Introduction
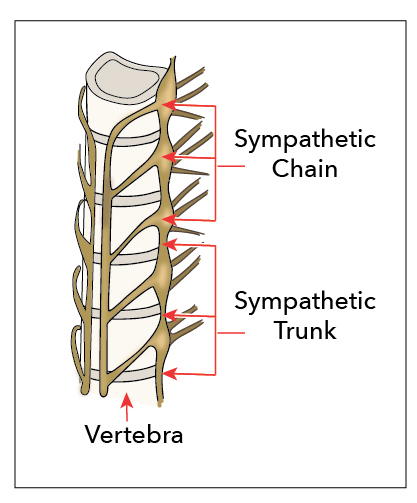
The sympathetic chain is a ganglionated chain present bilaterally extending from the base of the skull to the coccyx. It divides into cervical, thoracic, lumbar and sacral segments. The two side chains fuse at the ganglion in front of the sacrococcygeal junction. In this article, the lumbar sympathetic chain is discussed in detail below.
Location and relations: It presents four interconnected ganglia, on either side. Lumbar sympathetic chain lies anterolateral to the bodies of lumbar vertebrae, deep to the medial aspect of the psoas major muscle.
- Superiorly it is continuous with the thoracic sympathetic chain passing behind the medial arcuate ligament of a diaphragm
- Inferiorly it passes behind the common iliac vessels over the sacral ala and continuous with the sacral sympathetic chain
- On the right side, it lies posterior to inferior vena cava
- On the left, it lies postero-lateral to the aortic lymph nodes
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The lumbar sympathetic chain receives input from the first, second and the third lumbar sometimes are connected by the white rami communicantes, which contain the preganglionic neurons from the lateral horn of the spinal cord.
All lumbar spinal nerves close to the beginning of their ventral rami join by grey rami communicantes from the ganglia that contain postganglionic neurons. They supply the skin and vessels in the respective territory. Grey rami may leave the sympathetic trunk between the ganglia to form plexuses around the neighboring arteries to reach the target organs. Sympathetic trunk branches accompany lumbar, aorta, common, internal and external iliac arteries. The adrenal medulla is a unique structure in the body that it receives supply from the preganglionic neurons from T10 to L1 spinal segments.
The non-relayed preganglionic neurons emerge from the medial side of the sympathetic trunk as lumbar splanchnic nerves. Four lumbar splanchnic nerves arise from sympathetic trunk to join the coeliac, inferior mesenteric and superior hypogastric plexuses. First lumbar splanchnic nerve arises from the first ganglion gives branches to coeliac, renal and inferior mesenteric plexuses. The second nerve comes from the second ganglion joins the intermesenteric or inferior mesenteric plexuses. The third nerve emerges from the third or fourth ganglion joins the superior hypogastric plexuses. The fourth nerve is given from the fourth ganglion and joins with the lower part of superior hypogastric plexus.
Microscopic structure: Autonomic ganglia contain the ganglionic neurons, satellite glial cells, and small intensely fluorescent cells. Ganglionic neurons form many axodendritic synapses with preganglionic axons. Satellite glial cells are closely associated with neurons; they may influence synaptic transmission. Small intensely fluorescent cells possess several granules that contain noradrenaline, dopamine, and serotonin. Sympathetic ganglia contain multipolar neurons, preganglionic sympathetic axons synapse with many postganglionic neurons which is responsible for the widespread effects of the sympathetic activity.
Preganglionic sympathetic neurons release acetylcholine as the neurotransmitter, whereas noradrenaline is the neurotransmitter in postganglionic neurons. The postganglionic neurons are non-myelinated; they reach the target organs in several ways. They will return to the spinal nerves through grey rami communicantes, then distribute through ventral and dorsal rami to blood vessels, sweat glands, and hairs in their territory. In addition, they also travel via a medial branch to the viscera or innervate blood vessels or form plexuses on them to reach their periphery. The majority of the fibers accompany arteries and ducts to reach the distant effectors.
The postganglionic sympathetic fibers are vasoconstricting to blood vessels, secretomotor to sweat glands, and motor to arrector pili muscle. The fibers which follow the motor nerves to skeletal muscle are a vasodilator. The fibers which reach the viscera are responsible for general vasoconstriction, regulation of glandular secretion, and inhibition of smooth muscle contraction in the gastrointestinal system.
General visceral afferent fibers from the viscera and blood vessels follow their efferent fibers. They are the peripheral processes of pseudo-unipolar neurons situated in the dorsal root ganglion of thoracic and upper two lumbar spinal nerves. Visceral afferent fibers which enter the spinal cord through spinal nerve roots terminate in the gray matter. They form connections with CNS that controls autonomic reflex functions. Visceral pain is felt near the viscera or in a cutaneous area or other tissue whose somatic afferents enter the spinal segments that receiving visceral afferents from viscera, the explanation underlying the referred pain.
Embryology
Sympathetic ganglia and nerves except the preganglionic neurons form from the neural crest cells. During neurulation, the neural crest cells migrate to cranial, vagal, trunk and lumbosacral areas. Trunk neural crest population gives rise to sympathetic ganglia. Neural crest cells migrate ventrally to the area of future paravertebral and prevertebral plexuses forming the sympathetic chain and major ganglia around the ventral branches of the abdominal aorta.
Blood Supply and Lymphatics
Medial branches of the lumbar arteries will give ganglionic branches that supply the sympathetic ganglia and trunk. Veins drain into the corresponding lumbar veins. Lymphatics drain into lateral aortic lymph nodes.
Physiologic Variants
Lumbar sympathetic chain shows variations in its position and number of ganglia. Rami communicantes of lumbar sympathetic chain crossed the common iliac arteries and joined in front of first sacral vertebra.[1] The number of ganglia in a single chain varied from 2 to 6 with a mean of 3.9.[2] Sympathetic chain passed posterior to the crus of a diaphragm in the majority of the cases, in a few instances, it passed behind the medial arcuate ligament.[3] Hyperactivity of the sympathetic nervous system could be the cause of reflex sympathetic dystrophy/complex regional pain syndrome.
Surgical Considerations
Conventionally, the lumbar sympathetic chain is accessible through transperitoneal and retroperitoneal approaches. However, a novel, minimally invasive, a lateral peritoneal approach was also found safe and effective for sectioning of the sympathetic chain.[4] Retroperitoneoscopic resection technique was also successful in lumbar sympathectomy,[5] although the lumbar sympathetic chain is at risk while approaching an anterior lumbar spine through retroperitoneal oblique approach between psoas major muscle and aorta.[6] During chemical lumbar sympathectomy, the puncture needle tip is placed in front of psoas major muscle inactivating agent is injected around the sympathetic chain. This procedure is associated with ureteropelvic damage, hence the introduction of selective chemical lumbar sympathectomy in which gray rami communicantes are the targets.[7]
Clinical Significance
A sympathetic block is performed to treat several vascular disorders,[8] lumbar sympathectomy is indicated to improve blood circulation in vasospastic disorders like Raynaud disease.[9] It is advised to improve distal circulation to the extent that amputation can be avoided and in cases where vascular reconstruction is not available, such as Buerger disease.[10] It is the choice of treatment in idiopathic plantar hyperhidrosis,[11] frostbite,[12] reflex sympathetic dystrophy and complex regional pain syndrome.[13][8] The lumbar sympathectomy destroys sensory and vasomotor fibers as evidenced by relief of rest pain and increased blood flow.[14] For the sympathetic block, the medial border of the psoas major acts as a guide for needle placement at the level of L3 where there is consistency in its relation in people with spondylophytes. Complications of the procedure are significantly reduced with radiography guided needle insertion.[15]
Media
(Click Image to Enlarge)
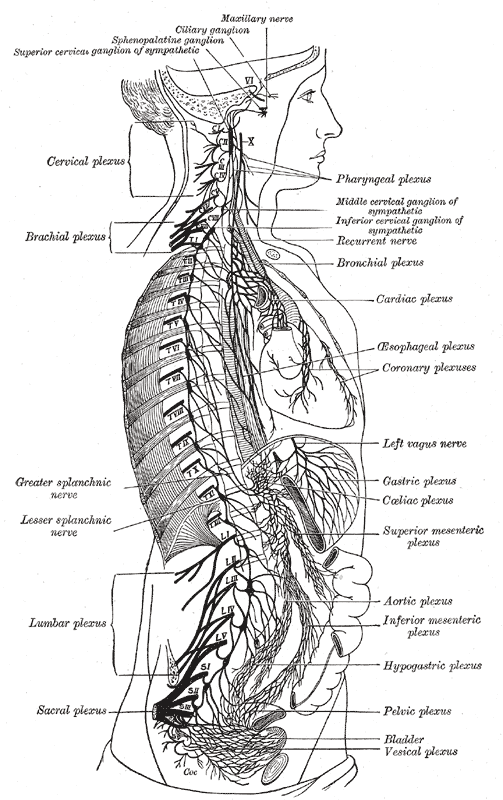
The Sympathetic Nerves. The illustration shows the right sympathetic chain and its connections with the thoracic, abdominal, and pelvic plexuses.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Jain P, Raza K, Singh S, Kumari C, Kaler S, Rani N. Lumbar sympathetic chain: anatomical variation and clinical perspectives. La Clinica terapeutica. 2016 Nov-Dec:167(6):185-187. doi: 10.7417/CT.2016.1970. Epub [PubMed PMID: 28051823]
Level 3 (low-level) evidenceMurata Y, Takahashi K, Yamagata M, Takahashi Y, Shimada Y, Moriya H. Variations in the number and position of human lumbar sympathetic ganglia and rami communicantes. Clinical anatomy (New York, N.Y.). 2003 Mar:16(2):108-13 [PubMed PMID: 12589664]
Gandhi KR, Verma VK, Chavan SK, Joshi SD, Joshi SS. The morphology of lumbar sympathetic trunk in humans: a cadaveric study. Folia morphologica. 2013 Aug:72(3):217-22 [PubMed PMID: 24068683]
Rodgers SD, Engler JA, Perin NL. A novel approach to the lumbar sympathetic chain: lateral access. Neurosurgical focus. 2013 Jul:35(2 Suppl):Video 12. doi: 10.3171/2013.V2.FOCUS13204. Epub [PubMed PMID: 23829842]
Rieger R, Pedevilla S. Retroperitoneoscopic lumbar sympathectomy for the treatment of plantar hyperhidrosis: technique and preliminary findings. Surgical endoscopy. 2007 Jan:21(1):129-35 [PubMed PMID: 16960674]
Mahatthanatrakul A, Itthipanichpong T, Ratanakornphan C, Numkarunarunrote N, Singhatanadgige W, Yingsakmongkol W, Limthongkul W. Relation of lumbar sympathetic chain to the open corridor of retroperitoneal oblique approach to lumbar spine: an MRI study. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2019 Apr:28(4):829-834. doi: 10.1007/s00586-018-5779-6. Epub 2018 Oct 16 [PubMed PMID: 30327910]
Wang WH, Zhang L, Dong GX, Zhao J, Li X. Targeting Gray Rami Communicantes in Selective Chemical Lumbar Sympathectomy. Journal of visualized experiments : JoVE. 2019 Jan 10:(143):. doi: 10.3791/58894. Epub 2019 Jan 10 [PubMed PMID: 30688314]
Bale R. [Ganglion block. When and how?]. Der Radiologe. 2015 Oct:55(10):886-95. doi: 10.1007/s00117-015-0015-4. Epub [PubMed PMID: 26384294]
Janoff KA, Phinney ES, Porter JM. Lumbar sympathectomy for lower extremity vasospasm. American journal of surgery. 1985 Jul:150(1):147-52 [PubMed PMID: 4014566]
Perez-Burkhardt JL, Gonzalez-Fajardo JA, Martin JF, Carpintero Mediavilla LA, Mateo Gutierrez AM. Lumbar sympathectomy as isolated technique for the treatment of lower limbs chronic ischemia. The Journal of cardiovascular surgery. 1999 Feb:40(1):7-13 [PubMed PMID: 10221378]
Level 2 (mid-level) evidenceLima SO, de Santana VR, Valido DP, de Andrade RLB, Fontes LM, Leite VHO, Neto JM, Santos JM, Varjão LL, Reis FP. Retroperitoneoscopic lumbar sympathectomy for plantar hyperhidrosis. Journal of vascular surgery. 2017 Dec:66(6):1806-1813. doi: 10.1016/j.jvs.2017.05.126. Epub [PubMed PMID: 29169540]
Taylor MS. Lumbar epidural sympathectomy for frostbite injuries of the feet. Military medicine. 1999 Aug:164(8):566-7 [PubMed PMID: 10459266]
Bandyk DF, Johnson BL, Kirkpatrick AF, Novotney ML, Back MR, Schmacht DC. Surgical sympathectomy for reflex sympathetic dystrophy syndromes. Journal of vascular surgery. 2002 Feb:35(2):269-77 [PubMed PMID: 11854724]
Level 2 (mid-level) evidenceCoventry BJ, Walsh JA. Cutaneous innervation in man before and after lumbar sympathectomy: evidence for interruption of both sensory and vasomotor nerve fibres. ANZ journal of surgery. 2003 Jan-Feb:73(1-2):14-8 [PubMed PMID: 12534731]
Feigl GC, Kastner M, Ulz H, Breschan C, Dreu M, Likar R. Topography of the lumbar sympathetic trunk in normal lumbar spines and spines with spondylophytes. British journal of anaesthesia. 2011 Feb:106(2):260-5. doi: 10.1093/bja/aeq345. Epub 2010 Dec 7 [PubMed PMID: 21138903]