Introduction
The thyroid is an endocrine gland located just below the cricoid cartilage in the neck, and it is composed of both the right and the left lobes separated by an isthmus. The thyroid gland functions to produce the thyroid hormone, which is needed by the body to carry out different metabolism. Follicles comprise the thyroid and are the functional and structural units of the gland.[1] Epithelial cells line the follicles, which could be cuboidal or columnar, depending on the state of activity. These cells could develop abnormal growth causing follicular malignancy. Thyroid cancer is one of the most common endocrine tumors and is classified as differentiated or undifferentiated.[2] Differentiated cancers include papillary and follicular thyroid carcinoma, and undifferentiated types include medullary thyroid cancer and anaplastic cancer. Papillary thyroid cancer accounts for most varieties. Follicular thyroid cancer is the second most prevalent type, accounting for 10 to 15% of all thyroid cancer.[3] The undifferentiated types are rare when compared to the differentiated types.[4]
Up to half of follicular carcinoma cases show RAS point mutations, while one-third may show PAX-PPAR-gamma rearrangements, and only 3% show both.[5][6] Follicular thyroid cancer is a tumor of the follicular cells that are cuboidal epithelial cells and have capsular and vascular invasive properties. Compared to follicular carcinoma, follicular adenoma is benign and occurs more commonly with a ratio estimated to be 5 to 1.[7] This article will focus more on the follicular type of thyroid cancer, discussing the etiology, epidemiology, histology, evaluation, staging, and complications of follicular thyroid cancer.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The cause of thyroid cancer has links to radiation exposure, iodine intake, diabetes, obesity, Hashimoto thyroiditis, exogenous estrogen use, and dietary choices.[2] After the 1986 Chornobyl explosion, many radiation-induced cancers were observed, including thyroid cancer.[8] The position of the thyroid makes it an easy target for radiation exposure. The thyroid is very sensitive to radiation at a younger age, and after exposure, the relative risk of having cancer is estimated to persist for over 50 years.[9] Apart from nuclear radiation, individuals can also get exposure through X-rays and CT scans. The increased use of these imaging studies could lead to an increased incidence of thyroid cancer. There is a controversy on whether iodine excess or deficiency causes thyroid cancer.[10]
In some studies, like the one reported by Knobel et al. in 2007, it was found that iodine intake was a predisposing factor for thyroid cancer[11]. In another study by Fortner J.G et al., the observation was that iodine deficiency could lead to thyroid epithelial cell carcinomas[12]. Diabetes and obesity also share links with the rise in thyroid cancer.[13] Hashimoto thyroiditis has been reported to cause thyroid cancer as well, mostly believed because it leads to an increase in the production of pro-inflammatory cytokines and oxidative stress.[2] Diet choices play a significant role in the incidence of thyroid cancer. Foods such as cabbage, broccoli, cauliflower, chicken, pork, and poultry have been found to cause an increased incidence of thyroid cancer while vegetables such as persimmons and tangerines correlate negatively with thyroid cancer incidence.[14] Too much multivitamin use has been shown to cause an increased incidence of thyroid cancer due to iodine content.[14] High nitrate or nitrite-containing foods have also been shown to increase the incidence of thyroid cancer.
Some occupations have been correlated with an increased incidence of thyroid cancer. Occupational exposure to radiation, pesticides, and working in the textile industry has also shown an increased association with thyroid cancer.[15]
Epidemiology
Thyroid cancer ranks as the ninth most common cancer and accounts for 3.8% of all new cancer cases in the United States.[16] In 2017, the number of new cases of thyroid cancer was projected to be 56,780, with females having a higher incidence compared to males.[17] Follicular thyroid cancer is the second most common cause of thyroid cancer, and it accounts for 4% to 39% of all thyroid cancers.[18] Follicular thyroid cancer is more common in older females, with a female-to-male ratio of 3 to 1 and an average age of presentation at 60 years old.[7]
Some studies report that follicular thyroid cancer incidence is approximately 10% in iodine-sufficient areas and 25 to 40% in areas of iodine deficiency.[7] In the United States, the incidence of follicular thyroid cancer has decreased due to the elimination of iodine deficiency.[7][19][7]
History and Physical
Patients with thyroid carcinoma might have an enlargement of the thyroid gland due to the presence of a nodule in either or both thyroid lobes. They can occasionally be symptomatic with either hypothyroid or hyperthyroid characteristics, but they are usually asymptomatic.
Evaluation
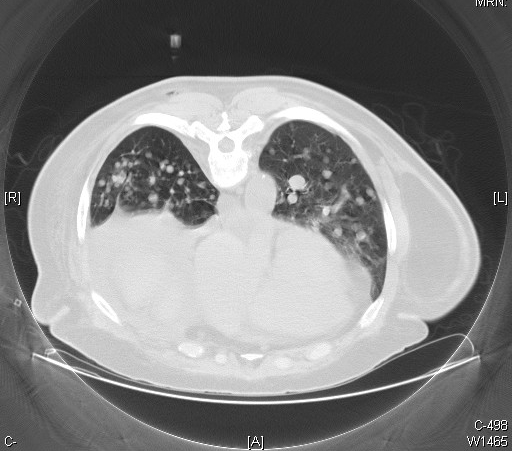
Ultrasound imaging and ultrasound-guided fine needle aspiration or core biopsy are used to diagnose primary thyroid carcinoma. Ultrasound of primary thyroid cancer usually shows solid hypoechoic nodules with micro-calcification, poorly defined margins, and vascular patterns with the dominant intranodular flow, as opposed to perinodular.[20] CT and MRI imaging studies are used to evaluate extrathyroidal tumor extension but not for the thyroid nodule itself.[20] The samples received from fine needle aspiration or core biopsy are then viewed under the microscope for confirmation. Follicular thyroid carcinoma is diagnosed based on pathologic confirmation of follicular cells that do not have the nuclear atypia seen in papillary thyroid cancer, including capsular and vascular invasion. Therefore, the basis of evaluation is mainly the histological findings of the pathologist. Thyroid carcinoma is classified as being follicular if it is invasive and contains mainly follicles. Histologic findings have been reported to vary among pathologists, leading to controversy in the classification of follicular thyroid carcinoma.[21] See Image. Metastatic Follicular Thyroid Carcinoma, CT Scan.
Treatment / Management
The treatment and management of follicular thyroid carcinoma depend on the stage at presentation. Follicular thyroid carcinoma with minimally invasive characteristics is treated with thyroid lobectomy and isthmectomy [22], but for invasive follicular carcinoma, total thyroidectomy, radioiodine ablation, and thyrotropin suppressing medications are all recommended.[23][24] A study reported a 2.1-fold increase in follicular thyroid cancer recurrence in those who did not undergo radioiodine ablation compared to those who did, which is why the standard treatment recommendation is total thyroidectomy followed by radioiodine radiation.[25][26] (B2)
For patients with metastasis to bones and soft tissues, either radiotherapy or chemotherapy, or both are indicated after the total thyroidectomy. Chemotherapy that has been reported to control tumor progression and prolong progression-free survival includes tyrosine kinase inhibitors such as sorafenib, lenvatinib, vandetanib, and cabozantinib.[27] Newer agents working through new pathways are also tested with some good responses.[28] Thyroglobulin levels are measured to monitor for recurrence.
Differential Diagnosis
Differential diagnosis of follicular thyroid carcinoma includes a follicular variant of papillary thyroid carcinoma, papillary thyroid carcinoma, noninvasive follicular thyroid neoplasm with papillary-like nuclear features or NIFTP, and follicular adenoma.[29] There is a controversy with the pathologic diagnosis of follicular thyroid carcinoma, and identification could differ from one pathologist to the other. This controversy is due to two factors: the degree of nuclear atypia and the degree of capsular or vascular invasion.[21][30]
NIFTP is one of the newest categories added to the pathology description of thyroid cancer cases. It is now considered benign, so it is recommended to be treated as such.[31][32][33] Special criteria for ultrasound radiologic diagnosis are being developed for distinguishing malignant from benign lesions.[34][35][31]
Staging
The TNM staging system is used to classify differentiated thyroid carcinoma. The T describes the size of the tumor. Tx indicates that the primary tumor cannot be assessed, T0 means the tumor is not palpable, T1 means less than 1cm, T2 means the tumor is 1 to 4 cm, T3 indicates it is greater than 4 cm, and T4 means any tumor size with extrapyramidal invasion. The N signifies lymph node involvement. Nx signifies regional adenopathy is not assessable, N0 means no palpable cervical adenopathy, N1 means ipsilateral cervical adenopathy, N2 means contralateral or bilateral cervical adenopathy, and finally, N3 means fixed cervical nodes. M means metastasis, with M0 indicative of no distant metastasis, and M1 indicates distant metastasis. Follicular thyroid carcinoma is classified into stages from I through IV. Stage I under 45 years old is any T, N, and M0, and over 45 years old is T1, N0, M0; for stage II under 45 years old is any T, N, and M1, and over 45 years old is T2, N0, M0; stage III is described for over 45 years of age with T4, N0, M0, and stage IV is described with any T, N, M1.[18]
Prognosis
The thyroid cancer death rate has remained steady despite the increase in incidence. It is one of the lowest mortality cancers in the United States.[36] In 2017, an estimated 2010 death occurred due to thyroid cancer compared to more than 150,000 deaths from lung cancer.[17] Follicular thyroid cancer has a worse prognosis compared to papillary thyroid cancer due to its higher incidence of distant metastasis and patients frequently presenting with more advanced-stage disease.[17]
Even though follicular thyroid cancers have distant metastasis, metastasis to lymph nodes is uncommon, and occurrence is estimated to be fewer than 10%.[37] On the other hand, some studies reported that there is no prognostic difference between follicular thyroid cancer and papillary thyroid cancer when controlling for factors such as age and sex.[21][38][39]
The overall 10-year survival of follicular cancer depends on the level of invasiveness. For minimally invasive cancers, 10-year survival is reported to be 98%, and for invasive follicular cancer, it is 80%.[7] Some studies report that the survival rate ranges from 46% to 97%, depending on the degree of capsular or vascular invasion.[21] The mortality rate of follicular thyroid carcinoma ranges from 5 to 15%, and those with capsular invasive characteristics have an overall worse prognosis than those without invasion.[40][41]
Complications
The most worrisome complication involved in follicular thyroid cancer is metastasis. Studies have reported metastases mostly to bones, lungs, and lymph nodes. In a study done by Parasmeswaran et al. (2017), they found that 42% of their subjects had metastasis to the bones, 33% to the lungs, and 8% to the lymph nodes.[3] The incidence of distance metastasis in follicular thyroid carcinoma is estimated to be 6 to 20%.[42]
Other complications correlate with surgery. The external and recurrent laryngeal nerves are near the thyroid gland and can mistakenly get damaged during surgery or resected due to invasion.[43] This will cause hoarseness in the patient's voice. There are also reports of hematoma and keloid formation in some patients after the surgery.[43]
Because the patient is undergoing total thyroidectomy, hypothyroidism will always develop, and patients will require thyroxine replacement therapy.
Deterrence and Patient Education
Although the prognosis of thyroid cancer has been reported to be good compared to other forms of cancer, the mention of the word "cancer" will still be a concern for most patients. For instance, most patients will still opt for surgical thyroid removal even if they have non-invasive follicular thyroid cancer that can be followed due to its slow growth. Patients and their physicians must work together to decide the best treatment option.[4] Knowledge gained by patients will enable them to make better decisions about their health.
Enhancing Healthcare Team Outcomes
The incidence of thyroid cancer has increased over the past few decades, attributed to its overdiagnosis.[44][45] As a result, in 2017, USPTF recommended against screening for thyroid cancer with either neck palpation or ultrasound in asymptomatic patients.[17] In 2015, the American thyroid association recommended active surveillance of low-risk thyroid carcinomas with serial ultrasound and that not all patients require surgery. Also, the organization released guidelines in 2015, not to biopsy thyroid nodules that are less than 1 cm.[17]
Health providers, including clinicians (MDs, DOs, NPs, and PAs) and other healthcare professionals (e.g., nurses and pharmacists), should operate as an interprofessional team. All interprofessional team members must coordinate their activities using open communication channels and maintain accurate and updated patient records. They should all be aware of these guidelines; this will prevent potential harm to patients from overtreatment of low-risk thyroid cancers and help appropriately treat patients with high-risk diseases. Reportedly, the overall cost of thyroid cancer in 2019 was nearly 21 billion dollars due to surgery costs.[17] Not all thyroid neoplasms require surgery, and physicians should keep this in mind when managing patients who develop thyroid cancer.
Media
(Click Image to Enlarge)
References
Lee J, Yi S, Kang YE, Kim HW, Joung KH, Sul HJ, Kim KS, Shong M. Morphological and Functional Changes in the Thyroid Follicles of the Aged Murine and Humans. Journal of pathology and translational medicine. 2016 Nov:50(6):426-435 [PubMed PMID: 27737529]
Liu Y, Su L, Xiao H. Review of Factors Related to the Thyroid Cancer Epidemic. International journal of endocrinology. 2017:2017():5308635. doi: 10.1155/2017/5308635. Epub 2017 May 2 [PubMed PMID: 28555155]
Parameswaran R, Shulin Hu J, Min En N, Tan WB, Yuan NK. Patterns of metastasis in follicular thyroid carcinoma and the difference between early and delayed presentation. Annals of the Royal College of Surgeons of England. 2017 Feb:99(2):151-154. doi: 10.1308/rcsann.2016.0300. Epub 2016 Sep 23 [PubMed PMID: 27659362]
Wallner LP, Banerjee M, Reyes-Gastelum D, Hamilton AS, Ward KC, Lubitz C, Hawley ST, Haymart MR. Multilevel Factors Associated With More Intensive Use of Radioactive Iodine for Low-Risk Thyroid Cancer. The Journal of clinical endocrinology and metabolism. 2021 May 13:106(6):e2402-e2412. doi: 10.1210/clinem/dgab139. Epub [PubMed PMID: 33687063]
Eberhardt NL, Grebe SK, McIver B, Reddi HV. The role of the PAX8/PPARgamma fusion oncogene in the pathogenesis of follicular thyroid cancer. Molecular and cellular endocrinology. 2010 May 28:321(1):50-6. doi: 10.1016/j.mce.2009.10.013. Epub 2009 Oct 31 [PubMed PMID: 19883731]
Level 3 (low-level) evidenceMarotta V, Bifulco M, Vitale M. Significance of RAS Mutations in Thyroid Benign Nodules and Non-Medullary Thyroid Cancer. Cancers. 2021 Jul 27:13(15):. doi: 10.3390/cancers13153785. Epub 2021 Jul 27 [PubMed PMID: 34359686]
McHenry CR, Phitayakorn R. Follicular adenoma and carcinoma of the thyroid gland. The oncologist. 2011:16(5):585-93. doi: 10.1634/theoncologist.2010-0405. Epub 2011 Apr 11 [PubMed PMID: 21482585]
Williams D. Radiation carcinogenesis: lessons from Chernobyl. Oncogene. 2008 Dec:27 Suppl 2():S9-18. doi: 10.1038/onc.2009.349. Epub [PubMed PMID: 19956182]
Furukawa K, Preston D, Funamoto S, Yonehara S, Ito M, Tokuoka S, Sugiyama H, Soda M, Ozasa K, Mabuchi K. Long-term trend of thyroid cancer risk among Japanese atomic-bomb survivors: 60 years after exposure. International journal of cancer. 2013 Mar 1:132(5):1222-6. doi: 10.1002/ijc.27749. Epub 2012 Aug 16 [PubMed PMID: 22847218]
Level 2 (mid-level) evidenceAceves C, Mendieta I, Anguiano B, Delgado-González E. Molecular Iodine Has Extrathyroidal Effects as an Antioxidant, Differentiator, and Immunomodulator. International journal of molecular sciences. 2021 Jan 27:22(3):. doi: 10.3390/ijms22031228. Epub 2021 Jan 27 [PubMed PMID: 33513754]
Knobel M, Medeiros-Neto G. Relevance of iodine intake as a reputed predisposing factor for thyroid cancer. Arquivos brasileiros de endocrinologia e metabologia. 2007 Jul:51(5):701-12 [PubMed PMID: 17891233]
Level 3 (low-level) evidenceFORTNER JG, GEORGE PA, STERNBERG SS. Induced and spontaneous thyroid cancer in the Syrian (golden) hamster. Endocrinology. 1960 Mar:6():364-76 [PubMed PMID: 13855794]
Level 3 (low-level) evidenceAvgerinos KI, Spyrou N, Mantzoros CS, Dalamaga M. Obesity and cancer risk: Emerging biological mechanisms and perspectives. Metabolism: clinical and experimental. 2019 Mar:92():121-135. doi: 10.1016/j.metabol.2018.11.001. Epub 2018 Nov 13 [PubMed PMID: 30445141]
Level 3 (low-level) evidenceChoi WJ, Kim J. Dietary factors and the risk of thyroid cancer: a review. Clinical nutrition research. 2014 Jul:3(2):75-88. doi: 10.7762/cnr.2014.3.2.75. Epub 2014 Jul 29 [PubMed PMID: 25136535]
Aschebrook-Kilfoy B, Ward MH, Della Valle CT, Friesen MC. Occupation and thyroid cancer. Occupational and environmental medicine. 2014 May:71(5):366-80. doi: 10.1136/oemed-2013-101929. Epub 2014 Mar 6 [PubMed PMID: 24604144]
Nguyen QT, Lee EJ, Huang MG, Park YI, Khullar A, Plodkowski RA. Diagnosis and treatment of patients with thyroid cancer. American health & drug benefits. 2015 Feb:8(1):30-40 [PubMed PMID: 25964831]
Roman BR, Morris LG, Davies L. The thyroid cancer epidemic, 2017 perspective. Current opinion in endocrinology, diabetes, and obesity. 2017 Oct:24(5):332-336. doi: 10.1097/MED.0000000000000359. Epub [PubMed PMID: 28692457]
Level 3 (low-level) evidenceLo CY, Chan WF, Lam KY, Wan KY. Follicular thyroid carcinoma: the role of histology and staging systems in predicting survival. Annals of surgery. 2005 Nov:242(5):708-15 [PubMed PMID: 16244545]
Level 2 (mid-level) evidenceKitahara CM, Sosa JA, Shiels MS. Influence of Nomenclature Changes on Trends in Papillary Thyroid Cancer Incidence in the United States, 2000 to 2017. The Journal of clinical endocrinology and metabolism. 2020 Dec 1:105(12):e4823-30. doi: 10.1210/clinem/dgaa690. Epub [PubMed PMID: 32984898]
King AD. Imaging for staging and management of thyroid cancer. Cancer imaging : the official publication of the International Cancer Imaging Society. 2008 Mar 25:8(1):57-69. doi: 10.1102/1470-7330.2008.0007. Epub 2008 Mar 25 [PubMed PMID: 18390389]
Cipriani NA, Nagar S, Kaplan SP, White MG, Antic T, Sadow PM, Aschebrook-Kilfoy B, Angelos P, Kaplan EL, Grogan RH. Follicular Thyroid Carcinoma: How Have Histologic Diagnoses Changed in the Last Half-Century and What Are the Prognostic Implications? Thyroid : official journal of the American Thyroid Association. 2015 Nov:25(11):1209-16. doi: 10.1089/thy.2015.0297. Epub 2015 Oct 26 [PubMed PMID: 26440366]
Zanella AB, Scheffel RS, Weinert L, Dora JM, Maia AL. New insights into the management of differentiated thyroid carcinoma in children and adolescents (Review). International journal of oncology. 2021 May:58(5):. pii: 13. doi: 10.3892/ijo.2021.5193. Epub 2021 Mar 2 [PubMed PMID: 33649842]
McHenry CR, Sandoval BA. Management of follicular and Hürthle cell neoplasms of the thyroid gland. Surgical oncology clinics of North America. 1998 Oct:7(4):893-910 [PubMed PMID: 9735140]
Yu F, Li X, Ji Y, Tan J, Zhang G, Wang P, He Y, Wang R. Delayed Initial Radioiodine Adjuvant Therapy Does Affect Biochemical Response in Intermediate- to High-Risk Differentiated Thyroid Cancer. Frontiers in endocrinology. 2021:12():743310. doi: 10.3389/fendo.2021.743310. Epub 2021 Nov 9 [PubMed PMID: 34858329]
Loh KC, Greenspan FS, Gee L, Miller TR, Yeo PP. Pathological tumor-node-metastasis (pTNM) staging for papillary and follicular thyroid carcinomas: a retrospective analysis of 700 patients. The Journal of clinical endocrinology and metabolism. 1997 Nov:82(11):3553-62 [PubMed PMID: 9360506]
Level 2 (mid-level) evidenceForrer F, Fischer GF, Maas O, Giovanella L, Hoffmann M, Iakovou I, Luster M, Mihailovic J, Petranovic Ovčariček P, Vrachimis A, Zerdoud S, Putora PM. Variations in Radioiodine Therapy in Europe: Decision-Making after Total Thyroidectomy. Oncology. 2022:100(2):74-81. doi: 10.1159/000520938. Epub 2021 Nov 17 [PubMed PMID: 34788758]
Raue F, Frank-Raue K. Thyroid Cancer: Risk-Stratified Management and Individualized Therapy. Clinical cancer research : an official journal of the American Association for Cancer Research. 2016 Oct 15:22(20):5012-5021 [PubMed PMID: 27742787]
Xu G, Chen J, Wang G, Xiao J, Zhang N, Chen Y, Yu H, Wang G, Zhao Y. Resveratrol Inhibits the Tumorigenesis of Follicular Thyroid Cancer via ST6GAL2-Regulated Activation of the Hippo Signaling Pathway. Molecular therapy oncolytics. 2020 Mar 27:16():124-133. doi: 10.1016/j.omto.2019.12.010. Epub 2020 Jan 10 [PubMed PMID: 32055676]
Chen DW, Rob FI, Mukherjee R, Giordano TJ, Haymart MR, Banerjee M. Variation in the Diagnosis of Noninvasive Follicular Thyroid Neoplasm with Papillary-like Nuclear Features. The Journal of clinical endocrinology and metabolism. 2022 Sep 28:107(10):e4072-e4077. doi: 10.1210/clinem/dgac466. Epub [PubMed PMID: 35918064]
Borowczyk M, Woliński K, Więckowska B, Jodłowska-Siewert E, Szczepanek-Parulska E, Verburg FA, Ruchała M. Sonographic Features Differentiating Follicular Thyroid Cancer from Follicular Adenoma-A Meta-Analysis. Cancers. 2021 Feb 24:13(5):. doi: 10.3390/cancers13050938. Epub 2021 Feb 24 [PubMed PMID: 33668130]
Level 1 (high-level) evidenceRuanpeng D, Cheungpasitporn W, Thongprayoon C, Hennessey JV, Shrestha RT. Systematic Review and Meta-analysis of the Impact of Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features (NIFTP) on Cytological Diagnosis and Thyroid Cancer Prevalence. Endocrine pathology. 2019 Sep:30(3):189-200. doi: 10.1007/s12022-019-09583-4. Epub [PubMed PMID: 31338752]
Level 1 (high-level) evidenceBeg S, Khan SI, Cui I, Scognamiglio T, Rao R. Analysis of a pre-2017 follicular variant papillary thyroid carcinoma cohort reclassified as noninvasive follicular thyroid neoplasm with papillary-like features (NIFTP): an 11-year retrospective single institution experience. Journal of the American Society of Cytopathology. 2023 Mar-Apr:12(2):112-119. doi: 10.1016/j.jasc.2022.09.006. Epub 2022 Sep 29 [PubMed PMID: 36372672]
Level 2 (mid-level) evidenceMainthia R, Wachtel H, Chen Y, Mort E, Parangi S, Sadow PM, Lubitz CC. Evaluating the projected surgical impact of reclassifying noninvasive encapsulated follicular variant of papillary thyroid cancer as noninvasive follicular thyroid neoplasm with papillary-like nuclear features. Surgery. 2018 Jan:163(1):60-65. doi: 10.1016/j.surg.2017.04.037. Epub 2017 Nov 13 [PubMed PMID: 29146229]
Xu D, Wang Y, Wu H, Lu W, Chang W, Yao J, Yan M, Peng C, Yang C, Wang L, Xu L. An artificial intelligence ultrasound system's ability to distinguish benign from malignant follicular-patterned lesions. Frontiers in endocrinology. 2022:13():981403. doi: 10.3389/fendo.2022.981403. Epub 2022 Oct 31 [PubMed PMID: 36387869]
Level 2 (mid-level) evidenceYang GCH, Fried KO. Pathologic basis of the sonographic differences between thyroid cancer and noninvasive follicular thyroid neoplasm with papillary-like nuclear features. Ultrasonography (Seoul, Korea). 2018 Apr:37(2):157-163. doi: 10.14366/usg.17045. Epub 2017 Aug 19 [PubMed PMID: 29137452]
Bauer AJ. Papillary and Follicular Thyroid Cancer in children and adolescents: Current approach and future directions. Seminars in pediatric surgery. 2020 Jun:29(3):150920. doi: 10.1016/j.sempedsurg.2020.150920. Epub 2020 May 16 [PubMed PMID: 32571505]
Level 3 (low-level) evidenceThompson LD, Wieneke JA, Paal E, Frommelt RA, Adair CF, Heffess CS. A clinicopathologic study of minimally invasive follicular carcinoma of the thyroid gland with a review of the English literature. Cancer. 2001 Feb 1:91(3):505-24 [PubMed PMID: 11169933]
Asban A, Chung SK, Xie R, Lindeman BM, Balentine CJ, Kirklin JK, Chen H. Gender and Racial Disparities in Survival After Surgery Among Papillary and Patients With Follicular Thyroid Cancer: A 45-Year Experience. Clinical medicine insights. Endocrinology and diabetes. 2019:12():1179551419866196. doi: 10.1177/1179551419866196. Epub 2019 Sep 25 [PubMed PMID: 31598065]
Su DH, Chang TC, Chang SH. Prognostic factors on outcomes of follicular thyroid cancer. Journal of the Formosan Medical Association = Taiwan yi zhi. 2019 Jul:118(7):1144-1153. doi: 10.1016/j.jfma.2018.11.010. Epub 2018 Dec 10 [PubMed PMID: 30541677]
Hassan A, Khalid M, Riaz S, Nawaz MK, Bashir H. Follicular Thyroid Carcinoma: Disease Response Evaluation Using American Thyroid Association Risk Assessment Guidelines. European thyroid journal. 2015 Dec:4(4):260-5. doi: 10.1159/000442237. Epub 2015 Nov 25 [PubMed PMID: 26835430]
Gillanders SL, O'Neill JP. Prognostic markers in well differentiated papillary and follicular thyroid cancer (WDTC). European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2018 Mar:44(3):286-296. doi: 10.1016/j.ejso.2017.07.013. Epub 2017 Aug 3 [PubMed PMID: 28801060]
Mihailovic J, Stefanovic L, Malesevic M. Differentiated thyroid carcinoma with distant metastases: probability of survival and its predicting factors. Cancer biotherapy & radiopharmaceuticals. 2007 Apr:22(2):250-5 [PubMed PMID: 17600472]
D'Avanzo A, Treseler P, Ituarte PH, Wong M, Streja L, Greenspan FS, Siperstein AE, Duh QY, Clark OH. Follicular thyroid carcinoma: histology and prognosis. Cancer. 2004 Mar 15:100(6):1123-9 [PubMed PMID: 15022277]
Level 2 (mid-level) evidenceTakano T. Natural history of thyroid cancer [Review]. Endocrine journal. 2017 Mar 31:64(3):237-244. doi: 10.1507/endocrj.EJ17-0026. Epub 2017 Feb 2 [PubMed PMID: 28154351]
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer research. 2014 Jun 1:74(11):2913-21. doi: 10.1158/0008-5472.CAN-14-0155. Epub [PubMed PMID: 24840647]