Introduction
An auricular hematoma is a blood collection underneath the ear's skin that typically occurs due to blunt trauma (see Image. Auricular Hematoma). If hematoma treatment is delayed or inadequate, cauliflower ear deformity may arise as a complication (see Image. Severe Cauliflower Ear Deformity). Combat sports like wrestling and boxing are the usual causes of auricular hematomas. Diagnostic testing is often unnecessary unless other clinical indications are present, such as hearing loss and neurologic deficits.
Prompt hematoma removal prevents complications such as infection and cauliflower ear deformity. To avoid recurrence, it is recommended to maintain pressure on the treated site for 5 to 7 days. A pinna injury specialist, such as an otolaryngologist or plastic surgeon, may provide recommendations regarding diagnosis, management, and follow-up care.
Outer Ear Histology
The auricle, or external ear pinna, consists of elastic cartilage enveloped by a dense, fiber-filled perichondrium and skin. The pinna's fibrocartilaginous structure contributes to its mechanical support and 3-dimensional shape, forming the helix, antihelix, scapha, concha, triangular fossa, tragus, and antitragus. The lobule is an exception, as it is composed chiefly of fibrofatty tissue (see Image. Auricle Surface Anatomy).
The perichondrium serves crucial functions, providing structural support to maintain the ear's shape and integrity. The poorly vascularized cartilage relies on the perichondrium's blood supply for oxygen and nutrients. This fibrous layer also facilitates cartilage repair and growth, containing cartilage progenitor cells in its inner stratum, and serves as an attachment site for the overlying skin.
Auricular skin contains sparse hairs, sebaceous glands, eccrine sweat glands, and keratinized stratified squamous epithelium. The anterolateral surface lacks subcutaneous tissue and tightly adheres to the underlying perichondrium. The posteromedial part features subcutaneous fat and skeletal muscle. This disparity makes the anterolateral pinna more vulnerable to injury than the posteromedial aspect.[1][2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Auricular hematomas result from blunt ear trauma, often due to shearing impacts rather than direct blows.[3] The condition is commonly seen in athletes engaging unprotected in contact sports like wrestling and rugby, though various other causes exist. In 2020, Dalal et al's study reported that 40% of auricular hematomas in 87 patients resulted from sports injuries, with assaults and falls each accounting for 10%. Self-harm and postoperative cases may give rise to a few auricular hematoma cases.[4]
Helical piercing is also known to cause pinna hematoma and subsequent bacterial infection. Patients with certain systemic conditions, such as relapsing polychondritis and psoriasis, are prone to developing auricular hematomas. Spontaneous auricular hematomas have also been reported in the literature.[5][6] Anticoagulation increases the risk of spontaneous auricular hematoma and blood accumulation after minor trauma. Children with recurrent auricular hematomas, despite lack of involvement in high-risk sporting activities, should undergo evaluation for potential nonaccidental trauma.[7]
Epidemiology
Characterizing auricular hematoma's epidemiology is challenging due to the potential underreporting of patients not seeking medical care. However, a 1989 survey of over 500 US college wrestlers revealed significant differences in hematoma incidence based on the use of headgear. About 52% of individuals who did not use protection were reported to develop auricular hematoma at least once, compared to only 26% of people who used headgear. Additionally, cauliflower ear deformity rates were 10.6% among individuals who used headgear, compared to 26.6% in people who did not use protection. Regrettably, more than 90% of wrestlers wear headgear inconsistently, primarily during competitions, leading to higher hematoma rates during practice, especially without coaches' supervision.[8][9]
A 2020 retrospective study found that 86% of patients with auricular hematoma at a tertiary care medical center were male. A slight predilection for right-sided injuries may also exist, but more data are needed for confirmation.
Pathophysiology
Debate surrounds the typical location of blood accumulation in auricular hematoma, with subcutaneous, subperichondrial, and intracartilaginous sites proposed. A 1975 study by Ohlsén et al demonstrated that blood injected into rabbit ears' subperichondrial space resulted in neocartilage formation, similar to human cauliflower ear evolution, suggesting a subperichondrial location.[10] However, a similar study by Pandya in 1973 found that hematomas tended to form within microfractures of auricular cartilage in rabbits after applying a blunt force, a finding supported by subsequent human and canine studies. While both subperichondrial and intracartilaginous locations may occur, definitive evidence for prevalence is lacking.[11][12]
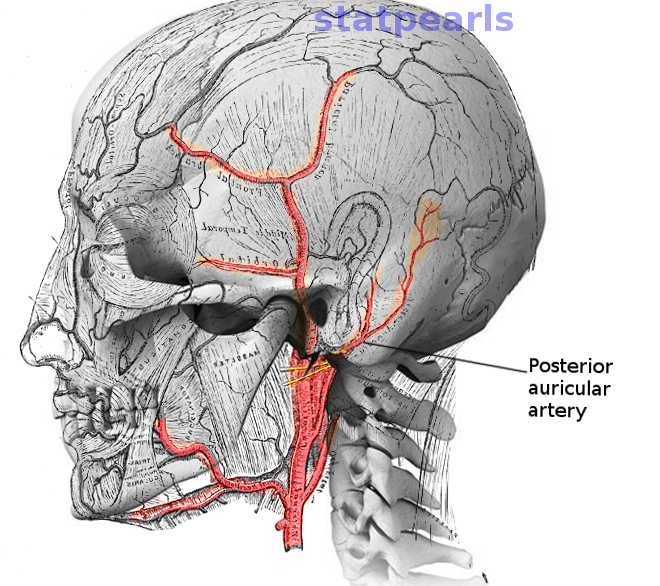
The auricle receives a rich blood supply from 2 carotid artery branches, the superficial temporal and posterior auricular arteries. The latter is the primary source, perfusing the posterior aspect and conchal bowl via branches perforating the cartilage (see Image. Posterior Auricular Artery). The superficial temporal artery supplies most of the anterior surface through its upper, middle, and lower branches. Microvasculature along the antihelix and helical arcade forms an anastomosis between the superficial temporal and posterior auricular arteries and serves as the blood source during auricular hematoma formation.[13]
The posterior pinna has thicker subcutaneous tissue and muscle. Thus, hematomas are more likely to form on the anterior surface, where minimal soft tissue cushioning makes the cartilage vulnerable to trauma. Shearing injuries have been shown to produce more hematomas than trauma perpendicular to the ear. An auricular hematoma can lead to vascular compromise and venous congestion, potentially causing cartilage necrosis. New fibrocartilage deposition by chondroblasts results in the characteristic distortion seen in cauliflower ear deformity.
Histopathology
The clotting cascade typically takes approximately 6 hours to convert a liquid hematoma into a semisolid mass. Thus, aspiration with a large-bore needle is relatively easy during the initial hours postinjury. However, as the clot organizes, incision, drainage, and irrigation become necessary after several hours. The clot begins to break down after several days, returning to a liquid state over about a week, allowing for needle aspiration again. However, pathologic neocartilage formation may start as early as 7 to 10 days postinjury, emphasizing the importance of promptly addressing the hematoma upon presentation.[14]
History and Physical
History
Auricular hematoma typically presents with symptoms such as pain, swelling, tenderness, and paresthesia in the affected ear. Patients may complain of ear fullness or pressure, accompanied by difficulty hearing. The skin over the hematoma may appear red and bruised, with the pinna visibly swollen or distorted. Blood or fluid drainage from the ear canal may occur in severe cases. Associated symptoms, such as headache or dizziness, may also be reported if the hematoma is large or if temporal structures are compressed.
The history should include inquiries about recent auricular trauma, ear pain or tenderness, previous similar episodes, fevers or chills, ear drainage, hearing changes, sudden salty rhinorrhea, or neurological symptoms like headache, loss of consciousness, or cranial neuropathy. Ear injuries during high-risk sports may coincide with closed head or cervical spine trauma.
Systemic conditions like psoriasis, relapsing polychondritis, hypertension, bleeding disorders, and anticoagulation may predispose to auricular hematomas. However, spontaneous cases are significant, accounting for 31% in the 2020 series by Dala et al. Thus, the absence of risk factors in the patient's history does not rule out the diagnosis. Onset timing should be established on history. Auricular hematomas manifest acutely, distinguishing them from keloids or cauliflower ear deformity (see Images. Helical Keloid Scar).
Physical Examination
The physical examination should thoroughly assess the external ear, paying close attention to its baseline anatomy to spot abnormalities. Auricular hematoma signs include ear contour irregularity with swelling, ecchymosis or erythema, and fluctuance over the scaphoid fossa, triangular fossa, antihelix, or concha. Auricular lacerations or abrasions may be noted. Using an otoscope to examine the external ear canal and tympanic membrane is vital, as high-energy blunt trauma may cause temporal bone fractures, often evidenced by external auditory canal laceration and hemotympanum.[15][16]
An auricular pseudocyst typically lacks trauma signs or ecchymosis. However, differentiating auricular pseudocysts or seromas from hematomas is not critical, as treatments for these conditions are similar.[17] Otitis externa, which has more external auditory canal involvement but can also present with significant pinna edema and erythema, should be distinguished from auricular hematomas.[18]
Evaluation
Auricular hematomas are typically diagnosed clinically, following a thorough history and physical examination. However, ultrasonography can provide clarity in uncertain cases with ambiguous findings and a lack of historical information. Computed tomography offers a rapid and reliable assessment of bony integrity if skull or cervical spine injuries are suspected. Magnetic resonance imaging may be needed for traumatic brain injury evaluation. A radiographic examination can identify foreign bodies. Patients on blood thinners should undergo coagulation studies to assess anticoagulation status. Extracting purulent material upon aspiration or drainage warrants Gram staining and culture with sensitivity analysis for appropriate antibiotic coverage. Hearing loss should prompt an audiometry.
Treatment / Management
Depending on severity and patient factors, auricular hematomas may be treated at the bedside or in the operating room. The procedure's risks, benefits, and alternatives must be discussed with the patient, with consent secured and documented before starting the treatment. Needle aspiration may be attempted if the patient presents within 6 hours of hematoma formation and the lesion has a diameter of less than 2 cm. On the other hand, older lesions require incision and drainage for successful treatment. Needle aspiration, incision, and drainage yield similar outcomes if performed correctly.
Clot liquefaction may permit further needle aspiration attempts for lesions untreated after 7 to 10 days. However, neocartilage may have already formed at this point, potentially requiring surgical removal. Patients may also refuse treatment and simply observe the injury if they understand the risks and likely poor cosmetic outcomes of such measures.
The steps involved in treating auricular hematomas are described below.
Preparation
The patient should be placed supine or in lateral decubitus, with the affected auricle facing the clinician. Reverse-Trendelenburg positioning may ease discomfort and reduce edema. Adequate lighting is essential, provided by an overhead examination light or portable headlight. Anesthesia and hemostasis are achieved via lidocaine with epinephrine injection as a circumauricular "diamond" block. Depending on the hematoma's location, this technique may be supplemented by direct infiltration into the conchal bowl.[19]
The auricle and surrounding skin are cleansed afterward with antiseptic agents like povidone iodine or chlorhexidine. Sterile conditions should be maintained. Required supplies include a #11 or #15 blade scalpel, an 18-gauge needle with a 10-cc syringe, a suction canister and tubing with Frazier suction tip, a hemostat, skin forceps, scissors, a needle driver, bolster material, and gauze.[20]
Needle Aspiration
The needle is inserted into the most fluctuant area while traction is applied to the 10-cc plunger, aided by a ring-handled control syringe if required. Blood is then aspirated until the hematoma is fully drained or no more fluid can be obtained. Remaining clots may be treated by a gentle massage and in-and-out needle fanning to disrupt loculations and further reduce the hematoma. Incision and drainage may be necessary if these measures are insufficient. A pressure dressing should be applied before discharging the patient. Notably, postdrainage radiation therapy is being explored for cauliflower ear prevention, with promising results in rabbit models.[21]
Incision and Drainage
Incision and drainage are often warranted after needle aspiration failure, the hematoma has remained for more than 6 hours, or the lesion's diameter exceeds 2 cm. Depending on the hematoma's location, a curvilinear incision may be made along the medial helical margin in the scaphoid fossa or within the conchal bowl. Incisions in concave areas typically result in more aesthetically pleasing outcomes than in convex surfaces. The incision is extended through the skin and soft tissue until the hematoma is reached. The blood collection is then manually expressed or suctioned out.
If purulence is present, a culture should be obtained. The cavity is then irrigated with sterile saline and inspected for hemostasis. Conservative bipolar electrocautery may be used for overt bleeding, but this occurrence is uncommon. Mild oozing, if any, may be managed with pressure or a topical thrombin/gel foam matrix.
Depending on clinical judgment, any remaining clot or hemostatic agent should be cleared before closure, with or without a drain. Closure typically involves a single-layer technique using a running, resorbable suture like 5-0 plain gut. If drainage is necessary, a Penrose (sterile rubber drain) or a small-caliber suction drain may be used. The drain is usually removed within 24 to 48 hours after placement. A pressure dressing may be applied afterward to prevent hematoma reaccumulation.
Recurrent hematomas may require a cartilage window technique, excising a small cartilage section from the scaphoid, triangular fossa, or conchal bowl, depending on the hematoma's location. This technique is often used in dogs but has demonstrated up to 100% effectiveness in preventing hematoma recurrences in humans. The technique eliminates the risk of blood reaccumulation in intracartilaginous and subperichondrial spaces.[22][23]
Pressure Options Posthematoma Evacuation
Various methods exist for applying pressure to the auricle posthematoma drainage to eliminate potential fluid accumulation space. One option is molding dental splinting material to the ear and securing it with a headband. Another is using fibrin glue to unite the perichondrium to the cartilage.[24][25] Through-and-through quilt/mattress suturing with 4-0 plain gut on a Keith needle is another alternative, favored by athletes for its absorbable sutures and lack of required dressing (see Image. Incision and Drainage of an Auricular Hematoma).[26][27](B2)
A traditional approach involves placing cotton dental rolls parallel to the helix on the anterior and posterior aspects of the auricle, secured with 3-0 nylon mattress sutures for compression. Bolster or dressing removal typically occurs after 5 to 7 days, and antibiotic use is at the clinician's discretion. Reconstruction via otoplasty may be necessary if a cauliflower ear deformity develops, which warrants a referral to an otolaryngologist, plastic surgeon, or facial plastic surgeon.
Differential Diagnosis
Infectious, autoimmune, and traumatic sources of auricular swelling must be ruled out. The most important differential diagnoses include hemangioma, cauliflower ear deformity, perichondritis, otitis externa, abscess, pseudocyst, seroma, cellulitis, keloid, Winkler disease (relapsing perichondritis), laceration, erysipelas, sunburn, and skin cancer. These conditions may resemble auricular hematoma but require different evaluation and management strategies.
Complications
Cauliflower ear deformity, an unsightly and inconvenient condition, is the most significant sequela of auricular hematoma. A misshapen ear can cause discomfort while wearing headphones or hearing protection. Earphones and earplugs may no longer fit with conchal bowl involvement. External auditory meatus stenosis may lead to conductive hearing loss and increase the risk of cerumen impaction.
Inadequately treated hematomas heighten the risk of developing a cauliflower ear, especially if recurrence follows initial drainage. Treatment by an otolaryngologist reduces the risk of reaccumulation compared to other specialists or primary care providers (25% compared to 77% reaccumulation rate), with even lower rates (14% compared to 60%) when using a bolster postdrainage. Referral to an otolaryngologist, plastic surgeon, or facial plastic surgeon is recommended for cauliflower ear reconstruction.[28]
Postoperative and Rehabilitation Care
Auricular hematomas may be managed as outpatients. Consultation with an otolaryngologist, plastic surgeon, facial plastic surgeon, or oromaxillofacial surgeon is recommended. Analgesic and antibiotic use depend on the treating clinician's judgment. Drains should be removed within 24 to 48 hours, but the pressure dressing should remain in place for 5 to 7 days. The patient should limit physical activity and avoid contact sports for 10 to 14 days.
Consultations
A surgical referral, specifically to an otolaryngologist, has been shown to decrease the reaccumulation rate of auricular hematomas after initial drainage. An otolaryngologist should also be consulted if concern for associated external, middle, or inner ear pathology remains. Plastic, facial plastic, and oromaxillofacial surgeons are also qualified and equipped to manage auricular hematomas.
Deterrence and Patient Education
The best way to prevent auricular hematomas is to wear protective headgear during activities predisposing to head or ear trauma. Individuals engaging in martial arts and wrestling are advised to wear ear protectors, while specialized helmets are recommended for participants in sports activities like American football, boxing, and skateboarding. Ear protection has reduced the incidence of auricular hematomas in college wrestling to 50%. Applying cold compresses every 15 to 20 minutes may help prevent hematoma formation in cases of unprotected auricular trauma.
If an auricular hematoma occurs, prompt drainage is recommended to prevent blood reaccumulation and reduce the risk of cauliflower ear deformity. Patients should avoid strenuous exercise and contact sports for 10 to 14 days. However, adherence to these restrictions may be challenging for competitive individuals.[29] Tight hypertension control and correction of supratherapeutic anticoagulation are crucial. Applying pressure dressing, such as bolsters sutured to the ear, dental silicone splints, through-and-through absorbable mattress sutures, and magnetic buttons, has decreased the risk of hematoma recurrence by 75%.
Pearls and Other Issues
The most important points to remember when evaluating or managing auricular auricular hematoma are the following:
- History and physical examination are sufficient to diagnose auricular hematoma. Diagnostic testing is warranted if clinical grounds alone cannot lead to a diagnosis or if serious conditions are suspected.
- Needle aspiration or incision and drainage should be performed promptly.
- A pressure dressing should be applied as soon as drainage of the hematoma is complete.
- The most significant complication of auricular hematomas is cauliflower ear deformity.
- After hematoma drainage, patients should be followed up by an otolaryngology, oromaxillofacial, or plastic surgery specialist to prevent recurrence and subsequent cauliflower ear deformity.
Patients should be counseled about the benefits of wearing head and ear protection when engaging in high-risk sports.
Enhancing Healthcare Team Outcomes
Auricular hematomas are commonly encountered in community settings like school sporting events but require multilevel care for proper management. School nurses may initially diagnose the condition, with confirmation by primary care providers or emergency medicine physicians, who may perform immediate aspiration if adequately trained. Surgical specialists handle follow-up to prevent reaccumulation and manage any deformities.
All healthcare team members must understand the importance of timely auricular hematoma identification and drainage and the need to prevent recurrence. Primary care providers and nurses should educate participants in high-risk sports about ear protection. Healthcare providers who encounter auricular abnormalities must adeptly rule out serious conditions like temporal bone fracture, skin cancer, and otitis externa. Collaborative, interprofessional care can improve outcomes for individuals with auricular hematomas or at risk of developing this condition.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)

Incision and Drainage of an Auricular Hematoma. Left: An incision is made along the junction of the helix and the scaphoid fossa. Note the fracture on the helical cartilage. Right: The incision is closed, and the anterior auricular skin flap is reopposed to the cartilage using a 4-0 plain gut quilting suture to eliminate dead space and prevent hematoma recurrence. This technique is an alternative to traditional bolster placement and is better tolerated.
Contribued by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
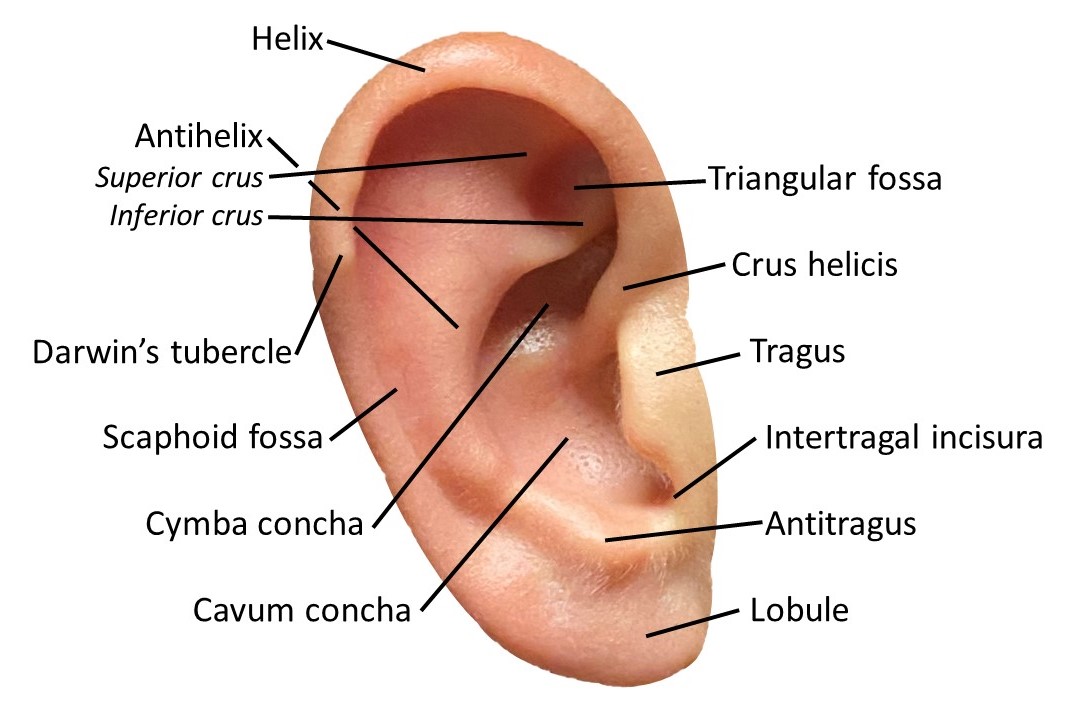
Auricle Surface Anatomy. This image shows the ear auricle's parts, parts, including the helix and its crus, the antihelix and its superior and inferior crura, the Darwin tubercle, triangular and scaphoid fossae, the tragus, conchal cymba and cavum, the intertragal incisura, antitragus, and lobule.
Contributed by MH Hohman, MD, FACS
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Sand M, Sand D, Brors D, Altmeyer P, Mann B, Bechara FG. Cutaneous lesions of the external ear. Head & face medicine. 2008 Feb 8:4():2. doi: 10.1186/1746-160X-4-2. Epub 2008 Feb 8 [PubMed PMID: 18261212]
Zucchelli E, Birchall M, Bulstrode NW, Ferretti P. Modeling Normal and Pathological Ear Cartilage in vitro Using Somatic Stem Cells in Three-Dimensional Culture. Frontiers in cell and developmental biology. 2020:8():666. doi: 10.3389/fcell.2020.00666. Epub 2020 Jul 28 [PubMed PMID: 32850801]
Pandya NJ. Experimental production of "cauliflower ear" in rabbits. Plastic and reconstructive surgery. 1973 Nov:52(5):534-7 [PubMed PMID: 4745576]
Dalal PJ, Purkey MR, Price CPE, Sidle DM. Risk factors for auricular hematoma and recurrence after drainage. The Laryngoscope. 2020 Mar:130(3):628-631. doi: 10.1002/lary.28310. Epub 2019 Oct 17 [PubMed PMID: 31621925]
Shakeel M, Vallamkondu V, Mountain R, Hussain A. Open surgical management of auricular haematoma: incision, evacuation and mattress sutures. The Journal of laryngology and otology. 2015 May:129(5):496-501. doi: 10.1017/S0022215115000249. Epub [PubMed PMID: 25994384]
Mohseni M, Szymanski T. Acute Non-Traumatic Spontaneous Auricular Hematoma. The American journal of case reports. 2019 Feb 16:20():204-206. doi: 10.12659/AJCR.913464. Epub 2019 Feb 16 [PubMed PMID: 30770527]
Level 3 (low-level) evidenceMathur S, Clarke R, John CM. 'Spontaneous' auricular haematoma: a rare differential diagnosis of NAI. Acta paediatrica (Oslo, Norway : 1992). 2009 Jun:98(6):928. doi: 10.1111/j.1651-2227.2009.01296.x. Epub [PubMed PMID: 19469716]
Schuller DE, Dankle SK, Martin M, Strauss RH. Auricular injury and the use of headgear in wrestlers. Archives of otolaryngology--head & neck surgery. 1989 Jun:115(6):714-7 [PubMed PMID: 2719830]
Giffin CS. Wrestler's ear: pathophysiology and treatment. Annals of plastic surgery. 1992 Feb:28(2):131-9 [PubMed PMID: 1567115]
Ohlsén L, Skoog T, Sohn SA. The pathogenesis of cauliflower ear. An experimental study in rabbits. Scandinavian journal of plastic and reconstructive surgery. 1975:9(1):34-9 [PubMed PMID: 1162288]
Level 3 (low-level) evidenceGhanem T, Rasamny JK, Park SS. Rethinking auricular trauma. The Laryngoscope. 2005 Jul:115(7):1251-5 [PubMed PMID: 15995516]
Level 3 (low-level) evidenceDubielzig RR, Wilson JW, Seireg AA. Pathogenesis of canine aural hematomas. Journal of the American Veterinary Medical Association. 1984 Oct 15:185(8):873-5 [PubMed PMID: 6501045]
Blaszczak AM, Abidi N, Pootrakul L, Carr DR. Necrosis of the Ear Following Skin Cancer Resection. Cutis. 2022 Apr:109(4):E2-E5. doi: 10.12788/cutis.0505. Epub [PubMed PMID: 35659849]
Starck WJ, Kaltman SI. Current concepts in the surgical management of traumatic auricular hematoma. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 1992 Aug:50(8):800-2 [PubMed PMID: 1634970]
Patel A, Lofgren DH, Varacallo M. Temporal Fracture. StatPearls. 2023 Jan:(): [PubMed PMID: 30571012]
Ricciardiello F, Mazzone S, Longo G, Russo G, Piccirillo E, Sequino G, Cavaliere M, Accardo N, Oliva F, Salomone P, Perrella M, Zeccolini F, Romano D, Di Maro F, Viola P, Cifali R, Muto F, Galli J. Our Experience on Temporal Bone Fractures: Retrospective Analysis of 141 Cases. Journal of clinical medicine. 2021 Jan 8:10(2):. doi: 10.3390/jcm10020201. Epub 2021 Jan 8 [PubMed PMID: 33429854]
Level 2 (mid-level) evidencePuza C, Nijhawan RI. Treatment of pseudocyst of auricle. Journal of the American Academy of Dermatology. 2023 Dec:89(6):e269-e270. doi: 10.1016/j.jaad.2022.02.010. Epub 2022 Feb 11 [PubMed PMID: 35151761]
Medina-Blasini Y, Sharman T. Otitis Externa. StatPearls. 2024 Jan:(): [PubMed PMID: 32310515]
Kravchik L, Ng M, VanHoy TB. Ear Nerve Block. StatPearls. 2024 Jan:(): [PubMed PMID: 30860741]
Greywoode JD, Pribitkin EA, Krein H. Management of auricular hematoma and the cauliflower ear. Facial plastic surgery : FPS. 2010 Dec:26(6):451-5. doi: 10.1055/s-0030-1267719. Epub 2010 Nov 17 [PubMed PMID: 21086231]
Hwang K, Kim CW, Lee SI, Park IS, Kim WC, Loh JJ. Could ionizing radiation forestall cauliflower ear? Annals of plastic surgery. 2001 Feb:46(2):141-5 [PubMed PMID: 11216608]
Lamb MM, Mims MM, Clark JM. "Hole-Punch" Technique for Recurrent Auricular Hematomas. The Laryngoscope. 2023 Apr:133(4):814-817. doi: 10.1002/lary.30298. Epub 2022 Jul 21 [PubMed PMID: 35861159]
Larsen S. Intrachondral rupture and hematoma formation in the external ear of dogs. Pathologia veterinaria. 1968:5(5):442-50 [PubMed PMID: 5752523]
Choung YH, Park K, Choung PH, Oh JH. Simple compressive method for treatment of auricular haematoma using dental silicone material. The Journal of laryngology and otology. 2005 Jan:119(1):27-31 [PubMed PMID: 15807959]
Mohamad SH, Barnes M, Jones S, Mahendran S. A new technique using fibrin glue in the management of auricular hematoma. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2014 Nov:24(6):e65-7. doi: 10.1097/JSM.0000000000000095. Epub [PubMed PMID: 24699189]
Level 3 (low-level) evidenceGiles WC, Iverson KC, King JD, Hill FC, Woody EA, Bouknight AL. Incision and drainage followed by mattress suture repair of auricular hematoma. The Laryngoscope. 2007 Dec:117(12):2097-9 [PubMed PMID: 17921905]
Level 2 (mid-level) evidenceKakarala K, Kieff DA. Bolsterless management for recurrent auricular hematomata. The Laryngoscope. 2012 Jun:122(6):1235-7. doi: 10.1002/lary.23288. Epub 2012 Mar 22 [PubMed PMID: 22447489]
Patel BC, Hohman MH, Hutchison J, Hatcher JD. Cauliflower Ear. StatPearls. 2025 Jan:(): [PubMed PMID: 29261905]
Schuller DE, Dankle SD, Strauss RH. A technique to treat wrestlers' auricular hematoma without interrupting training or competition. Archives of otolaryngology--head & neck surgery. 1989 Feb:115(2):202-6 [PubMed PMID: 2914091]