 Anatomy, Bony Pelvis and Lower Limb: Medial Patellofemoral Ligament
Anatomy, Bony Pelvis and Lower Limb: Medial Patellofemoral Ligament
Introduction
The medial patellofemoral ligament (MPFL) extends from the femur to the superomedial patella and is trapezoidal in shape. It plays a substantial role in stabilizing the medial aspect of the patella, especially in early flexion (0-30 degrees).[1] It restrains the patella and inhibits its lateral displacement.[2]
Injuries to the MPFL are rare but may occur in athletes during sporting accidents or during a traumatic event. If the patella is dislocated laterally, the MPFL is ruptured more than 90% of the time. Patients are at a significantly higher risk of suffering from patellar instability and potentially another patella dislocation if this occurs.[3]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Structure
The medial knee has three soft tissue layers. The most superficial layer only has a minor role in patellar stability. This layer includes the medial retinaculum. The second layer contains the MPFL, medial collateral ligament, and the patellotibial ligament medially.[1] This middle layer plays the most significant role in stabilizing the patella. The third layer is composed of deep tissue, including the joint capsule and the medial patellomeniscal ligament.[3]
The MPFL originates on the femur in a space between the medial epicondyle and adductor tubercle and is superior to the superficial medial collateral ligament.[4] From this origin, it travels anteriorly to unite with the deep portion of vastus medialis oblique fibers to insert on the superomedial aspect of the patella and provide further anatomical stability.
Function
The main function of the MPFL is to stabilize the patella; it is responsible for 50 to 80% of the stability required to prevent lateral patellar dislocation.[3] The MPFL is able to achieve such stability partly by maintaining the patella within the trochlear groove. The medial patellotibial ligament (MPTL) and the medial patellomeniscal ligament (MPML) are also important in maintaining medial patellar stabilization. With flexion greater than 30 degrees, the vastus medialis oblique becomes the primary medial stabilizer of the patella.[5]
Embryology
By the ninth week of gestation, most of the second layer of the knee begins to develop. The second layer contains the MPFL as well as the medial collateral ligament. They develop as a condensation of the joint capsule. By 14 weeks gestation, the development of the knee joint is complete, including its stabilizing ligaments.[6]
Blood Supply and Lymphatics
The main vascular supply to the knee joint is from the popliteal artery though there is a rich network of collaterals that join the deep femoral artery. In the popliteal fossa, the popliteal artery branches into the four genicular arteries that supply the anatomical structures of the knee. Branches of the medial superior genicular artery and the network of genicular anastomosis supply the MPFL and surrounding structures.[7]
Nerves
Cadaver studies have shown numerous free nerve fibers in the MPFL.[8] These fibers are important for proprioception and transmitting sensory information such as proprioception and inflammation. The MPFL, therefore, is vital to maintaining neuromuscular balance and coordination in the knee joint. Damage to the MPFL can disrupt these neurological pathways, which may contribute to instability.[9]
Muscles
While the MPFL is an important medial stabilizer of the patella, certain muscles play a crucial role as dynamic stabilizers of the knee. The muscles are the vastus medialis, rectus femoris, pes anserinus, popliteus, biceps femoris, and semimembranosus. Of these, only the semimembranosus, vastus medialis, and pes anserinus are dynamic stabilizers of the medial knee. Stabilizing factors depend on the position of the knee and the magnitude and direction of a force acting on the knee. These muscles act as primary restraints, reinforcing anatomical structures. The semimembranosus, in particular, has been found to be the primary knee restraint to external rotation and anteromedial rotation.[10]
The quadriceps femoris (QF) is composed of four muscles that insert at the patella and the tibial tuberosity. The patella is a sesamoid bone that is located inside the quadriceps tendon. The rectus femoris, vastus medialis, vastus lateralis, and the vastus intermedius compose the QF and are important stabilizers of the patella.
Of these muscles, the vastus medialis has the most significant contribution to medial knee stability. The deep fibers of the distal edge of the vastus medialis assist the medial patellar retinaculum in reinforcing the joint capsule. The fibers of the vastus medialis oblique are angled at 50 to 55 degrees and pull the patella medially. The vastus medialis oblique, and the vastus lateralis align the patella within the trochlear groove and aid in patellar tracking. This is crucial for patellar stability as the knee moves through flexion and extension.[11]
Physiologic Variants
The space in which the MPFL inserts onto the patella is variable.[12] In 57% of people, it occupies 67% of the proximal portion of the patellar border. In 41% of cases, it occupies 50% of the border. In 1.3%, the MPFL just covers the distal end, and in a separate 1.3% of cases, it inserts across the entire patella.[13]
While the length of the MPFL is rather consistent, averaging 55 mm, its width can vary between 3 to 33 mm. With such a highly variable width, identifying this ligament may be challenging. Additionally, there has also been variability in the literature regarding the origin of the MPFL. Common sites include the medial femoral epicondyle, the adductor tubercle, and the space in between the two. Schottle’s point is a radiographic landmark used to identify the origin of the MPFL. During MPFL reconstruction surgery, fluoroscopy is used intraoperatively to locate this point.[14]
Surgical Considerations
Injury to the MPFL occurs most frequently during lateral patellar dislocation. After an initial dislocation, conservative treatment with physical therapy and short-term immobilization is often recommended. About 35 to 50% of those patients will suffer from another dislocation. A patient with multiple dislocations is considered to have patellar instability and may be treated surgically.[15][12]
Evidence has shown that surgery is preferred in the acute setting, with the presence of a patellar or femoral-based avulsion.[16] Multiple surgical techniques have been reported for MPFL tear, with differences in both fixation and graft selection.[15]
If surgery is pursued, the MPFL will typically be reconstructed from the patient's own tissue or a cadaveric donor. Biomechanical studies have failed to show the superiority of autograft versus allograft, and surgeons thus are increasingly favoring cadaveric tissue.[17]
The surgeon will harvest a graft of this tissue, restructure it to the appropriate dimensions, and then implant it into the patient. This is typically performed as a combination of using both arthroscopic and open surgical techniques. Patients can be discharged on the same day of surgery with a knee brace for short-term immobilization of the joint. Athletes can typically return to sport four to seven months after reconstruction. MPFL reconstructions are often successful with good outcomes, and redislocations are rare. Although redislocations are rare, other postoperative complications such as apprehension and subluxation have been reported.[18]
Lastly, it is important to consider surrounding anatomy and other possible injuries following dislocations as concurrent injuries may substantially contribute to knee instability. In these cases, multiple procedures may be necessary to restore joint stability rather than MPFL repair alone. The quadriceps-angle (Q-angle), which is the angle between the quadriceps load vector and the patellar tendon load vector, has been implicated in patellar mal-tracking. A Q-angle of 20 degrees or larger tends to track the patella laterally, causing pain and putting the patient at an increased risk of dislocation. Patients with a large Q-angle may be candidates for surgical procedures such as an osteotomy of the tibial tubercle or distal femur to correct patellar mal-tracking.[19][20]
Clinical Significance
MPFL injuries occur most frequently in young athletes secondary to a sports accident or traumatic event and are a leading cause of traumatic knee hemarthroses.[18] Certain anatomic abnormalities have been reported that predispose certain patients to patellar instability and MPFL injuries. These include vastus medialis oblique atrophy, patellar dysplasia, trochlear dysplasia, patella alta, and valgus deformity of the knee, among others.[15] Congenital deformities leading to patellofemoral instability are more common in children and adolescents, therefore, placing this demographic at an increased risk of MPFL injury.[21]
In cases of patellar dislocation, the MPFL is ruptured over 90% of the time. In cases of repeat dislocation, it is ruptured nearly 100% of the time. This is the most common cause of MPFL injury, and its incidence is 2 to 3% of all knee injuries. It most often occurs when an internal force is applied to a slightly flexed knee in the valgus position. Patients with an MPFL rupture will present with pain and tenderness to palpation over the medial retinaculum and the medial border of the patella. Often, lateral displacement of the patella can be visualized. Additionally, in patients with a recurrent dislocation, cartilage damage of the trochlea, patella, and lateral femoral condyle are also appreciated on imaging.
An axial image plain film radiograph is sensitive to revealing patellar dislocation. Magnetic resonance imaging (MRI) is the most sensitive for evaluating MPFL injuries. Common injury patterns seen on MRI with MPFL injuries include a tear on the patellar attachment, a tear on the femoral attachment, a tear on both attachments, or attenuation. However, most tears occur on the femoral attachment. MRI in these patients may also show other injuries. Guerrero et al. found that these patients often have loose bodies present and may suffer from patella avulsion fracture, meniscal tears, medial collateral ligament tears, and osteochondral lesions.
Media
(Click Image to Enlarge)
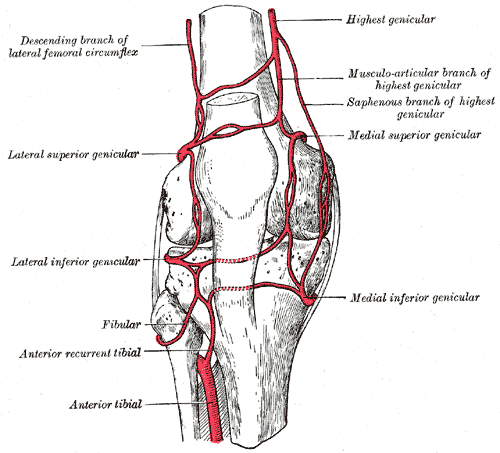
Genicular Anastomosis. This illustration shows the following arteries forming a network around the knee joint: highest genicular, musculoarticular and saphenous branches of the highest genicular, medial superior genicular, medial inferior genicular, anterior tibial, anterior recurrent tibial, fibular, lateral inferior genicular, lateral superior genicular, and descending branch of the lateral femoral circumflex.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Aframian A, Smith TO, Tennent TD, Cobb JP, Hing CB. Origin and insertion of the medial patellofemoral ligament: a systematic review of anatomy. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2017 Dec:25(12):3755-3772. doi: 10.1007/s00167-016-4272-1. Epub 2016 Sep 8 [PubMed PMID: 27631645]
Level 1 (high-level) evidenceBicos J, Fulkerson JP, Amis A. Current concepts review: the medial patellofemoral ligament. The American journal of sports medicine. 2007 Mar:35(3):484-92 [PubMed PMID: 17303819]
Guerrero P, Li X, Patel K, Brown M, Busconi B. Medial patellofemoral ligament injury patterns and associated pathology in lateral patella dislocation: an MRI study. Sports medicine, arthroscopy, rehabilitation, therapy & technology : SMARTT. 2009 Jul 30:1(1):17. doi: 10.1186/1758-2555-1-17. Epub 2009 Jul 30 [PubMed PMID: 19643022]
LaPrade MD, Kennedy MI, Wijdicks CA, LaPrade RF. Anatomy and biomechanics of the medial side of the knee and their surgical implications. Sports medicine and arthroscopy review. 2015 Jun:23(2):63-70. doi: 10.1097/JSA.0000000000000054. Epub [PubMed PMID: 25932874]
Waligora AC, Johanson NA, Hirsch BE. Clinical anatomy of the quadriceps femoris and extensor apparatus of the knee. Clinical orthopaedics and related research. 2009 Dec:467(12):3297-306. doi: 10.1007/s11999-009-1052-y. Epub 2009 Aug 19 [PubMed PMID: 19690926]
Mérida-Velasco JA, Sánchez-Montesinos I, Espín-Ferra J, Rodríguez-Vázquez JF, Mérida-Velasco JR, Jiménez-Collado J. Development of the human knee joint. The Anatomical record. 1997 Jun:248(2):269-78 [PubMed PMID: 9185993]
Shim SS, Leung G. Blood supply of the knee joint. A microangiographic study in children and adults. Clinical orthopaedics and related research. 1986 Jul:(208):119-25 [PubMed PMID: 3522019]
Tuxøe JI, Teir M, Winge S, Nielsen PL. The medial patellofemoral ligament: a dissection study. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2002 May:10(3):138-40 [PubMed PMID: 12012030]
Lobenhoffer P, Biedert R, Stauffer E, Lattermann C, Gerich TG, Müller W. Occurrence and distribution of free nerve endings in the distal iliotibial tract system of the knee. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 1996:4(2):111-5 [PubMed PMID: 8884732]
Kittl C, Becker DK, Raschke MJ, Müller M, Wierer G, Domnick C, Glasbrenner J, Michel P, Herbort M. Dynamic Restraints of the Medial Side of the Knee: The Semimembranosus Corner Revisited. The American journal of sports medicine. 2019 Mar:47(4):863-869. doi: 10.1177/0363546519829384. Epub [PubMed PMID: 30870030]
Miao P, Xu Y, Pan C, Liu H, Wang C. Vastus medialis oblique and vastus lateralis activity during a double-leg semisquat with or without hip adduction in patients with patellofemoral pain syndrome. BMC musculoskeletal disorders. 2015 Oct 12:16():289. doi: 10.1186/s12891-015-0736-6. Epub 2015 Oct 12 [PubMed PMID: 26459411]
Raoulis V, Fyllos A, Klontzas ME, Chytas D, Mitrousias V, Banios K, Maris TG, Karantanas AH, Zibis A. Surgical and Radiological Anatomy of the Medial Patellofemoral Ligament: A Magnetic Resonance Imaging and Cadaveric Study. Diagnostics (Basel, Switzerland). 2021 Nov 10:11(11):. doi: 10.3390/diagnostics11112076. Epub 2021 Nov 10 [PubMed PMID: 34829423]
Krebs C, Tranovich M, Andrews K, Ebraheim N. The medial patellofemoral ligament: Review of the literature. Journal of orthopaedics. 2018 Jun:15(2):596-599. doi: 10.1016/j.jor.2018.05.004. Epub 2018 May 7 [PubMed PMID: 29881201]
Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. The American journal of sports medicine. 2007 May:35(5):801-4 [PubMed PMID: 17267773]
Mistry JB, Bonner KF, Gwam CU, Thomas M, Etcheson JI, Delanois RE. Management of Injuries to the Medial Patellofemoral Ligament: A Review. The journal of knee surgery. 2018 May:31(5):439-447. doi: 10.1055/s-0037-1604142. Epub 2017 Jul 18 [PubMed PMID: 28719945]
Duchman KR, Bollier MJ. The Role of Medial Patellofemoral Ligament Repair and Imbrication. American journal of orthopedics (Belle Mead, N.J.). 2017 Mar/Apr:46(2):87-91 [PubMed PMID: 28437493]
Aliberti GM, Kraeutler MJ, Miskimin C, Scillia AJ, Belk JW, Mulcahey MK. Autograft Versus Allograft for Medial Patellofemoral Ligament Reconstruction: A Systematic Review. Orthopaedic journal of sports medicine. 2021 Oct:9(10):23259671211046639. doi: 10.1177/23259671211046639. Epub 2021 Oct 19 [PubMed PMID: 34692883]
Level 1 (high-level) evidenceKruckeberg BM, Chahla J, Moatshe G, Cinque ME, Muckenhirn KJ, Godin JA, Ridley TJ, Brady AW, Arendt EA, LaPrade RF. Quantitative and Qualitative Analysis of the Medial Patellar Ligaments: An Anatomic and Radiographic Study. The American journal of sports medicine. 2018 Jan:46(1):153-162. doi: 10.1177/0363546517729818. Epub 2017 Oct 10 [PubMed PMID: 29016187]
Level 2 (mid-level) evidenceMizuno Y,Kumagai M,Mattessich SM,Elias JJ,Ramrattan N,Cosgarea AJ,Chao EY, Q-angle influences tibiofemoral and patellofemoral kinematics. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2001 Sep; [PubMed PMID: 11562129]
Hall MJ, Mandalia VI. Tibial tubercle osteotomy for patello-femoral joint disorders. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2016 Mar:24(3):855-61. doi: 10.1007/s00167-014-3388-4. Epub 2014 Oct 19 [PubMed PMID: 25326765]
Hensler D, Sillanpaa PJ, Schoettle PB. Medial patellofemoral ligament: anatomy, injury and treatment in the adolescent knee. Current opinion in pediatrics. 2014 Feb:26(1):70-8. doi: 10.1097/MOP.0000000000000055. Epub [PubMed PMID: 24362407]
Level 3 (low-level) evidence