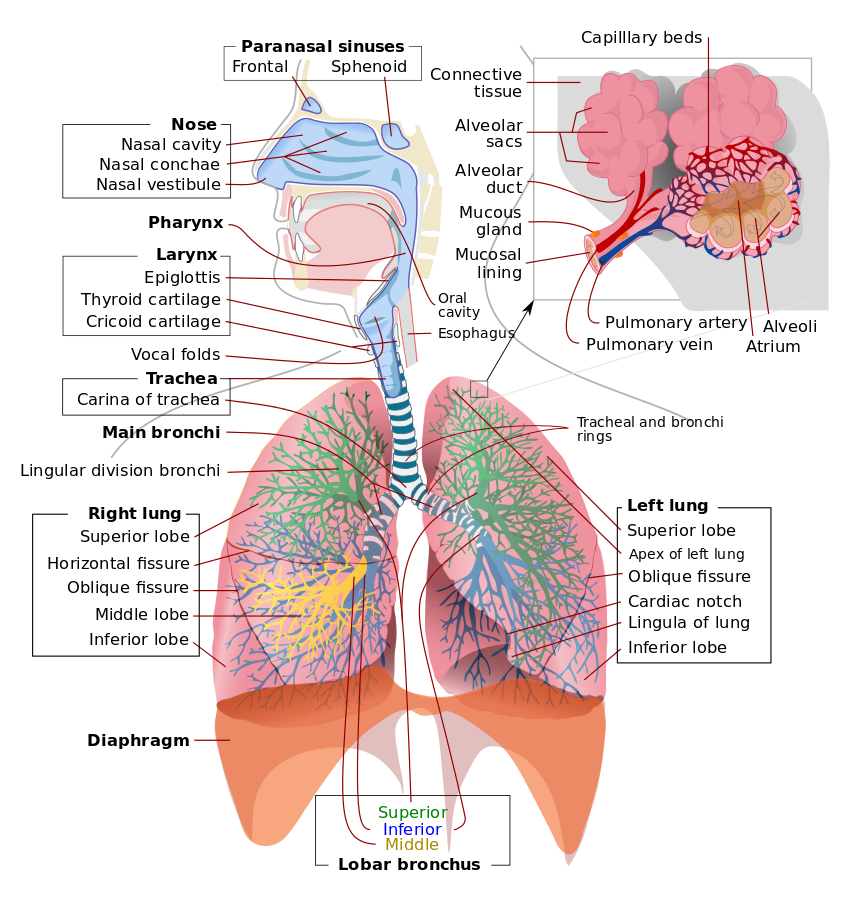
Monitoring a patient in respiratory distress involves gathering both subjective and objective information.[1] A focused history and physical examination offer valuable insights into the patient's airway protection ability. A thorough understanding of airway anatomy aids in conducting a thorough airway examination. The airway can be categorized into 2 parts: the upper airway, encompassing the nasal cavity, oropharynx, and larynx, and the lower airway, starting from the trachea and extending through the bronchus, bronchioles, and alveoli (see Image. Airway and Lung Anatomy).
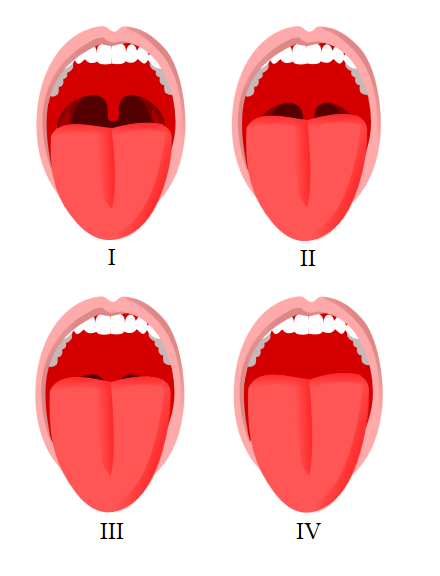
An airway exam should include an assessment of mouth opening, dentition, thyromental distance, neck circumference, Mallampati score (see Image. Mallampati Score Visual), and cervical spine mobility. The mnemonic, LEMON, is often used to evaluate an airway.
- L: Look
- E: Evaluate
- M: Mallampati
- O: Obstruction
- N: Neck mobility
Indicators such as a diminished mouth opening of fewer than 3 fingers, a large neck, a short thyromental distance of fewer than 3 fingerbreadths, Mallampati 3 or 4, or limited neck extension should alert the provider of a possible difficult airway and prompt for proper preparation.[2]
Different airway examination tests can be used; however, their accuracy may vary.[3] Some of the commonly used airway examination tests and their accuracy include the following:[4][5]
-
Mallampati Test: This test is a simple, noninvasive method to predict difficult intubation by evaluating the visibility of the oropharyngeal structures. However, the Mallampati test has limited accuracy, with a sensitivity ranging from 24% to 62% and a specificity of 78% to 82%.
-
Thyromental Distance: The thyromental distance measures the space between the thyroid notch and the mentum (lower jaw). A shorter distance is associated with a difficult airway. The test has a sensitivity of 44% to 55% and a specificity of 85% to 89%.
-
Sternomental Distance: This test measures the distance between the sternal notch and the mentum. A shorter distance suggests a difficult airway. The sensitivity of the sternomental distance test ranges from 50% to 62%, with a specificity of 88% to 89%.
-
Inter-incisor Gap: The inter-incisor gap is the distance between the upper and lower incisors with the mouth fully open. A smaller gap indicates a difficult airway. The test has a sensitivity of 29% to 61% and a specificity of 83% to 85%.
-
Neck Mobility: Limited neck mobility can make airway management more challenging. The test has a sensitivity of 29% to 54% and a specificity of 85% to 89%.
-
Upper Lip Bite Test: The upper lip bite test involves asking the patient to bite their upper lip with their lower incisors. The test has a sensitivity of 68% to 93% and a specificity of 82% to 97%.
Airway ultrasound has a place in assisting in predictions of difficult patient intubations.[6][7]
The most accurate predictor of difficult intubation is an inter-incisor distance of less than 3 cm. Upon intubation, physical exam signs, including fogging/mist in the endotracheal tube (ETT) lumen, chest rise with each breath, and bilateral breath sounds, indicate endotracheal intubation. Although a chest x-ray can help visualize placement, it is not mandatory. Clinical correlation is recommended instead. The most reliable measures of endotracheal intubation are direct visualization during laryngoscopy and persistently elevated end-tidal carbon dioxide (ETCO2).[8]
In addition to the LEMON mnemonic for airway assessment, other factors such as the patient's level of consciousness, respiratory rate, oxygen saturation, and use of accessory muscles can provide valuable information about the patient's airway status. Auscultation of breath sounds can also help identify abnormalities, such as wheezing, stridor, crackles, or diminished breath sounds.[9][10]
Indications
Airway monitors are essential for assessing a patient's physical condition and clinical situation. Indicators that a patient may need a secured airway through endotracheal intubation include symptoms like difficulty speaking, leaning forward in a tripod position, drooling, increased work of breathing, nasal flaring, tachypnea, declining mental status, cyanosis, and increasing demand for FiO2.
Obtaining a thorough medical history and physical examination can be challenging when dealing with unresponsive patients or children. In such cases, healthcare professionals must use alternative methods to assess the patient's airway. Monitoring vital signs and conducting laboratory tests can provide valuable insights and help identify potential respiratory failure.
While arterial blood gas analysis is reliable, it is an invasive procedure. Relying solely on physical examination findings, such as breath sounds, may not accurately confirm endotracheal intubation in patients with preexisting lung conditions. To ensure the proper placement of an endotracheal tube, waveform capnography is the most dependable technique.
Equipment
Capnography is an airway monitoring method applicable in controlled and spontaneously ventilating patients. The amount of infrared light absorbed by carbon dioxide in exhaled gas is measured and reported as a concentration value. Waveform capnography can provide qualitative data via waveform analysis and quantitative data via alveolar end-tidal carbon dioxide (ETCO2).[11] Other forms of capnography, such as colorimetric capnography, can confirm endotracheal intubation in remote, out-of-hospital settings, emergency departments, or intensive care units. Capnography can provide reliable information confirming adequate ventilation and cellular gas exchange.
The waveform shows 4 phases of the respiratory cycle.
- Phase 1: Inspiratory baseline
- Phase 2: Expiratory upstroke
- Phase 3: Expiratory plateau
- Phase 4: Inspiratory downstroke
Predicting catastrophic events is possible by analyzing changes in waveform morphology and amplitude. Elevated levels of ETCO2 could indicate various medical conditions, such as rebreathing, hypoventilation, malignant hyperthermia, sepsis, insufflation from laparoscopic surgery, or bicarbonate administration. Decreases in ETCO2 are found during hyperventilation, hypothermia, low cardiac output states (eg, pulmonary embolism or cardiac arrest), disconnection of the circuit, or accidental extubation. Morphology perturbations such as up-slanting of the expiratory upstroke or prolongation of the plateau phase can be evidence of airway obstruction seen in bronchospasm, asthma, pregnancy, chronic obstructive pulmonary disease (COPD), or a kinked endotracheal tube. Waveform capnography is a crucial monitoring tool for intubated patients, and its interpretation can aid in managing their ventilation.
Capnography has limitations, especially when a patient is not intubated or doesn't have a secure airway. Simply observing a positive return of end-tidal carbon dioxide may or may not confirm the endotracheal placement of the endotracheal tube. However, a sustained ETCO2 level greater than 30 mm Hg for at least 3 breaths can confirm endotracheal placement. It's worth noting that if a patient consumed a bicarbonate solution or carbonated beverage before intubation, this could alter ETCO2 readings. Furthermore, capnography is limited in pulseless patients because it requires cardiac output. However, it can guide chest compressions, where a sudden increase in ETCO2 may suggest a return of spontaneous circulation.
The pulse oximeter is a noninvasive monitor that detects changes in hemoglobin oxygenation saturation and heart rate. Pulse oximetry functions on spectrophotometry and photoplethysmography. Oxyhemoglobin absorbs infrared (IR) light at a wavelength of 940 nm, and deoxyhemoglobin absorbs red (R) light at 660 nm. When oxyhemoglobin absorbs emitted infrared light, it allows red light to be transmitted and received by the photodetector. The red-to-infrared light ratio determines the percentage of hemoglobin oxygen saturation. The pulsations occurring with each heartbeat are recorded as arterial blood and thus provide arterial blood oxygenation.[12]
Although a pulse oximeter can help determine blood oxygen levels, it has some limitations. For example, carboxyhemoglobin resulting from carbon monoxide poisoning can cause falsely elevated oxygen saturation readings since it has the same absorption wavelength as oxyhemoglobin. Methemoglobinemia, which has the same absorption coefficient for red and infrared light (resulting in a 1:1 R/IR ratio), depicts a saturation of approximately 85%. This phenomenon results in a falsely low oxygen saturation when the saturation is greater than 85% and a falsely elevated saturation when the saturation is less than 85%. Other factors affecting the accuracy of oxygen saturation readings include acid-base disorders, severe hypoxemia, dark nail polish, excessive motion, ambient light, low perfusion, hypothermia, increased systemic vascular resistance, profound anemia, methylene blue dye, and malpositioning. It's important to consider these limitations when interpreting pulse oximeter readings.
Capnography has been further studied and developed for various clinical applications recently. The usefulness of capnography as a noninvasive method for monitoring ventilation has been demonstrated in various settings, such as during procedural sedation, in the management of acute respiratory distress syndrome, and in emergency medicine for the early detection of respiratory failure.[13][14][15] Using capnography has also improved patient safety and outcomes by reducing the incidence of adverse events related to hypoventilation and hypoxia.[16]
Recent technological advances have led to new capnography devices that are more portable, user-friendly, and versatile, allowing for broader use in different clinical scenarios.[14] Despite these advances, it is essential to know capnography and pulse oximetry limitations and the factors influencing their accuracy.
Airway monitors are essential tools for identifying the need for airway management and guiding medical professionals in the process. In cases where patients cannot provide their medical history due to an altered mental state or age, alternative methods must be used to assess their airway and respiratory condition.
One alternative method is imaging, such as chest x-ray, ultrasound, and bronchoscopy. These modalities can help identify underlying lung pathologies, airway obstruction, and foreign bodies and provide visual guidance during endotracheal intubation.[17] In particular, point-of-care lung ultrasound (POCUS) has gained popularity recently due to its noninvasive nature, rapid results, and portability, making it an ideal tool for use in emergency settings and intensive care units.[18]
Another way to evaluate the condition of a patient's airway is through constant monitoring of their respiratory parameters. This includes keeping track of their respiratory rate, tidal volume, and minute ventilation with the help of advanced ventilators and monitoring tools. By monitoring these parameters, healthcare providers can quickly detect changes in the patient's respiratory status, enabling them to take timely action and provide appropriate treatment.[19]
In addition to waveform capnography, other noninvasive monitoring tools can provide valuable information about a patient's airway status. For instance, electrical impedance tomography (EIT) is a novel technique that measures regional lung ventilation and perfusion, which can aid in optimizing ventilation strategies and detecting complications such as pneumothorax, atelectasis, or bronchospasm.[20]
In conclusion, capnography is a valuable method for monitoring airway and ventilation in spontaneously breathing and ventilated patients. Its ability to provide real-time information on the patient's ventilation status makes it an essential tool in various clinical settings. While it has limitations, recent technological developments have expanded its applications and improved its usability. Capnography and pulse oximetry can help guide patient management and improve patient safety.
Personnel
All individuals involved in patient care must be able to identify the symptoms of respiratory distress in patients. In such cases, seeking advice from a qualified clinician experienced in airway management is essential, and objective assessments should be conducted. Additionally, in situations where a challenging airway is expected, it is recommended to have video-assisted laryngoscopy as a backup tool. Furthermore, the difficult airway algorithm should be carefully reviewed for all patients who may be difficult to ventilate or intubate.
Technique or Treatment
Understanding transpulmonary pressure is essential in assessing lung stress. It accurately reflects alveolar pressure and serves as a crucial physiological marker. Esophageal manometry, which utilizes esophageal balloon catheters, is used to measure pleural pressure and make necessary ventilator adjustments. However, calibration methods are necessary to account for air volume in the balloon. Clinical applications of esophageal manometry include assessing lung and chest wall compliance, estimating breathing effort for ventilator weaning, detecting upper airway obstruction post-extubation, and identifying patient-ventilator asynchrony.[21]
Clinical trials and meta-analyses suggest that intraoperative quantitative monitoring significantly decreases residual neuromuscular blockade risk and enhances postoperative respiratory outcomes by minimizing adverse events. Consequently, numerous international anesthesia societies endorse using quantitative monitoring when administering neuromuscular blocking agents in perioperative settings.[22]
Capnography, or real-time monitoring of exhaled carbon dioxide (CO2), is a valuable tool for assessing patient health during anesthesia, in emergency departments and critical care units, with end-tidal CO2 concentration being the fundamental measurement. The applications of this technology are varied, including verifying the placement of endotracheal tubes, assessing disease severity and treatment response, and monitoring sleep apnea in outpatient settings. With the progress of technology, smaller sensors have been utilized in different scenarios, such as pre-hospital surroundings and high-performance military planes. These offer possibilities for new applications that can be integrated into breathing masks.[23]
In a difficult airway, the effectiveness of airway nerve blocks compared to airway anesthesia without nerve blocks for awake tracheal intubation (ATI) has been compared. Airway nerve blocks significantly reduced intubation time, improved anesthesia quality, and decreased overall complications. In conclusion, airway nerve blocks provide superior airway anesthesia quality for ATI, offering better intubation conditions and patient satisfaction while reducing complications.[24]
Different surgical conditions require specific ventilation strategies that come with their challenges and considerations. For instance, laparoscopic surgery involving creating a pneumoperitoneum can lead to reduced lung compliance and increased ventilatory pressures due to the diaphragm's cephalad displacement. While prone positioning can benefit the respiratory system, it requires careful airway management to prevent disconnection of the endotracheal tube. One-lung ventilation during thoracic surgery affects ventilation-perfusion matching and requires lung-protective strategies. Jet ventilation is a specialized technique requiring a shared airway or a still chest. It can be performed at low frequencies for laryngeal procedures or at high frequencies for specialized interventions, with considerations for airway pressures and gas exchange. Knowing these ventilation strategies and their implications in various surgical scenarios can enhance patient care and outcomes.[25]
Clinical Significance
Properly monitoring an intubated patient's airway involves considering several variables. The ventilator visually represents a patient's ventilatory mechanics and can detect acute changes. Radiographic imaging can help identify developing lung pathology or diaphragmatic abnormalities. It is crucial to monitor the patient's airway appropriately when weaning them from a ventilator to ensure they can maintain and protect it. Following specific criteria is essential for safe extubation and preventing the need for re-intubation.
Enhancing Healthcare Team Outcomes
Patient-centered care is best achieved through an interprofessional approach with effective communication. The nursing staff and emergency medical services are among the first members of the healthcare team to monitor and assess a patient's airway. Guidelines established by the American College of Surgeons Advanced Trauma Life Support (ATLS) course and the American Heart Association have prioritized airway management when assessing a patient. Prehospital basic airway management for patients at risk for airway compromise ensures the best outcomes in morbidity and mortality when the patient reaches in-hospital care.[26]
Physicians, advanced practitioners, nurse anesthetists, respiratory therapists, nurses, radiologists, and pharmacists all play an essential role in detecting early airway compromise and in the event of an emergency endotracheal intubation. Proper advanced airway management is vital, and an expert skill level is required. Incorrect placement of an advanced airway can cause gastric insufflation, hypoxia resulting in anoxic brain injury, alterations in blood gases and acidosis, ischemia to vital organs, and if not corrected, may cause death.
Proper ventilation is crucial for sustaining life, so a collaborative approach among healthcare professionals is necessary to ensure positive patient outcomes. All healthcare team members should be vigilant in monitoring patients and alert the physician, advanced practice clinician, nurse anesthetist, or respiratory therapist if they suspect respiratory failure. Radiologists can provide valuable information on lung pathology or confirm the correct placement of an endotracheal tube. At the same time, respiratory therapists can identify early signs of deteriorating lung function and patient symptoms. Pharmacists also play a critical role in providing the necessary medications for rapid sequence induction and intubation and guiding clinicians in selecting appropriate drugs to avoid potential complications or drug interactions. If intubation proves to be challenging or unsuccessful, consulting an anesthesiologist or nurse anesthetist in a hospital setting is highly recommended.
Skills
Performing proper airway monitoring is a necessary skill set. Airway monitoring requires diligence, commitment, quality improvement, and compliance with appropriate and proven methods and interventions. Continued medical education, focused review, and training regarding airway monitoring are essential to patient safety.
Strategy
Maintaining continuous closed-loop communication among all members of the perioperative care team regarding the need, technique, and potential management issues associated with airway monitoring is ideal.
Ethics
Before monitoring the airway, obtaining detailed and complete informed consent from the patient or their authorized decision maker is essential if the patient cannot consent. Every team member should communicate concerns regarding the process with the patient and the team. This promotes participation from all stakeholders and facilitates the timely recognition and resolution of potential problems.
Responsibilities
All team members must communicate their concerns, responsibilities, and activities with all other team members contemporaneously and as indicated throughout the perioperative period, based on their professional discretion.
Interprofessional Communication
All team members should respect the free flow of information and concerns among team members without allowing or producing an environment of hostility.
Care Coordination
All interprofessional team members should consider it their duty to neither disrupt the work performed by other team members nor to, through their actions or inaction, create additional issues or increase the workload for other team members.
Media
References
Cammarota G, Simonte R, Longhini F, Spadaro S, Vetrugno L, De Robertis E. Advanced Point-of-care Bedside Monitoring for Acute Respiratory Failure. Anesthesiology. 2023 Mar 1:138(3):317-334. doi: 10.1097/ALN.0000000000004480. Epub [PubMed PMID: 36749422]
Christie J. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. International journal of nursing practice. 2020 Jun:26(3):e12805. doi: 10.1111/ijn.12805. Epub 2020 Feb 9 [PubMed PMID: 32036623]
Roth D, Pace NL, Lee A, Hovhannisyan K, Warenits AM, Arrich J, Herkner H. Bedside tests for predicting difficult airways: an abridged Cochrane diagnostic test accuracy systematic review. Anaesthesia. 2019 Jul:74(7):915-928. doi: 10.1111/anae.14608. Epub 2019 Mar 6 [PubMed PMID: 30843190]
Level 1 (high-level) evidenceLi WX, Wang DD, Li X, Li WX, Han Y, Cai YR. Risk factors for difficult mask ventilation and difficult intubation among patients undergoing pharyngeal and laryngeal surgery. Heliyon. 2023 Mar:9(3):e14408. doi: 10.1016/j.heliyon.2023.e14408. Epub 2023 Mar 6 [PubMed PMID: 36938445]
Bicalho GP, Bessa RC Jr, Cruvinel MGC, Carneiro FS, Castilho JB, Castro CHV. A prospective validation and comparison of three multivariate models for prediction of difficult intubation in adult patients. Brazilian journal of anesthesiology (Elsevier). 2023 Mar-Apr:73(2):153-158. doi: 10.1016/j.bjane.2021.07.028. Epub 2021 Aug 16 [PubMed PMID: 34411628]
Level 1 (high-level) evidenceBenavides-Zora D, Jaramillo MC, Townsley MM, Franco V, González S, Hoyos C, Cerón J, Arias-Botero JH, Sondekoppam RV, Kalagara H. Diagnostic Performance of Airway Ultrasound for the Assessment of Difficult Laryngoscopy: A Systematic Review and Meta-Analysis. Journal of cardiothoracic and vascular anesthesia. 2023 Jul:37(7):1101-1109. doi: 10.1053/j.jvca.2023.02.036. Epub 2023 Mar 2 [PubMed PMID: 37012134]
Level 1 (high-level) evidenceSotoodehnia M, Abbasi N, Bahri RA, Abdollahi A, Baratloo A. Accuracy of airway ultrasound parameters to predict difficult airway using the LEMON criteria as a reference: A cross-sectional diagnostic accuracy study. Turkish journal of emergency medicine. 2023 Jan-Mar:23(1):38-43. doi: 10.4103/2452-2473.366484. Epub 2023 Jan 2 [PubMed PMID: 36818949]
Level 2 (mid-level) evidenceSilvestri S, Ladde JG, Brown JF, Roa JV, Hunter C, Ralls GA, Papa L. Endotracheal tube placement confirmation: 100% sensitivity and specificity with sustained four-phase capnographic waveforms in a cadaveric experimental model. Resuscitation. 2017 Jun:115():192-198. doi: 10.1016/j.resuscitation.2017.01.002. Epub 2017 Jan 19 [PubMed PMID: 28111195]
Karamchandani K, Wheelwright J, Yang AL, Westphal ND, Khanna AK, Myatra SN. Emergency Airway Management Outside the Operating Room: Current Evidence and Management Strategies. Anesthesia and analgesia. 2021 Sep 1:133(3):648-662. doi: 10.1213/ANE.0000000000005644. Epub [PubMed PMID: 34153007]
Dres M, Demoule A. Monitoring diaphragm function in the ICU. Current opinion in critical care. 2020 Feb:26(1):18-25. doi: 10.1097/MCC.0000000000000682. Epub [PubMed PMID: 31876624]
Level 3 (low-level) evidenceBrochard L, Martin GS, Blanch L, Pelosi P, Belda FJ, Jubran A, Gattinoni L, Mancebo J, Ranieri VM, Richard JC, Gommers D, Vieillard-Baron A, Pesenti A, Jaber S, Stenqvist O, Vincent JL. Clinical review: Respiratory monitoring in the ICU - a consensus of 16. Critical care (London, England). 2012 Dec 12:16(2):219. doi: 10.1186/cc11146. Epub 2012 Dec 12 [PubMed PMID: 22546221]
Level 3 (low-level) evidenceNilsson LM. Respiration signals from photoplethysmography. Anesthesia and analgesia. 2013 Oct:117(4):859-865. doi: 10.1213/ANE.0b013e31828098b2. Epub 2013 Feb 28 [PubMed PMID: 23449854]
Level 3 (low-level) evidenceRamsay M. Ventilation Monitoring. Anesthesiology clinics. 2021 Sep:39(3):403-414. doi: 10.1016/j.anclin.2021.03.006. Epub 2021 Jul 1 [PubMed PMID: 34392876]
Olsen F, Suyderhoud JP, Khanna AK. Respiratory monitoring of nonintubated patients in nonoperating room settings: old and new technologies. Current opinion in anaesthesiology. 2022 Aug 1:35(4):521-527. doi: 10.1097/ACO.0000000000001129. Epub 2022 Jul 5 [PubMed PMID: 35788554]
Level 3 (low-level) evidenceScott JB, Kaur R. Monitoring Breathing Frequency, Pattern, and Effort. Respiratory care. 2020 Jun:65(6):793-806. doi: 10.4187/respcare.07439. Epub [PubMed PMID: 32457171]
Parker W, Estrich CG, Abt E, Carrasco-Labra A, Waugh JB, Conway A, Lipman RD, Araujo MWB. Benefits and harms of capnography during procedures involving moderate sedation: A rapid review and meta-analysis. Journal of the American Dental Association (1939). 2018 Jan:149(1):38-50.e2. doi: 10.1016/j.adaj.2017.08.030. Epub [PubMed PMID: 29304910]
Level 1 (high-level) evidenceGottlieb M, Holladay D, Burns KM, Nakitende D, Bailitz J. Ultrasound for airway management: An evidence-based review for the emergency clinician. The American journal of emergency medicine. 2020 May:38(5):1007-1013. doi: 10.1016/j.ajem.2019.12.019. Epub 2019 Dec 11 [PubMed PMID: 31843325]
Fernandez-Vaquero MÁ, Delgado-Cidranes E, Greif R. Next generation in ultrasound imaging to assess upper airway. Brazilian journal of anesthesiology (Elsevier). 2022 Sep-Oct:72(5):673-675. doi: 10.1016/j.bjane.2022.05.008. Epub 2022 Jun 15 [PubMed PMID: 35714713]
Costanzo I, Sen D, Rhein L, Guler U. Respiratory Monitoring: Current State of the Art and Future Roads. IEEE reviews in biomedical engineering. 2022:15():103-121. doi: 10.1109/RBME.2020.3036330. Epub 2022 Jan 21 [PubMed PMID: 33156794]
Yoshida T, Fujino Y. Monitoring the patient for a safe-assisted ventilation. Current opinion in critical care. 2021 Feb 1:27(1):1-5. doi: 10.1097/MCC.0000000000000788. Epub [PubMed PMID: 33278124]
Level 3 (low-level) evidenceShimatani T, Kyogoku M, Ito Y, Takeuchi M, Khemani RG. Fundamental concepts and the latest evidence for esophageal pressure monitoring. Journal of intensive care. 2023 May 22:11(1):22. doi: 10.1186/s40560-023-00671-6. Epub 2023 May 22 [PubMed PMID: 37217973]
Murphy GS, Brull SJ. Quantitative Neuromuscular Monitoring and Postoperative Outcomes: A Narrative Review. Anesthesiology. 2022 Feb 1:136(2):345-361. doi: 10.1097/ALN.0000000000004044. Epub [PubMed PMID: 34813652]
Level 3 (low-level) evidencePleil JD, Christensen LE. Rationale for developing tunable laser spectroscopy (TLS) technology for high resolution real-time carbon dioxide monitoring (capnography) in human breath. Journal of breath research. 2021 Sep 23:15(4):. doi: 10.1088/1752-7163/ac2723. Epub 2021 Sep 23 [PubMed PMID: 34525465]
Zheng J, Du L, Du B, Zhang W, Zhang L, Chen G. Airway nerve blocks for awake tracheal intubation: A meta-analysis of randomized control trials and trial sequential analysis. Journal of clinical anesthesia. 2023 Sep:88():111122. doi: 10.1016/j.jclinane.2023.111122. Epub 2023 Apr 11 [PubMed PMID: 37054484]
Level 1 (high-level) evidenceBalakrishna A, Brunker L, Hughes CG. Anesthesia Machine and New Modes of Ventilation. Advances in anesthesia. 2022 Dec:40(1):167-183. doi: 10.1016/j.aan.2022.07.008. Epub [PubMed PMID: 36333046]
Level 3 (low-level) evidenceLockey DJ, Crewdson K, Lossius HM. Pre-hospital anaesthesia: the same but different. British journal of anaesthesia. 2014 Aug:113(2):211-9. doi: 10.1093/bja/aeu205. Epub [PubMed PMID: 25038153]