Introduction
Subungual hematomas are injuries of the nail bed in which bleeding develops under the nail. Patients usually complain of pain and discoloration of the nail. The damage is caused by a direct blow or a crush injury to the distal phalanx, for example, getting a finger pinched in a doorway. As blood enters the space, it applies painful pressure to the nailbed. The injury may also be accompanied by distal phalanx fractures, nail avulsion, or finger-tip avulsions. Most subungual hematomas can be relieved with simple trephination, a procedure that involves making a small hole in the nail.[1][2][3][4]
Physical Examination
The provider should examine the entire nail structure for disruption of the nail fold and the whole finger for motor function, sensation, and evaluation of circulation. The extensor mechanism of the distal interphalangeal joint (DIP) should be evaluated by holding the middle phalange and testing the strength of extension by providing resistance to the motion. A decrease in strength compared to the contralateral side indicates a mallet finger injury. Circulation can be tested by capillary refill distal to the injury. In some patients, such as small children, practitioners may be required to perform a digital nerve block to examine the injury.
Testing
Three-view radiograph should be obtained to evaluate for underlying fracture, as distal tuft fractures are common. Point of care ultrasound (POCUS) can be used to identify nail bed lacerations and underlying distal tuft fractures that may indicate a more involved repair.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The complete nail structure is called the perionychium. It is composed of the nail fold, the paronychium (the dorsal skin of the fingertip), the hyponychium (the keratinized distal end of the nail bed which is in contact with the skin of the fingertip), the nailbed (composed of the germinal and sterile matrices) and nail. The germinal matrix is located on the ventral floor of the proximal nail fold and produces 90% of the nail cells. It extends to the lunula, the crescent-shaped lighter portion of the nail. The sterile matrix is highly vascularized and located on the ventral floor of the distal nail bed and adds layers of cells responsible for attaching the nail to the nail bed.
Indications
Current recommendations for drainage of acute (less than 48 hours) subungual hematomas advocate for trephination, a procedure where a hole is made in the nail to drain the hematoma. Previous recommendations were to remove the nail for any hematoma greater than 50% of the nail or greater than 25% of the nail in the presence of a fracture. Several studies have shown that trephination has an equal cosmetic outcome and similar complication rates for the majority of cases.[5][6][7][8][9]
Contraindications
There are no absolute contraindications to trephination; however, in some situations, patients may have better cosmetic outcomes with nail removal and nail bed repair. Subungal hematoma with associated avulsion of the nail, a displaced distal phalanx fracture, and a proximal fracture involving the germinal matrix may require a surgical consult for removal of the nail and nail bed repair. In the event of the nontraumatic development of subungual hematoma, the patient may not benefit from trephination. Examples of nontraumatic subungual hematoma include a variety of tumors, including a junctional nevus, melanoma, or splinter hemorrhages.
Equipment
Supplies include:
- Personal protective equipment (PPE): Face mask with eye shield and gloves
- Digital block: 25-gauge needle, 3-ml syringe, 1% lidocaine, topical antiseptic, and gauze
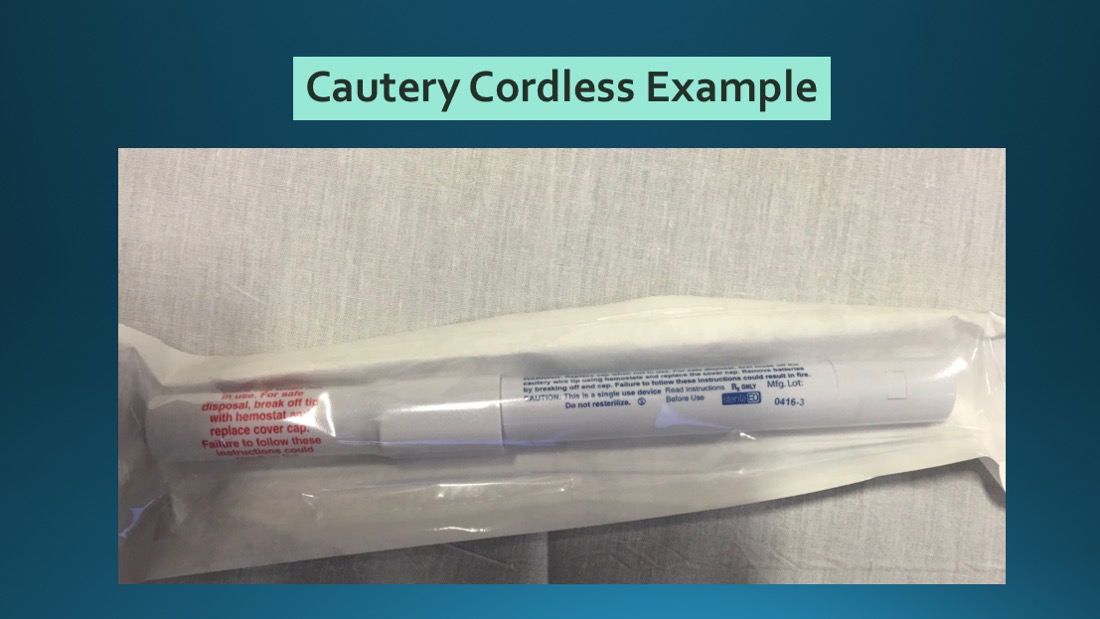
- Trephination: Electrocautery device or an 18-gauge needle
If you have no other supplies available, a heated paperclip can do in a pinch.
Preparation
Clean the digit with chlorhexidine or povidone/iodine solution.
Patients with distal phalanx fractures may benefit from a digital block. However, this is frequently more painful than the procedure.
Obtain consent before the procedure. Discuss with the patient that they can expect to bleed from the trephination site, and complications include loss of the nail, re-accumulation of hematoma, and infection.
Technique or Treatment
- Handheld electrocautery: Use electrocautery at a 90-degree angle to the nail to make a hole through the nail over the central area of the hematoma. A capillary tube, such as a heparinized hematocrit tube, can be used to draw out the hematoma.
- Needle: Place an 18-gauge needle at a 90-degree angle over the central area of the hematoma and rotate the needle in a drilling fashion to create a hole through the nail. Use smaller gauge needles in children if needed. If you use a smaller gauge needle, several holes may need to be drilled to provide relief.
- If no other supplies are present, use a heated paperclip. Heat the paperclip over a flame until red hot and touch to nail at a 90-degree angle to burn a hole through the nail over the central area of the hematoma.
Once a hole is created, it is expected that blood will drain out from the hematoma, resolving most of the patient's pain. It may take more than one trephination to decompress the hematoma completely. Take care when advancing through the nail to avoid damage to the nail bed. Bandage the site with sterile gauze in instruct the patient to keep the digit clean and dry.
Complications
Follow-up instructions should be given to the patient with advisement not to soak the finger as this can cause an introduction of bacteria. Also, inform the patient that blood may continue to ooze from the hole in the nail for 1 to 2 days. Instructions for re-evaluation should be given in the event of signs of infection such as warmth, redness, increasing swelling and fever, and reaccumulation of the hematoma with pain. Non-displaced distal phalanx fractures should be splinted in an extension splint for 4 weeks, and the patient should follow up with a hand specialist. The patient should be informed that the hematoma should advance distally over the next several weeks. If the hematoma is not advancing, they should see a dermatologist for further evaluation of the hematoma due to the possibility of abnormally growing tissue such as melanoma or a nevus. There is no current consensus on post-procedure antibiotics, and they are currently not recommended due to a small observational study that evaluated 47 patients and found no benefit from antibiotics.
Clinical Significance
This injury is a frequent complaint in both the pediatric and adult populations. It is also seen in austere environments. Multiple strategies, including low-tech ones, will be beneficial to promptly and adequately treat patients.
Enhancing Healthcare Team Outcomes
Management of a subungual hematoma is often done by the emergency department physician, nurse practitioner, primary care provider, or surgeon, typically with the assistance of a nurse stabilizing the finger. The key is to ensure that the hematoma is not older than 48 hours. In most cases, the hematoma can be drained with a large needle without complications. Follow-up of patients is recommended to ensure that there is no infection and the hematoma has resolved.
Media
(Click Image to Enlarge)
References
Garcia-Rodriguez JA. Draining a subungual hematoma: procedures and assessments video series. Canadian family physician Medecin de famille canadien. 2013 Aug:59(8):853 [PubMed PMID: 23946029]
Khan MA, West E, Tyler M. Two millimetre biopsy punch: a painless and practical instrument for evacuation of subungual haematomas in adults and children. The Journal of hand surgery, European volume. 2011 Sep:36(7):615-7. doi: 10.1177/1753193411414629. Epub 2011 Jul 1 [PubMed PMID: 21724686]
Level 3 (low-level) evidenceKain N, Koshy O. Evacuation of subungual haematomas using punch biopsy. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2010 Nov:63(11):1932-3. doi: 10.1016/j.bjps.2010.03.023. Epub 2010 Mar 31 [PubMed PMID: 20359972]
Level 3 (low-level) evidenceCohen PR, Schulze KE, Nelson BR. Subungual hematoma. Dermatology nursing. 2007 Feb:19(1):83-4 [PubMed PMID: 17330560]
Level 3 (low-level) evidenceSalter SA, Ciocon DH, Gowrishankar TR, Kimball AB. Controlled nail trephination for subungual hematoma. The American journal of emergency medicine. 2006 Nov:24(7):875-7 [PubMed PMID: 17098113]
Level 3 (low-level) evidenceSkinner PB Jr. Management of traumatic subungual hematoma. American family physician. 2005 Mar 1:71(5):856 [PubMed PMID: 15768614]
Level 3 (low-level) evidenceRichardson M. Selecting a treatment option in subungual haematoma management. Nursing times. 2004 Nov 16-22:100(46):59, 61, 63 [PubMed PMID: 15595491]
Scott PM. Subungual hematoma evacuation. JAAPA : official journal of the American Academy of Physician Assistants. 2002 Mar:15(3):63-5 [PubMed PMID: 11949545]
Roser SE, Gellman H. Comparison of nail bed repair versus nail trephination for subungual hematomas in children. The Journal of hand surgery. 1999 Nov:24(6):1166-70 [PubMed PMID: 10584937]