Introduction
A joint is a region where 2 bones make contact. Joints may be classified histologically or functionally. Histological classification is based on the predominant connective tissue type composing the joint, either fibrous, cartilaginous, or synovial. Functional classification is based on the amount of movement the joint permits. The 3 functional joint types include the immovable synarthrosis, slightly moveable amphiarthrosis, and freely moveable diarthrosis. The 2 joint classification schemes correlate: synarthroses are fibrous, amphiarthroses are cartilaginous, and diarthroses are synovial.[1][2]
Joints, comprised of bones and connective tissue, embryologically develop from mesenchyme. Bones may develop directly through intramembranous ossification or indirectly via endochondral ossification. Each joint has unique vascular and innervation schemes with recognizable patterns. Muscles stabilize joints. Muscle strength directly correlates with joint stability, particularly in synovial joints.
Many pathophysiological conditions affect joints, with histological class determining the kind of pathology that develops. Joint diseases are common across all ages. A thorough understanding of joint structure and function is of great clinical significance.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Joint classifications offer a broad understanding of joints. The different joint types are explained below.
Fibrous Joints
A fibrous joint is a fixed joint (synarthrosis) where collagenous fibrous connective tissue unites 2 bones. Fibrous joints are usually immovable and lack a joint cavity. These joints are further classified into sutures, gomphoses, and syndesmoses.
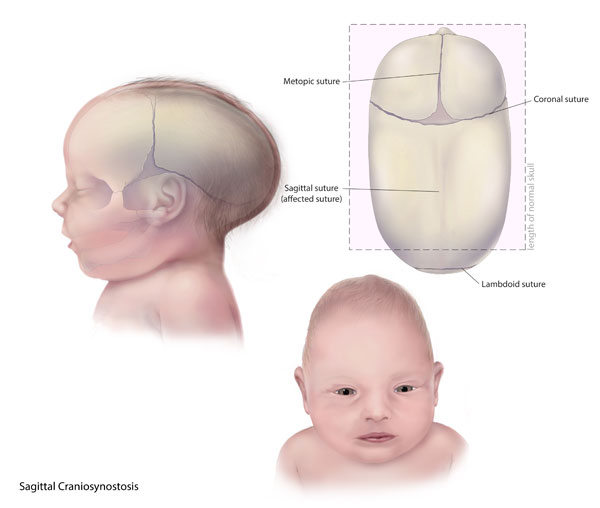
Sutures are immobile joints found only in the cranium (see Image. Coronal Suture). The spaces between the bones are termed "fontanelles." The skull's plate-like bones are slightly mobile at birth because of the soft connective tissue binding them in the fontanelles. This initial joint flexibility allows the fetal head to pass through the birth canal at delivery and permits brain enlargement after birth. As the skull enlarges, the fontanelles gradually diminish to form thin fibrous connective tissue layers called "Sharpey fibers," which help bind the bony plates together. Over time, these cranial sutures harden through ossification. Neighboring plates eventually merge into a single bone through a process known as synostosis.
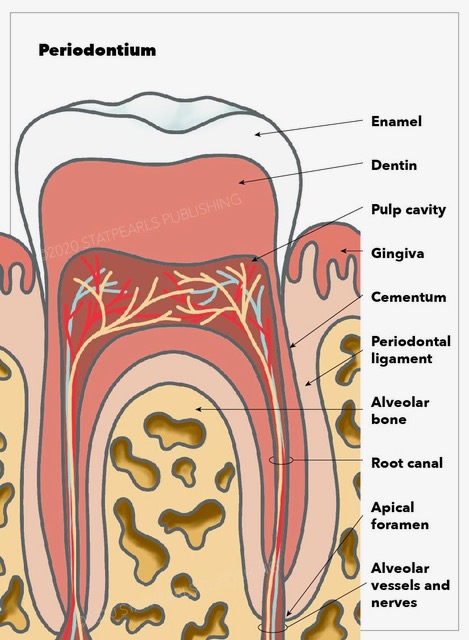
Gomphoses are immobile joints found only between the teeth and their sockets in the mandible and maxillae. The periodontal ligament is the fibrous tissue connecting the tooth to the socket (see Image. Periodontium Anatomy).
Syndesmoses are slightly movable joints (amphiarthroses). This fibrous joint type maintains the union between long bones, thus resisting divisive forces. All syndesmoses are amphiarthroses, though specific types may permit variable degrees of movement. For example, the tibiofibular syndesmosis primarily provides leg and ankle strength and stability during weight-bearing. However, the antebrachial interosseous membrane of the radioulnar syndesmosis permits radial rotation during supination and pronation (see Image. Radioulnar Joints). The leg and forearm interosseous membranes are also areas of muscle attachment.[3]
Cartilaginous Joints
Cartilaginous joints have bones attached by hyaline or fibrous cartilage. The joints are further classified as primary or secondary cartilaginous joints, depending on the cartilage type involved.
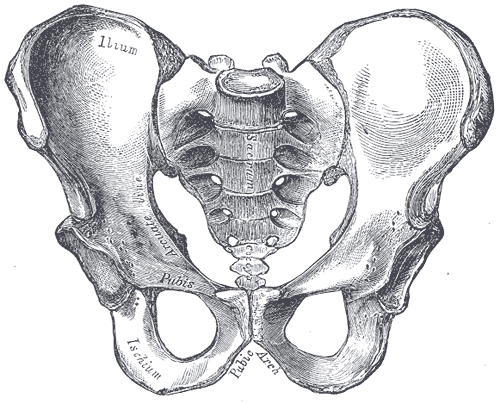
A synchondrosis, or primary cartilaginous joint, only contains hyaline cartilage and can be temporary or permanent. The epiphyseal plate (growth plate) is the best example of a temporary synchondrosis. The growth plate permits bone lengthening during development while connecting the diaphysis (bone shaft) with the epiphysis (bone tip) in children (see Image. Parts of a Long Bone). During development, the cartilaginous plate expands and ossifies, lengthening the diaphysis. Bones complete their linear growth once all hyaline cartilage ossifies, with the diaphysis and epiphysis fusing to form a synostosis. Other temporary synchondroses are found in children's hips, joining the ilium, ischium, and pubic bones. The ilium, ischium, and pubis later fuse completely to form the adult innominate bone.
A permanent synchondrosis does not ossify with age but retains its hyaline cartilage. Permanent synchondroses connect bones without allowing any movement, similar to a synarthrosis. These joints are commonly found in the thoracic cage. For instance, the 1st sternocostal joint unites the 1st rib to the manubrium by its costal cartilage. Other examples include the connections between the anterior ends of the remaining 11 ribs and their respective costal cartilages.[4]
A symphysis, or secondary cartilaginous joint, contains fibrocartilage (see Image. Male Pelvis Anatomy). This cartilage type is thick and strong. Thus, symphyses have a remarkable ability to resist pulling and bending forces. However, a symphysis is still often classified as an amphiarthrosis, permitting limited movement despite fibrocartilage uniting adjacent bones.
A symphysis may be narrow or wide. Narrow symphyses include the pubic symphysis and manubriosternal joint. In women, the pubic symphysis' slight mobility is critical during childbirth. Meanwhile, an example of a wide symphysis is the intervertebral symphysis, also known as the intervertebral disk (see Image. Intervertebral Disk). The thick fibrocartilage pad fills the gap between adjacent vertebrae and provides cushioning during high-impact activity.
Synovial Joints
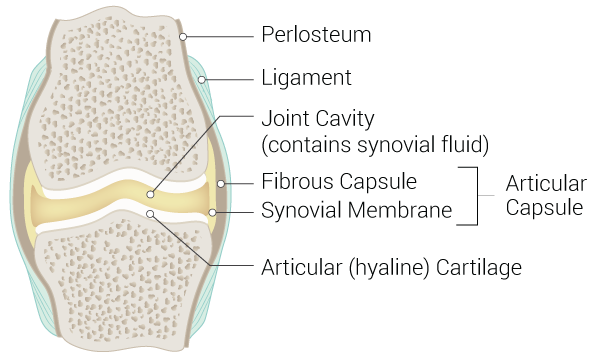
Synovial joints are freely mobile (diarthroses) and are considered the body's main functional joints (see Image. Synovial Joint). The synovial joint is characterized by the presence of a joint cavity. The synovial joint's primary function is to prevent friction between the articulating bones involved in body movements. The joint cavity is surrounded by the articular capsule, a fibrous connective tissue attached to the joint's participating bones just beyond the articulating surface. The joint cavity contains synovial fluid secreted by the synovial membrane (synovium), which lines the articular capsule. Hyaline cartilage forms the articular cartilage covering each bone's articulating surface. The articular cartilage is continuous with the synovial membrane. Some synovial joints, such as the knee menisci, have associated fibrocartilage between articulating bones.
While all synovial joints are diarthroses, the extent of movement varies among subtypes and is often limited by the ligaments connecting the bones. Thus, synovial joints are often classified by the movement types they permit: hinge, saddle, planar, pivot, condyloid, and ball-and-socket. These joint classes are explained below.
Hinge
A hinge joint is an articulation between the convex end of one bone and the concave edge of another. This joint type is uniaxial, permitting movement along only one axis. Flexion and extension are typically the only movements allowed by hinge joints. Examples include the elbow, knee, ankle, and interphalangeal joints.
Condyloid
A condyloid joint (ellipsoid joint) is an articulation between the shallow depression of one bone and the rounded structure of one or more other bones. This joint type is biaxial, permitting movement in 2 axes. Thus, 4 movements are possible at condyloid joints: flexion, extension, abduction, and adduction. Examples of condyloid joints are the knuckles, formed by the distal metacarpals and proximal phalanges of the medial 4 fingers.
Saddle
A saddle joint is an articulation between 2 saddle-shaped bones, which are concave in one direction and convex in another. This joint type is biaxial. One example is the joint formed by the trapezium and 1st metacarpal bone. This joint allows the thumb to flex and extend parallel to the palm and abduct and adduct perpendicular to the palm, making the digit opposable. The opposable thumb is critical for complex hand motions. Thumb loss by any mechanism severely limits hand function.
Planar
A planar joint (gliding joint) is an articulation between 2 flat bones of similar size. Planar joints are multiaxial but restricted by the surrounding ligaments. Examples include the acromioclavicular, intercarpal, and intertarsal joints. The calcaneocuboid joint is unlike other intertarsal joints, as it is classified as a saddle joint.
Pivot
A pivot joint occurs between one bone and the cylindrical end of another, enclosed within a ligamentous ring (see Image. Cervical Vertebrae). This joint is uniaxial, allowing rotation around a single axis as the bone moves within the ring. The atlantoaxial joint, formed by the 1st (atlas) and 2nd (axis) cervical vertebrae, is a pivot joint. The atlantoaxial joint permits side-to-side head motion. Another example is the proximal radioulnar joint. The radius sits in the annular radial ligament, which holds the bone in place as it articulates with the ulna's radial notch, thus permitting pronation and supination.
Ball-and-socket
A ball-and-socket joint is an articulation between the rounded head of one bone (ball) and the concavity of another (socket). This joint type is multiaxial, as possible movements include flexion, extension, abduction, adduction, and rotation. The body's only ball-and-socket joints are the hip and shoulder (glenohumeral) joints. The glenoid cavity's shallow socket permits an extensive range of motion in the shoulder. In contrast, the deep acetabular socket and the surrounding ligaments constrain femoral movement in the hip joint.
Embryology
Joints, comprised of bones and connective tissue, derive from embryonic mesenchyme. Bones develop directly through intramembranous ossification or indirectly through endochondral ossification. Mesenchymal cells directly differentiate into bone-producing cells during intramembranous ossification. In contrast, endochondral ossification involves hyaline cartilage differentiation from mesenchyme before getting replaced by bone. The joint connective tissue arises from the mesenchymal cells between the developing bones.
"Joint interzones" form between the emerging long bones around the 6th week of embryonic development, signifying the start of synovial joint formation. The mesoderm on each side, known as the paraxial blastema, condenses into hyaline cartilage models for the long bones. By the 8th week of embryonic development, mesenchymal cells at the interzones' margins become the articular capsule. Cell death within each interzone creates the joint cavity, filled with synovial fluid produced by mesenchymal cells. The articular cartilage is a remnant of the hyaline cartilage that transforms into long bones through endochondral ossification between gestational weeks 6 and 8.[5][6]
Blood Supply and Lymphatics
The histological type determines how blood vessels are arranged around a joint. Perforating branches of proximal vessels usually supply fibrous joints. For example, the tibiofibular joint's circulation is derived from anterior tibial and peroneal (fibular) arterial branches.
Cartilaginous joints only receive their vascular supply at the periphery because cartilage is an avascular tissue. For example, vertebral body capillaries supply intervertebral disks at the margins.
Synovial joints receive vascular supply through rich arterial anastomoses extending from either side of the joint, termed the "periarticular plexus." Some blood vessels penetrate the fibrous capsule to form a rich plexus deep within the synovial membrane, the circulus vasculosus. This plexus loops around the articular margins, supplying the articular capsule, synovial membrane, and terminal bones. The articular cartilage, which is essentially avascular hyaline cartilage, is nourished by synovial fluid.
Joint lymphatic vessels follow the lymph drainage of the surrounding tissue. Some joints house lymph nodes, eg, the popliteal lymph nodes in the knee's popliteal fossa.
Nerves
Synovial joint innervation is the most extensively understood among joint nerve arrangements. Sensory and autonomic fibers innervate synovial joints. Sympathetic nerves regulate vascular tone by norepinephrine and epinephrine's interaction with smooth muscle α-1 adrenergic receptors. The sensory nerves within the articular capsule and ligaments (articular nerves) provide proprioceptive feedback from Ruffini endings and Pacinian corpuscles. Joint proprioception permits reflex control of posture, locomotion, and movement. Free nerve endings convey diffuse, poorly localized pain sensations. Articular cartilage has no nerve supply.
Two general principles apply to synovial joint innervation: the Hilton law and the Gardner observation. The Hilton law states that articular nerves supplying a joint are branches of the nerves supplying the muscles responsible for moving that joint. Articular nerve irritation causes a reflex muscular spasm, positioning the joint for the greatest comfort. These nerves also supply the overlying skin, enabling referred pain from joint to skin. Meanwhile, the Gardner observation indicates that the articular capsule segment tightened by muscle contraction is supplied by the same nerves supplying the antagonist muscles. This relationship provides local reflex arcs that stabilize the joint.[7]
Muscles
Muscles are most critical in providing additional support for synovial joints. The muscles and their tendons crossing the joint resist the forces acting on that joint, behaving as a dynamic "ligament." Muscle strength is, thus, essential to synovial joint stability, especially during high-stress activity involving joints with weaker ligaments, such as the glenohumeral joint.
Surgical Considerations
Arthroplasty is a procedure that surgically replaces joints. This procedure may be used to treat osteoarthritis that causes chronic pain and limited mobility unresponsive to conservative therapies. The damaged bone is removed, and the articular surfaces are replaced with a metallic, plastic, or ceramic device (prosthesis) that mimics the joint's natural structure. The hips and knees are the most commonly replaced joints.
Clinical Significance
Different joint types are vulnerable to different pathologic conditions. Below is a review of some common joint type-specific injuries.
Fibrous Joint Conditions
Sutures are fibrous joints that normally remain immobile in the adult skull, binding the bony plates together. By comparison, neonatal skull plates are not fused to allow space for brain growth in all directions. Craniosynostosis is a condition whereby sutures fuse prematurely during development. Premature fusion alters head shape. For instance, if the sagittal suture fuses early, the head may grow long and narrow (scaphocephaly) instead of round (see Image. Scaphocephaly). Craniosynostosis can also cause headaches, developmental delays, or visual problems, as the restricted skull space increases intracranial pressure.[8]
Syndesmoses can be sprained. In the leg, excessive external rotation can tear the distal tibiofibular syndesmosis and displace the fibula away from the tibia. This condition results in a “high ankle sprain.”[9]
Cartilaginous Joint Disorders
Epiphyseal plates are vulnerable to damage from long bone fractures. Epiphyseal damage can disrupt bone lengthening and stunt growth.
Synovial Joint Diseases
Arthritis arises from various injury mechanisms and may cause synovial joint destruction. Osteoarthritis is the most common form, developing from gradual articular cartilage damage and subsequent thinning. This condition is considered a “wear and tear” injury, more common in older than younger patients. Osteoarthritis often correlates with prior injury and longstanding high-impact stress on the affected joint, usually from sports or excessive body weight. The degradation process itself does not cause pain because articular cartilage lacks innervation. However, pain arises due to articular cartilage thinning, stimulating pain fibers in nearby areas. The joint's damage response is synovial fluid production, leading to swelling and inflammation that stretches the highly innervated articular capsule and causes joint pain and stiffness. Compression of the underlying bone also results in pain, as bones are richly innervated.
Gout is an arthritic condition arising from uric acid deposition within a joint. Hyperuricemia results from overproduction or improper renal excretion and leads to uric acid precipitation within joints. The most commonly affected joint is the big toe's metatarsophalangeal joint, a condition termed "podagra."[10][11][12] Patients often present with excruciating pain and swelling on this digit.[13] Alcohol consumption may exacerbate podagra.[14][15][16]
Synovitis is inflammation of the synovial membrane that lines the synovial joints' articular capsules. Joint overuse is the most common cause of this condition in active, healthy people. Persistent synovitis in multiple joints may indicate rheumatoid arthritis, where the synovium is an autoimmune target. Patients with synovitis often present with pain out of proportion to examination. For example, arthralgia or joint pain without swelling or tenderness may be present.
Media
(Click Image to Enlarge)
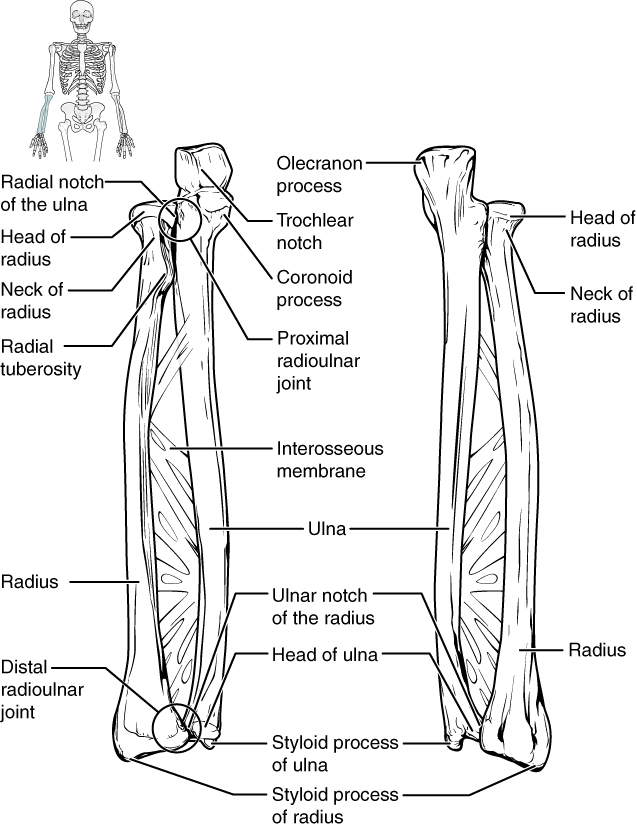
Radioulnar Joints. The radius and ulna connect at various points, including the proximal and distal radioulnar joints and the interosseous membrane.
OpenStax College, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
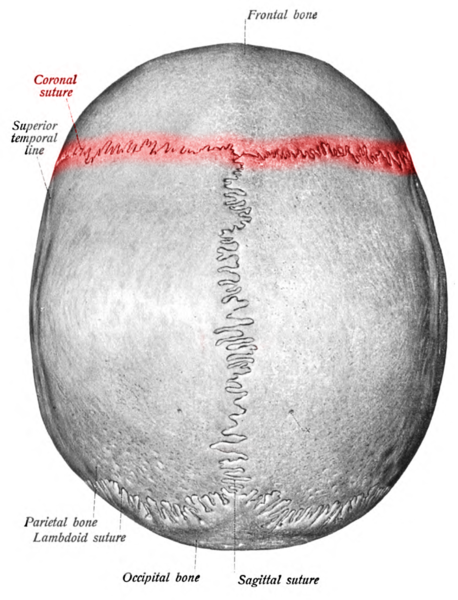
Coronal Suture, Labeled. This illustration shows the coronal (red), sagittal, and lambdoid sutures. Other labeled structures include the frontal, parietal, and occipital bones and the superior temporal line.
Atlas and Textbook of Human Anatomy, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
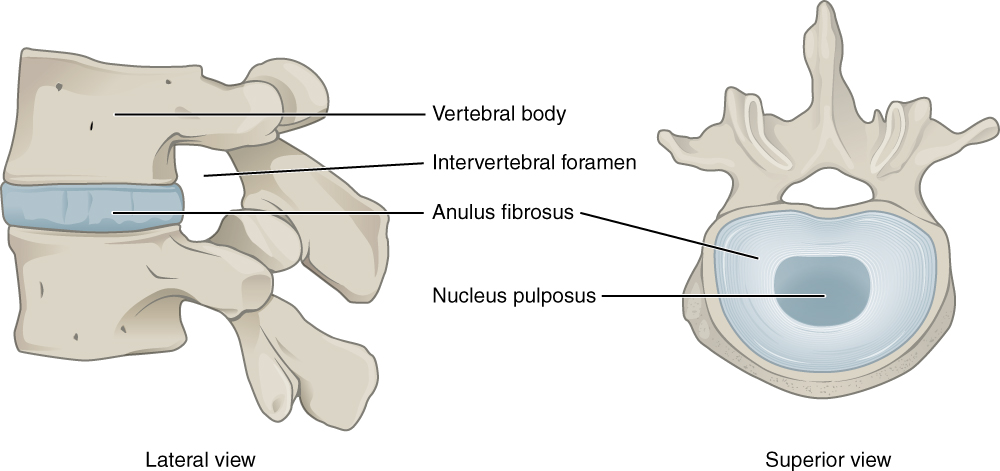
Intervertebral Disk. This lateral view shows the disc between two vertebrae. The superior view shows the annulus fibrosis at the outer layer and the nucleus pulposus in the inner layer.
Illustration from Anatomy & Physiology, Connexions Web site. http://cnx.org/content/col11496/1.6/, Jun 19, 2013. This file is licensed under the Creative Commons Attribution 3.0 Unported license.
(Click Image to Enlarge)
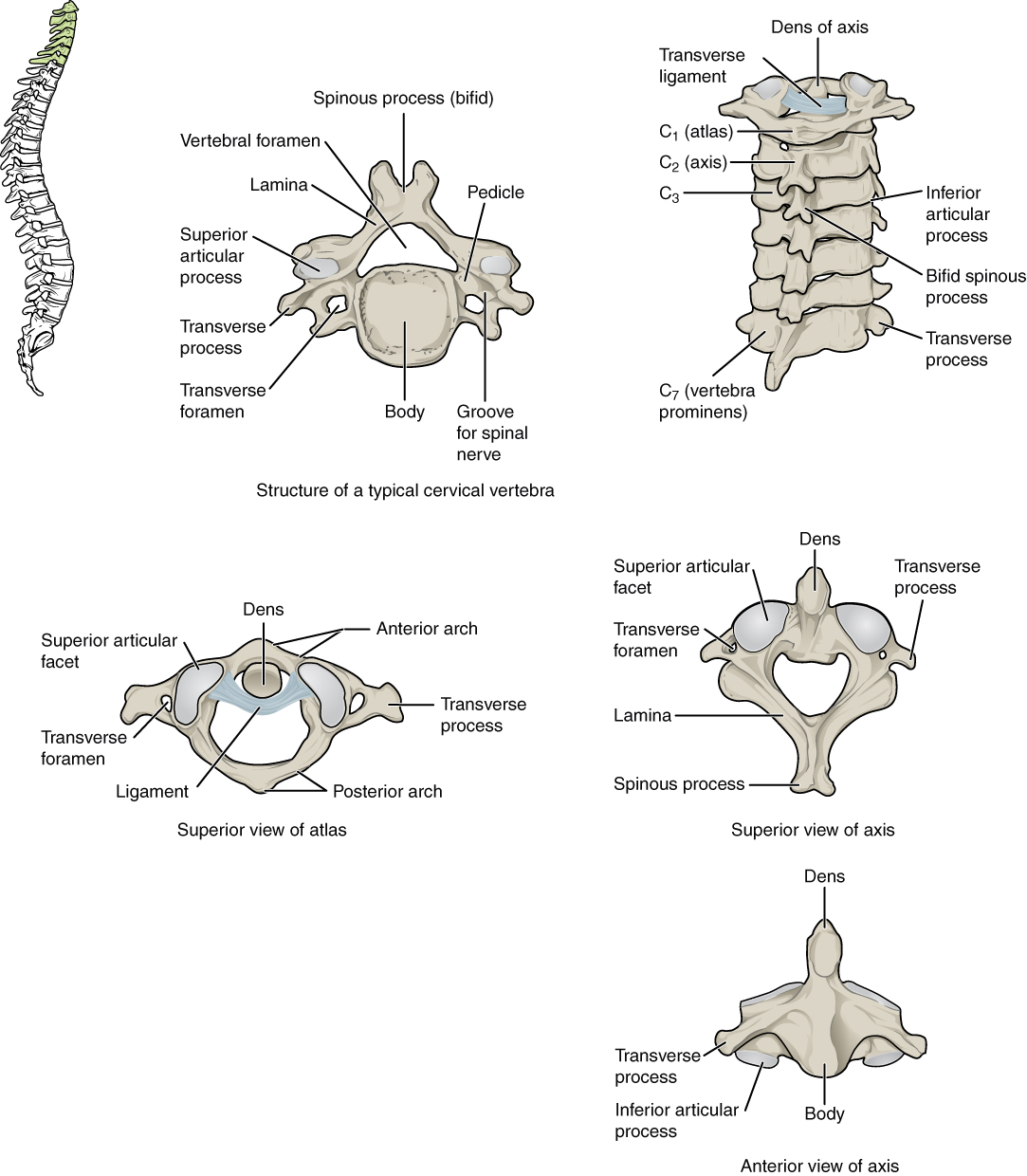
Cervical Vertebrae. A. Superior view of a typical cervical vertebra. B. Posterior view of the cervical spine. C. Superior view of C1 articulating with the dens. D. Superior view of C2. E. Anterior view of C2.
Contributed by Anatomy & Physiology, Connexions (http://cnx.org/content/col11496/1.6/, Jun 19, 2013)
(Click Image to Enlarge)
References
Cope PJ, Ourradi K, Li Y, Sharif M. Models of osteoarthritis: the good, the bad and the promising. Osteoarthritis and cartilage. 2019 Feb:27(2):230-239. doi: 10.1016/j.joca.2018.09.016. Epub 2018 Oct 25 [PubMed PMID: 30391394]
Tu C, He J, Wu B, Wang W, Li Z. An extensive review regarding the adipokines in the pathogenesis and progression of osteoarthritis. Cytokine. 2019 Jan:113():1-12. doi: 10.1016/j.cyto.2018.06.019. Epub 2018 Jun 28 [PubMed PMID: 30539776]
Piotrkowski M, Poszepczyński J, Domżalski M. Methods of Tibiofibular Syndesmosis Fixation. Ortopedia, traumatologia, rehabilitacja. 2021 Jun 30:23(3):221-228. doi: 10.5604/01.3001.0014.9258. Epub [PubMed PMID: 34187939]
Leonardi R, Ronsivalle V, Lagravere MO, Barbato E, Isola G, Lo Giudice A. Three-dimensional assessment of the spheno-occipital synchondrosis and clivus after tooth-borne and bone-borne rapid maxillary expansion. The Angle orthodontist. 2021 Nov 1:91(6):822-829. doi: 10.2319/013021-86.1. Epub [PubMed PMID: 34129666]
Breeland G, Sinkler MA, Menezes RG. Embryology, Bone Ossification. StatPearls. 2024 Jan:(): [PubMed PMID: 30969540]
Chijimatsu R, Saito T. Mechanisms of synovial joint and articular cartilage development. Cellular and molecular life sciences : CMLS. 2019 Oct:76(20):3939-3952. doi: 10.1007/s00018-019-03191-5. Epub 2019 Jun 14 [PubMed PMID: 31201464]
Hébert-Blouin MN, Tubbs RS, Carmichael SW, Spinner RJ. Hilton's law revisited. Clinical anatomy (New York, N.Y.). 2014 May:27(4):548-55. doi: 10.1002/ca.22348. Epub 2013 Nov 22 [PubMed PMID: 24272922]
Eisová S, Naňka O, Velemínský P, Bruner E. Craniovascular traits and braincase morphology in craniosynostotic human skulls. Journal of anatomy. 2021 Nov:239(5):1050-1065. doi: 10.1111/joa.13506. Epub 2021 Jul 8 [PubMed PMID: 34240418]
Level 3 (low-level) evidenceCorte-Real N, Caetano J. Ankle and syndesmosis instability: consensus and controversies. EFORT open reviews. 2021 Jun:6(6):420-431. doi: 10.1302/2058-5241.6.210017. Epub 2021 Jun 28 [PubMed PMID: 34267932]
Level 3 (low-level) evidenceAvhad G, Ghuge P. Podagra. Indian dermatology online journal. 2014 Dec:5(Suppl 2):S134-5. doi: 10.4103/2229-5178.146196. Epub [PubMed PMID: 25593807]
Dalbeth N, Gosling AL, Gaffo A, Abhishek A. Gout. Lancet (London, England). 2021 May 15:397(10287):1843-1855. doi: 10.1016/S0140-6736(21)00569-9. Epub 2021 Mar 30 [PubMed PMID: 33798500]
Weaver JS, Vina ER, Munk PL, Klauser AS, Elifritz JM, Taljanovic MS. Gouty Arthropathy: Review of Clinical Manifestations and Treatment, with Emphasis on Imaging. Journal of clinical medicine. 2021 Dec 29:11(1):. doi: 10.3390/jcm11010166. Epub 2021 Dec 29 [PubMed PMID: 35011907]
Dott C, Chin K, Compson J. Inflammatory arthritis and the elbow surgeon. Journal of clinical orthopaedics and trauma. 2021 Sep:20():101492. doi: 10.1016/j.jcot.2021.101492. Epub 2021 Jul 1 [PubMed PMID: 34277343]
Nieradko-Iwanicka B. The role of alcohol consumption in pathogenesis of gout. Critical reviews in food science and nutrition. 2022:62(25):7129-7137. doi: 10.1080/10408398.2021.1911928. Epub 2021 Apr 19 [PubMed PMID: 33866874]
Towiwat P, Li ZG. The association of vitamin C, alcohol, coffee, tea, milk and yogurt with uric acid and gout. International journal of rheumatic diseases. 2015 Jun:18(5):495-501. doi: 10.1111/1756-185X.12622. Epub [PubMed PMID: 26082349]
Syed AAS, Fahira A, Yang Q, Chen J, Li Z, Chen H, Shi Y. The Relationship between Alcohol Consumption and Gout: A Mendelian Randomization Study. Genes. 2022 Mar 22:13(4):. doi: 10.3390/genes13040557. Epub 2022 Mar 22 [PubMed PMID: 35456363]