Introduction
Extensive burns can cause considerable local damage, tissue injury, and a widespread inflammatory response affecting multiple organ systems.[1] All severely burned patients are trauma patients first, thus should always be handled systematically with an initial focus on the ABCs (airway, breathing, and circulation). After the primary and secondary surveys are completed, early and aggressive fluid resuscitation is initiated.
The fundamental critical elements in burn resuscitation have progressively evolved as more information is unveiled through decades of research. Many formulas and their respective modifications have been modeled to reflect the changes in knowledge. In the 1930s, Frank Pell Underhill reported the fluid within a blister sustained from a burn to be of similar composition to plasma, which led to fluid resuscitation parameters based on patient weight and serum protein levels or hematocrit. Cope and Moore established a relationship between burn size and fluid resuscitation in the 1940s. Initially, plasma was favored as the principal constituent in resuscitation, with the Evan formula advocating for 2 mL per patient weight in kilograms per percentage of total body surface area (TBSA) burned, plus 2 L of intravenous maintenance fluids, half of which consisted of plasma and the other half of normal saline solution. The original Brooke formula continued to use 2 mL per weight in kilograms per percentage of TBSA burn but decreased the plasma requirements to one-fourth of the total fluids administered, and the remainder consisted of Lactated Ringer's solution.[2]
Currently, the Parkland formula is the most frequently used burn resuscitation formula, followed by the Brooke formula.[3] The Parkland formula uses 4 mL per patient weight in kilograms per percentage of TBSA burned with Lactated Ringer's solution as the primary crystalloid solution. However, despite the Parkland formula being the gold standard in burn resuscitation, controversy continues to remain as many studies seek to evaluate the accuracy and feasibility of the Parkland formula in burn resuscitation.[4]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Severe burn injuries trigger a hypermetabolic response with the activation of the complement system and the release of inflammatory and vasoactive mediators. These mediators increase local and systemic capillary permeability, rapidly displacing intravascular fluids, electrolytes, and plasma proteins into the interstitium. The extensive capillary leak results in large fluid shifts, intravascular fluid depletion, and significant burned and non-burned tissue edema. This response can begin within minutes and rapidly transpires over the first 24 hours after the injury: maximum intravascular hypovolemia and edema formation peak at about 8 to 12 hours post-injury.
Massive systemic fluid loss, accompanied by decreased cardiac output and increased vascular resistance, eventually leads to critical hypoperfusion and subsequent tissue injury. This phenomenon, known as “burn shock,” is a combination of distributive, hypovolemia, and cardiogenic shock and is treated with aggressive fluid resuscitation. Fluid management in severe burn injuries aims to maintain tissue perfusion and prevent end-organ ischemia in the earliest phases of burn shock. Prompt and adequate fluid resuscitation has consistently decreased morbidity and mortality in victims of severe burns. This improvement in outcomes has led to the development of many resuscitation protocols that aid in calculating initial fluid requirements.[5][6][1]
Indications
The Parkland formula is an essential tool for calculating fluid resuscitation in patients with critical burns. This formula is indicated for those who have sustained large deep partial-thickness or full-thickness burns covering more than 20% of TBSA in adults and greater than 10% in children. The formula was first tested on large animals by Baxter and Shires before being utilized in human studies. The original version of the formula called for 3.8 mL ± 0.4 mL per weight in kilograms per TBSA burned, with only 12% of patients needing additional fluids for resuscitation. Years after their initial publication, the amount of crystalloid needed was rounded up to 4 mL, and the use of colloid was only recommended within 24 to 48 hours after resuscitation.[3][4]
Contraindications
It is crucial to understand that the Parkland formula is a widely accepted method for burn resuscitation. Although this method has no absolute contraindications, patients with comorbidities like heart failure or end-stage renal disease must be closely monitored regarding their volume status during fluid resuscitation. Patients with smaller burns who can maintain a diet do not require fluid resuscitation.
Preparation
Like with any trauma or critical patient, two large-bore peripheral intravenous catheters should be placed immediately, preferably through unburned skin; intravenous catheters can be placed through burned skin if needed. Peripheral intravenous access is the most efficient and least invasive way to administer high fluid volumes when patients arrive at emergency department rooms.
If peripheral access is unattainable, central venous catheterization or an interosseous line must be considered. A critical yet sometimes forgotten concept is that all burn patients are trauma patients; they may have additional injuries contributing to their presentation. Hypotension is often a late finding in burn shock. If a patient arrives hypotensive, consider other traumatic causes of low blood pressure, such as hemothorax, cardiac tamponade, neurogenic shock, and internal abdominal and pelvic bleeding.
Technique or Treatment
Determining the extent of the injury is crucial in addressing the fluid needs of a burn patient. Therefore, the TBSA affected by the injury is calculated first, but only partial-thickness and full-thickness burns are included; all superficial burns are excluded.
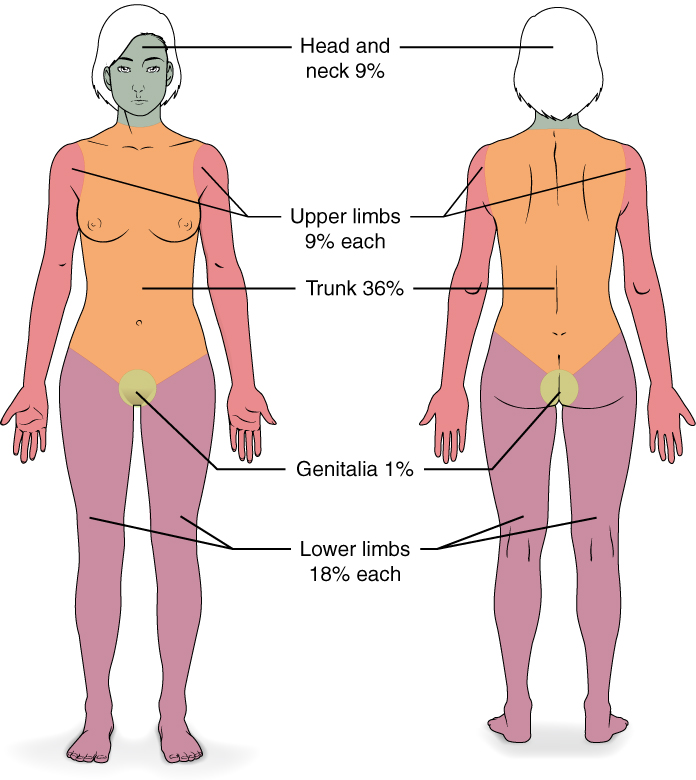
The rule of nines is the most commonly used and quickest method to determine TBSA (Figure 1). The head and circumferential upper extremities are each 9 percent. The anterior and posterior trunks and circumferential lower extremities are each 18 percent. The Lund and Browder Chart should be used for children as this method considers the differences in body proportions with age variations. Moreover, the Lund and Browder approach uses small body area percentages overall, which is why this method is deemed more accurate in determining TBSA.
The rule of palms is a quick and easy approach for estimating TBSA utilizing the patient's palm with the fingers abducted as one percent of their TBSA. This technique is appropriate for smaller TBSA burns.
After the TBSA is calculated and the patient's body weight is determined, the Parkland formula can be implemented to estimate the total fluid requirements for critically burned patients in the first 24 hours after the time of injury and not from the time of evaluation by a provider. The formula recommends 4 mL per kilogram of body weight in adults and 3 mL per kilogram in children per TBSA of crystalloid solution over the first 24 hours of care. In treating burn injury patients, half of the total fluid volume must be administered within the first 8 hours after the burn, with the remaining volume given over the next 16 hours.[7][8][9][10] Children should receive maintenance fluid on top of their calculated fluid requirements, as children are more susceptible to hypoglycemia due to limited glycogen stores.[11] Knowing the time of injury is imperative. In the case of a delayed patient evaluation, the first half of the total fluid amount may need to be administered at a faster rate.
Lactated Ringer solution is the preferred choice of resuscitative crystalloid solution as it effectively treats both hypovolemia and extracellular sodium deficits caused by burn injury. The crystalloid is isotonic, closer in plasma composition than normal saline solution, inexpensive, readily available, and easily stored. Normal saline is typically avoided in large quantities as a resuscitative fluid option in burn patients, as administration can lead to hyperchloremic acidosis.[7][8][9][10] All fluids administered before arrival should be accounted for and subtracted from the amount of fluid administered in the first 8 hours.
Urine output is the most reliable indicator of adequate fluid resuscitation in significant burn patients. Once intravenous access is established and fluids are initiated, a Foley catheter must be inserted to assess urine output accurately. The fluid rate should be adjusted to maintain urine output between 0.5 and 1 mL/kg/h in adults and between 1.0 and 1.5 mL/kg/h in children. Other clinical measures such as heart rate, blood pressure via arterial monitoring, capillary refill time, and mental status can be used to evaluate adequate organ perfusion. If patients with acceptable volume status and urine output remain hypotensive, they may require vasopressors or inotropic agents to improve cardiac output and maintain systemic perfusion pressures.
Though adequate fluid resuscitation is essential during the initial 24 hours after injury, burn patients must remain adequately hydrated throughout their recovery. After 24 hours, the fluid should be switched from Lactated Ringer solution to 5% dextrose in half normal saline (D5½NS) and administered at a maintenance rate using the 4-2-1 rule as a guide. Recent practice guidelines for burn resuscitation consider the supplementation of colloid-containing fluid ranging from the first 8 hours to the first 24 hours post-burn, as it has been shown to decrease overall fluid requirements.[10][7]
Complications
All burn resuscitation formulas are intended to serve as a guide for fluid resuscitation.[12] Recently, there has been some controversy surrounding the accuracy and practicality of the Parkland formula. It is imperative to avoid inadequate resuscitation, which can lead to increased burn depths and mortality from multiple organ failure. However, over-resuscitation can also have severe consequences, such as compartment syndrome, acute respiratory distress syndrome, and multiple organ dysfunction, resulting in fluid creep.[1]
In 2021, Daniels et al sought to determine if the Parkland formula is still the best method for determining adult fluid resuscitation. A retrospective study evaluated 500 patients with more than 20 percent TBSA treated in German burn centers, dividing the patients into groups according to the amount of fluid resuscitation. These authors found that patients who received volume according to the Parkland formula had significant mortality in the first week. Patients who received more fluid had more operations than those with lower administered volumes, and those with lower administered volumes had an increased mortality rate and risk of acute kidney injury. Patients with lower administered volumes were also more likely to be obese.[1]
Mitchell et al also demonstrated that patients with higher resuscitative volumes in the first 24 hours also received more fluids in the following 24 hours with higher mortality rates.[13] Blumetti et al performed a retrospective analysis and revealed that the actual fluid resuscitation volume received infrequently met the calculated amount by the Parkland formula. A majority of the patients received more fluids despite adequate urine output.[4] Similar studies by Cartotto et al and Engrav et al showed more patients receiving higher fluid resuscitation volumes.[14][15] Upon conducting a thorough comparison between the Parkland formula and the modified Brooke formula, which employs a 2 mL instead of a 4 mL calculation, it was noted that there were no notable clinical disparities between the 2 groups. However, it was found that the Parkland formula treatment group experienced fewer ventilator days.[3] Finally, in 2023, the Acute Burn ResUscitation Multicenter Prospective Trial (ABRUPT) revealed more successful volume resuscitation using the Parkland formula in 21 centers.[16][14]
An inaccurate assessment of burn size and depth may result in inadequate fluid resuscitation.[17] Patients who arrive by ground transportation are also at risk of receiving less than predicted required fluids than those transported more promptly by air.[3]
Clinical Significance
Managing the fluid status in burn and trauma patients is a challenging and demanding task. All resuscitative formulas should be used as a starting guide for fluid resuscitation; no formula is comprehensive enough to include the true complexity of burns as there are many unaccounted clinical variables.[3] Furthermore, most studies do not include electrical burns, chemical burns, and multiple trauma patients who traditionally require more resuscitation when calculating the total fluids required. Despite the challenges of one formula being unable to account for the individual intricacies of each burn treated, the Parkland formula is a reasonable starting point for achieving adequate fluid resuscitation despite its limitations.
Enhancing Healthcare Team Outcomes
To ensure the patient receives optimal care, it is absolutely essential that every member of the care team document and communicate all interventions made. This will enable trauma surgery, burn surgery, and emergency department teams to access all the necessary information when the patient arrives at a certified burn center. A team of nurses must be present to assist with Foley and intravenous catheters, while trained personnel will handle central and arterial catheter placement as required. It is crucial to document hourly all administered fluids, vital signs, and urine output, with any significant changes reported to both critical care and burn providers. This regular update schedule must be followed to empower interprofessional teams to make informed decisions and prevent complications related to inappropriate fluid resuscitation.[18][19][20] [Level 1]
Media
(Click Image to Enlarge)
References
Daniels M, Fuchs PC, Lefering R, Grigutsch D, Seyhan H, Limper U, The German Burn Registry, Schiefer JL. Is the Parkland formula still the best method for determining the fluid resuscitation volume in adults for the first 24 hours after injury? - A retrospective analysis of burn patients in Germany. Burns : journal of the International Society for Burn Injuries. 2021 Jun:47(4):914-921. doi: 10.1016/j.burns.2020.10.001. Epub 2020 Oct 17 [PubMed PMID: 33143988]
Level 2 (mid-level) evidenceRomanowski KS, Palmieri TL. Pediatric burn resuscitation: past, present, and future. Burns & trauma. 2017:5():26. doi: 10.1186/s41038-017-0091-y. Epub 2017 Sep 4 [PubMed PMID: 28879205]
Dahl R, Galet C, Lilienthal M, Dwars B, Wibbenmeyer L. Regional Burn Review: Neither Parkland nor Brooke Formulas Reach 85% Accuracy Mark for Burn Resuscitation. Journal of burn care & research : official publication of the American Burn Association. 2023 Apr 3:():. pii: irad047. doi: 10.1093/jbcr/irad047. Epub 2023 Apr 3 [PubMed PMID: 37010149]
Blumetti J, Hunt JL, Arnoldo BD, Parks JK, Purdue GF. The Parkland formula under fire: is the criticism justified? Journal of burn care & research : official publication of the American Burn Association. 2008 Jan-Feb:29(1):180-6. doi: 10.1097/BCR.0b013e31815f5a62. Epub [PubMed PMID: 18182919]
Level 2 (mid-level) evidenceGibran NS, Heimbach DM. Current status of burn wound pathophysiology. Clinics in plastic surgery. 2000 Jan:27(1):11-22 [PubMed PMID: 10665353]
Moore FD. The body-weight burn budget. Basic fluid therapy for the early burn. The Surgical clinics of North America. 1970 Dec:50(6):1249-65 [PubMed PMID: 4922821]
Haberal M, Sakallioglu Abali AE, Karakayali H. Fluid management in major burn injuries. Indian journal of plastic surgery : official publication of the Association of Plastic Surgeons of India. 2010 Sep:43(Suppl):S29-36. doi: 10.4103/0970-0358.70715. Epub [PubMed PMID: 21321653]
Zodda D. Calculated decisions: Parkland formula for burns. Pediatric emergency medicine practice. 2018 Apr 1:15(Suppl 4):1-2 [PubMed PMID: 29617546]
Baxter CR. Fluid volume and electrolyte changes of the early postburn period. Clinics in plastic surgery. 1974 Oct:1(4):693-703 [PubMed PMID: 4609676]
Level 3 (low-level) evidencePham TN, Cancio LC, Gibran NS, American Burn Association. American Burn Association practice guidelines burn shock resuscitation. Journal of burn care & research : official publication of the American Burn Association. 2008 Jan-Feb:29(1):257-66. doi: 10.1097/BCR.0b013e31815f3876. Epub [PubMed PMID: 18182930]
Level 1 (high-level) evidencePalmieri TL. Pediatric Burn Resuscitation. Critical care clinics. 2016 Oct:32(4):547-59. doi: 10.1016/j.ccc.2016.06.004. Epub 2016 Aug 2 [PubMed PMID: 27600126]
Perry V, Teague WJ. Same formula, different philosophy: more mindful use of the Modified Parkland Formula in severe burns. ANZ journal of surgery. 2021 Apr:91(4):490-492. doi: 10.1111/ans.16451. Epub [PubMed PMID: 33847054]
Mitchell KB, Khalil E, Brennan A, Shao H, Rabbitts A, Leahy NE, Yurt RW, Gallagher JJ. New management strategy for fluid resuscitation: quantifying volume in the first 48 hours after burn injury. Journal of burn care & research : official publication of the American Burn Association. 2013 Jan-Feb:34(1):196-202. doi: 10.1097/BCR.0b013e3182700965. Epub [PubMed PMID: 23292589]
Cartotto RC, Innes M, Musgrave MA, Gomez M, Cooper AB. How well does the Parkland formula estimate actual fluid resuscitation volumes? The Journal of burn care & rehabilitation. 2002 Jul-Aug:23(4):258-65 [PubMed PMID: 12142578]
Level 2 (mid-level) evidenceEngrav LH, Colescott PL, Kemalyan N, Heimbach DM, Gibran NS, Solem LD, Dimick AR, Gamelli RL, Lentz CW. A biopsy of the use of the Baxter formula to resuscitate burns or do we do it like Charlie did it? The Journal of burn care & rehabilitation. 2000 Mar-Apr:21(2):91-5 [PubMed PMID: 10752739]
Greenhalgh DG, Cartotto R, Taylor SL, Fine JR, Lewis GM, Smith DJ Jr, Marano MA, Gibson A, Wibbenmeyer LA, Holmes JH, Rizzo JA, Foster KN, Khandelwal A, Fischer S, Hemmila MR, Hill D, Aballay AM, Tredget EE, Goverman J, Phelan H, Jimenez CJ, Baldea A, Sood R. Burn Resuscitation Practices in North America: Results of the Acute Burn ResUscitation Multicenter Prospective Trial (ABRUPT). Annals of surgery. 2023 Mar 1:277(3):512-519. doi: 10.1097/SLA.0000000000005166. Epub 2021 Aug 19 [PubMed PMID: 34417368]
Ete G, Chaturvedi G, Barreto E, Paul M K. Effectiveness of Parkland formula in the estimation of resuscitation fluid volume in adult thermal burns. Chinese journal of traumatology = Zhonghua chuang shang za zhi. 2019 Apr:22(2):113-116. doi: 10.1016/j.cjtee.2019.01.006. Epub 2019 Mar 2 [PubMed PMID: 30962126]
Su L, Kaplan S, Burd R, Winslow C, Hargrove A, Waller M. Trauma resuscitation: can team behaviours in the prearrival period predict resuscitation performance? BMJ simulation & technology enhanced learning. 2017:3(3):106-110. doi: 10.1136/bmjstel-2016-000143. Epub 2017 Jul 6 [PubMed PMID: 35518911]
Carey MG, Valcin EK, Lent D, White M. Nursing Care for the Initial Resuscitation of Burn Patients. Critical care nursing clinics of North America. 2021 Sep:33(3):275-285. doi: 10.1016/j.cnc.2021.05.004. Epub 2021 Jun 16 [PubMed PMID: 34340790]
Alvarado R, Chung KK, Cancio LC, Wolf SE. Burn resuscitation. Burns : journal of the International Society for Burn Injuries. 2009 Feb:35(1):4-14. doi: 10.1016/j.burns.2008.03.008. Epub 2008 Jun 9 [PubMed PMID: 18539396]