Introduction
Gestational age is a key piece of data used by healthcare providers to determine the timing of various screening tests and assessments of the fetus and mother throughout pregnancy. Gestational age may be assessed at any time during pregnancy, and several modes of assessment exist, each requiring different equipment or skills and with varying degrees of accuracy. Obtaining more accurate estimates of gestational age through better diagnostic approaches may initiate more prompt medical management of a pregnant patient.
There are numerous approaches to assess gestational age. Before sonography, practitioners had to rely on detailed histories and physical exam findings. In particular, determining the date of the last known menstrual period was of significance. Inputting the date of the last menstrual period into various formulas can give both an estimated gestational age and an estimated delivery date. Physical exam findings such as determining uterine fundal height is also a method for estimating gestational age.[1][2]
Ultrasound has emerged as the more accurate method of assessing fetal gestational age, especially in the first trimester. Both transvaginal and transabdominal probe assessments are used to obtain a more accurate measurement of gestational age. Transvaginal is more helpful in first trimester pregnancies. Multiple parameters have been described using ultrasound to aid in calculating gestational age and will be described here. Additionally, postnatal scoring systems involving focused physical and neurologic exams may also provide insight into gestational age.[3][4]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The uterus is a pelvic organ that will nurture the developing fetus. Approximately 4 weeks after conception, the uterus will increase about 1 cm in size every week. Between 4.5 to 5 weeks of gestation, a gestational sac or intrauterine fluid collection will form. The next remarkable finding occurs between 5 to 6 weeks with the development of the yolk sac. This structure may remain present until 10 weeks. A fetal pole with cardiac activity can be detected between 5.5 to 6 weeks. After this period, the embryo further develops with more discernable organs and anatomical features. When using ultrasound to visualize anatomy, pelvic landmarks include the bladder, uterine wall, vaginal stripe, and rectum. The bladder is typically anterior and inferior to the uterus. The bladder wall will be circular with an anechoic (black) fluid-filled center. The bladder will range in size based on the amount of urine being retained. The uterus will have a thick muscular isoechoic (gray) wall with an anechoic (black) center where an intrauterine pregnancy at varying stages can be identified. Differentiating the bladder from the uterus can be done easily by looking at the thickness of the wall. The uterine wall is significantly thicker than the bladder wall. The vaginal stripe is posterior to the bladder. The rectum will be the most posterior circular structure, on pelvic ultrasound, with either an anechoic (black) or isoechoic (gray) center on the exam.[5]
Indications
All pregnant patients should have a gestational age calculated for safe prenatal evaluation throughout the remainder of the pregnancy for both mother and fetus.
Contraindications
There are no specific contraindications to assessing a pregnant patient's gestational age. However, the modality utilized to assess gestational age may not be appropriate for certain patients. A transvaginal ultrasound exam should not be performed in a pregnant patient with vaginal bleeding and known placenta previa, a pregnant patient with premature rupture of membranes, and a patient who refuses exam despite informed discussion. There are no specific contraindications to transabdominal ultrasound; however, scanning over an open wound would be suboptimal for patient care and image acquisition.
Equipment
Ultrasound machine with a phased array or curvilinear probe for the transabdominal approach. Endocavitary probe for the transvaginal approach.[6]
Personnel
An experienced ultrasonographer should evaluate gestational age in a pregnant patient. Experience can include specific bedside hands-on training with an ultrasound-credentialed instructor, continuous medical education courses or seminars, or other ultrasound education. The healthcare provider performing the bedside ultrasound evaluation should have specific training for estimating gestational age and feel comfortable making a gestational age estimate based on their previous experience and own-assessment of their capabilities and skill level. For a more accurate assessment of gestational age, a pregnant patient should undergo an evaluation by a certified ultrasound technician.
Preparation
Preparation for assessment of gestational age by ultrasound includes describing the procedure to the patient and the risks and benefits of using ultrasound to evaluate their pregnancy. Consent should be obtained from your patient before beginning. When performing a transvaginal ultrasound exam, an appropriate chaperone should be present. Patient comfort should be considered throughout the evaluation.
Technique or Treatment
Prenatal Techniques
Non-Sonographic Methods for Determining Gestational Age
- Naegele’s Rule: Establish the date of the last menstrual period by obtaining a history from the patient. From this date, add 1 year and 7 days, then subtract 3 months. This will approximate the estimated delivery date. The date of the last known menstrual period will give the approximate start date for age of the fetus.[7]
- Uterine Size: The uterus has been described as a soft and globular pelvic organ. In pregnancy, the uterus increases in size to accommodate the developing fetus. At approximately 12 weeks gestation the uterus becomes large enough to be palpable just above the pubic symphysis. At 16 weeks gestation, the fundus of the uterus can be palpated at the midpoint between the umbilicus and the pubic symphysis. At 20 weeks gestation, the fundus can be palpable at the level of the umbilicus. After 20 weeks of gestation, the pubic symphysis to fundal height in centimeters should correlate with the week of gestation.
Sonographic Methods for Determining Gestational Age
- First Trimester Dating: Sonographic assessment within the first 13 weeks and 6 days will provide the most accurate estimate of gestational age. Both transvaginal and transabdominal approaches may be used. However, the transvaginal approach may provide a more clear and accurate view of early embryonic structures. Although the gestational sac and yolk sac are the first measurable markers visible on ultrasound, these poorly correlate with gestational age.
- The crown-rump length (CRL) is the most accurate measurement correlating with gestational age. Using the mean of three measurements, CRL can be determined by using the calipers on the ultrasound machine, measuring a straight line from the outer margin of the cephalic pole to the rump of the embryo. This measurement can be plugged into numerous validated tables and formulas that correlate well with gestational age.[8]
- Second Trimester Dating: If gestational age is not determined within the first trimester, alternate sonographic techniques may be used to estimate gestational age. These techniques are generally not recommended as first-line options for dating but are more helpful in determining if fetal size is within normal range. These measurements should not change the gestational age or delivery date if a previous CRL has been calculated within the first trimester.
- Biparietal Diameter (BPD): This biometric parameter is recommended as a strong modality for dating because it has been extensively studied and is well reproduced. The technique involves a transabdominal approach by positioning the phased array or curvilinear transducer perpendicular to the fetal parietal bones. The calvarium should appear as a hyperechoic (bright white) structure that is smooth and symmetric. The BPD is measured along a plane that intersects the third ventricle and the thalami. Using the caliper function, cursors are placed on the outer edge of the proximal skull and the inner edge of the distal skull. This value will give the biparietal diameter.[9]
- Head Circumference (HC): This biometric parameter has been regarded as a good estimator of gestational age with some studies suggesting superiority to the biparietal diameter. This parameter may also be useful clinically in assessing for growth disorders. A similar sonographic approach as the BPD is used here. A phased array or curvilinear transducer is used to visualize a plane that intersects the third ventricle and thalami. However, to achieve the greatest anterior-posterior diameter, the cavum septum pellucidum must be visualized anteriorly, and the tentorial hiatus must be visualized posteriorly. The cerebellum and lateral ventricles should not be visualized in a standard HC view. Using the calipers, mark the cursors on the outer margins of the calvarium bilaterally. The ultrasound should have an elliptical measuring tool that will generate a measurement of the perimeter of the calvarium.[10]
- Femur Length (FL): The femur can be visualized as early as 10 weeks gestation due to its size and density on ultrasound. Using a phased array or curvilinear transducer, align along the long axis of the closest femur. Proximally, visualize either the femoral head or greater trochanter and distally, visualize the femoral condyle. Using the calipers, measure the length of the diaphysis, at the junction of bone and cartilage, taking care not to include the femoral head, greater trochanter, or femoral condyle.[10]
- Abdominal Circumference (AC): The biometric parameter is more difficult to measure and is less able to predict gestational age than the other described techniques accurately. However, it may be useful in fetuses with cranial or limb abnormalities and to estimate a fetal weight and note interval growth. Using the phased array or curvilinear transducer, position the transducer perpendicular to the fetal abdominal wall and visualize the symmetric appearance of the lower ribs. This view should be at the largest diameter of the fetal liver. Note, the fetal stomach is often visualized at this level. The umbilical portion of the left portal vein in its shortest view is another hallmark of appropriate positioning. Using the calipers, obtain four calibration points around the abdomen on the skin edge making sure not to include the rib cage. The elliptical tool may also be used to calculate circumference.[10]
- Third Trimester Dating: If gestational age has not been determined by the third trimester multiple parameters are correlated with estimated age and fetal maturity. For example, femoral epiphyseal ossification centers are often noted at 32 weeks. Proximal tibial ossification centers are visualized at 35 weeks. The proximal humeral ossification centers appear in the late trimester and have been correlated with fetal lung maturity.[11]
Postnatal Techniques
- Dubowitz Method: This was the historically standard method of determining postnatal gestational age based on 34 physical and neurologic assessments. These assessments are divided into 6 categories: tone, tone patterns, reflexes, movements, abnormal signs, and behaviors. Scores are assigned based on a detailed illustration sheet. Higher scores correlate with greater maturity. The total score can be plotted on a graph that also correlates with gestational age.[12]
- New Ballard Score: This improved scoring system is used to determine postnatal gestational age in infants as preterm as 20 weeks. The system is divided into 6 physical maturity components and six neuromuscular components. The physical maturity components include skin, lanugo, plantar creases, breast, ear/eye, and genitals. The neuromuscular components include posture, square window/wrist, arm recoil, popliteal angle, scarf sign, and heel to ear. Detailed illustrations have been created to assist the examiner in determining appropriate scores which correlate with gestational age. This exam is quicker to perform and may be more tolerable for sicker infants.[13]
Complications
Prenatal Techniques
Non-Sonographic Methods for Determining Gestational Age
- Naegele’s Rule: This rule assumes a standardized 28-day menstrual cycle with fertilization occurring on day 14. However, many women have irregular cycles with variability in the length of the follicular phase affecting ovulation. History of last menstrual period may be confounded by early pregnancy bleeding, hormonal contraceptive use, or incorrect recall of last menstrual period date.[7]
- Uterine Size: This finding primarily relies on the provider’s physical examination. This may be confounded by maternal factors including but not limited to obesity, multiple gestation, leiomyoma, and fibroids. The mother may also have a retroverted uterus which will alter normal progressive landmarks. Individual practitioner skill and experience make findings less reliable and reproducible.
Sonographic Methods for Determining Gestational Age
- Crown-rump length (CRL): This parameter becomes less accurate for predicting gestational age and delivery date with the advancement of gestation due to normal embryonic development and variability in anatomic positioning. Once the CRL exceeds 84 mm, the BDP serves as a better indicator for gestational age.[8]
- Biparietal Diameter (BPD): This parameter becomes limited after 22 weeks gestation due to normal biologic development with variations in fetal size and shape. If there is a physiologic or pathologic cause for the skull size and shape to be altered, the BPD may produce false measurements.[9]
- Head Circumference (HC): This parameter is useful for obtaining gestation age, but multiple landmarks need to be identified before taking measurements. After 22 weeks, there is significant variation due to normal development affecting size and shape.[10]
- Femur Length (FC): Multiple errors may occur when obtaining this parameter including but not limited to, non-ossified portions of the femur and not visualizing the full femur. This can lead to incorrect gestational age calculations. Average femur lengths may differ among certain ethnic groups or can be indicative of pathology. Again, this parameter does have variability after 22 weeks due to normal biologic development.[10]
- Abdominal Circumference (AC): This parameter has a wide margin of error for determining gestational age due to multiple factors including asymmetry of the abdomen, changes with respiration and movement, and user skills. Like the other parameters, significant variability is seen after 22 weeks.[10]
- Ossification Centers: These parameters do not directly correlate with exact gestational age. Presence of these ossified centers are rather markers of fetal maturity which is seen later in pregnancy.[11]
Postnatal Techniques
- Dubowitz Method: Due to a large number of criteria needed to perform the exam, this method may be more difficult to perform on sick and preterm infants. Also, it can take up to 20 minutes to perform this exam. Studies have shown that this method tends to overestimate the gestational age.[12]
- New Ballard Score: Although this exam is quicker to perform, studies have shown that this system can overestimate gestational age in preterm infants.[13]
Clinical Significance
Early sonography has been a useful adjunct to the history and physical exam findings in establishing gestational age. Although sonography can visualize the pregnancy at various stages, this tool must be applied appropriately, and the tool's specific limitations must be considered. Determining the most accurate gestational age as early as possible generally allows for the best medical care for both mother and fetus throughout the remainder of the pregnancy.
Enhancing Healthcare Team Outcomes
It is important to obtain a gestational age in all pregnancies to provide the standard of care medical management for both mother and fetus. A combination of history, physical exam, early sonography in the first trimester, and prenatal assessments are all essential to obtaining a more accurate gestational age. Different techniques may be more useful depending on how far along the pregnancy has progressed. Early sonography has been shown to be the most useful predictor of gestational age; however, other late modalities are available to help determine age.
Media
(Click Image to Enlarge)
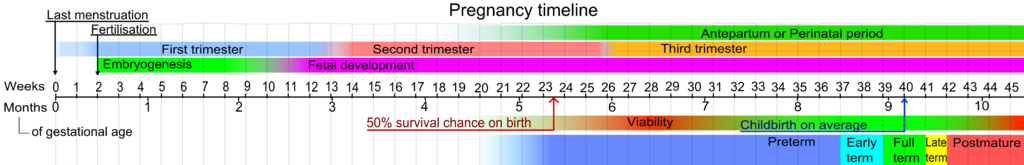
Pregnancy Timeline. The most important step in the initial evaluation of any pregnant patient is establishing an accurate delivery date or due date.
Mikael Häggström, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
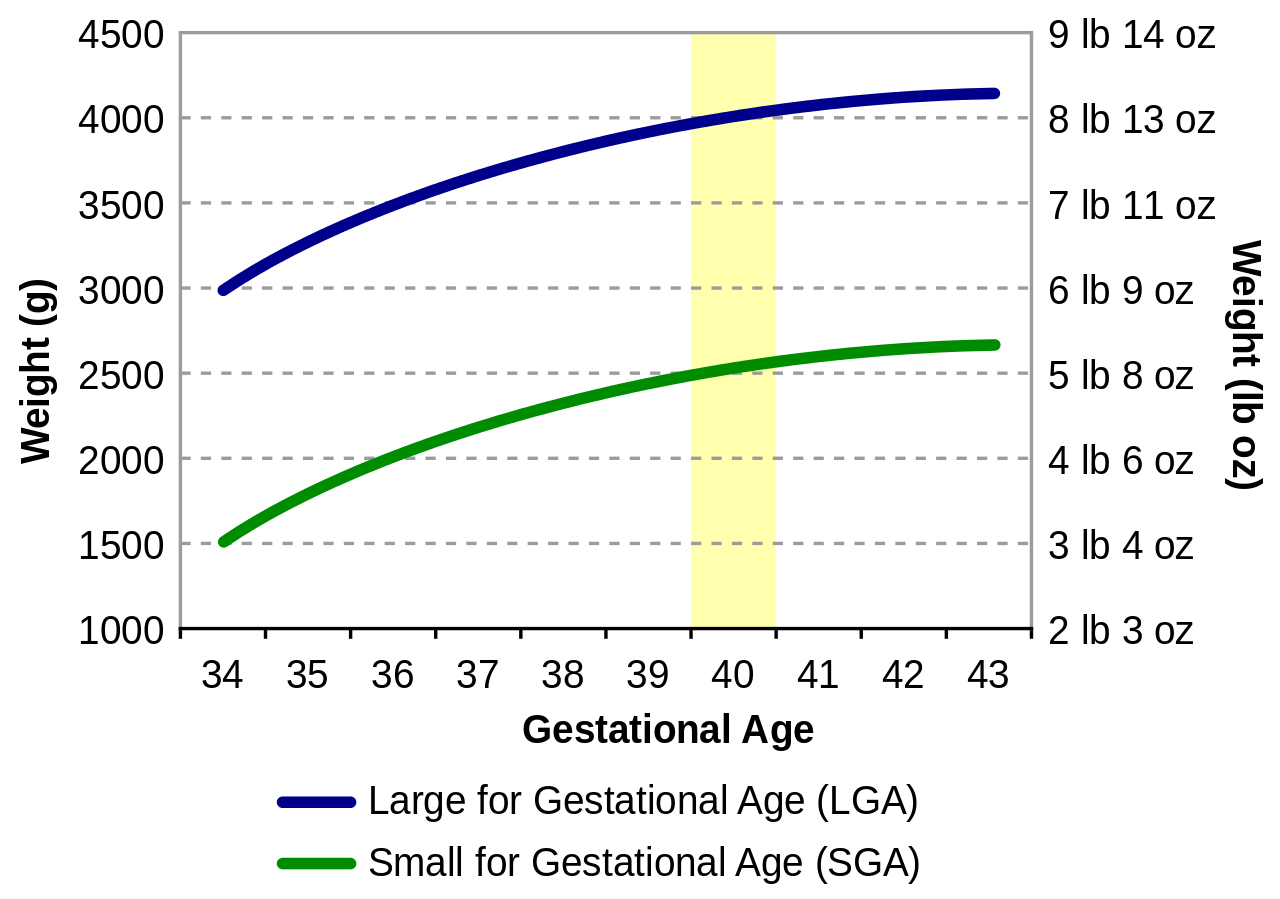
Birth Weight for Gestational Age Chart. Accurate knowledge of the gestational age is important to determine the appropriate intervals and interventions for prenatal care visits.
Public Domain via Wikimedia Commons
References
Robert Peter J, Ho JJ, Valliapan J, Sivasangari S. Symphysial fundal height (SFH) measurement in pregnancy for detecting abnormal fetal growth. The Cochrane database of systematic reviews. 2015 Sep 8:2015(9):CD008136. doi: 10.1002/14651858.CD008136.pub3. Epub 2015 Sep 8 [PubMed PMID: 26346107]
Level 1 (high-level) evidenceAverbach S, Puri M, Blum M, Rocca C. Gestational dating using last menstrual period and bimanual exam for medication abortion in pharmacies and health centers in Nepal. Contraception. 2018 Oct:98(4):296-300. doi: 10.1016/j.contraception.2018.06.004. Epub 2018 Jun 21 [PubMed PMID: 29936150]
van den Heuvel TLA, de Bruijn D, de Korte CL, Ginneken BV. Automated measurement of fetal head circumference using 2D ultrasound images. PloS one. 2018:13(8):e0200412. doi: 10.1371/journal.pone.0200412. Epub 2018 Aug 23 [PubMed PMID: 30138319]
Sasidharan K, Dutta S, Narang A. Validity of New Ballard Score until 7th day of postnatal life in moderately preterm neonates. Archives of disease in childhood. Fetal and neonatal edition. 2009 Jan:94(1):F39-44. doi: 10.1136/adc.2007.122564. Epub [PubMed PMID: 19103779]
Rowling SE, Langer JE, Coleman BG, Nisenbaum HL, Horii SC, Arger PH. Sonography during early pregnancy: dependence of threshold and discriminatory values on transvaginal transducer frequency. AJR. American journal of roentgenology. 1999 Apr:172(4):983-8 [PubMed PMID: 10587132]
Grisolia G, Milano K, Pilu G, Banzi C, David C, Gabrielli S, Rizzo N, Morandi R, Bovicelli L. Biometry of early pregnancy with transvaginal sonography. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 1993 Nov 1:3(6):403-11 [PubMed PMID: 12797241]
Loytved CA, Fleming V. Naegele's rule revisited. Sexual & reproductive healthcare : official journal of the Swedish Association of Midwives. 2016 Jun:8():100-1. doi: 10.1016/j.srhc.2016.01.005. Epub 2016 Feb 4 [PubMed PMID: 27179385]
Robinson HP, Fleming JE. A critical evaluation of sonar "crown-rump length" measurements. British journal of obstetrics and gynaecology. 1975 Sep:82(9):702-10 [PubMed PMID: 1182090]
Hohler CW, Quetel TA. Comparison of ultrasound femur length and biparietal diameter in late pregnancy. American journal of obstetrics and gynecology. 1981 Dec 1:141(7):759-62 [PubMed PMID: 7315902]
Hadlock FP, Deter RL, Harrist RB, Park SK. Estimating fetal age: computer-assisted analysis of multiple fetal growth parameters. Radiology. 1984 Aug:152(2):497-501 [PubMed PMID: 6739822]
Benson CB, Doubilet PM. Sonographic prediction of gestational age: accuracy of second- and third-trimester fetal measurements. AJR. American journal of roentgenology. 1991 Dec:157(6):1275-7 [PubMed PMID: 1950881]
Dubowitz L, Ricciw D, Mercuri E. The Dubowitz neurological examination of the full-term newborn. Mental retardation and developmental disabilities research reviews. 2005:11(1):52-60 [PubMed PMID: 15856443]
Ballard JL, Khoury JC, Wedig K, Wang L, Eilers-Walsman BL, Lipp R. New Ballard Score, expanded to include extremely premature infants. The Journal of pediatrics. 1991 Sep:119(3):417-23 [PubMed PMID: 1880657]