Introduction
The rectum initiates the terminal section of the large intestine at the level of the S3 vertebra, just after the sigmoid colon. Approximately 15 cm long, it is characterized by the cessation of the omental appendices and the absence of teniae coli and haustra. It is distally continuous with the anal canal as it protrudes through the pelvic diaphragm/levator ani. The rectum plays a significant role in fecal continence and the storage of feces via the ampulla. The anal canal is the final portion of the large intestine and is approximately 3 cm long. The anal canal also contributes to the maintenance of fecal continence and has great clinical significance due to the different embryological origins of the superior and inferior sections of the canal. Disruption in the development of the hindgut either environmentally or genetically can cause many disorders of the rectum and anal canal.[1][2]
Development
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Development
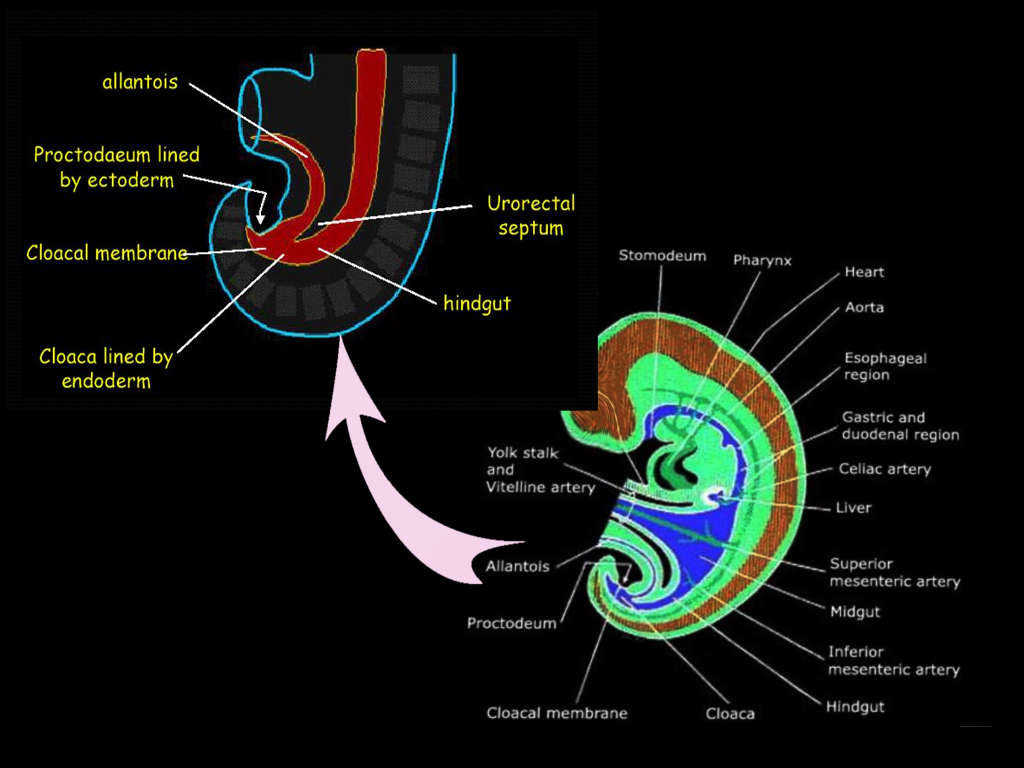
The gastrointestinal tract arises by the beginning of the third week of embryonic development. During a process called gastrulation, the three germ layers form. The germ layers include the ectoderm, mesoderm, and endoderm, which together compose the embryonic disc. The cranial end of the embryonic disc consists of the oropharyngeal membrane, which ultimately forms the mouth, and the caudal end includes the cloacal membrane, which forms the anus.[3] During the fourth week, the primordial gastrointestinal tract begins to form from the endoderm. As the embryo folds towards the midline, the endoderm creates a gut tube that is suspended by mesentery, or double layer of peritoneum. The gut tube divides into the foregut, midgut, and hindgut. The hindgut forms the distal one-third of the transverse colon, the descending colon, the sigmoid colon, rectum, and the superior portion of the anal canal. The terminal end of the hindgut includes the cloaca, which forms not only the gastrointestinal tract but also the urogenital tract.
Towards the caudal end of the cloaca is an area called the cloacal membrane, which is a boundary between the endoderm layer and the ectoderm layer with no mesoderm in between; this ultimately forms the proctodeum. A mesoderm-derived urorectal septum divides the cloaca into the ventral urogenital cavity and the dorsal anorectal canal by week seven or eight.[3] At this point, the terminal ends of both the urogenital cavity and the anorectal canal open at the cloacal membrane. This opening at the cloacal membrane is significant because the anal canal now forms from both endoderm and ectoderm. The superior two-thirds of the anal canal derives from the hindgut, and the inferior one-third of the anal canal derives from the ectodermal proctodeum. The junction that delineates these two epithelia is called the pectinate line or the dentate line.[3]
Cellular
Rectum
- The rectum derives from the endoderm.
- The layers of the rectum include the mucosa (which itself includes the simple columnar epithelial cells, lamina propria, and muscularis mucosa), submucosa, muscularis propria, and serosa.[2]
Anal Canal
- The anal canal divides into superior and inferior parts. The superior two-thirds are derived from the endoderm and are lined by simple columnar epithelial cells. The inferior one-third is derived from ectoderm and is lined by stratified squamous epithelial cells.[2]
Molecular Level
Sonic Hedgehog
- This sonic hedgehog signal transduction pathway is associated with the development of the gastrointestinal tract. The thought is that the development of the concentric layers of the gut tube, including the mucosa, submucosa, and muscularis propria are due to the expression of sonic hedgehog proteins in the endoderm.[4] The growth of these layers has as its basis the expression of sonic hedgehog molecule. For example, the initial high expression of sonic hedgehog stops the growth of nervous tissue and smooth muscle that are close to the endoderm. This inhibition allows the creation of a thin layer of connective tissue called the lamina propria and the surrounding submucosa. As we go further out into the outer layers, the concentration of sonic hedgehog diminishes, allowing the growth of the muscularis externa with its two layers of muscle as well as the myenteric (Auerbach's) plexus.[4][5]
- The sonic hedgehog gene also has a role in inducing other gene expressions such as Bmp4 (bone morphogenetic protein) and Hoxdl3 in the hindgut. These genes seem to play an important role in the morphology of the hindgut, as well.[5]
Homeobox Gene
- The HOX genes are expressed along the lateral plate mesoderm of the GI tract during development and might play a role in the growth and differentiation of the epithelium. Some mice studies have shown that misaligning sequences of these genes or ectopic expression of hox genes have resulted in the development of hamartomas in the gastric mucosa. Inactivation of some hox genes has correlated with absence anal sphincters, lumen blockage, and disruption of GI musculature, which demonstrates the importance of these genes in the development of the GI tract.[6][7]
- The cranio-caudal development of the gut and differentiation into various organs depends on the expression of many genes, including the hox genes. The expression of these genes appears to be highly regulated by the concentration gradient of retinoic acid.[6]
Para-Hox Cluster
- Cdx1 and Cdx2 gene expression is upregulated during gut maturation and gets transcribed in the endoderm of the hindgut. A relationship exists between the expression of these genes and the development, differentiation, and maintenance of the intestinal epithelium. Disruption in the Cdx2 gene has links to various hindgut abnormalities such as failure of colon development, terminal blockage, colonic polyps, and intestinal metaplasia in mice.[6][7]
Sox Family
- There is evidence showing that the Sox genes play a critical role in the development of the intestines and its stem cell function. These DNA-sequence specific transcription factors, specifically Sox9, Sox2, and Sox17, get expressed in the intestinal epithelium. These genes also get expressed in Paneth cells, enteroendocrine cells, and intestinal crypts, all of which contribute to the development of stem cells.[8][9]
- The Sox genes also seem to play a role in cancer. Some Sox genes, including Sox7 and Sox 9, have tumor suppressive functions and are sometimes down-regulated in colorectal cancer. [8]
GDNF
- The enteric nervous system is a system of neurons embedded in the lining of the GI tract and derive from neural crest cells. It has a significant role in the regulation of GI motility (peristalsis) and secretion of enzymes through an autonomous operation.[10] Studies have shown that GDNF or glial-cell-line-derived neurotrophic factor is essential in the proliferation, differentiation, and migration of enteric neural crest cells, which demonstrates the significance of GDNF in the development of the enteric nervous system. Studies have shown the possibility of the enhancement of enteric neural progenitors using GDNF for stem cell therapy for congenital diseases of the enteric nervous system.[10][11]
Endothelin
- Endothelin also contributes to the development of the enteric neural crest cells. Endothelin has associated with the prevention of premature neuronal differentiation. ETB receptors seem to play a role in smooth muscle development, and it works together with endothelin to regulate the development and differentiation of the enteric nervous system.[12] When ETB receptors are activated, endothelin halts neuron differentiation and promotes smooth muscle development. Without the interaction of ETB receptors and endothelin, neurons develop prematurely, and it may leave segments of the colon without ganglions.[12][13]
Function
The rectum plays a role in fecal continence and the storage of feces. Directly above the pelvic diaphragm or the levator ani and the anococcygeal ligament is a dilation of the terminal rectum known as the ampulla. This area is the location where feces accumulate and remain until defecation. The ampulla of the rectum is very distensible and is capable of regulating the movement of fecal material into the anal canal for expulsion. The shape of the rectum, in conjunction with the flexures created along the way, also aids in the mechanism of fecal continence.[14]
The anal canal also helps with the storage and expulsion of feces. The superior portion of the anal canal contains a circular muscle layer called the internal anal sphincter, which is tonically contracted most of the time to prevent leakage. The involuntary contraction of this muscle gets stimulated by the sympathetic nervous system and gets inhibited by the parasympathetic nervous system. As feces or gas passes through, the distension in the rectal ampulla causes a temporary relaxation of the internal anal sphincter and a voluntary contraction of the external anal sphincter, which is in the inferior portion of the anal canal.[15] Occasionally, recruitment of the puborectalis muscle is required to halt fecal expulsion. For defecation to occur, both sphincters must be relaxed.[14]
Testing
Anorectal manometry: Measures and assesses the anal sphincter (internal and external) and rectal pressure and its function. This method is used to evaluate patients with fecal incontinence and constipation. It can directly measure the luminal pressure, including the high-pressure zone, resting pressure, squeezing pressure, rectal sensation/compliance, and the anorectal inhibitory reflex.[16]
Defecating proctography/Defecography: A study using X-ray imaging to evaluate anatomic defects of the anorectal region and function of the puborectalis muscle. A contrast filled paste gets initially introduced to the rectum, and the patient is instructed to defecate in a series of stages (relaxation, contraction, tensing of the abdomen, and evacuation).[16]
Balloon capacity and compliance test: Evaluates the function of the rectum using a device (plastic catheter with a latex balloon attached), which is inserted into the rectum and gradually filled with warm water. During this process, the volume and pressure are measured.[16]
Balloon evacuation study: This test is similar to the balloon capacity and compliance test in which a catheter with a small balloon gets inserted into the rectum and filled with water. Different volumes of water get loaded inside the balloon, and the patient is instructed to evacuate the balloon. This procedure is done to evaluate the opening of the anal canal and to assess the relaxation of the pelvic floor.[16]
Pudendal nerve terminal motor latency: A probe designed to stimulate and record nerve activity is placed on the physician's gloved finger, which is then inserted into the rectum to measure pudendal nerve activity (latency to contraction of the anal sphincter muscle). The pudendal nerve innervates the anal sphincter muscles; therefore, this test can be used to assess any injury to that nerve.[16]
Electromyography: A test to measure the ability of the puborectalis muscle and sphincter muscles to relax properly. An electrode is placed inside the rectum, and the activity of these muscles gets evaluated throughout a series of stages (relaxation, contraction, and evacuation).[16]
Endoanal Ultrasonography: The use of ultrasound imaging to examine rectal lesions, defects, or injuries to the surrounding tissues.[16]
Suction rectal biopsy: Gold standard for the diagnosis of Hirschsprung disease. A biopsy is taken two cm above the dentate line, and the absence of ganglion cells on histology confirms the diagnosis. Hypertrophic nerve fibers may be present in addition to this finding.[16]
Contrast enema: Used as one of the diagnostic methods for Hirschsprung disease. Useful for localization of the aganglionic segment by looking for a narrowed rectum. Diagnostic confirmation is via a rectal biopsy.[16]
Pathophysiology
The pectinate or dentate line is the junction between the superior and inferior anal canal. There are many differences between these two regions, including their embryological origins, innervation, venous and arterial supply, and lymphatic supply. Above the pectinate line, the anal canal has an endodermal origin and is lined by simple columnar epithelia. Blood supply is from the superior rectal artery, which originates from the inferior mesenteric artery and returns via the superior rectal veins into the inferior mesenteric vein.[17] Due to the venous anastomoses that occurs in the anal canal and the backup of blood flow into the rectal veins, hemorrhoids may be present in patients with portal hypertension. The lymphatic drainage of the superior anal canal is via internal iliac lymph nodes. The superior anal canal receives innervation from the inferior hypogastric plexus, which is a visceral innervation. It has both sympathetic and parasympathetic functions that control the tonicity of the internal anal sphincter, thereby contributing to the rectal ampulla reflex. The rectal ampulla senses the distension created by the buildup of feces and causes an inhibitory reflex of the internal anal sphincter, facilitating fecal continence.
Below the pectinate line, the anal canal has an ectodermal origin and is predominantly lined by stratified squamous epithelium. The inferior rectal canal obtains its blood supply from the inferior rectal artery, which originates from the internal iliac artery. Blood returns via the inferior rectal vein, which ultimately drains into the inferior vena cava.[17] The lymphatic drainage of the inferior anal canal is the superficial inguinal lymph nodes. The inferior anal canal receives somatic innervation via the branches of the pudendal nerve, specifically the inferior anal/rectal nerve. Its efferent somatic innervation controls the voluntary actions of the external anal sphincter. Due to its somatic innervation, it can sense pain, temperature, and touch. This difference in innervation is implicated in the clinical presentation of hemorrhoids and anal fissures. Patients with lesions below the pectinate line usually complain of significant pain with any contact near the lesions, and pain is often unbearable, whereas lesions above the pectinate line often go unnoticed because of its visceral innervation and the lack of pain sensation.[2]
Clinical Significance
- Anorectal malformations result from any disruption or abnormality during the process of embryological development of the gut tube. By the completion of the fifth week of development, the endoderm proliferates and occludes the lumen of the entire GI tract. The lumen becomes recanalized via apoptosis during the seventh week and completes by the ninth week.[3] Errors in the recanalization process can lead to many pathologies, including stenosis, occlusion, or duplication of the gut tube. These anomalies often cause significant challenges in daily living. Duplication of bowel may leave blind pouches throughout the gut where food particles or feces can accumulate, which will eventually lead to inflammation and infection. Other anomalies such as occlusion or stricture can prevent normal fecal continence and evacuation of feces. The presence of trisomy 21 is a significant risk factor in anorectal malformations. The abnormal development of the urorectal septum also seems to play a vital role in the development of these malformations. When the distal rectum ends in a blind pouch above the level of the puborectalis muscle, it classifies as anorectal agenesis. A blind-ending rectum below the level of the puborectalis muscle classifies as anal agenesis. These conditions are usually associated with an absent anus and anal canal, and it may present with or without a fistula.[3]
- Hirschsprung's disease
- During the development of the GI tract, enteric neural crest cells migrate from the anterior foregut caudally throughout the entire GI tract and form the enteric nervous system. Disruption of this migration results in an aganglionic segment of the colon, which causes physiologic obstruction most commonly in the distal portion of the colon.[3] Patients typically present with symptoms of distal intestinal obstruction, including abdominal distension, bilious emesis, and failure to pass meconium or stool. A positive "squirt sign" or an explosive excretion of gas and stool may be present during a digital rectal exam. It is also worth noting that the RET protooncogene usually presents in patients with Hirschsprung disease.
- Imperforate anus
- Failure in the breakdown of the anal membrane before birth. This congenital defect disrupts the opening to the anus.
- Adenocarcinoma
- Superior to the pectinate line, the lining of the anal canal is simple columnar epithelium. Therefore, the superior anal canal is more likely to develop adenocarcinoma.[17]
- Squamous cell carcinoma
- Inferior to the pectinate line, the lining of the anal canal is stratified squamous epithelium. Therefore, the inferior anal canal is more likely to develop squamous cell carcinoma.[17]
Media
References
Wang YHW, Wiseman J. Anatomy, Abdomen and Pelvis, Rectum. StatPearls. 2024 Jan:(): [PubMed PMID: 30725930]
Lee JM, Kim NK. Essential Anatomy of the Anorectum for Colorectal Surgeons Focused on the Gross Anatomy and Histologic Findings. Annals of coloproctology. 2018 Apr:34(2):59-71. doi: 10.3393/ac.2017.12.15. Epub 2018 Apr 30 [PubMed PMID: 29742860]
Bhatia A, Shatanof RA, Bordoni B. Embryology, Gastrointestinal. StatPearls. 2024 Jan:(): [PubMed PMID: 30725857]
Merchant JL, Hedgehog signalling in gut development, physiology and cancer. The Journal of physiology. 2012 Feb 1 [PubMed PMID: 22144577]
Level 3 (low-level) evidenceFukuda K, Yasugi S. Versatile roles for sonic hedgehog in gut development. Journal of gastroenterology. 2002:37(4):239-46 [PubMed PMID: 11993506]
Level 3 (low-level) evidenceBeck F. Homeobox genes in gut development. Gut. 2002 Sep:51(3):450-4 [PubMed PMID: 12171973]
Level 3 (low-level) evidenceGao N, White P, Kaestner KH. Establishment of intestinal identity and epithelial-mesenchymal signaling by Cdx2. Developmental cell. 2009 Apr:16(4):588-99. doi: 10.1016/j.devcel.2009.02.010. Epub [PubMed PMID: 19386267]
Level 3 (low-level) evidenceFu L, Shi YB. The Sox transcriptional factors: Functions during intestinal development in vertebrates. Seminars in cell & developmental biology. 2017 Mar:63():58-67. doi: 10.1016/j.semcdb.2016.08.022. Epub 2016 Aug 25 [PubMed PMID: 27567710]
Gracz AD, Magness ST. Sry-box (Sox) transcription factors in gastrointestinal physiology and disease. American journal of physiology. Gastrointestinal and liver physiology. 2011 Apr:300(4):G503-15. doi: 10.1152/ajpgi.00489.2010. Epub 2011 Feb 3 [PubMed PMID: 21292996]
Level 3 (low-level) evidenceYoung HM, Hearn CJ, Farlie PG, Canty AJ, Thomas PQ, Newgreen DF. GDNF is a chemoattractant for enteric neural cells. Developmental biology. 2001 Jan 15:229(2):503-16 [PubMed PMID: 11150245]
Level 3 (low-level) evidencePeters RJ, Osinski MA, Hongo JA, Bennett GL, Okragly AJ, Haak-Frendscho M, Epstein ML. GDNF is abundant in the adult rat gut. Journal of the autonomic nervous system. 1998 May 28:70(1-2):115-22 [PubMed PMID: 9686911]
Level 3 (low-level) evidenceGershon MD. Endothelin and the development of the enteric nervous system. Clinical and experimental pharmacology & physiology. 1999 Dec:26(12):985-8 [PubMed PMID: 10626067]
Level 3 (low-level) evidenceBondurand N, Dufour S, Pingault V. News from the endothelin-3/EDNRB signaling pathway: Role during enteric nervous system development and involvement in neural crest-associated disorders. Developmental biology. 2018 Dec 1:444 Suppl 1():S156-S169. doi: 10.1016/j.ydbio.2018.08.014. Epub 2018 Aug 30 [PubMed PMID: 30171849]
Shafik A, Mostafa RM, Shafik I, Ei-Sibai O, Shafik AA. Functional activity of the rectum: A conduit organ or a storage organ or both? World journal of gastroenterology. 2006 Jul 28:12(28):4549-52 [PubMed PMID: 16874870]
Broens PM, Penninckx FM, Ochoa JB. Fecal continence revisited: the anal external sphincter continence reflex. Diseases of the colon and rectum. 2013 Nov:56(11):1273-81. doi: 10.1097/DCR.0b013e3182a42d16. Epub [PubMed PMID: 24105003]
Level 2 (mid-level) evidenceCho HM. Anorectal physiology: test and clinical application. Journal of the Korean Society of Coloproctology. 2010 Oct:26(5):311-5. doi: 10.3393/jksc.2010.26.5.311. Epub 2010 Oct 31 [PubMed PMID: 21152132]
Salati SA, Al Kadi A. Anal cancer - a review. International journal of health sciences. 2012 Jun:6(2):206-30 [PubMed PMID: 23580899]