Introduction
Ocular astigmatism accounts for 13% of the total refractive errors encountered in patients.[1] The first treatment of astigmatism dates back to 1825, when George Airy used cylindrical lenses to correct his own refractive error.[2] Uncorrected ocular astigmatism results in a blurred image and significant deterioration of visual acuity.[3]
The cause of astigmatism is still not known; several etiologies, including genetics, the pressure of eyelids over the globe, tension due to extraocular muscles, and visual feedback mechanisms, have been attributed.[4] Total ocular astigmatism is considered to be a sum of corneal astigmatism which is contributed by the corneal surface changes, and internal or residual astigmatism, which is contributed by the irregularities of the crystalline lens. The anterior and posterior corneal curvatures contribute to the total corneal astigmatism.[5]
Initially, the estimation of corneal astigmatism was based on the measurement of anterior corneal curvature by keratometry and videokeratography. The calculation of the refractive power was based on empirical estimation of the posterior corneal surface.[6] With advanced imaging technologies like Scheimpflug imaging, Purkinje images-based technologies, and optical coherence tomography, the measurement of the posterior corneal surface has helped us aim for better refractive outcomes in cataract surgery. Posterior corneal astigmatism was evaluated to range from -0.26 to -0. 78 D.[7][8]
Modern-day cataract surgery has emerged as a refractive procedure that aims to eliminate spherical and cylindrical power and achieve spectacle independence.[9] The prevalence of corneal astigmatism >1.00D is 40%, greater than 1.50D was 20% in patients, and >2. 00 D was found in 8% of patients with corneal astigmatism undergoing cataract surgery.[10][11]
The various methods of correcting corneal astigmatism during cataract surgery include toric intraocular lenses (IOL), the placement of the clear corneal phacoemulsification incision on the steeper corneal axis, paired opposite clear corneal incisions over the steeper meridian, and limbal relaxing incisions over the steeper meridians.[12]
Toric IOLs are considered the most predictable way of correcting corneal astigmatism.[13] Shimizu et al introduced toric IOLs 1992 as a rigid 3-piece polymethylmethacrylate lens.[14] The toric IOLs have undergone multiple improvements since then to address stability and postoperative alignment issues.
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
Toric IOLs are ideal for candidates with preexisting corneal astigmatism greater than 1 D.
- Age-related cataracts with corneal astigmatism: Toric IOLs are indicated in patients with preexisting corneal astigmatism of >1.00 D and a significant grade of cataract planned for cataract surgery.[15] Patients who desire spectacle-free near vision can be counseled for multifocal toric IOLs.
- Corneal ectatic disorders: Patients with mild-to-moderate grades of keratoconus and other ectasias with regular astigmatism, which has been stable over time, are also suitable candidates. Off-label use of customized IOLs may also benefit patients with irregular astigmatism but should be prescribed only after assessing patient expectations.[16][17]
- In patients who have undergone penetrating keratoplasty and who have high levels of irregular astigmatism and stable keratometry post-suture removal, customized or conventional toric IOLs can be implanted.[18]
- They may also be used in patients with stable astigmatism due to corneal scars following healed corneal ulcers, pterygium excision, and corneal tear repairs.[19]
Contraindications
For patients with preexisting zonulopathy due to various congenital and acquired causes and zonular strength is a prerequisite for IOL stability.
Corneal scars and irregular astigmatism are relative contraindications for the placement of toric IOLs. They may not be relieved of astigmatism completely, but the magnitude of astigmatism may be reduced and may be taken up after adequate counseling depending on patient expectations.[20]
Poorly dilating pupils may hamper visualization for adequate alignment.
Patients with preexisting retinal pathologies and who have undergone vitreoretinal surgical procedures may not be suitable candidates as their visual outcomes may be compromised due to the retinal pathologies.[21] Patients with uveitic pathologies, glaucoma, and patients who have undergone glaucoma surgeries may not achieve good visual outcomes by their primary pathologies.
Intraoperative posterior capsular rent is a relative contraindication as it may lead to IOL decentration or tilt in the postoperative period.
Patients with unrealistic visual expectations.
Equipment
This table summarises the types of equipment required to perform various steps to implant a toric IOL.
|
Computing total corneal astigmatism |
Schiempflug imaging devices, scanning slit devices, anterior segment optical coherence tomography, and ray tracing devices[22][23][24] |
| Spherical power calculation | Optical biometry devices like IOL master or Lenstar individually compute keratometry using manual keratometers and axial length measurement using A scan or B scan.[25][26] |
| Pre-planning of incision and IOL alignment | Online toric calculators help plan the IOL alignment and incision planning. Various available calculators include the Barret calculator, Alcon, and AMO toric IOL calculator. Apart from the values mentioned above, they also consider the surgically induced astigmatism values, which are unique for each surgeon and calculated using the SIA calculator.[27][28] |
| Pre-operative axis marking |
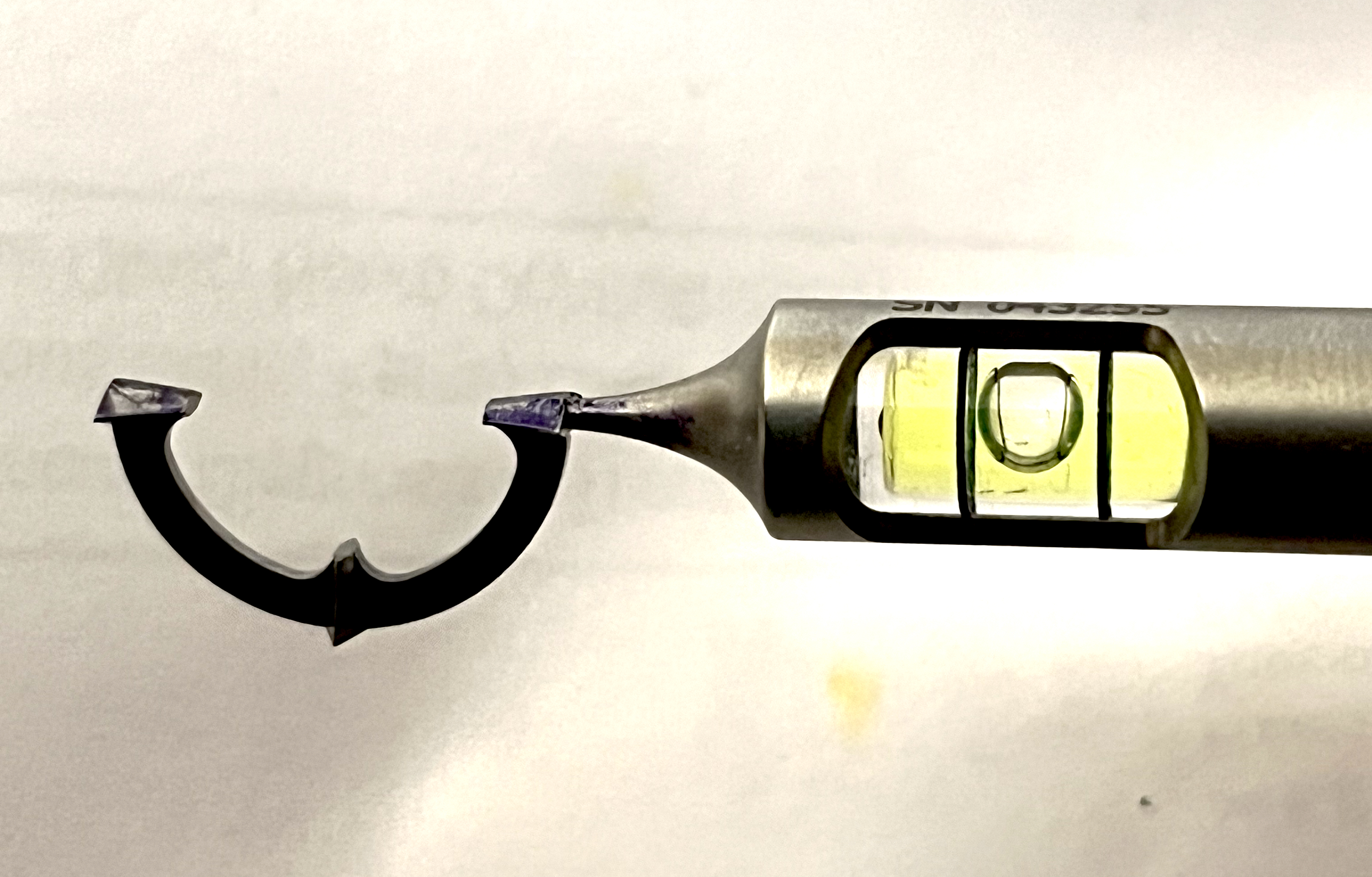
Manual Reference marking: Weighted thread, Geuder-Gerten pendulum marker, Nuijts-Solomon bubble marker, or tonometer marker[29][12]
|
| Intra-operative alignment of IOLs |
Manual Marking Intraoperative axis marking: Mendez gauge, beveled degree gauge[30] Marking of the desired axis: Nuijts Solomon bubble marker, Cionni toric marker[31] FLACS guided marking A Femtosecond laser can mark the axis in patients undergoing FLACS.[32] Image-guided marking systems Various image-guided marking systems like Verion, iTrace, true guide, Callisto, and Z aligns.[33][34] |
| Phacoemulsification/ FLACS for implanting IOL | A peristaltic or venturi-based phacoemulsification machine is used to perform the surgery. In the case of FLACS, a femtosecond laser system for making the incisions, capsulorhexis, and segmentation of the nucleus. |
Toric IOL design
They are single-piece hydrophobic acrylic IOLs with dot or line axis markings on their posterior surface. These markings indicate the flatter axis and must be aligned with the pre-operative markings. They are more stable when compared with silicone IOLs.[35]
With greater than 5-degree misalignment seen in only 6.9% of the cases. Silicone IOLs with C-shaped haptics had a rotation in an anticlockwise direction within two weeks of the postoperative period.[36][37] They can correct astigmatism from 1.00 D to 6.00 D, and IOLs are customized to correct higher astigmatism. Silicone plat haptic IOLs are also available. Toric IOLs can be monofocal, multifocal, extended depth of focus, and phakic toric IOLs.[38][39][40][41]
Personnel
Trained optometrists are required to perform pre-operative workup of the patient, including measurement of uncorrected and best-corrected visual acuity, refraction, and ocular biometry, including axial length and keratometry values. An anesthetic evaluation is required to assess the patient's fitness for the planned procedure.
The surgery is generally performed under local anesthesia, but anxious patients may require sedation to complete the procedure. Patients with systemic medical conditions like cardiac and neurological pathologies may require monitoring throughout the surgery.
An ophthalmologist usually performs standard phacoemulsification or a femtosecond laser-assisted cataract surgery (FLACS) to implant the intraocular lens. A skilled operating theatre assistant usually assists while performing the surgery. The ward nurses or the ophthalmologist can do postoperative care and counseling.
Preparation
Patient Selection
The patient should be thoroughly evaluated clinically to grade the cataract assess pupillary dilatation and tear film status, and rule out significant anterior and posterior segment disorders. Any dry eye or ocular surface disorders should be addressed adequately before cataract surgery. The patient is clearly explained about the surgical procedure and what to expect on the day of surgery. Informed written consent is obtained from the patient.
Steps in Preparing For Toric IOL Implantation
- Computing total corneal astigmatism
- Spherical power calculation
- Pre-planning of incision and IOL alignment
- Phacoemulsification/ FLACS for implanting IOL
- Post-surgical care
Computing Total Corneal Astigmatism
Preoperative estimation of anterior and posterior corneal astigmatism is essential to calculate the IOL power. It can be calculated using one of the abovementioned devices or the Baylor toric nomogram to estimate corneal astigmatism.[42]
Spherical Power Calculation
Intraocular lens power calculation should consider the posterior corneal curvature, effective lens position, and surgically induced astigmatism.[43] Axial length measurement is undertaken using ultrasonic or optical measurement systems. Keratometry to assess the corneal curvatures and astigmatism can be done using manual and automated keratometry. They may include slit scanning systems, optical coherence tomography-based systems, Scheimpflug imaging systems, Placido-based topographers, and an aberrometer. The various measurements are done on two different devices with different principles, and results cross verified for accuracy. Intraoperative wavefront aberrometry rapidly replaces all these calculators to determine the power and axis.
The Barrett toric calculator has better predictability since it considers both estimated lens position and posterior corneal power.[44][45]
Pre-Planning of Incision and IOL Alignment
Axis marking is essential to implant the toric IOLs in the desired axis and achieve optimal visual outcomes. It helps in planning the incision and in the intraoperative alignment of the IOL. The marking can be done manually or using advanced technologies like intra-operative marking systems and intraoperative aberrometry-based methods. Various online calculators and formulae are available for calculating the IOL power and axis of implantation. They include AcrySof online toric calculator, iTRACE calculator, TECNIS calculator, and the Hollday formula.
Various commercial brands of toric IOLs are available, and a choice of a particular IOL depends on availability, financial considerations, and surgeon preference refraction. The IOL with the least amount of residual astigmatism is chosen. Overcorrection of corneal astigmatism leads to postoperative residual astigmatism acting in an axis perpendicular to the preoperatively measured axis, termed as flipping of the axis.[46] Preoperative reference marking of 0 and 180 degrees is done before the patient is shifted to the operating table using manual marking, slit lamp marking, bubble, or a pendulum marker.[31][47][48]
Technique or Treatment
Steps of IOL Implantation
1. Anaesthesia
The patient can be operated on under topical, sub-tenon or peribulbar anesthesia, depending on the patient's and the surgeon's comfort.
2. Intra-operative axis alignment and toric axis marking
Manual Marking
This 3-step technique consists of preoperative reference marking by free hand marking, slit lamp, or a Nuijt-Solomon bubble marker. This is done preoperatively under topical anesthesia. The ocular surface should be dry and excess drops or tear fluid should be removed. Primary gaze in a sitting position is preferred as a change in position from lying down to sitting can cause significant cyclotorsion. The second step is the intra-operative alignment of the horizontal axis using a Mendez gauge. The third step is the intraoperative marking of the desired axis, along which the IOL markings should be aligned.
FLACS Assisted Marking
It aids in making two markings 180 degrees apart in the steep axis. The advantages included avoidance of parallax error found with manual markings and aiding in making astigmatically neutral arcuate incisions.[49]
Image-guided Marking
Various image-guided systems are available to overcome the disadvantages associated with the manual marking of the axis. These images capture high-resolution images of the iris architecture, iris, and limbal vessels, which serve as landmarks to plan the incisions intraoperatively. They help plan the location of clear corneal incisions, limbal relaxing incisions, and capsulorhexis. They may also help optimize the results based on the individual surgeon’s surgically induced astigmatism (SIA).
Placido disc-based topography with ray tracing aberrometer may provide power maps, corneal curvatures, and internal, corneal, and total higher-order aberrations. Considering the SIA, they have an inbuilt toric IOL power calculator that guides the incision placement.[50]
3. Wound Construction
Clear corneal incisions that do not leak and are self-sealing are placed in astigmatically neutral sites, and their placement may be guided by the systems mentioned above.
4. Capsulorhexis
Adequate-sized continuous curvilinear capsulorhexis covering 0.5 mm of the edges is essential to prevent postoperative rotation. A centered round rhexis is required for ideal IOL positioning. A large rhexis may lead to instability of IOL.
5. Removal of Lens Material
The lens material is removed by phacoemulsification, and cortex wash is done. Thorough polishing of the capsule is done to prevent posterior capsular opacification, which may cause IOL tilt and visual discomfort to the patient.
6. IOL Implantation
A cohesive viscoelastic is preferred over a dispersive viscoelastic to inflate the bag for IOL implantation, considering the ease of removal. The IOL is implanted into the bag with the axis markings left around 3 to 5 degrees anticlockwise to the final lens position.
If the patient is operated on under topical anesthesia, they are asked to fix at the microscope light, and the IOL is perfectly centered based on the first Purkinje image. The viscoelastic is removed completely from the anterior chamber and behind the IOL in the bag, and the wound is hydrated before the final rotation of the IOL is made to align with the axis. Intraoperative aberrometry is advantageous in estimating the residual astigmatism of the eye and adjusting the IOL position intraoperatively.
7. Postoperative Care
The patient is asked to maintain a supine position an hour after surgery to avoid changes in the IOL position. The postoperative IOL alignment can be confirmed by refraction, dilated examination to look for the IOL axis, keratometry, and ray tracing aberrometer. Postoperative steroids are prescribed in tapering doses.
Complications
The complication unique to toric IOL implantation is IOL misalignment. IOL alignment is influenced by various factors, including marking technique, capsulorhexis size, coverage of IOL edge by rhexis margins, corneal incision sealing at the end of the surgery, rotational stability of IOL, and surgeon experience.
IOL misalignment may occur secondary to either incorrect calculation of the IOL axis, incorrect placement of the IOL intraoperatively, or due to postoperative rotation. When the misalignment exceeds 30 degrees, it may induce a cylindrical power in a new meridian. One degree of misalignment leads to a 3% loss of effective power, and 30 degrees of misalignment results in the loss of the entire toric effect with significantly worse visual acuity.[51][52]
Postoperative IOL rotation may occur as early as one hour to up to ten days post-surgery. Incomplete removal of the viscoelastic from the bag results in early postoperative rotation, and late postoperative rotations may occur due to IOL design, rhexis extension, large bag size, axial length, and inadequate coverage of IOL by the rhexis margins. With-the-rule astigmatisms were associated with a higher rate of postoperative rotations.[53]
Realignment of the IOL has to be considered in cases with more than 10 degrees of malalignment. An intraoperative marking indicates the new target axis in relation to the current misaligned axis. A side port incision is made, and a long cannula is mounted on a syringe filled with the balanced salt solution is used to rotate the IOL to the desired position.[54] Corneal ablative procedures, piggyback IOLs, and IOL exchange procedures are required for higher degrees of astigmatism not amenable to rotation alone.
The complications inherent to routine phacoemulsification may be encountered while or after the surgery for implanting toric IOLs.
Intraoperative Complications
- Corneal wounds, burns, leaky corneal wounds
- Iris prolapse, iris chaffing by the phacoemulsification probe
- Smaller rhexis, large rhexis, rhexis margin run out
- Posterior capsular rent
- The nucleus or cortical matter drops into the vitreous
- Intraoperative zonular dialysis
- Suprachoroidal hemorrhage
Postoperative Complications
Early
- Corneal edema, striate keratopathy
- Raised intraocular pressure
- Ocular hypotony due to wound leak
- Toxic anterior segment syndrome
- Hyphaema
- Residual lens material
- Refractive surprise
Late
- Posterior capsular opacification
- Cystoid macular edema
- Endophthalmitis
- Retinal detachment
- Subluxation/ dislocation of intraocular lens
- Corneal decompensation/ bullous keratopathy
- Recurrent uveitis
Clinical Significance
Toric IOLs result in better patient satisfaction, and uncorrected visual acuity of 20/40 or better is achieved in most patients.[55][56][57]
Appropriate pre-operative workups for patient selection, intraoperative IOL alignment, and incidence of intraoperative and postoperative complications determine the outcomes of post-toric IOL implantation. The facilitation of posterior corneal power measurement by newer investigations has made estimations of both anterior and posterior corneal curvature possible. Femtosecond laser-assisted cataract surgery, when combined with implantation of toric IOLs, may significantly reduce higher-order aberrations and superior visual outcomes.[58]
Newer advanced toric IOLs have better stability limiting postoperative rotation and predictable visual outcomes. They may have an extended spectrum of indications like irregular astigmatism, higher corneal astigmatisms, post keratoplasty, and corneal ectatic cases.
Enhancing Healthcare Team Outcomes
A coordinated interprofessional team approach is essential for ensuring optimum outcomes with toric IOL implantation. The optometrist evaluates the best-corrected spectacle refraction and performs corneal topography and optical biometry required for IOL power and axis calculation.
They upload the patient's values in online toric IOL calculators and generate patient reports pre-operatively which helps in deciding the axis of implantation and the planning of incisions. The operating theatre personnel ensures the appropriate IOL and other instruments required for the pre-operative marking and performing phacoemulsification. An ophthalmologist/ optometrist or trained personnel can perform the pre-operative axis marking on the patient.
A trained ophthalmologist performs the surgery under peribulbar/sub-tenon/ topical anesthesia. An anesthetist may be required to monitor the patient intraoperatively in patients with systemic ailments and in anxious or uncooperative patients to provide intravenous sedation.
The postoperative care of the patient is taken care of by the ward nurses who counsel the patient regarding the dosage and the procedure of administration of topical medications and other postoperative instructions. The optometrist and ophthalmologist can do the postoperative follow-up of patients at routine intervals.
Media
References
Porter J, Guirao A, Cox IG, Williams DR. Monochromatic aberrations of the human eye in a large population. Journal of the Optical Society of America. A, Optics, image science, and vision. 2001 Aug:18(8):1793-803 [PubMed PMID: 11488483]
Read SA, Collins MJ, Carney LG. A review of astigmatism and its possible genesis. Clinical & experimental optometry. 2007 Jan:90(1):5-19 [PubMed PMID: 17177660]
Level 3 (low-level) evidenceSaw SM, Goh PP, Cheng A, Shankar A, Tan DT, Ellwein LB. Ethnicity-specific prevalences of refractive errors vary in Asian children in neighbouring Malaysia and Singapore. The British journal of ophthalmology. 2006 Oct:90(10):1230-5 [PubMed PMID: 16809384]
Namba H, Sugano A, Murakami T, Utsunomiya H, Nishitsuka K, Ishizawa K, Kayama T, Yamashita H. Age-Related Changes in Astigmatism and Potential Causes. Cornea. 2020 Nov:39 Suppl 1():S34-S38. doi: 10.1097/ICO.0000000000002507. Epub [PubMed PMID: 33038156]
Koch DD, Ali SF, Weikert MP, Shirayama M, Jenkins R, Wang L. Contribution of posterior corneal astigmatism to total corneal astigmatism. Journal of cataract and refractive surgery. 2012 Dec:38(12):2080-7. doi: 10.1016/j.jcrs.2012.08.036. Epub 2012 Oct 12 [PubMed PMID: 23069271]
Level 3 (low-level) evidenceKohnen T. Posterior corneal astigmatism. Journal of cataract and refractive surgery. 2013 Dec:39(12):1795. doi: 10.1016/j.jcrs.2013.10.017. Epub [PubMed PMID: 24286837]
Royston JM, Dunne MC, Barnes DA. Measurement of posterior corneal surface toricity. Optometry and vision science : official publication of the American Academy of Optometry. 1990 Oct:67(10):757-63 [PubMed PMID: 2247298]
Módis L Jr, Langenbucher A, Seitz B. Evaluation of normal corneas using the scanning-slit topography/pachymetry system. Cornea. 2004 Oct:23(7):689-94 [PubMed PMID: 15448494]
Amesbury EC, Miller KM. Correction of astigmatism at the time of cataract surgery. Current opinion in ophthalmology. 2009 Jan:20(1):19-24. doi: 10.1097/ICU.0b013e328319c27a. Epub [PubMed PMID: 19077825]
Level 3 (low-level) evidenceMohammadi M, Naderan M, Pahlevani R, Jahanrad A. Prevalence of corneal astigmatism before cataract surgery. International ophthalmology. 2016 Dec:36(6):807-817 [PubMed PMID: 26909501]
Arriola-Villalobos P, Burgos-Blasco B, Fernández-Vigo JI, Ariño-Gutiérrez M, Burgos-Blasco P, Carmona-González D, Fernández-Pérez C. Biometry data and prevalence of corneal astigmatism in caucasian spanish candidates for cataract surgery. Journal francais d'ophtalmologie. 2021 Jan:44(1):76-83. doi: 10.1016/j.jfo.2020.03.025. Epub 2020 Nov 6 [PubMed PMID: 33162179]
Kaur M, Shaikh F, Falera R, Titiyal JS. Optimizing outcomes with toric intraocular lenses. Indian journal of ophthalmology. 2017 Dec:65(12):1301-1313. doi: 10.4103/ijo.IJO_810_17. Epub [PubMed PMID: 29208810]
Núñez MX, Henriquez MA, Escaf LJ, Ventura BV, Srur M, Newball L, Espaillat A, Centurion VA. Consensus on the management of astigmatism in cataract surgery. Clinical ophthalmology (Auckland, N.Z.). 2019:13():311-324. doi: 10.2147/OPTH.S178277. Epub 2019 Feb 11 [PubMed PMID: 30809088]
Level 3 (low-level) evidenceShimizu K, Misawa A, Suzuki Y. Toric intraocular lenses: correcting astigmatism while controlling axis shift. Journal of cataract and refractive surgery. 1994 Sep:20(5):523-6 [PubMed PMID: 7996408]
Statham M, Apel A, Stephensen D. Comparison of the AcrySof SA60 spherical intraocular lens and the AcrySof Toric SN60T3 intraocular lens outcomes in patients with low amounts of corneal astigmatism. Clinical & experimental ophthalmology. 2009 Nov:37(8):775-9. doi: 10.1111/j.1442-9071.2009.02154.x. Epub [PubMed PMID: 19878222]
Level 2 (mid-level) evidenceNanavaty MA, Lake DB, Daya SM. Outcomes of pseudophakic toric intraocular lens implantation in Keratoconic eyes with cataract. Journal of refractive surgery (Thorofare, N.J. : 1995). 2012 Dec:28(12):884-9 [PubMed PMID: 23310966]
Level 2 (mid-level) evidenceGao Y, Ye Z, Chen W, Li J, Yan X, Li Z. Management of Cataract in Patients with Irregular Astigmatism with Regular Central Component by Phacoemulsification Combined with Toric Intraocular Lens Implantation. Journal of ophthalmology. 2020:2020():3520856. doi: 10.1155/2020/3520856. Epub 2020 Apr 30 [PubMed PMID: 32411427]
Srinivasan S, Ting DS, Lyall DA. Implantation of a customized toric intraocular lens for correction of post-keratoplasty astigmatism. Eye (London, England). 2013 Apr:27(4):531-7. doi: 10.1038/eye.2012.300. Epub 2013 Jan 25 [PubMed PMID: 23348728]
Level 2 (mid-level) evidenceRa H, Hwang HS, Kim HS, Kim MS, Kim EC. Toric intraocular lens implantation in cataract patients with corneal opacity. BMC ophthalmology. 2020 Mar 13:20(1):98. doi: 10.1186/s12886-020-01352-w. Epub 2020 Mar 13 [PubMed PMID: 32169054]
Stewart CM, McAlister JC. Comparison of grafted and non-grafted patients with corneal astigmatism undergoing cataract extraction with a toric intraocular lens implant. Clinical & experimental ophthalmology. 2010 Nov:38(8):747-57. doi: 10.1111/j.1442-9071.2010.02336.x. Epub [PubMed PMID: 20497428]
Level 2 (mid-level) evidenceSingh VM, Ramappa M, Murthy SI, Rostov AT. Toric intraocular lenses: Expanding indications and preoperative and surgical considerations to improve outcomes. Indian journal of ophthalmology. 2022 Jan:70(1):10-23. doi: 10.4103/ijo.IJO_1785_21. Epub [PubMed PMID: 34937203]
Güçlü H, Akaray İ, Kaya S, Sattarpanah S, Çınar AC, Sakallıoğlu K, Korkmaz S, Gürlü V. Agreement of Anterior Segment Parameters Between Schiempflug Topography and Swept-Source Optic Coherence Based Optic Biometry in Keratoconus and Healthy Subjects. Eye & contact lens. 2021 Oct 1:47(10):539-545. doi: 10.1097/ICL.0000000000000787. Epub [PubMed PMID: 33813587]
Goto S, Maeda N. Corneal Topography for Intraocular Lens Selection in Refractive Cataract Surgery. Ophthalmology. 2021 Nov:128(11):e142-e152. doi: 10.1016/j.ophtha.2020.11.016. Epub 2020 Nov 19 [PubMed PMID: 33221325]
Wang L, Koch DD. Intraocular Lens Power Calculations in Eyes with Previous Corneal Refractive Surgery: Review and Expert Opinion. Ophthalmology. 2021 Nov:128(11):e121-e131. doi: 10.1016/j.ophtha.2020.06.054. Epub 2020 Jun 29 [PubMed PMID: 32615201]
Level 3 (low-level) evidenceMontés-Micó R, Pastor-Pascual F, Ruiz-Mesa R, Tañá-Rivero P. Ocular biometry with swept-source optical coherence tomography. Journal of cataract and refractive surgery. 2021 Jun 1:47(6):802-814. doi: 10.1097/j.jcrs.0000000000000551. Epub [PubMed PMID: 33315731]
Chung J, Bu JJ, Afshari NA. Advancements in intraocular lens power calculation formulas. Current opinion in ophthalmology. 2022 Jan 1:33(1):35-40. doi: 10.1097/ICU.0000000000000822. Epub [PubMed PMID: 34854826]
Level 3 (low-level) evidencePantanelli SM, Kansara N, Smits G. Predictability of Residual Postoperative Astigmatism After Implantation of a Toric Intraocular Lens Using Two Different Calculators. Clinical ophthalmology (Auckland, N.Z.). 2020:14():3627-3634. doi: 10.2147/OPTH.S276285. Epub 2020 Oct 29 [PubMed PMID: 33154622]
Shukhaev SV, Boiko EV, Kudlakhmedov SS. [Comparative assessment of the accuracy of toric intraocular lens calculations]. Vestnik oftalmologii. 2022:138(1):5-12. doi: 10.17116/oftalma20221380115. Epub [PubMed PMID: 35234415]
Level 2 (mid-level) evidenceSheen-Ophir S, Reitblat O, Levy A, Assia EI, Kleinmann G. Deviation from the planned axis of three toric intraocular lenses. Scientific reports. 2022 Aug 12:12(1):13760. doi: 10.1038/s41598-022-17811-x. Epub 2022 Aug 12 [PubMed PMID: 35962050]
Lipsky L, Barrett G. Comparison of toric intraocular lens alignment error with different toric markers. Journal of cataract and refractive surgery. 2019 Nov:45(11):1597-1601. doi: 10.1016/j.jcrs.2019.06.013. Epub [PubMed PMID: 31706514]
Farooqui JH, Koul A, Dutta R, Shroff NM. Comparison of two different methods of preoperative marking for toric intraocular lens implantation: bubble marker versus pendulum marker. International journal of ophthalmology. 2016:9(5):703-6. doi: 10.18240/ijo.2016.05.11. Epub 2016 May 18 [PubMed PMID: 27275425]
O'Neill BP, Diakonis VF, Tsaousis KT, Weinstock RJ. Outcomes of toric IOL implantation guided by iris-registered femtosecond laser capsulotomy markings. International ophthalmology. 2021 Dec:41(12):4009-4015. doi: 10.1007/s10792-021-01973-0. Epub 2021 Jul 27 [PubMed PMID: 34313930]
Zhou F, Jiang W, Lin Z, Li X, Li J, Lin H, Chen W, Wang Q. Comparative meta-analysis of toric intraocular lens alignment accuracy in cataract patients: Image-guided system versus manual marking. Journal of cataract and refractive surgery. 2019 Sep:45(9):1340-1345. doi: 10.1016/j.jcrs.2019.03.030. Epub [PubMed PMID: 31470944]
Level 2 (mid-level) evidenceRaucau M, El Chehab H, Agard E, Lagenaite C, Dot C. Toric lens implantation in cataract surgery: Automated versus manual horizontal axis marking, analysis of 50 cases. Journal francais d'ophtalmologie. 2018 Jan:41(1):e1-e9. doi: 10.1016/j.jfo.2017.11.002. Epub 2018 Jan 10 [PubMed PMID: 29331293]
Level 3 (low-level) evidenceMiyake T, Kamiya K, Amano R, Iida Y, Tsunehiro S, Shimizu K. Long-term clinical outcomes of toric intraocular lens implantation in cataract cases with preexisting astigmatism. Journal of cataract and refractive surgery. 2014 Oct:40(10):1654-60. doi: 10.1016/j.jcrs.2014.01.044. Epub 2014 Aug 20 [PubMed PMID: 25149554]
Level 2 (mid-level) evidencePrinz A, Neumayer T, Buehl W, Vock L, Menapace R, Findl O, Georgopoulos M. Rotational stability and posterior capsule opacification of a plate-haptic and an open-loop-haptic intraocular lens. Journal of cataract and refractive surgery. 2011 Feb:37(2):251-7. doi: 10.1016/j.jcrs.2010.08.049. Epub [PubMed PMID: 21241906]
Level 2 (mid-level) evidenceShah GD, Praveen MR, Vasavada AR, Vasavada VA, Rampal G, Shastry LR. Rotational stability of a toric intraocular lens: influence of axial length and alignment in the capsular bag. Journal of cataract and refractive surgery. 2012 Jan:38(1):54-9. doi: 10.1016/j.jcrs.2011.08.028. Epub 2011 Nov 4 [PubMed PMID: 22055077]
Jung NY, Lim DH, Hwang SS, Hyun J, Chung TY. Comparison of clinical outcomes of toric intraocular lens, Precizon vs Tecnis: a single center randomized controlled trial. BMC ophthalmology. 2018 Nov 9:18(1):292. doi: 10.1186/s12886-018-0955-3. Epub 2018 Nov 9 [PubMed PMID: 30413154]
Level 2 (mid-level) evidenceEpitropoulos AT. Visual and Refractive Outcomes of a Toric Presbyopia-Correcting Intraocular Lens. Journal of ophthalmology. 2016:2016():7458210. doi: 10.1155/2016/7458210. Epub 2016 Jan 13 [PubMed PMID: 26885382]
Ribeiro FJ, Ferreira TB. Comparison of visual and refractive outcomes of 2 trifocal intraocular lenses. Journal of cataract and refractive surgery. 2020 May:46(5):694-699. doi: 10.1097/j.jcrs.0000000000000118. Epub [PubMed PMID: 32358262]
Piovella M, Colonval S, Kapp A, Reiter J, Van Cauwenberge F, Alfonso J. Patient outcomes following implantation with a trifocal toric IOL: twelve-month prospective multicentre study. Eye (London, England). 2019 Jan:33(1):144-153. doi: 10.1038/s41433-018-0076-5. Epub 2018 Sep 6 [PubMed PMID: 30190549]
Koch DD, Jenkins RB, Weikert MP, Yeu E, Wang L. Correcting astigmatism with toric intraocular lenses: effect of posterior corneal astigmatism. Journal of cataract and refractive surgery. 2013 Dec:39(12):1803-9. doi: 10.1016/j.jcrs.2013.06.027. Epub 2013 Oct 26 [PubMed PMID: 24169231]
Kodavoor SK, Divya J, Dandapani R, Ramamurthy C, Ramamurthy S, Sachdev G. Randomized trial comparing visual outcomes of toric intraocular lens implantation using manual and digital marker. Indian journal of ophthalmology. 2020 Dec:68(12):3020-3024. doi: 10.4103/ijo.IJO_465_20. Epub [PubMed PMID: 33229690]
Level 1 (high-level) evidenceUckmann MS, Stattin M, Zehetner C, Neururer S, Speicher L. [Comparison of two optical biometric devices for intraocular lens calculation]. Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2019 Mar:116(3):253-260. doi: 10.1007/s00347-018-0655-7. Epub [PubMed PMID: 29372303]
Ortiz A, Galvis V, Tello A, Viaña V, Corrales MI, Ochoa M, Rodriguez CJ. Comparison of three optical biometers: IOLMaster 500, Lenstar LS 900 and Aladdin. International ophthalmology. 2019 Aug:39(8):1809-1818. doi: 10.1007/s10792-018-1006-z. Epub 2018 Aug 22 [PubMed PMID: 30136018]
Melles RB, Holladay JT, Chang WJ. Accuracy of Intraocular Lens Calculation Formulas. Ophthalmology. 2018 Feb:125(2):169-178. doi: 10.1016/j.ophtha.2017.08.027. Epub 2017 Sep 23 [PubMed PMID: 28951074]
Bayramlar H, Dag Y, Karadag R, Cakici O. An easy and practical method for toric intraocular lens implantation: marking corneal astigmatic axis at slit-lamp. International ophthalmology. 2017 Feb:37(1):179-184. doi: 10.1007/s10792-016-0250-3. Epub 2016 May 12 [PubMed PMID: 27169419]
Popp N, Hirnschall N, Maedel S, Findl O. Evaluation of 4 corneal astigmatic marking methods. Journal of cataract and refractive surgery. 2012 Dec:38(12):2094-9. doi: 10.1016/j.jcrs.2012.07.039. Epub 2012 Oct 23 [PubMed PMID: 23098629]
Level 1 (high-level) evidenceCha D, Kang SY, Kim SH, Song JS, Kim HM. New axis-marking method for a toric intraocular lens: mapping method. Journal of refractive surgery (Thorofare, N.J. : 1995). 2011 May:27(5):375-9. doi: 10.3928/1081597X-20101005-01. Epub 2010 Oct 15 [PubMed PMID: 20954592]
Hura AS, Osher RH. Comparing the Zeiss Callisto Eye and the Alcon Verion Image Guided System Toric Lens Alignment Technologies. Journal of refractive surgery (Thorofare, N.J. : 1995). 2017 Jul 1:33(7):482-487. doi: 10.3928/1081597X-20170504-02. Epub [PubMed PMID: 28681908]
Ma JJ, Tseng SS. Simple method for accurate alignment in toric phakic and aphakic intraocular lens implantation. Journal of cataract and refractive surgery. 2008 Oct:34(10):1631-6. doi: 10.1016/j.jcrs.2008.04.041. Epub [PubMed PMID: 18812110]
Till JS, Yoder PR Jr, Wilcox TK, Spielman JL. Toric intraocular lens implantation: 100 consecutive cases. Journal of cataract and refractive surgery. 2002 Feb:28(2):295-301 [PubMed PMID: 11821213]
Level 3 (low-level) evidenceRuhswurm I, Scholz U, Zehetmayer M, Hanselmayer G, Vass C, Skorpik C. Astigmatism correction with a foldable toric intraocular lens in cataract patients. Journal of cataract and refractive surgery. 2000 Jul:26(7):1022-7 [PubMed PMID: 10946194]
Level 2 (mid-level) evidenceChang DF. Repositioning technique and rate for toric intraocular lenses. Journal of cataract and refractive surgery. 2009 Jul:35(7):1315-6. doi: 10.1016/j.jcrs.2009.02.035. Epub [PubMed PMID: 19545827]
Level 3 (low-level) evidenceThomas BC, Khoramnia R, Auffarth GU, Holzer MP. Clinical outcomes after implantation of a toric intraocular lens with a transitional conic toric surface. The British journal of ophthalmology. 2018 Mar:102(3):313-316. doi: 10.1136/bjophthalmol-2017-310386. Epub 2017 Aug 3 [PubMed PMID: 28774937]
Level 2 (mid-level) evidenceVale C, Menezes C, Firmino-Machado J, Rodrigues P, Lume M, Tenedório P, Menéres P, Brochado Mdo C. Astigmatism management in cataract surgery with Precizon(®) toric intraocular lens: a prospective study. Clinical ophthalmology (Auckland, N.Z.). 2016:10():151-9. doi: 10.2147/OPTH.S91298. Epub 2016 Jan 19 [PubMed PMID: 26855559]
Xiao XW, Hao J, Zhang H, Tian F. Optical quality of toric intraocular lens implantation in cataract surgery. International journal of ophthalmology. 2015:8(1):66-71. doi: 10.3980/j.issn.2222-3959.2015.01.12. Epub 2015 Feb 18 [PubMed PMID: 25709910]
Level 2 (mid-level) evidenceEspaillat A, Pérez O, Potvin R. Clinical outcomes using standard phacoemulsification and femtosecond laser-assisted surgery with toric intraocular lenses. Clinical ophthalmology (Auckland, N.Z.). 2016:10():555-63. doi: 10.2147/OPTH.S102083. Epub 2016 Mar 30 [PubMed PMID: 27099462]
Level 2 (mid-level) evidence