Introduction
The Achilles tendon, also known as the triceps surae, ranks as the strongest and largest tendon in the human body.[1] This tendon connects the aponeuroses of the gastrocnemius, soleus, and plantaris muscles to the calcaneus bone.[2] A sheath-like structure comprised of a single layer of cells surrounds the tendon; this is not a true synovial sheath but rather a “fake sheath” called paratenon.[2][3][4] The paratenon supplies a significant portion of the blood supply to the tendon.[4]
Studies have identified a hypovascular area susceptible to injury, located approximately 2 to 6 cm proximal to calcaneal insertion.[5] The Achilles tendon is essential for enabling calf muscles to exert force on the heel, which is necessary for walking or running.[6]
Various factors can contribute to Achilles tendon injuries, with specific locations being more commonly affected. This activity explores insertional and non-insertional tendonitis, paratenonitis, and tendon rupture.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The causes and mechanisms of Achilles tendinopathy include the following:
- Intrinsic factors: These include anatomic factors, age, sex, metabolic dysfunction,[7] foot cavity, dysmetria, muscle weakness, imbalance, gastrocnemius dysfunction,[8] anatomical variation of the plantaris muscle,[9] tendon vascularization,[10] torsion of the Achilles tendons,[11] slippage of the fascicle,[12] and lateral instability of the ankle.
- Extrinsic factors: These include mechanical overload, constant effort, inadequate equipment,[13] obesity,[14] medications (corticosteroids, anabolic steroids, fluoroquinolones),[15][16] improper footwear, insufficient warming or stretching,[17] hard training surfaces, and direct trauma, among others.[18]
Several factors increase the risk of Achilles tendon rupture, including older age, tendon inhomogeneity, fascicle slippage, and excessive exercise in athletes.[19] Sports-minded individuals tend to have an injury at the Achilles tendon insertion site.[20]
Epidemiology
The Achilles tendon has a cumulative lifetime injury incidence of approximately 24% in athletes. Running-related injuries have a prevalence between 11% and 85% or 2.5 to 59 injuries per 1,000 hours of running.[21] Results from one study cite the frequency of Achilles tendinopathy to be 1 to 2% in elite adolescent athletes.[22] Another study cited the frequency of injury as 9% in recreational athletes.[23] The lifetime injury incidence of 2.35 per 1000 is strongly associated with sporting activities.[24][25][26] This incidence increases in older men.[27] The overall incidence rate of Achilles tendinopathy ruptures is 2.1 per 100,000 person-years, and most AT ruptures occur in males, with a 3.5:1 male-to-female ratio.[28]
Pathophysiology
The Achilles tendon consists of 2 tendinous portions. One is located proximally, and another gradually merges distally, forming a single, homogenous tendon. It comprises 3 muscular heads; the soleus is monoarticular, and the plantaris and gastrocnemius are biarticular. The mechanical tension of the tendon is concentrated at 2 sites. These are the medial or central portion of the paratenon and the middle segment of the tendon, which is the most common site of injury.[29]
As the Achilles tendon descends from its origin, it twists counterclockwise on the right and clockwise on the left, rotating 90°.[30] This makes smaller soleus fibers insert anteromedially while larger gastrocnemius fibers insert posterolaterally. This configuration is thought to contribute to an alteration in the biomechanics of the tendon and influence the pathophysiologic mechanisms of Achilles tendinopathies.[2][12]
In insertional Achilles tendinopathy cases, the tendon's degeneration is characterized by loss of strong parallel collagen I fibers, fatty infiltration, and capillary proliferation.[2][31] This is seen as a thickening of the tendon in advanced imaging and will be further discussed in the next sections.
Histopathology
The Achilles tendon comprises 95% type I collagen fibers;[31] these fibers are very strong and flexible. A decrease in type I collagen fibers can happen with normal aging or injury. Tendinopathy, encompassing both tendinosis and tendinitis, increases proteoglycans, water content, and disorganized type III collagen.[31]
The tendon is enveloped in a thin layer of connective tissue called the paratenon, rich in elastin, and extends into the tendon, binding the collagen bundles together while permitting movement among them.[32]
Their respective characteristics distinguish tendinosis and tendinitis. Tendinosis involves degenerative changes in the structure of the tendon and its sheath, making it more vulnerable and prone to breaking. At the cellular level, no evidence recent or acute inflammatory process is observed. In contrast, tendinitis is marked by an acute inflammatory response resulting from acute trauma, excessive use, or lack of training.[33]
Paratenonitis is an inflammation affecting the outer layers of the tendon and includes conditions such as tenosynovitis and tenovaginitis.[34] This pathologic condition results in edema and exudate formation accompanied by inflammatory cells. Subsequently, a fibrinous exudate develops, leading to crepitus and restriction of the tendon's movement within the sheath. If left untreated, it can progress to a chronic state by developing an immature connective tissue that expands an organized fibrin network known as adhesions.[35]
In a study conducted on rats, it was observed that the microenvironment of the Achilles tendon promoted the differentiation of stem cells towards chondrogenic and osteogenic lineages, which predispose to tendon rupture (tendinosis). Following this rupture, an inflammatory cascade begins, leading to elevated expression of proinflammatory cytokine mRNA, including matrix metalloproteinase-3 (MMP-3), cyclooxygenase-2 (COX-2), interleukin-6 (IL-6), and necrosis factor tumor alpha (TNF-a).[36]
Chronic inflammation, on the other hand, triggers neovascularization, which promotes the risk of tendon rupture, resulting in increased disability and complexity to its management.[37] In a study with rats, researchers noted that denervated tendons expressed morphological alterations such as disorganization of the collagen network, increased production of type III collagen, hypercellularity, disfigured cell morphology, and elevated expression of NK-1R. These changes resemble those observed in Achilles tendon injuries.[38]
History and Physical
The term "Achilles tendinopathy" refers to tendinitis (acute inflammation) and tendinosis (chronic inflammation). Achilles tendinopathy is characterized by pain, inflammation, and Achilles tendon stiffness.[39][40][41] This condition can occur in athletes and nonathlete patients, usually due to an imbalance between muscle power and tendon elasticity.[42] Achilles tendinopathies are divided anatomically into insertional and non-insertional tendinopathies.
Insertional Achilles tendinopathy is the condition that affects the tendon's osseous attachment to the posterior calcaneus. Patients with this condition will experience pain in the distal third of the tendon, extending up to its insertion. They may also experience morning stiffness.[43]
Non-insertional Achilles tendinopathy occurs in the mid to proximal third of the tendon (2-6 cm proximal to the insertion). When palpated, nodules may be noticeable, and the tendon may exhibit enlargement.[43]
Evaluation
The diagnosis of Achilles tendinopathy mainly relies on physical examination.[44] The patient should be evaluated while standing and in a prone position for specific clinical signs of localized pain, focal or diffuse sensitivity, swelling, stiffness, and perceived rigidity in the Achilles tendon.[44] Clinical tests include:
- Arc sign: Swelling or nodules within the tendon are palpated while the ankle joint is moved in plantarflexion and dorsiflexion. A positive arc sign is observed when the swelling or nodules move with the range of motion.[42][44][45] In cases of paratendinopathy, the area of maximum thickening remains fixed in one position.[44]
- Royal London Hospital test: The point of maximum tenderness is palpated when the ankle is in a neutral position. The patient is then instructed to dorsiflex and plantarflex the ankle joint actively. The previous area of maximum tenderness is again palpated when the ankle joint is in maximum plantarflexion and dorsiflexion. Tendinopathy is present when the tenderness significantly decreases or disappears when the tendon is under tension.[42][44]
Tests Used to Diagnose Achilles Tendinopathy
- Lateral and Axial Calcaneus X-rays: These imaging studies may reveal calcifications in the proximal extension of the tendon insertion or bony prominences in the upper portion of the calcaneus. Also, x-rays are useful in excluding pathological bone tumors.[46][47][48]
- Ultrasound: This is a valuable tool for evaluating tendon injuries and assessing the risk of tendinopathy and rupture.[49][50] It may provide information such as an increased thickness of the Achilles tendon, hyperemia associated with hypervascularity, a decrease in the gastrocnemius-soleus rotation angle, and a reduction in the length of the Kager fat pad. Ultrasound is also useful during interventional treatment.[51] Besides being easily accessible with a large volume of tissue, the Achilles tendon can be dynamically evaluated through its range of motion with an ultrasound.[52]
- Insertional Achilles tendinopathy: hypoechoic area and loss of fibrillar appearance at the distal third of the tendon.[43]
- Noninsertional Achilles tendinopathy: focal or diffuse thickening of the mid to proximal section of the tendon; also contains hypoechoic areas with loss of compact linear fibrillar appearance.[43]
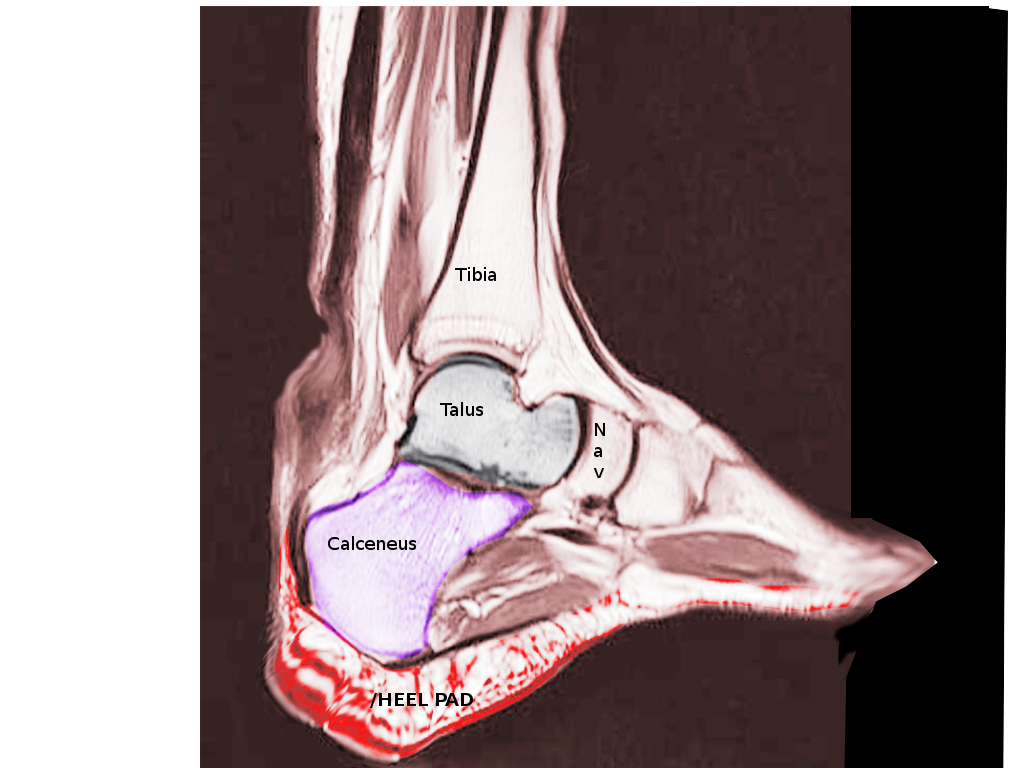
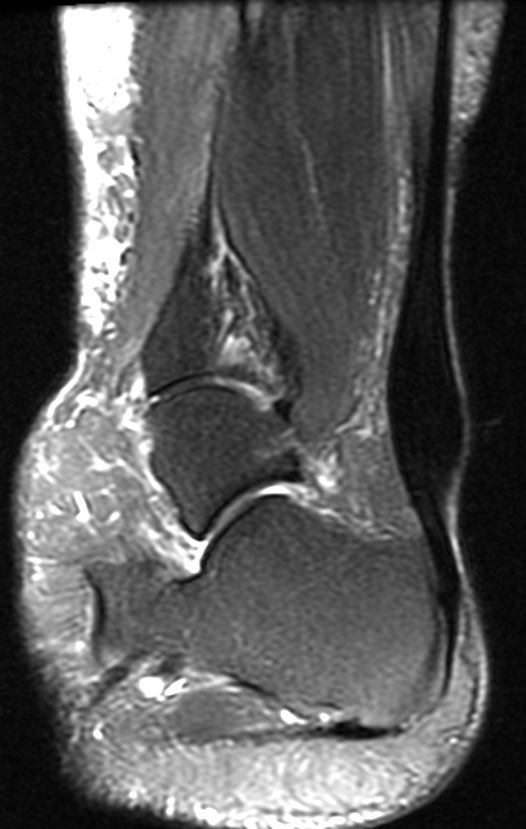
- Magnetic Resonance Imaging (MRI): This imaging modality offers comprehensive information about the condition of joint structures, enabling studies in multiple planes and static and dynamic views.[53][54] The normal Achilles tendon is less than 7 mm thick from anterior to posterior on a sagittal MRI. Increased measurements suggest chronic intrasubstance tendinopathy and degeneration.[55] One study found that MRI had lower sensitivity than ultrasound in detecting early changes of enthesopathy.[56] However, another study demonstrated excellent agreement between tendon thickness measurements obtained from magnetic resonance and ultrasound.[57]
Treatment / Management
Management of Achilles tendinopathy can be divided into conservative and surgical approaches, considering whether acute or chronic. In cases of a full rupture, surgical treatment is usually recommended.
Conservative Therapy
Conservation therapy is first-line management of Achilles tendinitis and includes the following:[63][64][65][66][67][68][69][70](A1)
- Reduction of activity levels.[71]
- Administration of nonsteroidal anti-inflammatory drugs (NSAIDs).[72][73]
- The rehabilitation process for Achilles tendinopathy can be enhanced by adapting footwear and applying manual therapy targeted at specific local sites.[74]
- Eccentric stretching exercises should be an integral component of physiotherapy and can achieve a 40% reduction in pain. Moderate-level evidence favors eccentric exercise over concentric exercise for reducing pain.[63][64][65] Eccentric exercises for chronic insertional Achilles tendinopathy are less effective in patients with metabolic syndrome but most effective when combined with extracorporeal shockwave therapy.[75]
- Tendon loading exercise at short- and long-term follow-up[66][67][68]
- If unresponsive to initial management, extracorporeal shock wave therapy (ESWT) has reduced pain by 60% and achieved 80% patient satisfaction, improving the functionality and quality of life.[69] ESWT has received a grade B strength of recommendation and has been shown to provide effective short-term pain relief and tendon healing, making it the first choice treatment for some healthcare professionals.[59][75] The combination of ESWT with eccentric exercises has been found to yield the best results.[75]
- Physiotherapy has been found to improve pain and functionality in cases of Achilles tendinopathy affecting the middle portion. However, studies do not indicate a preference for any particular exercise over others. Therefore, the use of a splint combined with an eccentric exercise protocol or orthoses to improve pain and function is not currently recommended.[65]
- Biologics
- Platelet-rich plasma (PRP): autologous treatment that contains many growth factors. Meta-analysis and recent studies have shown no improved effectiveness between PRP and placebo groups and no improvement in symptom duration.[52][76]
- Bone marrow aspirate concentrate (BMAC): controls inflammation, reduces fibrosis, and recruits tenocytes and mesenchymal cells to damaged tissues. One study showed that 92% of patients with Achilles ruptures augmented with BMAC returned to sports in about 6 months with no reruptures noted.[52]
- Peripheral blood mononuclear cells (PBMNCs) comprise monocytes, macrophages, and lymphocytes. They are considered the new generation of regenerative autologous cell concentrates, but studies are lacking in the literature.[52]
- Scaffolds: composed of a combination of natural and synthetic materials. Among these options, an acellular graft comprising human dermal allograft showed the most promising outcomes in studies. These studies reported an increase in return to activity without any associated complications.[52]
(A1)
Surgical therapy is optional for 10 to 30% of patients who fail conservative therapy after 6 months.[77][78] Surgical procedures and approaches can vary and are described below. (B2)
- Open Debridement[79]
- Endoscopic or Minimally Invasive Procedures: comparable results to open procedures, but limited evidence shows fewer postoperative complications[80]
- Topaz or Tenax: no additional benefit compared to open debridement surgery[81]
- Resection of the superior calcaneus (Haglund deformity) and bursa: the calcaneal prominence theoretically compresses against the bursa, contributing to tendinopathy symptoms; however, recent literature has presented debates regarding the relationship between calcaneal shape and pain symptoms in this condition. Angles measured in Haglund deformities, such as Fowler-Philip and Bohler angles, are not associated with insertional Achilles tendinopathy.[2]
- Detachment and reattachment of the Achilles tendon
- Surgical approaches can involve central tendon splitting detachment, either through a medial or lateral approach. In 2021, a systematic review concluded that a lateral takedown approach resulted in a statistically significant lower rate of complications.[82]
- Tendon transfer
- Flexor hallucis longus (FHL) tendon transfer: considered the most reliable tendon to reconstruct or augment Achilles tendon insufficiency. It serves as an excellent option to restore plantarflexion force.[76]
- PeroneBrevisvis, flexor digitorum longus (FDL), and tibialis anterior tendon transfers have been reported when the FHL is unavailable.[76]
- Strayer gastrocnemius recession: significantly reduces pain but decreases plantarflexion power and endurance; therefore, it is not recommended for athletes.[2] (A1)
The evidence suggests that conservative treatments should be considered the first-line treatment for Achilles tendinopathy. However, despite a growing body of research in this field, there is still a lack of high-quality studies evaluating the effectiveness of these interventions.[83][84](A1)
- Inspection and clinical examination supplemented by ultrasound and MRI are essential to achieving the correct diagnosis. A high interrelation between hypervascularization and tendinopathy of the Achilles tendon was found using Doppler ultrasound, but these outcomes were not reproducible.[85]
- Evidence supports using eccentric exercises as an effective treatment for persistent Achilles tendinopathy, showing short-term benefits over the brace.[66]
- A combined treatment approach consisting of soft tissue treatment and eccentric exercise appears to be a beneficial treatment program clinicians should recommend to patients with insertional Achilles tendinopathy.[64]
- Surgery for insertional Achilles tendinopathy can lead to good functional outcomes and a satisfactory return to sports when the tailoring of surgical care matches the degree of tendon involvement.[78]
- Evidence suggests the effectiveness of traditional needle acupuncture may be beneficial for Achilles tendinopathy.[86]
- Studies comparing minimally invasive techniques to open procedures reported an average success rate of 83.6% and 78.9%, respectively (p = 0.987). The complication rate was 5.3% for minimally invasive techniques and 10.5% for open procedures.[87]
- Endoscopic and minimally invasive procedures may be the future surgical treatment of mid-Achilles tendinopathy.[88]
- According to available evidence, there is no consensus on using pharmacological treatments (comprising injection of a substance or local application) as the best nonoperative option for Achilles tendinopathy instead of the most commonly used eccentric loading rehabilitation program. However, combining different medications administered with physical therapy may prove beneficial. There is a need for more long-term investigations.[89]
- Local infiltrations of autologous plasma and the injection of platelet-rich plasma with eccentric training should be avoided, as there is no association between the therapeutic effects and the duration of symptoms in patients with chronic Achilles tendinopathy.[90][91] (A1)
In cases of insertional Achilles tendinopathy, a combination of surgical interventions, including debridement, resection of superior calcaneus and bursa, and reattachment of the Achilles tendon, have shown over 95% of success rate. On average, patients can return to activity within approximately 7 months following surgery.[79] While calcinosis may be present, it does not interfere with results. Furthermore, recurrent calcification is common but not associated with inferior surgical outcomes.[79][92]
In the case of non-insertional Achilles tendinopathy, satisfaction rates following surgery can range from 69% to 100%.[76] Complications are higher with non-insertional tendinopathy surgeries. In situations with a more than 50% tendon rupture, reattachment of the Achilles tendon should be considered.[76]
Differential Diagnosis
Posterior heel and ankle pain is a common complaint in primary care settings, and the risk of experiencing pain is elevated in individuals with higher body mass index and age. Further investigations become necessary when patients fail to show improvement with initial management approaches.[65] The most common musculoskeletal disorders of the soft tissues associated with posterior ankle pain are:
- Retrocalcaneal bursitis: easily identified on ultrasound or MRI.[43]
- Kager's fat pad inflammation: elicit pain with palpation on both sides of the ankle anterior to the Achilles.
- Achilles tendon rupture: positive Thompson test.[43]
- Achilles paratenonitis: ultrasound will show fluid and adhesions around the tendon.[43]
- Posterior impingement (Os Trigonum syndrome): posterior ankle pain with forced dorsiflexion. Plain radiographs will indicate the presence of Os Trigonum.
- Calcaneal stress fracture: positive squeeze test.[43]
- FHL tendinopathy: pain on the toe-off phase of gait. Increase fluid around FHL tendon on STIR MRI.[43]
- Plantar fasciitis: elicit pain with palpation of plantar medial calcaneal tubercle.[66][67]
- Nerve entrapment or neuroma: pain accompanied by burning, tingling, or numbness. Positive Tinel sign along the course of the sural nerve.[43]
- Heel pad syndrome: deep, bruise-like pain in the mid heel.[66][67]
- Haglund deformity: acute or chronic onset of pain in the posterolateral heel due to a prominence of the calcaneus; may lead to retrocalcaneal bursa inflammation and often requires surgical calcaneal resection.[93]
- Sever's disease: clinical diagnosis of calcaneal apophysitis in children and adolescents with immature growth plates.[66][67]
- Insertional calcific tendinosis: due to mucoid degeneration of the tendon, gradually worsening pain in middle-aged patients with high BMI often requires surgical detachment and reattachment of the tendon.[93]
- Lumbar (S1) radiculopathy: pain with decreased sensation over the posterior lateral ankle.[43]
Erdheim-Chester disease (ECD) is a rare histiocytosis of non-Langerhans cells reported in a 36-year-old man who presented with bilateral xanthogranulomas of the Achilles tendon. Although rare, ECD should be considered in the differential diagnosis of intratendinous masses.[68] As with all clinical presentations, the potential for non-musculoskeletal, more sinister causes of pain and systemic disease deserves scrutiny.[69]
Prognosis
Achilles tendinopathy has a better prognosis with early and adequate initial management. Surgical intervention for Achilles tendinosis of insertion (TAI) has a success rate exceeding 80% in most cases. According to a study by Stenson et al, the likelihood of failure in nonoperative treatment increases with the number of risk factors present.[94] Factors such as higher scores on the visual analog scale, limited ankle range of motion, previous corticosteroid injections, and the presence of Achilles tendon enthesophytes were associated with a 55% probability of failure with conservative treatment. Therefore, these risk factors can assist surgeons in deciding when surgical intervention is warranted in the appropriate clinical setting.
In a retrospective study conducted by Sanalla and colleagues, strengthening the Achilles tendon with a bone-tendon autograft was an effective procedure with a low risk of complications and reliable outcomes.[95]
Complications
When considering major and minor complications, the incidence ranges from 3% to 41% in surgical treatments for Achilles tendinopathy.[76] In addition, a study by Lohrer et al. concluded that the success rates of open and minimally invasive surgical treatment did not differ (83.4%), and patient satisfaction rates were comparable.[87] However, the complication rates were lower for the minimally invasive procedures. Baltes and his colleagues classified complications associated with surgical treatment as follows:[76][88]
- Major complications: tendon avulsion or rupture, any reoperation, deep vein thrombosis (DVT), reflex dystrophy, persistent neuralgia, deep infections, deep suture reactions, and major wound problems[76][79]
- Minor complications: discomfort, superficial infections, minor wound problems, scar sensitivity, hypertrophy, mild paraesthesia, prolonged hospitalization.
Complication rates also vary depending on whether the surgery is performed for insertional or non-insertional Achilles tendinopathy. While following insertional Achilles tendinopathy surgeries, the complication rate can reach up to 41%; similar severity of complications reaches up to 85% after non-insertional Achilles tendinopathy procedures.[76]
Postoperative and Rehabilitation Care
Following surgery for Achilles tendinopathy, a period of immobilization is required, which can involve using a cast, walking boot, or posterior splint. The duration of immobilization ranges from 3 to 8 weeks. However, there has been a recent increase in articles advocating for accelerated weight-bearing postoperative rehabilitation protocols.
In 2021, a study conducted by Arunakul and colleagues prospectively analyzed groups in both conventional and accelerated protocols following insertional Achilles tendinopathy surgery. The study found that an accelerated protocol improves short-term functional outcome scores. A template of both protocols is described below.[96]
- Conventional Postoperative Protocol
- Weeks 0-2: Non-weight bearing (NWB) with immobilization in a cast or splint in the equinus position
- Weeks 2-4: Transition into partial weight bearing (25%) with axillary crutches in the CAM boot with a 3-layer heel lift (2.4 cm)
- Weeks 4-6: Increase partial weight bearing to 50% with axillary crutches and a 1.6 cm heel lift.
- Weeks 6-8: Increase partial weight bearing to 75% with axillary crutches in the CAM boot with a 0.8 cm heel lift.
- Weeks 8-10: Full weight bearing with axillary crutches in the CAM boot without a heel lift.
- Week 10: Transition into regular shoes, as tolerated.[96]
- Accelerated Postoperative Weighbearing Protocol
- Weeks 0-2: NWB with immobilization in a cast or splint in equinus position
- Weeks 2-3: Transition to full weight bearing as tolerated in CAM boot with a 3-layer (2.4 cm) step heel lift
- Weeks 3-4: Same as above, but heel lift is decreased to 1.6 cm
- Weeks 4-5: Same as above, but heel lift is decreased to 0.8 cm
- Weeks 5-6: Full weight bearing in CAM boot without a heel lift
- Week 6: Transition into regular shoes, as tolerated[96]
Consultations
Collaborative care involving multiple specialty groups is necessary to treat Achilles tendinopathy comprehensively. The involvement of various healthcare professionals ensures a multidisciplinary approach, leading to more effective management and improved patient outcomes. The 3 specialty groups commonly involved in the treatment of Achilles tendinopathy are as follows:
-
Podiatry: Podiatrists are crucial in managing Achilles tendinopathy, providing expertise in foot biomechanics, gait analysis, and prescribing orthotics or custom footwear. Podiatrists may also perform corticosteroid injections or extracorporeal shockwave therapy to alleviate pain and promote healing.
-
Physical Therapy: Physical therapists are instrumental in the rehabilitation process for Achilles tendinopathy. They design individualized exercise programs focusing on strengthening the affected tendon, improving flexibility, and addressing any associated biomechanical issues. Physical therapists may utilize various modalities, such as therapeutic exercises, manual therapy, ultrasound, and electrical stimulation, to facilitate recovery and restore optimal function.
-
Orthopedic Surgeons: Orthopedic surgeons specialize in cases where conservative treatments fail to provide adequate relief or in situations involving severe tendon damage or rupture; orthopedic consultation may be necessary. Orthopedic surgeons can assess the need for surgical intervention, perform tendon repairs or reconstructions, and provide postoperative care to facilitate recovery.
Deterrence and Patient Education
Patient education and a more conservative approach can prevent chronic tendinopathy.[97][98][99][100] Some strategies that have been supported by scientific evidence include:
- Sport Modification: Switching to low-impact activities (swimming, weight training, rowing, cycling) allows the Achilles tendon time to rest.[100]
- Eccentric Exercise Therapy: Incorporating eccentric exercises, which involve controlled lengthening of the muscle-tendon unit, has decreased pain and prevented progression to chronic tendinopathy.[53][54][56]
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Scientific evidence supports many conservative treatments, such as NSAIDs (eg, ibuprofen, naproxen), to help reduce inflammation and manage pain.[50][51][76]
- Proper Footwear: Choosing running shoes that provide adequate cushioning and support for the heel strike can reduce stress on the Achilles tendon.[77]
- Warm-up and Stretching: Before engaging in sports or exercise, it is beneficial to stretch the calf muscles.[77]
- Gradual Progression: Gradually increase the distance and running speed by only 10% per week. Avoiding sudden increases in intensity, running on uneven slopes, and ensuring proper cool-down after exercise is important to prevent overloading of the Achilles tendon.[77][78]
- Extracorporeal Shock Wave Therapy (ESWT): ESWT is a non-invasive treatment that uses shock waves to stimulate healing in the Achilles tendon. It may be beneficial if other interventions have not provided satisfactory results.[59]
Surgical intervention is typically reserved as a last resort for cases where conservative treatments have failed to improve symptoms or if there is a significant tendon rupture.
Enhancing Healthcare Team Outcomes
Achilles tendinopathy is a complex condition that can significantly impact individuals, both athletes and nonathletes, by limiting their ability to engage in exercise and physical activities. The management of Achilles tendinopathy typically starts with conservative or physical therapies as the initial approach. An interprofessional healthcare team may be necessary when managing cases of Achilles tendinopathy to improve patient outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
O'Brien M. The anatomy of the Achilles tendon. Foot and ankle clinics. 2005 Jun:10(2):225-38 [PubMed PMID: 15922915]
Chimenti RL, Cychosz CC, Hall MM, Phisitkul P. Current Concepts Review Update: Insertional Achilles Tendinopathy. Foot & ankle international. 2017 Oct:38(10):1160-1169. doi: 10.1177/1071100717723127. Epub 2017 Aug 8 [PubMed PMID: 28789557]
Weinfeld SB. Achilles tendon disorders. The Medical clinics of North America. 2014 Mar:98(2):331-8. doi: 10.1016/j.mcna.2013.11.005. Epub [PubMed PMID: 24559878]
Ahmed IM, Lagopoulos M, McConnell P, Soames RW, Sefton GK. Blood supply of the Achilles tendon. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 1998 Sep:16(5):591-6 [PubMed PMID: 9820283]
Mahan J, Damodar D, Trapana E, Barnhill S, Nuno AU, Smyth NA, Aiyer A, Jose J. Achilles tendon complex: The anatomy of its insertional footprint on the calcaneus and clinical implications. Journal of orthopaedics. 2020 Jan-Feb:17():221-227. doi: 10.1016/j.jor.2019.06.008. Epub 2019 Jun 10 [PubMed PMID: 31889745]
Rabusin CL, Menz HB, McClelland JA, Evans AM, Malliaras P, Docking SI, Landorf KB, Gerrard JM, Munteanu SE. Efficacy of heel lifts versus calf muscle eccentric exercise for mid-portion Achilles tendinopathy (HEALTHY): a randomised trial. British journal of sports medicine. 2021 May:55(9):486-492. doi: 10.1136/bjsports-2019-101776. Epub 2020 Sep 28 [PubMed PMID: 32988930]
Level 1 (high-level) evidenceAbate M, Salini V. Mid-portion Achilles tendinopathy in runners with metabolic disorders. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2019 Apr:29(3):697-703. doi: 10.1007/s00590-018-2336-2. Epub 2018 Oct 26 [PubMed PMID: 30367279]
Zhao H, Ren Y, Roth EJ, Harvey RL, Zhang LQ. Concurrent deficits of soleus and gastrocnemius muscle fascicles and Achilles tendon post stroke. Journal of applied physiology (Bethesda, Md. : 1985). 2015 Apr 1:118(7):863-71. doi: 10.1152/japplphysiol.00226.2014. Epub 2015 Feb 5 [PubMed PMID: 25663670]
Olewnik Ł, Wysiadecki G, Podgórski M, Polguj M, Topol M. The Plantaris Muscle Tendon and Its Relationship with the Achilles Tendinopathy. BioMed research international. 2018:2018():9623579. doi: 10.1155/2018/9623579. Epub 2018 May 31 [PubMed PMID: 29955614]
Yang X, Coleman DP, Pugh ND, Nokes LD. The volume of the neovascularity and its clinical implications in achilles tendinopathy. Ultrasound in medicine & biology. 2012 Nov:38(11):1887-95. doi: 10.1016/j.ultrasmedbio.2012.07.002. Epub 2012 Sep 10 [PubMed PMID: 22975033]
Slane LC, Dandois F, Bogaerts S, Vandenneucker H, Scheys L. Non-uniformity in the healthy patellar tendon is greater in males and similar in different age groups. Journal of biomechanics. 2018 Oct 26:80():16-22. doi: 10.1016/j.jbiomech.2018.08.021. Epub 2018 Aug 23 [PubMed PMID: 30224164]
Pękala PA, Henry BM, Ochała A, Kopacz P, Tatoń G, Młyniec A, Walocha JA, Tomaszewski KA. The twisted structure of the Achilles tendon unraveled: A detailed quantitative and qualitative anatomical investigation. Scandinavian journal of medicine & science in sports. 2017 Dec:27(12):1705-1715. doi: 10.1111/sms.12835. Epub 2017 Jan 30 [PubMed PMID: 28139009]
Level 2 (mid-level) evidenceFederer AE, Steele JR, Dekker TJ, Liles JL, Adams SB. Tendonitis and Tendinopathy: What Are They and How Do They Evolve? Foot and ankle clinics. 2017 Dec:22(4):665-676. doi: 10.1016/j.fcl.2017.07.002. Epub 2017 Sep 27 [PubMed PMID: 29078821]
Moon JL, Moon KM, Carlisle DM. Obesity-Related Foot Pain: Diagnosis and Surgical Planning. Clinics in podiatric medicine and surgery. 2019 Jan:36(1):141-151. doi: 10.1016/j.cpm.2018.08.008. Epub 2018 Oct 25 [PubMed PMID: 30446041]
Bolon B. Mini-Review: Toxic Tendinopathy. Toxicologic pathology. 2017 Oct:45(7):834-837. doi: 10.1177/0192623317711614. Epub 2017 May 28 [PubMed PMID: 28553748]
Alušík Š, Paluch Z. [Drug induced tendon injury]. Vnitrni lekarstvi. 2018 Winter:63(12):967-971 [PubMed PMID: 29334747]
Camargo PR, Alburquerque-Sendín F, Salvini TF. Eccentric training as a new approach for rotator cuff tendinopathy: Review and perspectives. World journal of orthopedics. 2014 Nov 18:5(5):634-44. doi: 10.5312/wjo.v5.i5.634. Epub 2014 Nov 18 [PubMed PMID: 25405092]
Level 3 (low-level) evidenceGodoy-Santos AL, Bruschini H, Cury J, Srougi M, de Cesar-Netto C, Fonseca LF, Maffulli N. Fluoroquinolones and the Risk of Achilles Tendon Disorders: Update on a Neglected Complication. Urology. 2018 Mar:113():20-25. doi: 10.1016/j.urology.2017.10.017. Epub 2017 Oct 23 [PubMed PMID: 29074337]
Almekinders LC, Engle CR. Common and Uncommon Injuries in Ultra-endurance Sports. Sports medicine and arthroscopy review. 2019 Mar:27(1):25-30. doi: 10.1097/JSA.0000000000000217. Epub [PubMed PMID: 30601398]
Brund RBK, Rasmussen S, Kersting UG, Arendt-Nielsen L, Palsson TS. Prediction of running-induced Achilles tendinopathy with pain sensitivity - a 1-year prospective study. Scandinavian journal of pain. 2019 Jan 28:19(1):139-146. doi: 10.1515/sjpain-2018-0084. Epub [PubMed PMID: 30407913]
Colbert LH, Hootman JM, Macera CA. Physical activity-related injuries in walkers and runners in the aerobics center longitudinal study. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2000 Oct:10(4):259-63 [PubMed PMID: 11086751]
Level 2 (mid-level) evidenceCassel M, Risch L, Intziegianni K, Mueller J, Stoll J, Brecht P, Mayer F. Incidence of Achilles and Patellar Tendinopathy in Adolescent Elite Athletes. International journal of sports medicine. 2018 Sep:39(9):726-732. doi: 10.1055/a-0633-9098. Epub 2018 Jun 25 [PubMed PMID: 29940667]
Mulvad B, Nielsen RO, Lind M, Ramskov D. Diagnoses and time to recovery among injured recreational runners in the RUN CLEVER trial. PloS one. 2018:13(10):e0204742. doi: 10.1371/journal.pone.0204742. Epub 2018 Oct 12 [PubMed PMID: 30312310]
Molyneux P, Carroll M, Stewart S, Brenton-Rule A, Rome K. Ultrasound characteristics of the mid-portion of the Achilles tendon in runners: a systematic review protocol. Systematic reviews. 2017 May 30:6(1):108. doi: 10.1186/s13643-017-0501-z. Epub 2017 May 30 [PubMed PMID: 28558847]
Level 1 (high-level) evidencede Jonge S, van den Berg C, de Vos RJ, van der Heide HJ, Weir A, Verhaar JA, Bierma-Zeinstra SM, Tol JL. Incidence of midportion Achilles tendinopathy in the general population. British journal of sports medicine. 2011 Oct:45(13):1026-8. doi: 10.1136/bjsports-2011-090342. Epub [PubMed PMID: 21926076]
Level 2 (mid-level) evidenceWeber J, Buchhorn T. [Midportion Achilles tendinopathy]. Der Unfallchirurg. 2017 Dec:120(12):1038-1043. doi: 10.1007/s00113-017-0411-5. Epub [PubMed PMID: 28921035]
Wezenbeek E, De Clercq D, Mahieu N, Willems T, Witvrouw E. Activity-Induced Increase in Achilles Tendon Blood Flow Is Age and Sex Dependent. The American journal of sports medicine. 2018 Sep:46(11):2678-2686. doi: 10.1177/0363546518786259. Epub 2018 Aug 1 [PubMed PMID: 30067065]
Lemme NJ, Li NY, DeFroda SF, Kleiner J, Owens BD. Epidemiology of Achilles Tendon Ruptures in the United States: Athletic and Nonathletic Injuries From 2012 to 2016. Orthopaedic journal of sports medicine. 2018 Nov:6(11):2325967118808238. doi: 10.1177/2325967118808238. Epub 2018 Nov 26 [PubMed PMID: 30505872]
Li HY, Hua YH. Achilles Tendinopathy: Current Concepts about the Basic Science and Clinical Treatments. BioMed research international. 2016:2016():6492597 [PubMed PMID: 27885357]
Edama M, Takabayashi T, Yokota H, Hirabayashi R, Sekine C, Maruyama S, Otani H. Classification by degree of twisted structure of the fetal Achilles tendon. Surgical and radiologic anatomy : SRA. 2021 Oct:43(10):1691-1695. doi: 10.1007/s00276-021-02803-9. Epub 2021 Jul 14 [PubMed PMID: 34263342]
Pirozzi KM. Histophysiology of Fibrocartilage. Clinics in podiatric medicine and surgery. 2022 Jul:39(3):363-370. doi: 10.1016/j.cpm.2022.02.002. Epub 2022 May 21 [PubMed PMID: 35717055]
Kvist M, Józsa L, Järvinen MJ, Kvist H. Chronic Achilles paratenonitis in athletes: a histological and histochemical study. Pathology. 1987 Jan:19(1):1-11 [PubMed PMID: 3588019]
Klatte-Schulz F, Minkwitz S, Schmock A, Bormann N, Kurtoglu A, Tsitsilonis S, Manegold S, Wildemann B. Different Achilles Tendon Pathologies Show Distinct Histological and Molecular Characteristics. International journal of molecular sciences. 2018 Jan 30:19(2):. doi: 10.3390/ijms19020404. Epub 2018 Jan 30 [PubMed PMID: 29385715]
Feilmeier M. Noninsertional Achilles Tendinopathy Pathologic Background and Clinical Examination. Clinics in podiatric medicine and surgery. 2017 Apr:34(2):129-136. doi: 10.1016/j.cpm.2016.10.003. Epub 2016 Dec 24 [PubMed PMID: 28257670]
DeCarbo WT, Bullock MJ. Midsubstance Tendinopathy, Surgical Management. Clinics in podiatric medicine and surgery. 2017 Apr:34(2):175-193. doi: 10.1016/j.cpm.2016.10.006. Epub 2016 Dec 23 [PubMed PMID: 28257673]
Jeong C, Kim SE, Shim KS, Kim HJ, Song MH, Park K, Song HR. Exploring the In Vivo Anti-Inflammatory Actions of Simvastatin-Loaded Porous Microspheres on Inflamed Tenocytes in a Collagenase-Induced Animal Model of Achilles Tendinitis. International journal of molecular sciences. 2018 Mar 12:19(3):. doi: 10.3390/ijms19030820. Epub 2018 Mar 12 [PubMed PMID: 29534523]
Level 3 (low-level) evidenceDakin SG, Newton J, Martinez FO, Hedley R, Gwilym S, Jones N, Reid HAB, Wood S, Wells G, Appleton L, Wheway K, Watkins B, Carr AJ. Chronic inflammation is a feature of Achilles tendinopathy and rupture. British journal of sports medicine. 2018 Mar:52(6):359-367. doi: 10.1136/bjsports-2017-098161. Epub 2017 Nov 8 [PubMed PMID: 29118051]
El-Habta R, Chen J, Pingel J, Backman LJ. Tendinosis-like changes in denervated rat Achilles tendon. BMC musculoskeletal disorders. 2018 Nov 30:19(1):426. doi: 10.1186/s12891-018-2353-7. Epub 2018 Nov 30 [PubMed PMID: 30497469]
Obst SJ, Heales LJ, Schrader BL, Davis SA, Dodd KA, Holzberger CJ, Beavis LB, Barrett RS. Are the Mechanical or Material Properties of the Achilles and Patellar Tendons Altered in Tendinopathy? A Systematic Review with Meta-analysis. Sports medicine (Auckland, N.Z.). 2018 Sep:48(9):2179-2198. doi: 10.1007/s40279-018-0956-7. Epub [PubMed PMID: 29961208]
Level 1 (high-level) evidenceTu P. Heel Pain: Diagnosis and Management. American family physician. 2018 Jan 15:97(2):86-93 [PubMed PMID: 29365222]
Martin RL, Chimenti R, Cuddeford T, Houck J, Matheson JW, McDonough CM, Paulseth S, Wukich DK, Carcia CR. Achilles Pain, Stiffness, and Muscle Power Deficits: Midportion Achilles Tendinopathy Revision 2018. The Journal of orthopaedic and sports physical therapy. 2018 May:48(5):A1-A38. doi: 10.2519/jospt.2018.0302. Epub [PubMed PMID: 29712543]
Maffulli N, Kenward MG, Testa V, Capasso G, Regine R, King JB. Clinical diagnosis of Achilles tendinopathy with tendinosis. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2003 Jan:13(1):11-5 [PubMed PMID: 12544158]
Vo TP, Ho GWK, Andrea J. Achilles Tendinopathy, A Brief Review and Update of Current Literature. Current sports medicine reports. 2021 Sep 1:20(9):453-461. doi: 10.1249/JSR.0000000000000884. Epub [PubMed PMID: 34524189]
Longo UG, Ronga M, Maffulli N. Achilles Tendinopathy. Sports medicine and arthroscopy review. 2018 Mar:26(1):16-30. doi: 10.1097/JSA.0000000000000185. Epub [PubMed PMID: 29300224]
Matthews W, Ellis R, Furness J, Hing WA. The clinical diagnosis of Achilles tendinopathy: a scoping review. PeerJ. 2021:9():e12166. doi: 10.7717/peerj.12166. Epub 2021 Sep 28 [PubMed PMID: 34692248]
Level 2 (mid-level) evidenceBulstra GH, van Rheenen TA, Scholtes VA. Can We Measure the Heel Bump? Radiographic Evaluation of Haglund's Deformity. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2015 May-Jun:54(3):338-40. doi: 10.1053/j.jfas.2014.07.006. Epub 2014 Aug 30 [PubMed PMID: 25179453]
Gladman DD, Abufayyah M, Salonen D, Thavaneswaran A, Chandran V. Radiological characteristics of the calcaneal spurs in psoriatic arthritis. Clinical and experimental rheumatology. 2014 May-Jun:32(3):401-3 [PubMed PMID: 24850064]
Level 1 (high-level) evidenceRachel JN, Williams JB, Sawyer JR, Warner WC, Kelly DM. Is radiographic evaluation necessary in children with a clinical diagnosis of calcaneal apophysitis (sever disease)? Journal of pediatric orthopedics. 2011 Jul-Aug:31(5):548-50. doi: 10.1097/BPO.0b013e318219905c. Epub [PubMed PMID: 21654464]
Mahoney JM. Imaging Techniques and Indications. Clinics in podiatric medicine and surgery. 2017 Apr:34(2):115-128. doi: 10.1016/j.cpm.2016.10.014. Epub 2017 Jan 19 [PubMed PMID: 28257669]
Matthews W, Ellis R, Furness J, Hing W. Classification of Tendon Matrix Change Using Ultrasound Imaging: A Systematic Review and Meta-analysis. Ultrasound in medicine & biology. 2018 Oct:44(10):2059-2080. doi: 10.1016/j.ultrasmedbio.2018.05.022. Epub 2018 Jul 12 [PubMed PMID: 30007477]
Level 1 (high-level) evidenceRomero-Morales C, Martín-Llantino PJ, Calvo-Lobo C, Palomo-López P, López-López D, Pareja-Galeano H, Rodríguez-Sanz D. Comparison of the sonographic features of the Achilles Tendon complex in patients with and without achilles tendinopathy: A case-control study. Physical therapy in sport : official journal of the Association of Chartered Physiotherapists in Sports Medicine. 2019 Jan:35():122-126. doi: 10.1016/j.ptsp.2018.12.003. Epub 2018 Dec 5 [PubMed PMID: 30543997]
Level 2 (mid-level) evidenceIndino C, D'Ambrosi R, Usuelli FG. Biologics in the Treatment of Achilles Tendon Pathologies. Foot and ankle clinics. 2019 Sep:24(3):471-493. doi: 10.1016/j.fcl.2019.04.009. Epub 2019 May 21 [PubMed PMID: 31370998]
Bullock MJ, Mourelatos J, Mar A. Achilles Impingement Tendinopathy on Magnetic Resonance Imaging. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2017 May-Jun:56(3):555-563. doi: 10.1053/j.jfas.2017.01.024. Epub 2017 Feb 28 [PubMed PMID: 28258946]
Tuite MJ. MR imaging of the tendons of the foot and ankle. Seminars in musculoskeletal radiology. 2002 Jun:6(2):119-31 [PubMed PMID: 12077701]
Leslie HD, Edwards WH. Neglected ruptures of the Achilles tendon. Foot and ankle clinics. 2005 Jun:10(2):357-70 [PubMed PMID: 15922924]
Kamel M, Eid H, Mansour R. Ultrasound detection of heel enthesitis: a comparison with magnetic resonance imaging. The Journal of rheumatology. 2003 Apr:30(4):774-8 [PubMed PMID: 12672198]
Albano D, Messina C, Usuelli FG, De Girolamo L, Grassi M, Maccario C, Bignotti B, Tagliafico A, Sconfienza LM. Magnetic resonance and ultrasound in achilles tendinopathy: Predictive role and response assessment to platelet-rich plasma and adipose-derived stromal vascular fraction injection. European journal of radiology. 2017 Oct:95():130-135. doi: 10.1016/j.ejrad.2017.08.006. Epub 2017 Aug 9 [PubMed PMID: 28987658]
Ficek K, Filipek J, Ficek J, Muzalewska M, Humpa F. Calcaneal CT is a useful tool for identifying Achilles tendon disorders: a pilot study. Journal of orthopaedic surgery and research. 2017 Sep 25:12(1):139. doi: 10.1186/s13018-017-0638-4. Epub 2017 Sep 25 [PubMed PMID: 28946912]
Level 3 (low-level) evidenceHuang YB, Zhao YX, Xiao JJ, Li MW, Zhang R, Li SL. [Comparative analysis of the ankle joints in juvenile male soccer players with imaging]. Zhonghua yi xue za zhi. 2016 Jul 5:96(25):1971-5. doi: 10.3760/cma.j.issn.0376-2491.2016.25.003. Epub [PubMed PMID: 27470952]
Level 2 (mid-level) evidenceLang TR, Cook J, Rio E, Gaida JE. What tendon pathology is seen on imaging in people who have taken fluoroquinolones? A systematic review. Fundamental & clinical pharmacology. 2017 Feb:31(1):4-16. doi: 10.1111/fcp.12228. Epub 2016 Oct 5 [PubMed PMID: 27477928]
Level 1 (high-level) evidenceMurphy M, Rio E, Debenham J, Docking S, Travers M, Gibson W. EVALUATING THE PROGRESS OF MID-PORTION ACHILLES TENDINOPATHY DURING REHABILITATION: A REVIEW OF OUTCOME MEASURES FOR SELF- REPORTED PAIN AND FUNCTION. International journal of sports physical therapy. 2018 Apr:13(2):283-292 [PubMed PMID: 30090686]
Palazón-Bru A, Tomás-Rodríguez MI, Mares-García E, Gil-Guillén VF. A Reliability Generalization Meta-Analysis of the Victorian Institute of Sport Assessment Scale for Achilles Tendinopathy (VISA-A). Foot & ankle international. 2019 Apr:40(4):430-438. doi: 10.1177/1071100718816953. Epub 2018 Dec 20 [PubMed PMID: 30569746]
Level 1 (high-level) evidenceVerrall GM, Dolman BK, Best TM. Applying physical science principles to mid-substance Achilles tendinopathy and the relationship to eccentric lengthening exercises. Scandinavian journal of medicine & science in sports. 2018 Mar:28(3):1159-1165. doi: 10.1111/sms.12978. Epub 2017 Oct 4 [PubMed PMID: 28948634]
McCormack JR, Underwood FB, Slaven EJ, Cappaert TA. Eccentric Exercise Versus Eccentric Exercise and Soft Tissue Treatment (Astym) in the Management of Insertional Achilles Tendinopathy. Sports health. 2016 May/Jun:8(3):230-237. doi: 10.1177/1941738116631498. Epub [PubMed PMID: 26893309]
Wilson F, Walshe M, O'Dwyer T, Bennett K, Mockler D, Bleakley C. Exercise, orthoses and splinting for treating Achilles tendinopathy: a systematic review with meta-analysis. British journal of sports medicine. 2018 Dec:52(24):1564-1574. doi: 10.1136/bjsports-2017-098913. Epub 2018 Aug 31 [PubMed PMID: 30170996]
Level 1 (high-level) evidenceWoitzik E, Jacobs C, Wong JJ, Côté P, Shearer HM, Randhawa K, Sutton D, Southerst D, Varatharajan S, Brison RJ, Yu H, van der Velde G, Stern PJ, Taylor-Vaisey A, Stupar M, Mior S, Carroll LJ. The effectiveness of exercise on recovery and clinical outcomes of soft tissue injuries of the leg, ankle, and foot: A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Manual therapy. 2015 Oct:20(5):633-45. doi: 10.1016/j.math.2015.03.012. Epub 2015 Mar 28 [PubMed PMID: 25892707]
Level 2 (mid-level) evidenceRabello LM, van den Akker-Scheek I, Brink MS, Maas M, Diercks RL, Zwerver J. Association Between Clinical and Imaging Outcomes After Therapeutic Loading Exercise in Patients Diagnosed With Achilles or Patellar Tendinopathy at Short- and Long-Term Follow-up: A Systematic Review. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2020 Jul:30(4):390-403. doi: 10.1097/JSM.0000000000000624. Epub [PubMed PMID: 29952842]
Level 1 (high-level) evidenceMurphy M, Travers M, Gibson W, Chivers P, Debenham J, Docking S, Rio E. Rate of Improvement of Pain and Function in Mid-Portion Achilles Tendinopathy with Loading Protocols: A Systematic Review and Longitudinal Meta-Analysis. Sports medicine (Auckland, N.Z.). 2018 Aug:48(8):1875-1891. doi: 10.1007/s40279-018-0932-2. Epub [PubMed PMID: 29766442]
Level 1 (high-level) evidenceDedes V, Stergioulas A, Kipreos G, Dede AM, Mitseas A, Panoutsopoulos GI. Effectiveness and Safety of Shockwave Therapy in Tendinopathies. Materia socio-medica. 2018 Jun:30(2):131-146. doi: 10.5455/msm.2018.30.141-146. Epub [PubMed PMID: 30061805]
Le ADK, Enweze L, DeBaun MR, Dragoo JL. Current Clinical Recommendations for Use of Platelet-Rich Plasma. Current reviews in musculoskeletal medicine. 2018 Dec:11(4):624-634. doi: 10.1007/s12178-018-9527-7. Epub [PubMed PMID: 30353479]
McClinton S, Luedke L, Clewley D. Nonsurgical Management of Midsubstance Achilles Tendinopathy. Clinics in podiatric medicine and surgery. 2017 Apr:34(2):137-160. doi: 10.1016/j.cpm.2016.10.004. Epub 2016 Dec 1 [PubMed PMID: 28257671]
Bussin ER, Cairns B, Bovard J, Scott A. Randomised controlled trial evaluating the short-term analgesic effect of topical diclofenac on chronic Achilles tendon pain: a pilot study. BMJ open. 2017 May 4:7(4):e015126. doi: 10.1136/bmjopen-2016-015126. Epub 2017 May 4 [PubMed PMID: 28473518]
Level 3 (low-level) evidenceHeinemeier KM, Øhlenschlæger TF, Mikkelsen UR, Sønder F, Schjerling P, Svensson RB, Kjaer M. Effects of anti-inflammatory (NSAID) treatment on human tendinopathic tissue. Journal of applied physiology (Bethesda, Md. : 1985). 2017 Nov 1:123(5):1397-1405. doi: 10.1152/japplphysiol.00281.2017. Epub 2017 Aug 31 [PubMed PMID: 28860166]
Jayaseelan DJ, Kecman M, Alcorn D, Sault JD. Manual therapy and eccentric exercise in the management of Achilles tendinopathy. The Journal of manual & manipulative therapy. 2017 May:25(2):106-114. doi: 10.1080/10669817.2016.1183289. Epub 2016 May 30 [PubMed PMID: 28559670]
Silbernagel KG, Hanlon S, Sprague A. Current Clinical Concepts: Conservative Management of Achilles Tendinopathy. Journal of athletic training. 2020 May:55(5):438-447. doi: 10.4085/1062-6050-356-19. Epub 2020 Apr 8 [PubMed PMID: 32267723]
Phisitkul P, Mansur NSB, Netto CC. Failed Surgery for Achilles Tendinopathy. Foot and ankle clinics. 2022 Jun:27(2):431-455. doi: 10.1016/j.fcl.2021.11.027. Epub 2022 May 5 [PubMed PMID: 35680298]
Alfredson H, Masci L, Spang C. Surgical plantaris tendon removal for patients with plantaris tendon-related pain only and a normal Achilles tendon: a case series. BMJ open sport & exercise medicine. 2018:4(1):e000462. doi: 10.1136/bmjsem-2018-000462. Epub 2018 Dec 5 [PubMed PMID: 30588327]
Level 2 (mid-level) evidenceHardy A, Rousseau R, Issa SP, Gerometta A, Pascal-Moussellard H, Granger B, Khiami F. Functional outcomes and return to sports after surgical treatment of insertional Achilles tendinopathy: Surgical approach tailored to the degree of tendon involvement. Orthopaedics & traumatology, surgery & research : OTSR. 2018 Sep:104(5):719-723. doi: 10.1016/j.otsr.2018.05.003. Epub 2018 May 28 [PubMed PMID: 29852319]
Saxena A, Maffulli N, Jin A, Isa E, Arthur WP, Wahl A. Insertional Achilles Tendinopathy: Analysis of 166 Procedures and Return to Activity. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2021 Nov-Dec:60(6):1117-1123. doi: 10.1053/j.jfas.2021.01.011. Epub 2021 Apr 20 [PubMed PMID: 34024676]
Akoh CC, Phisitkul P. Minimally Invasive and Endoscopic Approach for the Treatment of Noninsertional Achilles Tendinopathy. Foot and ankle clinics. 2019 Sep:24(3):495-504. doi: 10.1016/j.fcl.2019.04.007. Epub 2019 May 21 [PubMed PMID: 31370999]
Morrison RJM, Brock TM, Reed MR, Muller SD. Radiofrequency Microdebridement Versus Surgical Decompression for Achilles Tendinosis: A Randomized Controlled Trial. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2017 Jul-Aug:56(4):708-712. doi: 10.1053/j.jfas.2017.01.049. Epub 2017 May 9 [PubMed PMID: 28495412]
Level 1 (high-level) evidenceThompson JM, Nguyen K, Ahluwalia J, Casciato D, Tewilliager T, So E, Prissel M. Surgical Takedown Approaches to Insertional Achilles Tendinopathy: A Systematic Review. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2021 Nov-Dec:60(6):1217-1221. doi: 10.1053/j.jfas.2021.04.015. Epub 2021 Apr 30 [PubMed PMID: 34108118]
Level 1 (high-level) evidenceSussmilch-Leitch SP, Collins NJ, Bialocerkowski AE, Warden SJ, Crossley KM. Physical therapies for Achilles tendinopathy: systematic review and meta-analysis. Journal of foot and ankle research. 2012 Jul 2:5(1):15. doi: 10.1186/1757-1146-5-15. Epub 2012 Jul 2 [PubMed PMID: 22747701]
Level 1 (high-level) evidenceYu H, Randhawa K, Côté P, Optima Collaboration. The Effectiveness of Physical Agents for Lower-Limb Soft Tissue Injuries: A Systematic Review. The Journal of orthopaedic and sports physical therapy. 2016 Jul:46(7):523-54. doi: 10.2519/jospt.2016.6521. Epub 2016 Jun 6 [PubMed PMID: 27266884]
Level 1 (high-level) evidenceGaulke R, Krettek C. [Tendinopathies of the foot and ankle : Evidence for the origin, diagnostics and therapy]. Der Unfallchirurg. 2017 Mar:120(3):205-213. doi: 10.1007/s00113-016-0301-2. Epub [PubMed PMID: 28120032]
Cox J, Varatharajan S, Côté P, Optima Collaboration. Effectiveness of Acupuncture Therapies to Manage Musculoskeletal Disorders of the Extremities: A Systematic Review. The Journal of orthopaedic and sports physical therapy. 2016 Jun:46(6):409-29. doi: 10.2519/jospt.2016.6270. Epub 2016 Apr 26 [PubMed PMID: 27117725]
Level 1 (high-level) evidenceLohrer H, David S, Nauck T. Surgical treatment for achilles tendinopathy - a systematic review. BMC musculoskeletal disorders. 2016 May 10:17():207. doi: 10.1186/s12891-016-1061-4. Epub 2016 May 10 [PubMed PMID: 27165287]
Level 1 (high-level) evidenceBaltes TPA, Zwiers R, Wiegerinck JI, van Dijk CN. Surgical treatment for midportion Achilles tendinopathy: a systematic review. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2017 Jun:25(6):1817-1838. doi: 10.1007/s00167-016-4062-9. Epub 2016 Mar 12 [PubMed PMID: 26971111]
Level 1 (high-level) evidenceMaffulli N, Papalia R, D'Adamio S, Diaz Balzani L, Denaro V. Pharmacological interventions for the treatment of Achilles tendinopathy: a systematic review of randomized controlled trials. British medical bulletin. 2015 Mar:113(1):101-15. doi: 10.1093/bmb/ldu040. Epub 2015 Jan 12 [PubMed PMID: 25583629]
Level 1 (high-level) evidenceLin MT, Chiang CF, Wu CH, Hsu HH, Tu YK. Meta-analysis Comparing Autologous Blood-Derived Products (Including Platelet-Rich Plasma) Injection Versus Placebo in Patients With Achilles Tendinopathy. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2018 Jun:34(6):1966-1975.e5. doi: 10.1016/j.arthro.2018.01.030. Epub [PubMed PMID: 29685839]
Level 1 (high-level) evidenceZhang YJ, Xu SZ, Gu PC, Du JY, Cai YZ, Zhang C, Lin XJ. Is Platelet-rich Plasma Injection Effective for Chronic Achilles Tendinopathy? A Meta-analysis. Clinical orthopaedics and related research. 2018 Aug:476(8):1633-1641. doi: 10.1007/s11999.0000000000000258. Epub [PubMed PMID: 29601383]
Level 1 (high-level) evidenceGreiner F, Trnka HJ, Chraim M, Neunteufel E, Bock P. Clinical and Radiological Outcomes of Operative Therapy in Insertional Achilles Tendinopathy With Debridement and Double-Row Refixation. Foot & ankle international. 2021 Sep:42(9):1115-1120. doi: 10.1177/10711007211002814. Epub 2021 Apr 10 [PubMed PMID: 33843294]
Grambart ST, Lechner J, Wentz J. Differentiating Achilles Insertional Calcific Tendinosis and Haglund's Deformity. Clinics in podiatric medicine and surgery. 2021 Apr:38(2):165-181. doi: 10.1016/j.cpm.2020.12.003. Epub 2021 Feb 13 [PubMed PMID: 33745649]
Stenson JF, Reb CW, Daniel JN, Saini SS, Albana MF. Predicting Failure of Nonoperative Treatment for Insertional Achilles Tendinosis. Foot & ankle specialist. 2018 Jun:11(3):252-255. doi: 10.1177/1938640017729497. Epub 2017 Sep 8 [PubMed PMID: 28884594]
Sanalla H, Hart R, Komzák M, Paša L. [Surgical Treatment of the Achilles Insertional Tendinopathy Using the Augmentation with the BT Graft from M. Quadriceps Femoris]. Acta chirurgiae orthopaedicae et traumatologiae Cechoslovaca. 2018:85(4):266-270 [PubMed PMID: 30257757]
Arunakul M, Pholsawatchai W, Arunakul P, Pitakveerakul A. Conventional vs Accelerated Rehabilitation Protocol Following Reattachment of Achilles Tendon for Insertional Achilles Tendinopathy. Foot & ankle international. 2021 Sep:42(9):1121-1129. doi: 10.1177/10711007211003871. Epub 2021 May 24 [PubMed PMID: 34024153]
Barry ME. Patient-education guide. Heel pain. Nursing. 2004 Feb:34(2):43 [PubMed PMID: 14758327]
Chang HJ, Burke AE, Glass RM. JAMA patient page. Achilles tendinopathy. JAMA. 2010 Jan 13:303(2):188. doi: 10.1001/jama.303.2.188. Epub [PubMed PMID: 20068216]
Chinn L, Hertel J. Rehabilitation of ankle and foot injuries in athletes. Clinics in sports medicine. 2010 Jan:29(1):157-67, table of contents. doi: 10.1016/j.csm.2009.09.006. Epub [PubMed PMID: 19945591]
Sartorio F, Zanetta A, Ferriero G, Bravini E, Vercelli S. The EdUReP approach plus manual therapy for the management of insertional Achilles tendinopathy. The Journal of sports medicine and physical fitness. 2018 May:58(5):664-668. doi: 10.23736/S0022-4707.17.06952-3. Epub 2017 Feb 21 [PubMed PMID: 28222571]