Introduction
Pregnancy is the state of carrying a developing embryo or fetus. The human gestational period is 39 weeks and is divided into trimesters, the first spanning from week zero to week twelve. Numerous significant developmental milestones occur as the fetus develops during this time frame. Additionally, as the fetus grows, it becomes visible via ultrasonography, and laboratory testing can be performed to track progression.
Specimen Collection
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Specimen Collection
On initial presentation, pregnancy can be confirmed through beta-human chorionic gonadotropin (beta-HCG) testing of the urine or blood. This hormone comprises dissimilar alpha and beta subunits required for biological activity.[1] Levels correlate well between the serum and urine but depend on urine-specific gravity. Thus, obtaining a first void (concentrated) urine specimen is ideal. Interestingly, it appears that whole blood used on a urine pregnancy test can be accurate.[2] The serum can also be tested for early pregnancy factor (EPF), a hormone detected 48 hours after fertilization. This differs from beta-HCG, which is present after implantation, and, thus, EPF can be detected sooner.[3] Serum progesterone may also be tested, and its concentration increases linearly between weeks 5 and 13; an insignificant increase during this timeframe is associated with threatened miscarriages.[4]
While both testing types are highly sensitive and specific, the result from a single test should not be used as definitive evidence of pregnancy or lack thereof.[5] Urine testing is typically positive ten days after the missed period. False-negative urine results are seen with dilute urine, low beta-HCG levels (typically less than 25 mIU/mL), and less frequently due to the "hook effect" or "hook-like effect."[6][7] This phenomenon can be seen with high beta-HCG levels where either excess beta-HCG or its multiple fragments prevent "sandwiching" of the test's antibodies, which prevents activation of the reporter label. Suppose a falsely negative urine HCG test is suspected. In that case, a quantitative serum level of beta-HCG should be obtained, considering that the most common cause of a false-negative urine test is a low beta-HCG urine level.[6] Beta-HCG can be quantified by testing 9 days after the luteinizing hormone peak.[5] False-positive urine results can be the result of fertility drugs containing beta-HCG, malignancies, and device error.[6] It is important to note that an elevated beta-HCG level is not definitive of a normal or viable pregnancy. Conditions that result in elevated beta-HCG levels must be considered, including ectopic and heterotopic pregnancy, miscarriage, and the presence of abnormal germ cells, placental, and embryonal tissues. Evaluation of pregnancy may include serial beta-HCG titers, pelvic ultrasonography, and culdocentesis, although the latter has fallen out of favor due to poor test characteristics. Approximate doubling of beta-HCG hormone levels in 48 hours is reassuring of a viable pregnancy in the early first trimester.[5] Consideration should be given to collecting swabs of vaginal fluid in patients reporting vaginal discharge, burning, and or pain. This is especially important in pregnancy as sexually transmitted infections can pose risks to the fetus and complicate pregnancy.[8][9]
Procedures
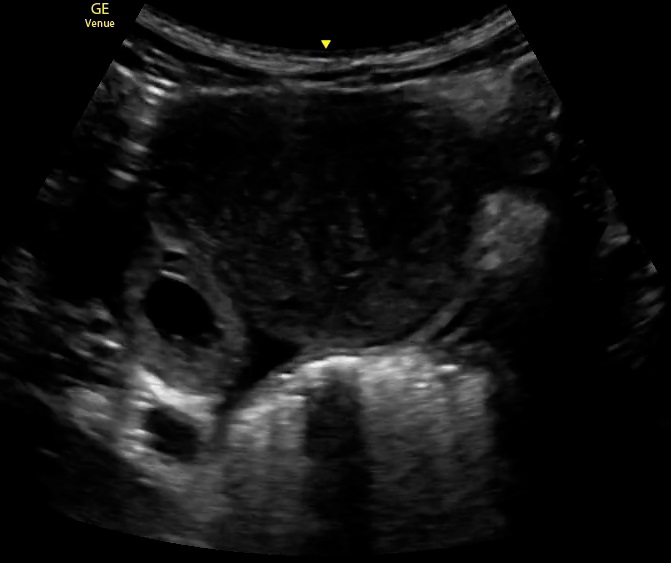
Ultrasonography is a sophisticated imaging technology that utilizes high-frequency sound waves.[10] An image is produced based on the varying echogenicity of the object being targeted and the tissue between that object and the ultrasound probe. In early pregnancy, ultrasounds are used to determine the presence of an intrauterine pregnancy (see Image. Intrauterine Pregnancy With a Yolk Sac). Additionally, ultrasound can be used to evaluate for the presence of an ectopic pregnancy (corneal, tubal, adnexal, cervical, abdominal, cesarean section ectopic), free fluid in the pelvis, uterine and adnexal pathology, fetal cardiac activity and heart rate, miscarriage, or gestational trophoblastic disease (see Image. Ectopic Pregnancy, Ultrasound).
Using ultrasound, 2 anatomical approaches are used to visualize a pregnancy: transvaginal and transabdominal. A transvaginal ultrasound is performed using a high-frequency endocavitary probe placed into the vagina and visualizing the pelvic organs through the cervix. In contrast, a transabdominal ultrasound uses a lower-frequency sound wave that can also be used to visualize pelvic organs but does so by looking through the abdominal wall with a curvilinear probe. The difference in frequency and the probe's anatomical placement during the exam results in the transvaginal approach being superior for visualizing a very early pregnancy and evaluating the adnexa. Deciding which ultrasound modality to use is multifaceted; anatomy, age, weight, and beta-HCG levels should be considered. This may also be limited by the setting (clinic, hospital, emergency dept, radiology suite, etc.) and equipment available. It is reasonable to start with a transabdominal ultrasound, which is less invasive. A full bladder is ideal for performing this study, providing an acoustic window. If the transabdominal approach is indeterminate, the transvaginal approach can be used, given its superior imaging, for the reasons discussed above. It is paramount that privacy is offered to the patient when using either form of ultrasonography. A drape should be placed to cover any external anatomy that does not need to be exposed to provide comfort and privacy to the patient.
Indications
Indications for obtaining a pregnancy test, urine, or serum include a female of child-bearing age with any of the following symptoms: amenorrhea/dysmenorrhea, abdominal/pelvic pain, nausea, vomiting, vaginal discharge, urinary symptoms, dizziness/lightheadedness/syncope, hypotension, or tachycardia. These are a sample of indications, and there are many more clinical scenarios where this information would be useful. Pregnancy status is essential to consider before the administration of potentially teratogenic medications. Indications for an emergent or urgent ultrasound in early pregnancy include a positive pregnancy test with abdominal pain, pelvic pain, or vaginal bleeding, as these may be the result of complications. Additionally, it should also be utilized in hemodynamically unstable females of child-bearing age to evaluate for sonographic evidence of ruptured ectopic pregnancy.[11] Also, ultrasound in the first trimester of pregnancy is routine for patients, and an obstetrician for dating and evaluating viability follows it.
Potential Diagnosis
In the emergency department, a positive pregnancy test should spark further evaluation, especially if the patient is reporting abdominal or pelvic pain and or vaginal bleeding.[12] Consideration must be given to the possibility of an ectopic pregnancy, a potentially life-threatening condition that occurs in approximately 2% of reported pregnancies.[13] A single beta-HCG level does not provide information on whether a pregnancy is intrauterine. An emergent ultrasound should be performed for any pregnant female in whom ectopic pregnancy is suspected. Ultrasound may demonstrate an intrauterine pregnancy, an ectopic pregnancy, findings suggestive of an extrauterine pregnancy (solid or complex adnexal mass), or might be indeterminate.[14] The ultrasound may identify free fluid in the abdomen or pelvis concerning a ruptured ectopic. Once an intrauterine pregnancy is identified on ultrasound, the presence of a concomitant extrauterine pregnancy, also known as a heterotopic pregnancy, is highly unlikely in the general population, with estimates ranging from approximately 1 per 8,000 to 1 per 30,000 pregnancies.[15] This does not apply to those with risk factors for heterotopic, such as receiving fertility medications, history of ectopic, or history of pelvic inflammatory disease.
If the ultrasound results are indeterminate, the "discriminatory zone" can help clinically correlate the ultrasound findings with the beta-HCG level. The discriminatory zone is the approximate beta-HCG threshold where an intrauterine pregnancy can typically be identified by ultrasound. Transvaginal ultrasound has high sensitivity when beta-HCG levels are above 1,500 mIU/mL, while the threshold is much higher using the transabdominal approach (approximately 6,000 mIU/mL).[16] If a symptomatic patient has an indeterminate ultrasound with a beta-HCG above the "discriminatory zone," the diagnosis of ectopic pregnancy must be considered, and consultation with OB/GYN is recommended. If the patient has an indeterminate ultrasound and the beta-HCG is less than the discriminatory zone, and the patient is hemodynamically stable without significant pain or vaginal bleeding, she should be directed to have a quantitative serum beta-HCG level repeated in 48 hours. If this repeat level rises, ideally doubling every 48 hours, this is highly suggestive of a normal pregnancy. In contrast, if the beta-HCG level is declining or not doubling in 48 hours, miscarriage or failed pregnancy should be suspected.
Normal and Critical Findings
Products of conception in a normal pregnancy should be identifiable via transvaginal ultrasound when the beta-HCG level is above 1,500 mIU/mL. Fetal heart tones can be appreciated between 6 and 8 weeks of gestation. Between 8 and 10 weeks of gestation, the provider can obtain important information about the pregnancy, including placental location, fetal position and anatomy, amniotic fluid volume, and maternal anatomy, including dimensions of the cervix and uterus. It is noted that anatomic abnormalities diagnosed within the early first trimester are often by chance, while late first trimester diagnoses are typically made during the anatomic ultrasound scans.[17] Ultrasound images that do not reveal an intrauterine pregnancy with beta-HCG levels either at or above the discriminatory zone should raise concern for abnormal pathology, including ectopic pregnancy, heterotopic pregnancy, and mass. Similarly, adnexal masses also warrant further investigation. Also, free fluid in the abdominal and pelvis should be taken seriously, especially in a hemodynamically unstable patient. A ruptured ectopic pregnancy must remain on the differential, and obstetrics should be contacted emergently.
Interfering Factors
It is important to gather a complete past medical and surgical history when evaluating for pregnancy and diagnosing an intrauterine pregnancy. Pelvic inflammatory disease, an intrauterine device (IUD), prior ectopic pregnancies, and dysplasia are all risk factors for ectopic pregnancies. Additionally, infertility treatment increases the risk of heterotopic pregnancies. It should also be noted that favorable visualization using transabdominal ultrasound of the reproductive organs can be limited by a large body habitus and an empty bladder. A full bladder offers an ideal acoustic window for a transabdominal ultrasound. Ultrasound is a modality that is user-dependent. Limitations to serum or urine qualitative HCG testing were described above (see specimen collection).
Complications
The list of early pregnancy complications is vast, including ectopic pregnancy, heterotopic pregnancy, molar pregnancy, and miscarriage. The provider needs to visualize an intrauterine pregnancy for reasons discussed in prior sections. Complications resulting from ultrasonography in early pregnancy are minor. Transvaginal ultrasound may cause vaginal and or cervical discomfort during the exam, especially in the setting of a gynecologic infection. Given the theoretical risks of harm to the fetus, the principle of ALARA (as low as reasonably achievable) should be practiced by limiting scan time, avoiding the use of Doppler, etc. However, the consensus is that ultrasonography is a safe diagnostic tool for both the patient and the fetus.
Patient Safety and Education
It is important to discuss the results with the patient upon pregnancy diagnosis. It is essential to determine whether the pregnancy was desired, if the patient has a strong support system if she feels safe in her current living conditions, and what resources she has available. The medical team should provide the patient with appropriate protection and resources. Patients with confirmed intrauterine pregnancies in the emergency department should be directed to follow up with an obstetrician. A healthcare professional must follow pregnancy. Regular imaging via ultrasound is the standard of care in the United States to monitor fetal development. Additionally, genetic testing is also part of routine pregnancy care. High-risk pregnancies are considered to be those that pose a potential health or life risk to the mother or fetus.[18] Examples of such factors include advanced maternal age, autoimmune diseases, infectious diseases, diabetes, prior miscarriages, or substance abuse. Close monitoring by healthcare professionals is paramount to minimize the risks to the mother and fetus.[19]
Patients should be encouraged to start or continue to take prenatal vitamins; some patients may need additional folic acid supplementation if their fetus is at increased risk of neural tube defects, as per the American College of Obstetricians and Gynecologists. In the case of a patient with an indeterminate first-trimester ultrasound with an initial beta-HCG level under the discriminatory zone, the hemodynamic patient should be instructed to return in 48 hours for repeat beta-HCG level testing. If this same patient is unstable, an emergent OB/GYN consultation is needed, as ruptured ectopic is the most worrisome consideration. Hemodynamically stable patients with ultrasound findings concerning ectopic pregnancy (not ruptured), mass, or other complications should be directed to an obstetrician.
Clinical Significance
A pregnancy test is 1 of the most important tests to obtain in any female of child-bearing age complaining of abdominal/pelvic pain, amenorrhea, vaginal bleeding, or that is hemodynamically unstable. It is a highly sensitive and specific test, but limitations should be understood. If positive for pregnancy, ectopic pregnancy must be considered as a possibility. Ultrasonography is a widely used imaging tool in early pregnancy due to its accuracy and favorable safety profile for both the patient and fetus. Information on the ultrasound should be interpreted within the clinical context of the patient and the beta-HCG level.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Montagnana M, Trenti T, Aloe R, Cervellin G, Lippi G. Human chorionic gonadotropin in pregnancy diagnostics. Clinica chimica acta; international journal of clinical chemistry. 2011 Aug 17:412(17-18):1515-20. doi: 10.1016/j.cca.2011.05.025. Epub 2011 May 25 [PubMed PMID: 21635878]
Fromm C, Likourezos A, Haines L, Khan AN, Williams J, Berezow J. Substituting whole blood for urine in a bedside pregnancy test. The Journal of emergency medicine. 2012 Sep:43(3):478-82. doi: 10.1016/j.jemermed.2011.05.028. Epub 2011 Aug 27 [PubMed PMID: 21875776]
Igarashi S. [Clinical significance of early pregnancy factor]. Nihon Sanka Fujinka Gakkai zasshi. 1986 Jun:38(6):896-902 [PubMed PMID: 2426377]
Ku CW, Allen JC Jr, Lek SM, Chia ML, Tan NS, Tan TC. Serum progesterone distribution in normal pregnancies compared to pregnancies complicated by threatened miscarriage from 5 to 13 weeks gestation: a prospective cohort study. BMC pregnancy and childbirth. 2018 Sep 5:18(1):360. doi: 10.1186/s12884-018-2002-z. Epub 2018 Sep 5 [PubMed PMID: 30185145]
Stephenson JN. Pregnancy testing and counseling. Pediatric clinics of North America. 1989 Jun:36(3):681-96 [PubMed PMID: 2660091]
Gnoth C, Johnson S. Strips of Hope: Accuracy of Home Pregnancy Tests and New Developments. Geburtshilfe und Frauenheilkunde. 2014 Jul:74(7):661-669 [PubMed PMID: 25100881]
Griffey RT, Trent CJ, Bavolek RA, Keeperman JB, Sampson C, Poirier RF. "Hook-like effect" causes false-negative point-of-care urine pregnancy testing in emergency patients. The Journal of emergency medicine. 2013 Jan:44(1):155-60. doi: 10.1016/j.jemermed.2011.05.032. Epub 2011 Aug 10 [PubMed PMID: 21835572]
Fontenot HB, George ER. Sexually transmitted infections in pregnancy. Nursing for women's health. 2014 Feb-Mar:18(1):67-72. doi: 10.1111/1751-486X.12095. Epub [PubMed PMID: 24548498]
Silasi M, Cardenas I, Kwon JY, Racicot K, Aldo P, Mor G. Viral infections during pregnancy. American journal of reproductive immunology (New York, N.Y. : 1989). 2015 Mar:73(3):199-213. doi: 10.1111/aji.12355. Epub 2015 Jan 13 [PubMed PMID: 25582523]
Level 3 (low-level) evidenceWhitworth M, Bricker L, Mullan C. Ultrasound for fetal assessment in early pregnancy. The Cochrane database of systematic reviews. 2015 Jul 14:2015(7):CD007058. doi: 10.1002/14651858.CD007058.pub3. Epub 2015 Jul 14 [PubMed PMID: 26171896]
Level 1 (high-level) evidenceKnez J, Day A, Jurkovic D. Ultrasound imaging in the management of bleeding and pain in early pregnancy. Best practice & research. Clinical obstetrics & gynaecology. 2014 Jul:28(5):621-36. doi: 10.1016/j.bpobgyn.2014.04.003. Epub 2014 Apr 24 [PubMed PMID: 24841987]
Mausner Geffen E, Slywotzky C, Bennett G. Pitfalls and tips in the diagnosis of ectopic pregnancy. Abdominal radiology (New York). 2017 May:42(5):1524-1542. doi: 10.1007/s00261-016-1020-4. Epub [PubMed PMID: 28144719]
Belics Z, Gérecz B, Csákány MG. [Early diagnosis of ectopic pregnancy]. Orvosi hetilap. 2014 Jul 20:155(29):1158-66. doi: 10.1556/OH.2014.29933. Epub [PubMed PMID: 25016448]
Brown DL, Doubilet PM. Transvaginal sonography for diagnosing ectopic pregnancy: positivity criteria and performance characteristics. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 1994 Apr:13(4):259-66 [PubMed PMID: 7932989]
Level 1 (high-level) evidenceReece EA, Petrie RH, Sirmans MF, Finster M, Todd WD. Combined intrauterine and extrauterine gestations: a review. American journal of obstetrics and gynecology. 1983 Jun 1:146(3):323-30 [PubMed PMID: 6344638]
Barnhart KT, Simhan H, Kamelle SA. Diagnostic accuracy of ultrasound above and below the beta-hCG discriminatory zone. Obstetrics and gynecology. 1999 Oct:94(4):583-7 [PubMed PMID: 10511363]
Blaas HG. Detection of structural abnormalities in the first trimester using ultrasound. Best practice & research. Clinical obstetrics & gynaecology. 2014 Apr:28(3):341-53. doi: 10.1016/j.bpobgyn.2013.11.004. Epub 2013 Dec 4 [PubMed PMID: 24355991]
Holness N. High-Risk Pregnancy. The Nursing clinics of North America. 2018 Jun:53(2):241-251. doi: 10.1016/j.cnur.2018.01.010. Epub 2018 Apr 7 [PubMed PMID: 29779516]
Coco L, Giannone TT, Zarbo G. Management of high-risk pregnancy. Minerva ginecologica. 2014 Aug:66(4):383-9 [PubMed PMID: 25020057]