Indications
Procaine is a pharmaceutical medication belonging to the aminoester group of local anesthetics. German chemist Alfred Einhorn first synthesized the drug as a safer anesthetic alternative to cocaine due to its side effect profile, patenting procaine under the trade name “Novocain,” and even today, procaine is often labeled generically as “novocaine” in some parts of the world.[1] Historically, procaine has been used for local, regional, and neuraxial anesthesia via local infiltration, peripheral nerve blockade, and intrathecal injection. Since its development, however, newer local anesthetics such as lidocaine, bupivacaine, and mepivacaine have largely supplanted the use of procaine in everyday practice.[2] Nonetheless, more contemporary applications of procaine include[3][4][2][5]:
- Co-administration with intramuscular penicillin for the treatment of syphilis, pneumococcal pneumonia, scarlet fever, pharyngitis, rheumatic fever, and glomerulonephritis
- Dental procedures such as tooth extractions, cavity fillings, and root canals
- Local analgesia in patients with hypersensitivity to aminoamide local anesthetics
Mechanism of Action
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Mechanism of Action
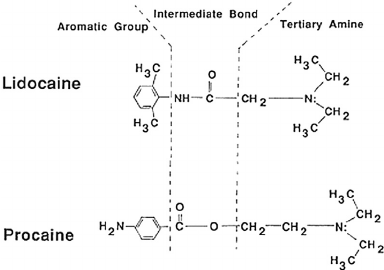
Procaine belongs to a class of analgesic medications known as local anesthetics. All local anesthetics consist of three constituents: a lipophilic aromatic ring, a terminal amine, and an intermediate ester or amide group. The aromatic ring serves to improve the anesthetic's lipid solubility and promote diffusion through epineural and neural membranes, thus correlating to the anesthetic's potency.[5] The terminal amine may be configured in a lipid-soluble tertiary form or as a water-soluble quaternary form and imparts the anesthetic with binary active/inactive states.[5] Finally, the intermediate linkage determines the manner of metabolism and classification, either as an aminoamide (amino group) or aminoester (ester group) local anesthetic. Aminoamides undergo hepatic metabolism, whereas aminoesters are hydrolyzed intravascularly by plasma butyrylcholinesterase into para-aminobenzoic acid (PABA). Procaine belongs to the aminoesters, along with tetracaine, cocaine, benzocaine. Aminoamides include bupivacaine, lidocaine, ropivacaine, and mepivacaine. The primary characteristics and clinical correlates of local anesthetics are [5]:
- Lipid solubility: Potency
- Dissociation constant: Onset
- Intermediate linkage: Metabolism
- Plasma-protein binding affinity: Duration
The fundamental mechanism of analgesia underlying all local anesthetics is the blockade of neurotransmission via inhibition of sodium channels along nerve fibers. The progression of anesthesia, referred to as differential blockage, is predicated on nerve caliber and myelination and generally blocks nerve fibers in the following order from first to last [6]:
- Type B fibers (sympathetic tone)
- Type C (dull pain, warm temperature)
- Type A-delta (sharp pain, cold temperature)
- Type A-gamma (proprioception)
- Type A-beta (touch, pressure)
- Type A-alpha (motor)
After epineural and neural diffusion, procaine reversibly and preferentially binds to active sites on the cytoplasmic aspect of neuronal voltage-gated sodium channels. This binding occurs preferentially during activated states and causes selective inhibition of the open configuration of the sodium channel, thereby preventing sodium influx. The interruption of this influx prevents depolarization needed to initiate and propagate action potentials along the nerve fiber resulting in suppression of neurotransmission of nerve fibers mentioned above, with type C and A-delta fiber suppression mediating the primarily desired analgesic effects of procaine.[7]
Administration
In the United States to date, the Food and Drug Administration (FDA) has approved several formulations of procaine in the form of procaine hydrochloride at 1%, 2%, and 10% concentrations. Dilution and addition of epinephrine may be undertaken depending on the procedure performed. A full discussion of such is beyond the scope of this review. Briefly, for infiltrative administration, 0.25% and 0.5% solutions are generally appropriate with a target single-dose total of up to 350 to 600 mg. Pediatric patients may receive a 0.5% solution for local infiltration with a maximum dose of up to 15 mg/kg. For peripheral nerve blocks, procaine solutions of 0.5%, 1%, and 2% are generally appropriate up to 200 mL, 100 mL, and 50 mL, respectively. For neuraxial anesthesia, the 10% solution is usually the choice with total single doses ranging from 50 to 200 mg, depending on the extent of desired anesthesia with an injection rate of 1mL/5 seconds. For local and regional blockade, epinephrine may be supplemented to induce local vasoconstriction and prolong the duration of action at the local site of injection. Single administration dose should never exceed 100 0mg procaine hydrochloride. Patients with cardiac, renal, and hepatic disease and patients who are elderly or acutely ill should receive reduced doses.
Adverse Effects
The adverse effects of procaine administration are similar to those of other aminoester anesthetics. Increased intravascular levels mediate most side effects; this can be due to overdosage, entry into intravascular spaces, and potentiation from reduced metabolism. More rarely, patients may experience adverse effects secondary to hypersensitivity or idiosyncrasy.
Hypersensitivity may develop in patients either due to procaine or constituent components in the therapeutic suspension such as sulfites (local vasoconstriction) or chlorobutanol (antimicrobial preservative) with aminoesters more likely to induce hypersensitivity than aminoamides.[5] The derivation of procaine from PABA may also result in cross-sensitivity to PABA and its derivatives, as well. Patients often present with anaphylactoid-like symptomatology, including urticaria, pruritus, erythema, laryngeal edema, tachycardia, nausea, vomiting, dizziness, syncope, perspiration, and hyperthermia. Treatment includes cessation of procaine and a tailored regimen of intramuscular epinephrine, supplemental oxygen, intravenous corticosteroids, resuscitative fluids, beta-agonists, and supportive care.
Systemic presence of procaine at supratherapeutic levels results in the compromise of multiple organ systems in a dose-dependent manner known as local anesthetic systemic toxicity (LAST). Procaine, like other anesthetics, binds to beta-adrenergic receptors in addition to voltage-gated sodium channels to mediate cardiotoxic and neurotoxic effects.[8] Cardiac symptoms include heart block, arrhythmia, hemodynamic instability, heart failure, and cardiac arrest.[8][9] Depression of the central nervous system depression may result in varying presentations of tinnitus, blurred vision, dizziness, akathisia, anxiety, tremors, seizures, coma, unconsciousness, and respiratory arrest.[5][9] Management and treatment of procaine-induced LAST include airway management (ventilation, oxygenation), circulatory support (e.g., epinephrine, rhythm control), seizure prophylaxis, and suppression (benzodiazepines, succinylcholine), and reduction of intravascular anesthetic levels (lipid-emulsion, cardiopulmonary bypass).[9][10][11]
Contraindications
Contraindications to procaine include hypersensitivity to procaine or other ester group local anesthetics, PABA, metabolic derivatives of PABA, or to other components of the pharmaceutical suspension. Spinal anesthesia with procaine is contraindicated in cases of septicemia and cerebrospinal diseases such as syphilis and meningitis. Currently, no evidence suggests that procaine is carcinogenic, mutagenic, or gonadotoxic.[12] Per the FDA, the medication has a Pregnancy Category C rating - therefore, its capacity to cause fetal compromise remains not yet fully established.[13] Ideally, procaine should only be given to pregnant women only if the benefit of analgesia and subsequent intervention outweighs the risks. Like with other local anesthetics, procaine administration should be undertaken cautiously in patients with cardiac arrhythmias, asthma, sulfite sensitivity, local/systemic infection, and advanced age or debility.[14]
Monitoring
Following the administration of procaine, signs of local and systemic toxicity or hypersensitivity require monitoring.[9] Moreover, clinicians should note changes to vital signs and the patient's mental status during and after injection. According to the American Society of Anesthesiology, all patients receiving regional or neuraxial anesthetics require monitoring for [15]:
- Electrocardiography (EKG)
- Pulse oximetry
- Blood pressure
The presence of toxicity, hypersensitivity, or concerning findings from monitoring warrants cessation of the medication and undertaking steps to mitigate and/or reverse symptoms.[16]
Enhancing Healthcare Team Outcomes
Newer, more efficacious local anesthetics have largely overshadowed the clinical use of procaine, and as such, is only applicable in a narrow medical context now. Nonetheless, practitioners who continue to use the medication should be acutely aware of its indications, benefits, and risks and should inform patients of these as well. All involved clinical professionals must undertake careful effort (e.g., physicians, dentists, nurses, pharmacists, etc.) to monitor the patient during and after administration of procaine and to promptly recognize signs of hypersensitivity or toxicity as discussed before to prevent and/or abort any adverse outcomes, should they arise.
When a clinician opts to use procaine, they should consult with the pharmacist to ensure there are no potential interactions and that dosing is correct. Nursing will likely administer the drug and should be up to speed on adverse events so they can monitor the patient during the procedure and alert the clinician if there are any concerns. These interprofessional team measures demonstrate how collaboration can optimize procaine use to drive better patient outcomes. [Level 5]
Media
(Click Image to Enlarge)
References
Dunsky JL. Alfred Einhorn: the discoverer of procaine. Journal of the Massachusetts Dental Society. 1997 Fall:46(3):25-6 [PubMed PMID: 9540713]
Ruetsch YA,Böni T,Borgeat A, From cocaine to ropivacaine: the history of local anesthetic drugs. Current topics in medicinal chemistry. 2001 Aug; [PubMed PMID: 11895133]
Level 3 (low-level) evidenceBazakis AM, Akhondi H, Weir AJ. Procaine Penicillin. StatPearls. 2023 Jan:(): [PubMed PMID: 29493977]
Gartlan WA, Rahman S, Pellegrini MV, Reti K. Benzathine Penicillin. StatPearls. 2024 Jan:(): [PubMed PMID: 29939545]
Becker DE, Reed KL. Essentials of local anesthetic pharmacology. Anesthesia progress. 2006 Fall:53(3):98-108; quiz 109-10 [PubMed PMID: 17175824]
Ford DJ, Raj PP, Singh P, Regan KM, Ohlweiler D. Differential peripheral nerve block by local anesthetics in the cat. Anesthesiology. 1984 Jan:60(1):28-33 [PubMed PMID: 6691593]
Level 3 (low-level) evidenceRiccioppo Neto FR,Sperelakis N, Effects of lidocaine, procaine, procainamide and quinidine on electrophysiological properties of cultured embryonic chick hearts. British journal of pharmacology. 1985 Dec; [PubMed PMID: 4075018]
Level 3 (low-level) evidenceShafiei FT,Lopez J, Bupivacaine 2019 Jan; [PubMed PMID: 30422478]
Mahajan A, Derian A. Local Anesthetic Toxicity. StatPearls. 2023 Jan:(): [PubMed PMID: 29763139]
Weinberg GL. Treatment of local anesthetic systemic toxicity (LAST). Regional anesthesia and pain medicine. 2010 Mar-Apr:35(2):188-93. doi: 10.1097/AAP.0b013e3181d246c3. Epub [PubMed PMID: 20216036]
Picard J, Meek T. Lipid emulsion to treat overdose of local anaesthetic: the gift of the glob. Anaesthesia. 2006 Feb:61(2):107-9 [PubMed PMID: 16430560]
Level 3 (low-level) evidenceTurner MD,Singh F,Glickman RS, Dental management of the gravid patient. The New York state dental journal. 2006 Nov; [PubMed PMID: 17203851]
Lee JM,Shin TJ, Use of local anesthetics for dental treatment during pregnancy; safety for parturient. Journal of dental anesthesia and pain medicine. 2017 Jun; [PubMed PMID: 28879335]
Petrikas AZh, Ol'khovskaia EB, Medvedev DV, Diubaĭlo MV. [Disputable issues of Malamed's "Handbook of local anesthesia" (2004)]. Stomatologiia. 2013:92(2):71-6 [PubMed PMID: 23715461]
Gelb AW,Morriss WW,Johnson W,Merry AF,Abayadeera A,Belîi N,Brull SJ,Chibana A,Evans F,Goddia C,Haylock-Loor C,Khan F,Leal S,Lin N,Merchant R,Newton MW,Rowles JS,Sanusi A,Wilson I,Velazquez Berumen A, World Health Organization-World Federation of Societies of Anaesthesiologists (WHO-WFSA) International Standards for a Safe Practice of Anesthesia. Anesthesia and analgesia. 2018 Jun; [PubMed PMID: 29734240]
Wolfe RC, Spillars A. Local Anesthetic Systemic Toxicity: Reviewing Updates From the American Society of Regional Anesthesia and Pain Medicine Practice Advisory. Journal of perianesthesia nursing : official journal of the American Society of PeriAnesthesia Nurses. 2018 Dec:33(6):1000-1005. doi: 10.1016/j.jopan.2018.09.005. Epub [PubMed PMID: 30449428]