Introduction
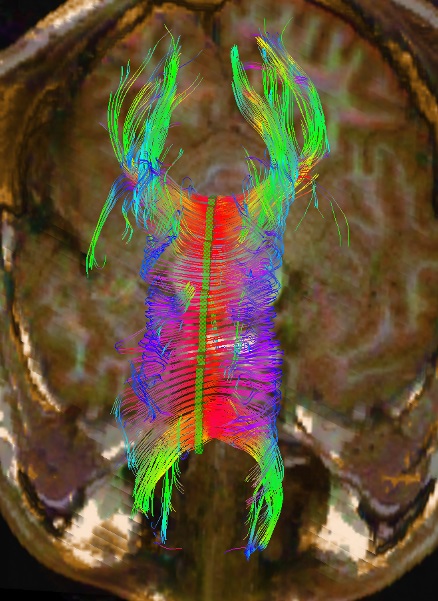
The corpus callosum is the primary commissural region of the brain consisting of white matter tracts that connect the left and right cerebral hemispheres (see Images. Corpus Callosum From Above, Diffusion Tensor Imaging of Corpus Callosum). It is composed of approximately 200 million heavily myelinated nerve fibers that form homotopic or heterotopic projections to contralateral neurons in the same anatomical layer.[1] During infancy, the corpus callosum expands rapidly due to an increase in the number of axons, axon diameter, and myelin. Although the development of the corpus callosum is complete by age four, growth continues until the third decade of life at a much slower rate.[1] Anatomically from anterior to posterior, the corpus callosum is composed of four parts based on previous histological findings: the rostrum, genu, body, and splenium, each responsible for connecting distinct areas of the cortex. The isthmus refers to the narrow region between the body and splenium in the posterior aspect of the corpus callosum.[2] Fibers of the genu cross over and give rise to the forceps minor, a connection between regions of the frontal cortices.[2] The fibers of the splenium move posteriorly and contribute to the forceps major, providing a connection between the occipital lobes.[3] The body fibers form the corona radiata as well as other large white matter pathways as they move transversely through the cerebral cortex. Finally, the orbital regions of the frontal lobes connect via the rostral fibers.[3] Due to its anatomical location, the corpus callosum is strongly related to the fornix and lateral ventricles (see Image. The Fornix and Corpus Callosum From Below). In conjunction with the fornix, the corpus callosum forms a physical barrier to separate the two lateral ventricles (see Image. Central and Anterior and Posterior Cornua of Lateral Ventricles Exposed From Above).[3]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The primary function of the corpus callosum is to integrate and transfer information from both cerebral hemispheres to process sensory, motor, and high-level cognitive signals. There have been significant advances made in learning more about the corpus callosum's role by studying callosotomy patients with partial or total hemispheric disconnection.[4] Based on these observations, the corpus callosum seems to have a topographical organization, involved in the transfer of visual, auditory, and somatosensory information in posterior regions, and higher cognition is processing anteriorly.[4] There is evidence for the idea that the anterior callosal fibers transfer motor information between the frontal lobes, and the posterior fibers are involved in the processing of somatosensory (posterior midbody), auditory (isthmus) and visual (splenium) cues by connecting the parietal, temporal, and occipital lobes.[3] As the brain matures and white matter develops, the corpus callosum seems to play a crucial role in refining motor movements and cognitive functions.[3] Additional studies have shown that the corpus callosum has an inhibitory effect that normally prevents alien-hand syndrome and uncoordinated hand-motor behavior.[4] See Image. Coronal Tractography, Corpus Callosum.
Embryology
There are approximately 200 million axons that form the corpus callosum, which arises primarily from neurons in neocortical layers II/III, V, and VI.[5] At 12 to 13 weeks of gestation, nerve fibers begin to cross the midline, giving rise to connections that later become the corpus callosum. By 18 weeks, all four components of the corpus callosum can be visualized using a transvaginal sonogram.[6] There is some debate about the anatomic direction in which development progresses; some data support the hypothesis that the corpus callosum develops in the cranial/caudal direction while others have observed the opposite developmental pattern. Interestingly, the corpus callosum is present in all primates and evolved with the neocortex.[7]
Blood Supply and Lymphatics
The internal carotid artery network provides arterial blood supply to a majority of the corpus callosum, specifically via the pericallosal artery (a branch of the anterior cerebral artery). The splenium is the exception as it receives vascular input from the vertebrobasilar system. The terminal and choroidal branches of the posterior cerebral artery supply the splenium with arterial blood. Venous drainage occurs via the callosal and callosal cingular veins and, ultimately, the internal cerebral veins.[7]
Physiologic Variants
Physiologic variants of the corpus callosum include agenesis or hypoplasia. Agenesis of the corpus callosum is an uncommon brain malformation that either leads to a partial or total absence of the corpus callosum. Though rare, it is one of the more frequently occurring congenital malformations, affecting three to seven people per 1000 births.[7] A diagnosis can be made using prenatal ultrasound and can be concurrent with malformations in midline structures like cavum septum pellicidum, as well as cortical and posterior fossa abnormalities.[7][8][7] In part, it is the result of multiple developmental abnormalities, affecting steps as early as midline telencephalic patterning to later neuronal differentiation and axonal guidance.[5] The cause is unknown but appears to be sporadic and possibly non-genetic. Despite the corpus callosum's crucial role in normal cognition, patients with isolated agenesis of the corpus callosum typically have good prognoses. Common deficits observed in this population include difficulty with problem-solving and socializing, often placing patients on the autism spectrum.[9] These deficits, known as "disconnection syndrome," are different from those observed in commissurotomy patients, who most notably have impaired bimanual coordinated motor activity.[5] Currently, 55% to 70% of agenesis of the corpus callosum cases are not identified based on clinical features. Hypoplasia is most benign when the rostrum is absent and often is not clinically significant. Therefore, it is commonly an incidental finding in a magnetic resonance imaging (MRI) scan obtained for other clinical reasons.[5][10]
Surgical Considerations
A corpus callosotomy is a surgical procedure for patients with refractory disorders despite maximum medical management. Also, it is the preferred surgical procedure for patients with refractory seizure disorder with drop attacks. Though controversial, some advocate for the surgical resection of the corpus callosum to treat low-grade gliomas as the migration patterns of these tumors typically involve the invasion of white matter tracts.
Clinical Significance
The most common pathology associated with the corpus callosum is multiple sclerosis, resulting in demyelinating lesions in the corpus callosum and pericallosal region. Corpus callosum congenital anomalies are often associated with other brain defects, so evidence of an abnormality in corpus callosum development should prompt a workup for other potentially serious defects. In addition to the physiologic variants, corpus callosum lipomas are considered to be congenital malformations of the primitive meninges. Corpus callosum lipomas classify as either curvilinear, which are usually located posteriorly and are asymptomatic, and tubulonodular, which are found anteriorly and associated with severe frontal abnormalities. Ischemia of the corpus callosum is uncommon due to vascular inputs from three main arteries: the anterior communicating, anterior pericallosal, and posterior cerebral arteries. However, ischemia can result from emboli, and stenosis the result of atherosclerotic plaques, or vasospasm of the supplying arteries. Ruptured aneurysms in the anterior cerebral or pericallosal arteries typically cause hemorrhages of the corpus callosum. Consequently, hematomas located in the anterior corpus callosum should be investigated using computed tomogram (CT) angiography or three-dimensional time of flight MR angiography. The corpus callosum has been implicated in many other pathologies as well. Marchiava-Bignami disease involves acute demyelination and necrosis of the corpus callosum, most commonly observed in the body region of the corpus callosum in patients with chronic alcoholism. Other toxins like carbon monoxide and drugs like cocaine and heroin have also correlated with demyelination and lesions in the corpus callosum. Other pathologies that can cause corpus callosum lesions and demyelination include exposure to certain viruses, metabolic dysfunction, and traumatic brain injury. The most common tumors found in the corpus callosum are glioblastomas, as well as lymphomas and metastases.[7] The corpus callosum can undergo infarction, but the presenting symptoms of a corpus callosum stroke are vague and non-specific. One study found the most common signs and symptoms of a corpus callosum stroke in decreasing order are: different degrees of limb dyskinesia (84%), language disorder including some degree of mixed aphasia, complete motor aphasia, incomplete motor aphasia, or unclear words or clumsy speech (48%), cognitive or mental abnormality (40%), grope for action and forced laughter and crying (20%), alien hand syndrome (4%), partial body hypoalgesia(8%) in the patients who can cooperate physical examination, visual field loss (4%), and incontinence (8%).[11]
Media
(Click Image to Enlarge)
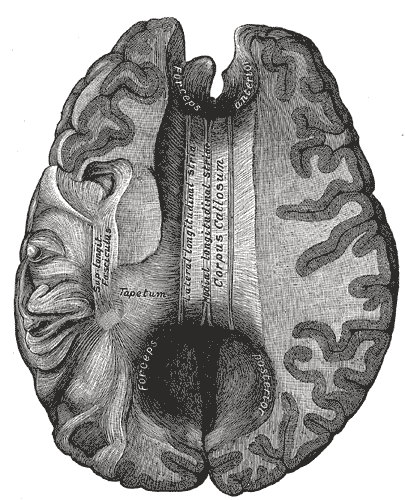
Corpus Callosum From Above. The image depicts the lateral and medial longitudinal stria, tapetum, superior longitudinal fasciculus, and forceps posterior and anterior.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
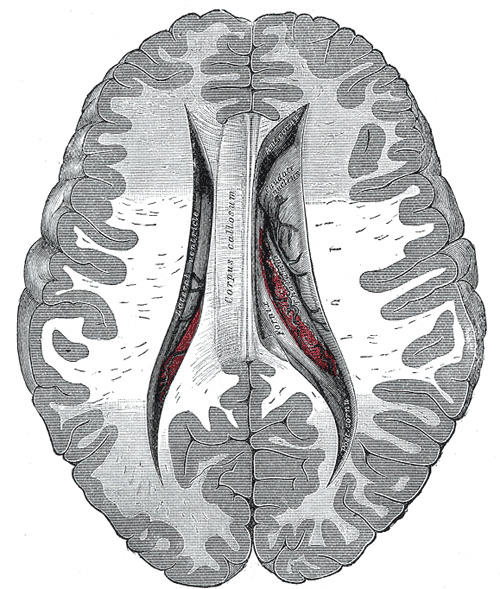
Central and Anterior and Posterior Cornua of Lateral Ventricles Exposed From Above.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
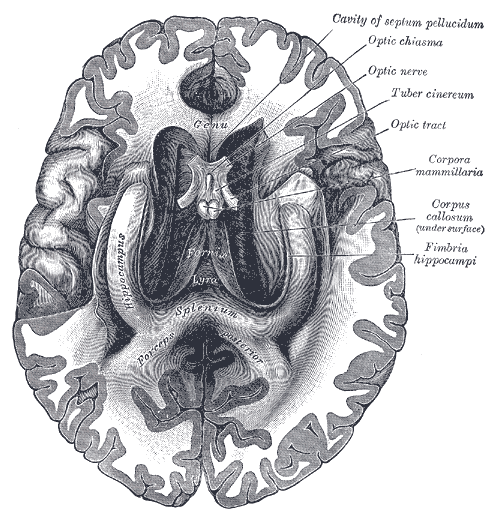
The Fornix and Corpus Callosum From Below. The image depicts the genu, hippocampus, forceps posterior, cavity of septum pellucidum, optic chiasma, optic nerve, tuber cinereum, optic tract, corpora mammillaria, and fimbria hippocampi.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Tanaka-Arakawa MM, Matsui M, Tanaka C, Uematsu A, Uda S, Miura K, Sakai T, Noguchi K. Developmental changes in the corpus callosum from infancy to early adulthood: a structural magnetic resonance imaging study. PloS one. 2015:10(3):e0118760. doi: 10.1371/journal.pone.0118760. Epub 2015 Mar 19 [PubMed PMID: 25790124]
Sakai T, Mikami A, Suzuki J, Miyabe-Nishiwaki T, Matsui M, Tomonaga M, Hamada Y, Matsuzawa T, Okano H, Oishi K. Developmental trajectory of the corpus callosum from infancy to the juvenile stage: Comparative MRI between chimpanzees and humans. PloS one. 2017:12(6):e0179624. doi: 10.1371/journal.pone.0179624. Epub 2017 Jun 27 [PubMed PMID: 28654656]
Level 2 (mid-level) evidenceMusiek FE. Neuroanatomy, neurophysiology, and central auditory assessment. Part III: Corpus callosum and efferent pathways. Ear and hearing. 1986 Dec:7(6):349-58 [PubMed PMID: 3792676]
Intra- and Inter-hemispheric Connectivity Supporting Hemispheric Specialization, Tzourio-Mazoyer N,,, 2016 [PubMed PMID: 28590670]
Edwards TJ, Sherr EH, Barkovich AJ, Richards LJ. Clinical, genetic and imaging findings identify new causes for corpus callosum development syndromes. Brain : a journal of neurology. 2014 Jun:137(Pt 6):1579-613. doi: 10.1093/brain/awt358. Epub 2014 Jan 28 [PubMed PMID: 24477430]
Level 3 (low-level) evidenceMalinger G, Zakut H. The corpus callosum: normal fetal development as shown by transvaginal sonography. AJR. American journal of roentgenology. 1993 Nov:161(5):1041-3 [PubMed PMID: 8273605]
Fitsiori A, Nguyen D, Karentzos A, Delavelle J, Vargas MI. The corpus callosum: white matter or terra incognita. The British journal of radiology. 2011 Jan:84(997):5-18. doi: 10.1259/bjr/21946513. Epub [PubMed PMID: 21172964]
Das JM, Dossani RH. Cavum Septum Pellucidum. StatPearls. 2024 Jan:(): [PubMed PMID: 30725733]
Paul LK, Brown WS, Adolphs R, Tyszka JM, Richards LJ, Mukherjee P, Sherr EH. Agenesis of the corpus callosum: genetic, developmental and functional aspects of connectivity. Nature reviews. Neuroscience. 2007 Apr:8(4):287-99 [PubMed PMID: 17375041]
Das JM, Geetha R. Corpus Callosum Agenesis. StatPearls. 2024 Jan:(): [PubMed PMID: 31082030]
Yang LL, Huang YN, Cui ZT. Clinical features of acute corpus callosum infarction patients. International journal of clinical and experimental pathology. 2014:7(8):5160-4 [PubMed PMID: 25197390]